-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Successes and Challenges on the Road to Cure Hepatitis C
article has not abstract
Published in the journal: . PLoS Pathog 11(6): e32767. doi:10.1371/journal.ppat.1004854
Category: Pearls
doi: https://doi.org/10.1371/journal.ppat.1004854Summary
article has not abstract
Introduction
Hepatitis C virus (HCV) represents a significant health burden worldwide, with an estimated 185 million people chronically infected [1]. A leading cause of liver transplantation, HCV infection can result in severe liver disease including cirrhosis and hepatocellular carcinoma [2]. Cure of HCV infection results in substantial decreases in such liver-related morbidity and mortality [3]. Prior therapies for HCV offered only 40% cure for the most difficult-to-treat genotype-1 infection, required 48 weeks of therapy with an injectable interferon, and included significant adverse events [4]. The past year has seen the approval of five interferon-free direct-acting antiviral (DAA) regimens for HCV, including combinations of DAAs and fixed-dose combination pills (Tables 1 and 2) [5–13]. Sustained virologic response (SVR), the virologic surrogate for clinical cure, has improved to >90% for most populations across all HCV genotypes (Table 2). While the successes attributable to DAA combination therapies will be many, there also remain challenges and much for us to learn as we embark on this journey to eradicate HCV. Here, we will discuss several of the greatest successes and future challenges in HCV therapeutics today.
Tab. 1. All-oral direct acting antiviral regimens available for clinical use. 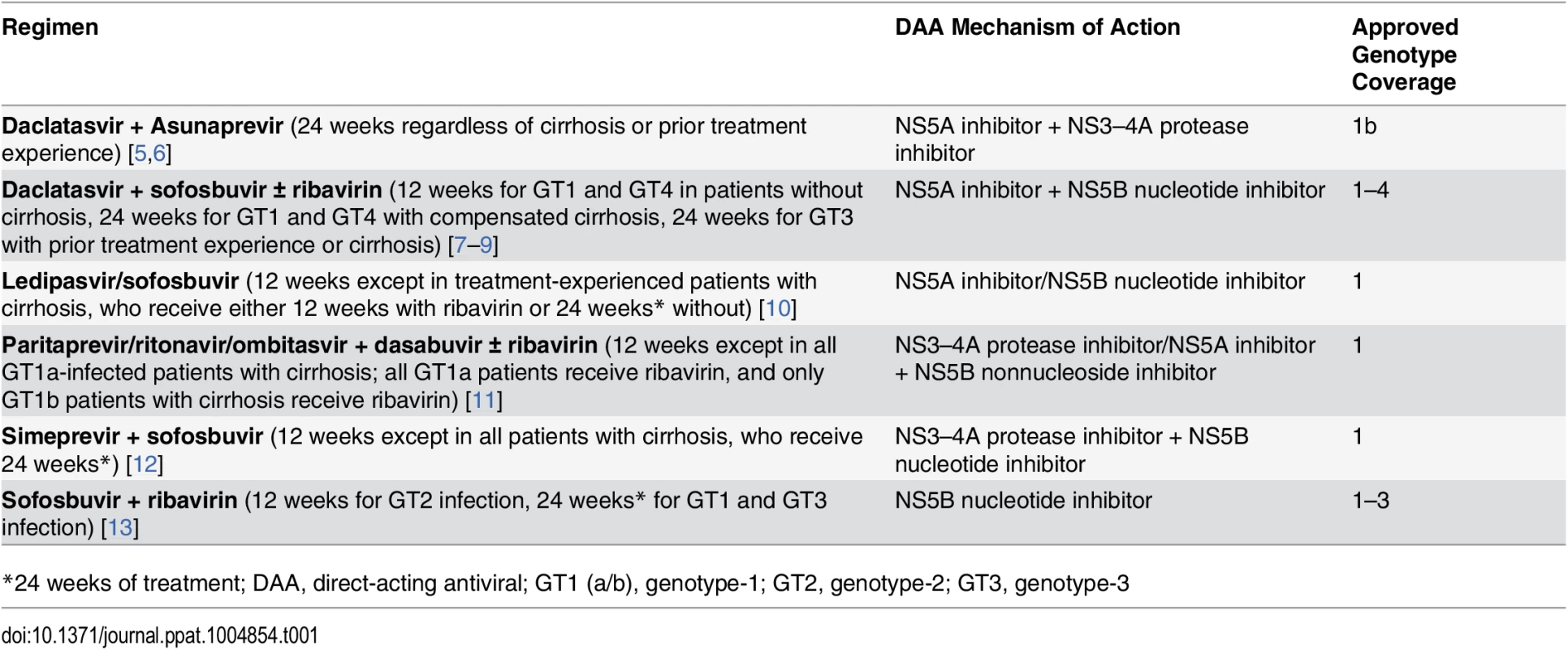
*24 weeks of treatment; DAA, direct-acting antiviral; GT1 (a/b), genotype-1; GT2, genotype-2; GT3, genotype-3 Tab. 2. Sustained virologic response for all-oral direct acting antiviral regimens. 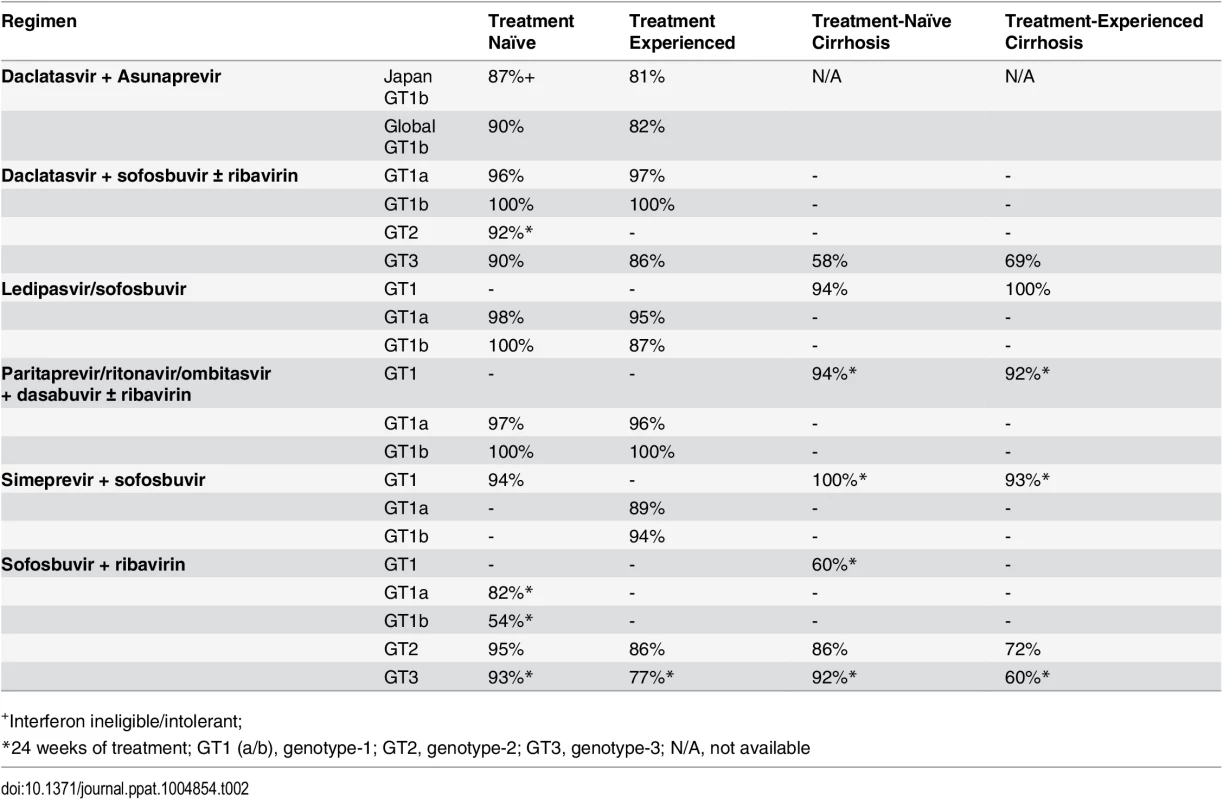
+Interferon ineligible/intolerant; Potent DAA Combinations Are Closing the Gap for Unique Patient Populations
Although all patients with HCV infection will benefit from the availability of oral DAA combination therapies, several unique patient populations have seen dramatic improvements in SVR, revealing the great clinical impact of these therapies. Specifically, patients with HIV/HCV dual infection, patients with compensated and decompensated cirrhosis, and patients who have had liver transplantation for HCV-associated liver disease are exhibiting fantastic (87%–98%) SVR rates with oral DAA combination therapy [14–16]. These patients, who have a greater risk of progression of liver disease, hepatocellular carcinoma, and death, previously had low response rates or even absolute contraindications to treatments with interferon [17–18].
The potential impact of HCV eradication for these highest-risk populations could be enormous, including decreases in hepatocellular carcinoma and liver transplantation, as well as prolonged survival for those already living with liver grafts. And yet, we do not know for sure how this story ends. While the liver has the ability to repair injured tissue [19] and there is evidence to suggest that fibrosis induced by chronic HCV infection is reversible [3], is there a point of no return? Previously, patients with HCV-associated decompensated liver disease (ascites, hepatic encephalopathy, and variceal bleeding) had only one choice for survival: organ transplantation. Is viral eradication enough to change their fate? The largest study to date in patients with decompensated cirrhosis reported SVR of nearly 90% with a DAA combination regimen [15]. Importantly, the study also reported on improvement in serum markers of synthetic liver function for a majority (>50%) of patients at post-treatment week 4. Whether these improvements translate to improved clinical outcomes over time remains to be seen, but there is reason for optimism.
HCV Genotype Diversity Has Complicated the Search for a Pangenotypic Regimen
HCV is a positive-stranded RNA virus. Its 9.6-kb genome is translated into a polyprotein that is processed into structural and nonstructural (NS; including NS3, NS4A, NS4B, NS5A, and NS5B) proteins (Fig 1) [20]. The NS proteins are the targets for the current approved DAA, including NS3–4A protease inhibitors (PI), NS5A inhibitors, and NS5B nucleot(s)ide (NA) and non-nucleoside (NNA) analogues (Table 3). A major challenge to the design and implementation of DAA for HCV is the incredible genetic diversity of HCV. HCV contains six major genotypes, as defined by phylogenetic and sequence analysis of the viral genome. These genotypes vary by 30%–35% at the nucleotide level and contain nearly 70 subtypes [20]. Clinically, this genetic diversity has translated into different regimens based on genotype and even subtype (1a versus 1b).
Fig. 1. The HCV proteins. 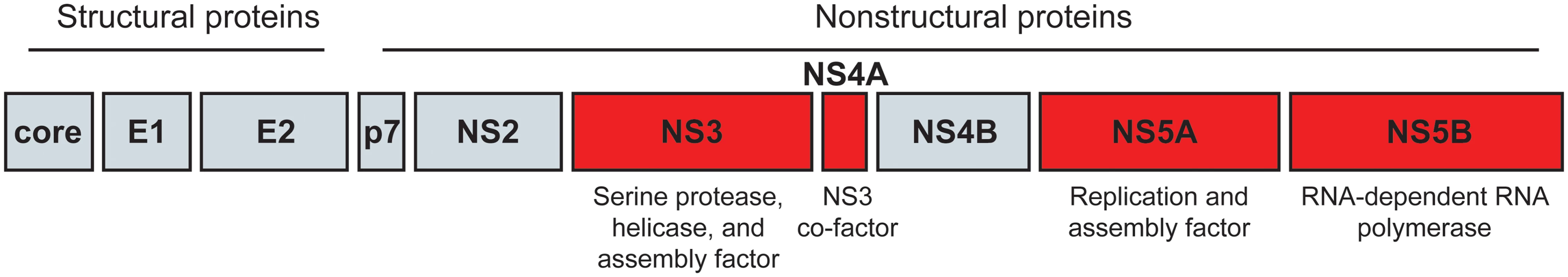
The HCV polyprotein is processed into the structural and nonstructural proteins of the virus, as shown here. The NS3–4A, NS5A, and NS5B proteins, all targets of newly developed direct-acting antivirals for HCV, are highlighted in red and their major functions described. Tab. 3. Properties of HCV direct-acting antivirals. 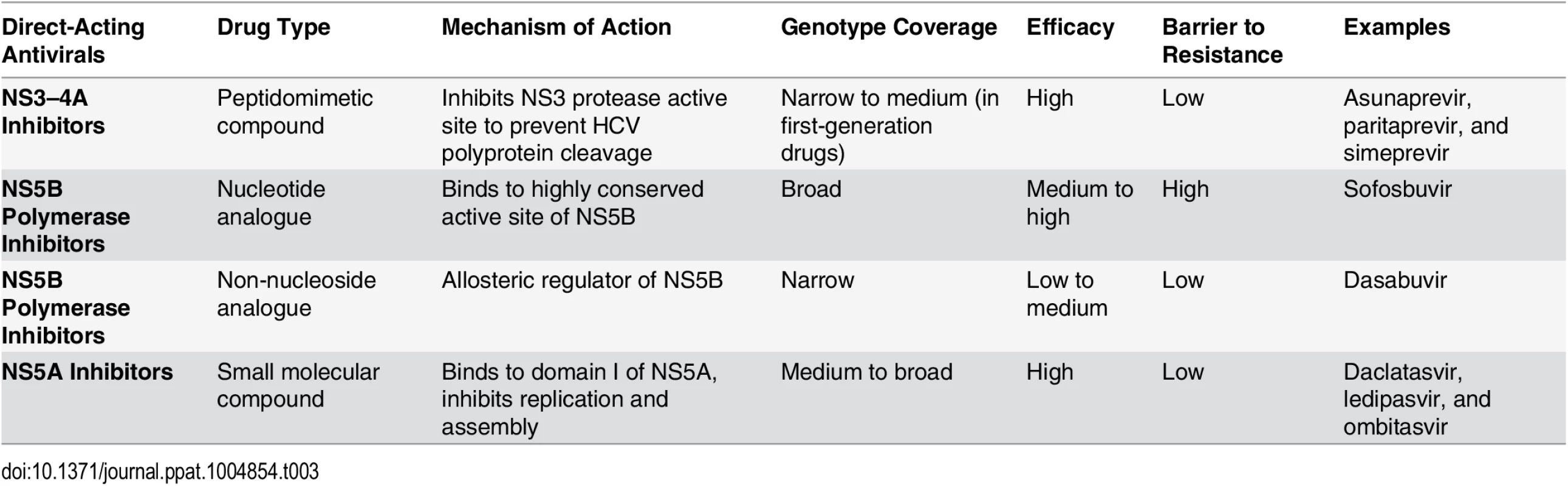
The ideal HCV DAA regimen would have pangenotype efficacy. However, because of the viral genetic diversity and mechanisms of action of the DAAs, this has been difficult to achieve. Of the five interferon-free DAA regimens available in either the United States or Europe, only two have been approved as pangenotypic regimens. The regimen of sofosbuvir, a first-in-class NA, and ribavirin was approved for genotypes 1–4 and has in vivo evidence to support efficacy in genotypes 5 and 6 [13]. While this regimen remains the standard of care for genotypes 2 and 3, its efficacy was suboptimal in the most common HCV genotype in the US, genotype 1. Daclatasvir, a pangenotypic NS5A inhibitor, when combined with sofosbuvir, provides the most potent pangenotypic activity to date and was approved in Europe for genotypes 1–4. Daclatasvir has good activity against genotype 3 and maintains activity against genotype 2 polymorphisms [7]. Unfortunately, the recently reported efficacy of 12 weeks of this regimen in genotype 3 cirrhotic patients was quite poor [8]. Other DAA regimens either lack pangenotypic coverage or have pangenotypic activity but lack clinical data in all genotypes. Ledipasvir, an NS5A inhibitor approved in combination with sofosbuvir, loses activity for a majority of genotype 2 infections because of a common NS5A polymorphism and has suboptimal in vitro activity versus genotype 3 [10]. Simeprevir, a first-generation PI approved in combination with sofosbuvir, has limited activity versus genotype 3 and has not been studied in humans for genotypes 2, 5, or 6, although it has in vitro activity [21]. The most recently approved regimen, which combines three DAAs (all with low barrier to resistance): a pangenotypic NS5A inhibitor, ombitasvir, used with a first-generation PI (paritaprevir) and an NNA (dasabuvir), is limited by the narrow genotype 1 activity of the NNA [11].
This fragmentation of treatment by genotype complicates the clinical approach to care and limits the feasibility of HCV treatment in the resource-limited setting, where genotyping and access to multiple regimens is not feasible. Moving forward, investigational second-generation PIs with broad genotypic coverage (such as MK-5172), highly potent pangenotypic NS5A inhibitors (including GS-5816), and triple DAA combinations with NA backbones are expected to help us achieve more potent pangenotypic coverage, including better options to treat genotype 3.
The Clinical Role of Resistance-Associated Variants (RAVs) Is Becoming More Clear
Viral sequences with preexisting polymorphisms can present a therapeutic challenge. The best clinical example is the preexisting NS3 Q80K polymorphism, found in 5%–48% of those with genotype 1a. This polymorphism confers resistance to simeprevir and limits its efficacy (SVR 58% versus 84%; in combination with pegylated interferon and ribavirin), thereby necessitating pretreatment polymorphism testing [12]. Combining simeprevir with the potent DAA sofosbuvir appears to overcome this limitation only in patients without cirrhosis [22,23]. Nucleotide analogues including sofosbuvir have exceptional genetic barriers to resistance. The signature RAV with sofosbuvir is the S282T mutation, which was not detected in any patient at baseline or time of virologic failure in the sofosbuvir phase 3 program [24]. Other treatment-emergent variants (TEVs) have been reported in the phase 3 program, including the L159F and V321A mutations. The change in sofosbuvir EC50 for these TEVs does not appear to be clinically significant, and retreatment of subjects with these TEVs with sofosbuvir-containing regimens did not support a role for them in treatment failure. Baseline NS5A polymorphisms that confer resistance are significantly more common and will likely be more problematic in the setting of retreatment. In a pooled resistance analysis of the ledipasvir/sofosbuvir phase 3 programs, while only 16% of patients had NS5A RAVs at baseline, significantly more patients (43%) suffering virologic failure harbored these RAVs at baseline [25]. There are now several patient subgroups in which baseline NS5A RAVs may lower SVR, including genotype 3 patients with cirrhosis treated with daclatasvir and sofosbuvir and treatment-experienced patients receiving ledipasvir and sofosbuvir [25,26]. While baseline polymorphism testing is not recommended at this time because of the overall high SVR (>90%), it may become more relevant in the setting of retreatment. The first retreatment study of prior NS5A failures confirmed that evidence of NS5A RAVs at time of retreatment confers greater risk of relapse [27].
The ability of HCV to develop de novo resistance to antiviral drugs is quite high. HCV replicates as a quasispecies; therefore, RAVs can preexist within the viral population at baseline and emerge as the dominant species during treatment. The high mutability of HCV has to do with the high error-prone nature of the HCV RNA-dependent RNA polymerase and large viral populations [28]. In fact, it has been predicted that in a single day, HCV can generate genomes with all possible single and double nucleotide changes, and as long as these genomes maintain fitness, they could confer antiviral resistance [28]. This same model predicted that combination DAA regimens would require a genetic barrier of four or more resistance mutations to achieve clinical efficacy.
Each class of DAAs can select for RAVs; however, the genetic barriers and fitness of these RAVs varies. NAs inherently have high barriers to resistance, because they directly target the conserved polymerase active site and resistant variants have low fitness [28]. On the other hand, NS5A inhibitors, PIs, and NNAs all have low barriers to resistance, with single amino acid substitutions conferring high-level resistance. In the minority of patients who suffer virologic failure during DAA combination therapy, dual and triple RAVs are being reported [10–13].
What happens to RAVs after the cessation of treatment? This depends on the fitness of those variants. For first-generation PIs, a recent report of long-term follow-up of patients treated with boceprevir (first-generation NS3–NS4A PI) found that after 3 years, 27% of patients still had RAVs and that the median time for all RAVs to become undetectable was 1.11 years [29]. This carries important clinical implications for retreatment decisions in a patient with RAVs. For example, NS5A RAVs exhibit more replicative fitness and can persist for >96 weeks [30]. Early retreatment studies suggest this will impact success of retreatment and thus significantly limit options for patients with NS5A RAVs for the foreseeable future [27].
Even with Highly Effective DAA Combination Therapies, Some Historic Baseline Predictors of SVR Remain
One of the greatest surprises thus far in the new era of treating HCV is that some of the same factors that predicted response to interferon therapies still play a role in DAA response rates. Although SVR rates are high across all subgroups, recent pooled multivariable analyses of phase 3 trials provide some granularity on treatment response. While these predictors may vary across regimens, higher rates of relapse are being reported in patients based on genotype subtype, presence of cirrhosis (in particular those with prior treatment failure), IL28B TT genotype, sex, race, and higher baseline HCV RNA [31,32]. Based on the presence or absence of these predictors, some patients may achieve SVR with 8 weeks of therapy, while others require 24 weeks. Moving forward, these “difficult-to-treat” populations should be targeted for innovative approaches to therapy so that no patient is left without a chance of cure.
Our Greatest Challenge Just Might Be of Our Own Making
Direct-acting antivirals for HCV are likely to be heralded as one of medicine’s greatest advancements. The possibility of eradicating HCV from the globe seems within arm’s reach. With SVR pushing 100% for many HCV-infected populations and ongoing studies pushing the limits of treatment to just 6 weeks with triple DAA combinations, there is much reason for hope. Yet, the unfortunate reality is that because of the high cost of these medications, many patients will be denied coverage and the opportunity for cure. Many payers are only providing coverage to those patients with the highest stages of fibrosis. Is there another precedent in medicine in which we don’t treat a curable transmissible disease? The recent exclusivity agreements between Express Scripts and AbbVie and CVS/Caremark and Gilead mark a new era in the battle against HCV, although in this case we seem to be battling against ourselves. We should carefully consider the consequences of pricing and such relationships, as much of this has overshadowed the bright light of medical innovation—what a shame.
Zdroje
1. Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013;57 : 1333–1342. doi: 10.1002/hep.26141 23172780
2. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380 : 2095–128. doi: 10.1016/S0140-6736(12)61728-0 23245604
3. Mallet V, Gilgenkrantz H, Serpaggi J, Verkarre V, Vallet-Pichard et al. Brief Communication: The Relationship of Regression of Cirrhosis to Outcome in Chronic Hepatitis C. Annals Int Med. 2008;149 : 399–403. 18794559
4. McHutchison JG, Lawitz EJ, Shiffman ML, Muir AJ, Galler GW, et al. Peginterferon Alfa-2b or Alfa-2a with Ribavirin for Treatment of Hepatitis C Infection. New Engl J Med. 2009;361 : 580–93. doi: 10.1056/NEJMoa0808010 19625712
5. Kumada H, Suzuki Y, Ikeda K, Toyota J, Karino Y, et al. Daclatasvir plus asunaprevir for chronic HCV genotype 1b infection. Hepatology 2014; 59 : 2083–91. doi: 10.1002/hep.27113 24604476
6. Manns M, Pol S, Jacobson IM, Marcellin P, Gordon SC, et al. All-oral daclatasvir plus asunaprevir for hepatitis C virus genotype 1b: a multinational, phase 3, multicohort study. Lancet 2014; 384 : 1597–605. doi: 10.1016/S0140-6736(14)61059-X 25078304
7. Wyles D, Ruane P, Sulkowski M, Dieterich D, Luetkemeyer AF, et al. Daclatasvir in Combination with Sofosbuvir for HIV/HCV Coinfection: ALLY-2 Study. [Abstract 151LB] Conference on Retroviruses and Opportunistic Infections (CROI). February 23–26; Seattle, WA.
8. Nelson DR, Cooper JN, Lalezari JP et al. All-oral 12-week treatment with daclatasvir (DCV) and sofosbuvir (SOF) in patients infected with hepatitis C virus genotype 3 infection: ALLY-3 phase 3 study. Hepatology 2015;61 : 1127–35. doi: 10.1002/hep.27726 25614962
9. Sulkowski MS, Gardiner DF, Rodriguez-Torres M, Reddy KR, Hassanein T, et al. Daclatasvir plus Sofosbuvir for Previously Treated or Untreated Chronic HCV Infection. New Engl J Med. 2014;370 : 211–221. doi: 10.1056/NEJMoa1306218 24428467
10. Harvoni [package insert]. Gilead Sciences, Inc., Foster City, CA; 2014.
11. Pak Viekira [package insert]. AbbVie, Inc., North Chicago, IL; 2014.
12. Olysio [package insert]. Janssen Therapeutics, Titusville, NJ; 2013.
13. Sovaldi [package insert]. Gilead Sciences, Inc., Foster City, CA; 2013.
14. Sulkowski MS, Naggie S, Lalezari J, Fessel WJ, Mounzer K, et al. Sofosbuvir and Ribavirin for Hepatitis C in Patients with HIV Coinfection. JAMA. 2014;312 : 353–361. doi: 10.1001/jama.2014.7734 25038354
15. Flamm SL, Everson GT, Charlton M, Denning JM, Arterburn S, et al. Ledipasvir/sofosbuvir with ribavirin for the treatment of HCV in patients with decompensated cirrhosis: preliminary results of a prospective, multicenter study. 65th Annual Meeting of the American Association for the Study of Liver Diseases (AASLD). November 1–5, 2014; Boston, MA.
16. Reddy KR, Everson GT, Flamm SL, Denning JM, Arterburn S, et al. Ledipasvir/sofosbuvir with ribavirin for the treatment of HCV in patients with post transplant recurrence: preliminary results of a prospective, multicenter study. [Abstract 8.] 65th Annual Meeting of the American Association for the Study of Liver Diseases (AASLD). November 7–11, 2014; Boston, MA.
17. Lo Re V, Kallan MJ, Tate JP, et al. Hepatic decompensation in antiretroviral-treated patients co-infected with HIV and hepatitis C virus compared with hepatitis C virus-monoinfected patients: a cohort study. Ann Intern Med. 2014; 160 : 369–79. doi: 10.7326/M13-1829 24723077
18. Chung RT, Andersen J, Volberding P, Robbins GK, Liu T, et al. Peginterferon Alfa-2a plus Ribavirin versus Interferon Alfa-2a plus Ribavirin for Chronic Hepatitis C in HIV-Coinfected Persons. N Engl J Med. 2004;351 : 451–9. 15282352
19. Falkowski O, An HJ, Ianus IA, Chiriboga L, Yee H, West AB, et al. Regeneration of hepa - tocyte “buds” in cirrhosis from intrabiliary stem cells. J Hepatol 2003;39 : 357–64. 12927921
20. Smith DB, Bukh J, Kuiken C, Muerhoff AS, Rice CM, et al. (2013) Expanded classification of hepatitis C Virus into 7 genotypes and 67 Subtypes: updated criteria and assignment web resource. Hepatology 59(1): 318–327. doi: 10.1002/hep.26744 24115039
21. Moreno C, Berg T, Tanwandee T, et al. Antiviral activity of TMC435 monotherapy in patients infected with HCV genotypes 2–6: TMC435-C202, a phase IIa, open-label study. J Hepatol. 2012;56(6):1247–1253. doi: 10.1016/j.jhep.2011.12.033 22326470
22. . Kwo P, Gitlin N, Nahass R, Bernstein D, Rojter S, et al. A phase 3, randomized, open-label study to evaluate the efficacy and safety of 12 and 8 weeks of simeprevir (SMV) plus sofosbuvir (SOF) in treatment-naïve and—experienced patients with chornic HCV genotype 1 infection without cirrhosis: OPTIMIST-1. EASL April 2015, Vienna Austria. Abstract LP14.
23. Lawitz E, Matusow G, DeJesus E, Yoshida E, Felizarta F, et al. A phase 3, open-label, single-arm study to evaluate the efficacy and safety of 12 weeks of simeprevir (SMV) plus sofosbuvir (SOF) in treatment-naïve and—experienced patients with chronic HCV genotype 1 infection and cirrhosis: OPTIMIST-2. EASL April 2015, Vienna Austria. Abstract LP04.
24. Svarovskaia ES, Dvory-Sobol H, Doehle B, Gane E, Jacobson IM, et al. L159F and V321A Sofosbuvir Treatment-Emergent HCV NS5B Substitutions. 65th Annual Meeting of the American Association for the Study of Liver Diseases (AASLD). November 7–11, 2014; Boston, MA.
25. Sarrazin C, Dvory-Sobol H, Svarovskaia E, Doehle B, McCarville JF, et al. Baseline and Post-Baseline Resistance Analyses of Phase 2/3 Studies of Ledipasvir/Sofosbuvir ± RBV. [Abstract 1926] 65th Annual Meeting of the American Association for the Study of Liver Diseases (AASLD). November 7–11, 2014; Boston, MA.
26. Nelson DR, Cooper JN, Lalezari JP, Lawitz E, Pockros P, et al. All-Oral 12-Week Combination Treatment With Daclatasvir and Sofosbuvir in Patients Infected with HCV Genotype 3: ALLY-3 Phase 3 Study. 24th Conference of the Asian Pacific Association for the Study of Liver Disease (APASL). March 12–15, 2015; Istanbul, Turkey.
27. Lawitz E, Flamm S, Yang JC, Pang PS, Zhu Y, et al. Retreatment of Patients who failed 8 or 12 weeks of ledipasvir/sofosbuvir-based regimens with ledipasvir/sofosbuvir for 24 weeks. EASL April 2015, Vienna Austria. Abstract O005.
28. Rong L, Dahari H, Ribeiro RM, Perelson AS (2010) Rapid emergence of protease inhibitor resistance in hepatitis C virus. Sci Transl Med 2 : 30ra32. doi: 10.1126/scitranslmed.3000544 20445200
29. Howe AYM, Long J, Nickle D, Barnard R, Thompson S, et al. Long-term follow-up of patients receiving boceprevir for treatment of chronic hepatitis C. Antiviral Res. 2015;113 : 71–78. doi: 10.1016/j.antiviral.2014.10.010 25446895
30. Dvory-Sobol H, Wyles D, Ouyang W, Chodavarapu K, McNally J, et al. Long-Term Persistence of HCV NS5A Variants After Treatment with NS5A Inhibitor Ledipasvir. EASL April 2015, Vienna Austria. Abstract O059.
31. Fried MW, Forns X, Reau N, Wedemeyer H, Shiffman ML, et al. TURQUIOSE-II: Regimens of ABT-450/r/ombitasvir and Dasabuvir with Ribavirin Achieve High SVR12 Rates in HCV Genotype 1-Infected Patients with Cirrhosis, Regardless of Baseline Characteristics. [Abstract 81] 65th Annual Meeting of the American Association for the Study of Liver Diseases (AASLD). November 7–11, 2014; Boston, MA.
32. Naggie S, Cooper C, Saag M, Yang J, Stamm L, et al. Ledipasvir/Sofosbuvir for 12 Weeks in Patients Coinfected with HCV and HIV-1. [Abstract 152LB] Conference on Retroviruses and Opportunistic Infections (CROI). February 23–26; Seattle, WA.
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek Clearance of Pneumococcal Colonization in Infants Is Delayed through Altered Macrophage TraffickingČlánek An Model of Latency and Reactivation of Varicella Zoster Virus in Human Stem Cell-Derived NeuronsČlánek Protective mAbs and Cross-Reactive mAbs Raised by Immunization with Engineered Marburg Virus GPsČlánek Specific Cell Targeting Therapy Bypasses Drug Resistance Mechanisms in African TrypanosomiasisČlánek Peptidoglycan Branched Stem Peptides Contribute to Virulence by Inhibiting Pneumolysin ReleaseČlánek HIV Latency Is Established Directly and Early in Both Resting and Activated Primary CD4 T CellsČlánek Sequence-Specific Fidelity Alterations Associated with West Nile Virus Attenuation in Mosquitoes
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2015 Číslo 6- Stillova choroba: vzácné a závažné systémové onemocnění
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
- Diagnostika virových hepatitid v kostce – zorientujte se (nejen) v sérologii
- Jak souvisí postcovidový syndrom s poškozením mozku?
- Familiární středomořská horečka
-
Všechny články tohoto čísla
- Introducing “Research Matters”
- Exploring Host–Pathogen Interactions through Biological Control
- Analysis of Bottlenecks in Experimental Models of Infection
- Expected and Unexpected Features of the Newly Discovered Bat Influenza A-like Viruses
- Clearance of Pneumococcal Colonization in Infants Is Delayed through Altered Macrophage Trafficking
- Recombinant Murine Gamma Herpesvirus 68 Carrying KSHV G Protein-Coupled Receptor Induces Angiogenic Lesions in Mice
- TRIM30α Is a Negative-Feedback Regulator of the Intracellular DNA and DNA Virus-Triggered Response by Targeting STING
- Targeting Human Transmission Biology for Malaria Elimination
- Two Cdc2 Kinase Genes with Distinct Functions in Vegetative and Infectious Hyphae in
- An Model of Latency and Reactivation of Varicella Zoster Virus in Human Stem Cell-Derived Neurons
- Protective mAbs and Cross-Reactive mAbs Raised by Immunization with Engineered Marburg Virus GPs
- Virulence Factors of Induce Both the Unfolded Protein and Integrated Stress Responses in Airway Epithelial Cells
- Peptide-MHC-I from Endogenous Antigen Outnumber Those from Exogenous Antigen, Irrespective of APC Phenotype or Activation
- Specific Cell Targeting Therapy Bypasses Drug Resistance Mechanisms in African Trypanosomiasis
- An Ultrasensitive Mechanism Regulates Influenza Virus-Induced Inflammation
- The Role of Human Transportation Networks in Mediating the Genetic Structure of Seasonal Influenza in the United States
- Host Delivery of Favorite Meals for Intracellular Pathogens
- Complement-Opsonized HIV-1 Overcomes Restriction in Dendritic Cells
- Inter-Seasonal Influenza is Characterized by Extended Virus Transmission and Persistence
- A Critical Role for CLSP2 in the Modulation of Antifungal Immune Response in Mosquitoes
- Twilight, a Novel Circadian-Regulated Gene, Integrates Phototropism with Nutrient and Redox Homeostasis during Fungal Development
- Surface-Associated Lipoproteins Link Virulence to Colitogenic Activity in IL-10-Deficient Mice Independent of Their Expression Levels
- Latent Membrane Protein LMP2A Impairs Recognition of EBV-Infected Cells by CD8+ T Cells
- Bank Vole Prion Protein As an Apparently Universal Substrate for RT-QuIC-Based Detection and Discrimination of Prion Strains
- Neuronal Subtype and Satellite Cell Tropism Are Determinants of Varicella-Zoster Virus Virulence in Human Dorsal Root Ganglia Xenografts
- Molecular Basis for the Selective Inhibition of Respiratory Syncytial Virus RNA Polymerase by 2'-Fluoro-4'-Chloromethyl-Cytidine Triphosphate
- Structure of the Virulence Factor, SidC Reveals a Unique PI(4)P-Specific Binding Domain Essential for Its Targeting to the Bacterial Phagosome
- Activated Brain Endothelial Cells Cross-Present Malaria Antigen
- Fungal Morphology, Iron Homeostasis, and Lipid Metabolism Regulated by a GATA Transcription Factor in
- Peptidoglycan Branched Stem Peptides Contribute to Virulence by Inhibiting Pneumolysin Release
- A Macrophage Subversion Factor Is Shared by Intracellular and Extracellular Pathogens
- A Novel AT-Rich DNA Recognition Mechanism for Bacterial Xenogeneic Silencer MvaT
- Reovirus FAST Proteins Drive Pore Formation and Syncytiogenesis Using a Novel Helix-Loop-Helix Fusion-Inducing Lipid Packing Sensor
- The Role of ExoS in Dissemination of during Pneumonia
- IRF-5-Mediated Inflammation Limits CD8 T Cell Expansion by Inducing HIF-1α and Impairing Dendritic Cell Functions during Infection
- Discordant Impact of HLA on Viral Replicative Capacity and Disease Progression in Pediatric and Adult HIV Infection
- Crystal Structure of USP7 Ubiquitin-like Domains with an ICP0 Peptide Reveals a Novel Mechanism Used by Viral and Cellular Proteins to Target USP7
- HIV Latency Is Established Directly and Early in Both Resting and Activated Primary CD4 T Cells
- HPV16 Down-Regulates the Insulin-Like Growth Factor Binding Protein 2 to Promote Epithelial Invasion in Organotypic Cultures
- The νSaα Specific Lipoprotein Like Cluster () of . USA300 Contributes to Immune Stimulation and Invasion in Human Cells
- RSV-Induced H3K4 Demethylase KDM5B Leads to Regulation of Dendritic Cell-Derived Innate Cytokines and Exacerbates Pathogenesis
- Leukocidin A/B (LukAB) Kills Human Monocytes via Host NLRP3 and ASC when Extracellular, but Not Intracellular
- Border Patrol Gone Awry: Lung NKT Cell Activation by Exacerbates Tularemia-Like Disease
- The Curious Road from Basic Pathogen Research to Clinical Translation
- From Cell and Organismal Biology to Drugs
- Adenovirus Tales: From the Cell Surface to the Nuclear Pore Complex
- A 21st Century Perspective of Poliovirus Replication
- Is Development of a Vaccine against Feasible?
- Waterborne Viruses: A Barrier to Safe Drinking Water
- Battling Phages: How Bacteria Defend against Viral Attack
- Archaea in and on the Human Body: Health Implications and Future Directions
- Degradation of Human PDZ-Proteins by Human Alphapapillomaviruses Represents an Evolutionary Adaptation to a Novel Cellular Niche
- Natural Variants of the KPC-2 Carbapenemase have Evolved Increased Catalytic Efficiency for Ceftazidime Hydrolysis at the Cost of Enzyme Stability
- Potent Cell-Intrinsic Immune Responses in Dendritic Cells Facilitate HIV-1-Specific T Cell Immunity in HIV-1 Elite Controllers
- The Mammalian Cell Cycle Regulates Parvovirus Nuclear Capsid Assembly
- Host Reticulocytes Provide Metabolic Reservoirs That Can Be Exploited by Malaria Parasites
- The Proteome of the Isolated Containing Vacuole Reveals a Complex Trafficking Platform Enriched for Retromer Components
- NK-, NKT- and CD8-Derived IFNγ Drives Myeloid Cell Activation and Erythrophagocytosis, Resulting in Trypanosomosis-Associated Acute Anemia
- Successes and Challenges on the Road to Cure Hepatitis C
- BRCA1 Regulates IFI16 Mediated Nuclear Innate Sensing of Herpes Viral DNA and Subsequent Induction of the Innate Inflammasome and Interferon-β Responses
- A Structural and Functional Comparison Between Infectious and Non-Infectious Autocatalytic Recombinant PrP Conformers
- Phosphorylation of the Peptidoglycan Synthase PonA1 Governs the Rate of Polar Elongation in Mycobacteria
- Human Immunodeficiency Virus Type 1 Nef Inhibits Autophagy through Transcription Factor EB Sequestration
- Sequence-Specific Fidelity Alterations Associated with West Nile Virus Attenuation in Mosquitoes
- EBV BART MicroRNAs Target Multiple Pro-apoptotic Cellular Genes to Promote Epithelial Cell Survival
- Single-Cell and Single-Cycle Analysis of HIV-1 Replication
- TRIM32 Senses and Restricts Influenza A Virus by Ubiquitination of PB1 Polymerase
- The Herpes Simplex Virus Protein pUL31 Escorts Nucleocapsids to Sites of Nuclear Egress, a Process Coordinated by Its N-Terminal Domain
- Host Transcriptional Response to Influenza and Other Acute Respiratory Viral Infections – A Prospective Cohort Study
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- HIV Latency Is Established Directly and Early in Both Resting and Activated Primary CD4 T Cells
- Battling Phages: How Bacteria Defend against Viral Attack
- A 21st Century Perspective of Poliovirus Replication
- Adenovirus Tales: From the Cell Surface to the Nuclear Pore Complex
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



