-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Adventures in Wonderland
article has not abstract
Published in the journal: . PLoS Genet 11(4): e32767. doi:10.1371/journal.pgen.1005086
Category: Perspective
doi: https://doi.org/10.1371/journal.pgen.1005086Summary
article has not abstract
For the last several decades, there has been little debate over the origins of central and peripheral glia. Central nervous system (CNS) glia, including oligodendrocytes, astrocytes, and radial glia, are specified from CNS neural precursors[1], whereas peripheral nervous system (PNS) glia, including Schwann cells and satellite glia, are derivatives of the neural crest [2]. However, this strict delineation of central versus peripheral glia is being challenged, and the implications could revolutionize human medicine. In the February issue of PLOS Genetics, Weider and colleagues report that a cell population with characteristics very similar to CNS oligodendrocytes can arise from satellite glia in the periphery with only the overexpression of a single transcription factor [3]. This work, in conjunction with several other recent papers [4–7], has us not only peering through Alice’s looking glass but also crossing straight through.
Glial Surprises Down the Rabbit Hole
Decades of careful fate-mapping and lineage tracing has left us with the conclusion that the myelinating glia of the CNS, oligodendrocytes, are derived from spinal cord neural precursors [8]. The vast majority of these oligodendrocyte progenitor cells (OPC) originate from ventral spinal cord precursors found in the pMN domain. Their development is tightly regulated by a concert of morphogens and transcription factors, with sonic hedgehog (SHH) initiating the cascade and regulating the expression of oligodendrocyte transcription factor 2 (Olig2) [8]. Additional transcription factors come into play with Nkx2.2 and Sox10 acting as two players that, in coordination with Olig2, induce the expression of pro-myelinating genes, including proteolipid protein (Plp) and myelin basic protein (MBP) (Fig. 1A) [8]. In Multiple Sclerosis (MS), the immune system attacks and damages the myelin made by mature oligodendrocytes, ultimately leading to axon conduction deficits and severe disability. One promising avenue of research to combat this debilitating disease involves using transcription factor-mediated reprogramming to directly convert one cell type into another. In vitro, mouse fibroblasts were directly converted into OPCs using a cocktail of transcription factors that mirrors their development in vivo, including Sox10 and Olig2 [9,10]. Of these two transcription factors, Sox10 is often considered a master glial transcription factor as it is expressed by OPCs and all known peripheral glial lineages. However, these cell conversion strategies yield low efficiency of conversion and are rarely studied in vivo.
Fig. 1. Conversion of satellite glia into oligodendrocyte-like cells. 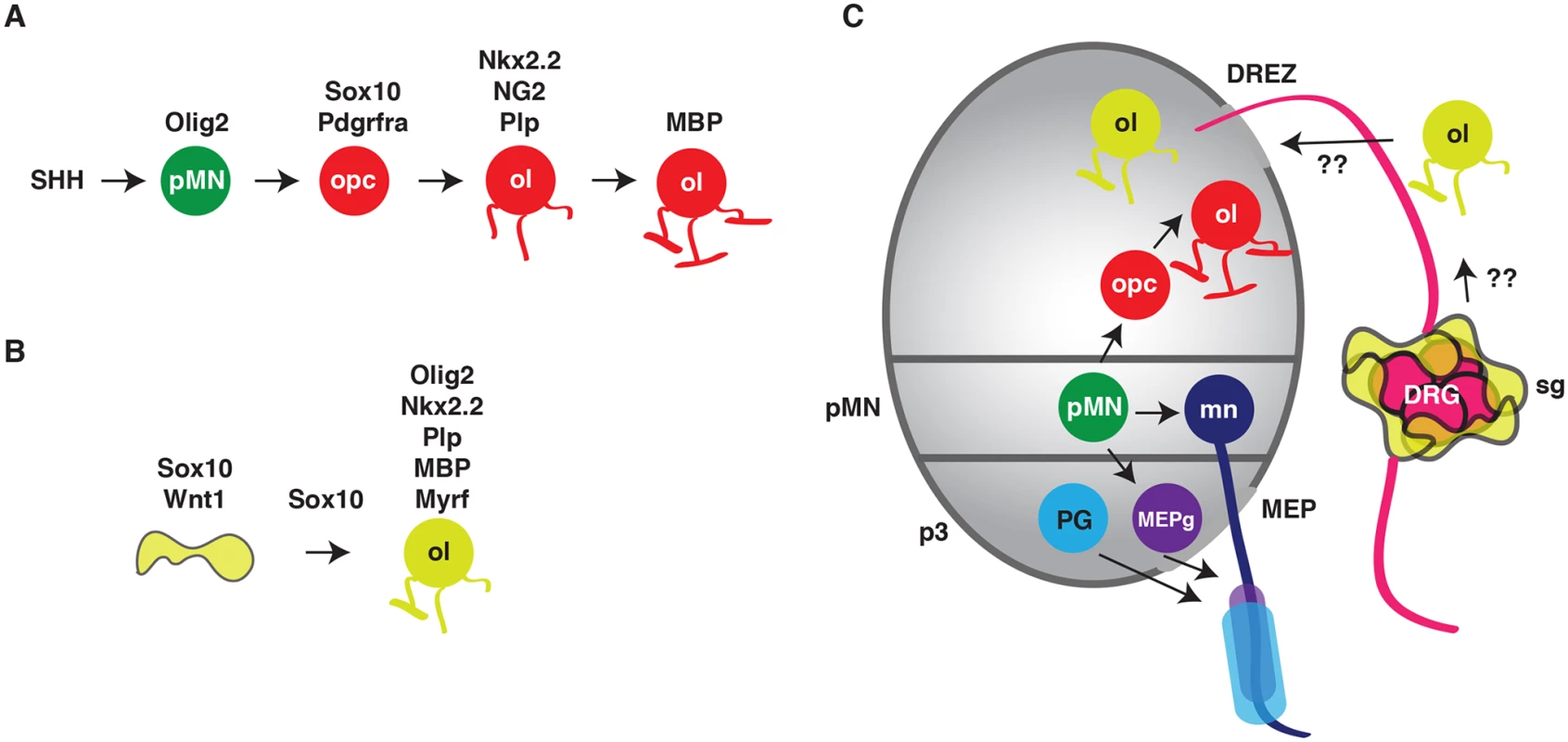
(A) In the ventral spinal cord, sonic hedgehog (SHH) induces the expression of Olig2 in pMN ventral spinal cord precursors (pMN, green circle). During gliogenesis, Olig2 initiates expression of Sox10 and other transcription factors, which leads to the specification of oligodendrocyte progenitor cells (opc, red circle). Differentiation of opcss results in mature, myelinating oligodendrocytes (ol). (B) Weider et al. present evidence that when overexpresed, Sox10 alone can convert a satellite glial cell (yellow cell) into an oligodendrocye-like cell (ol, yellow circle), which shares many of the same genetic signatures as CNS-derived oligodendrocytes. (C) Recently, a handful of papers have described that a subset of peripheral glia, including myelinating motor exit point glia (MEPg, purple cells) and perineurial glia (blue cells), arise from ventral spinal cord precursors. The work presented by Weider and colleagues raises the intriguing possibility that satellite glia (yellow cells) might normally give rise to oligodendrocyte-like cells and that they can migrate into the spinal cord via the dorsal root entry zone (DREZ) or that direct conversion of satellite glia into oligodendrocyte-like cells may be a valuable treatment option for diseases like MS if these cells could be induced to migrate directly into the spinal cord via the DREZ. This paper by Weider et al. demonstrates that overexpression of Sox10 alone can convert an already Sox10-positive satellite glial cell within the dorsal root ganglia (DRG) into oligodendrocyte-like cells in vivo (Fig. 1B) [3]. This finding has three major implications: 1) Sox10 might be the only transcription factor required to convert cells into an oligodendrocyte-like lineage, 2) there is more than one way to make an oligodendrocyte, and 3) we need to learn more about these understudied satellite glia. The authors genetically dissect this glial conversion and find that, in contrast to OPC specification in the ventral spinal cord, where Olig2 initiates gliogenesis by promoting Sox10 expression, overexpression of Sox10 in satellite glia directly activates Olig2 and it is this step in cell conversion that is key to creating oligodendrocyte-like cells in the PNS (Fig. 1B). The authors then take this information to the next level and map a Sox10 evolutionarily conserved non-coding region (ECR) upstream of the Olig2 transcriptional start site, which they call the Olig2 ECR (OLE). Weider et al. demonstrate via bioinformatics that the distal fragment of this OLE (OLEa) has fourteen potential Sox binding sites and this same OLEa is expressed in cells of the oligodendrocyte lineage in the spinal cord. Additionally, these oligodendrocyte-like cells in the DRG expressed Nkx2.2, Myrf, Plp1, and Mbp, but not Sox9, Pdgfra, and NG2, demonstrating that the conversion cascade in satellite glia is distinct from oligodendrogensis in the CNS (Fig. 1A and B). Intriguingly, when the authors attempt to recapitulate spinal cord genesis of oligodendrocytes in satellite glia by overexpressing Olig2, they observed none of the expected oligodendrocyte markers in the DRG. Therefore, conversion of satellite glia into oligodendrocyte-like cells is similar, but distinct from, normal spinal cord OPC specification.
The implications for this work are immense. In MS, repeated immune activation and attack of CNS myelin eventually leads to a loss of oligodendrocytes. Although attempted regeneration of this cell population is observed in many models of this disease, eventually, remyelination fails. These studies presented by Weider and colleagues describe, for the first time, the overexpression of a single transcription factor and its ability to convert satellite glia in the DRG into oligodendrocyte-like cells in vivo. This experimental design not only demonstrates the competency of satellite glia for conversion, but also reveals the possibility of using this method in human patients. The DRG sits immediately adjacent to the spinal cord and afferent sensory axons enter the CNS at the dorsal root entry zone (DREZ). If satellite glia can be converted to oligodendrocyte-like cells and induced to migrate into the spinal cord, these studies could represent a treatment option for patients with CNS myelinopathies, including MS, which avoid the ethical entanglements of stem cell biology and painful cell infusions.
Through the Looking Glass
These fascinating studies not only impact human disease biology but also demand that we take a closer look at what we know about basic glial biology. What if satellite glia normally make oligodendrocytes? A second, much smaller population of spinal cord oligodendrocytes are derived from dorsal spinal cord precursors [11]. Could this population also have members that are derived from peripheral satellite glia that migrate into the spinal cord via the DREZ (Fig. 1C)? Recently, a handful of studies have investigated two peripheral glial lineages that arise from ventral spinal cord precursors and migrate into the periphery via the motor exit point (MEP) [4–6]. The studies in this paper in PLOS Genetics also raise the exciting possibility that satellite glia might normally contribute cells to the CNS. This would imply that it is not just axons that connect the CNS and PNS together into functional circuits but also glial populations that do this. Further investigation into the ultimate fate of these ectopic oligodendrocyte-like cells and their precursors, and close examination of whether these phenomenon occur under normal conditions, will yield intriguing insights into not only the basic biology of satellite glia but also how these cells may be useful in treating disease. And, not unlike Alice in Wonderland, we may have to follow glia through the looking glass (or spinal cord transition zones) to discover more about the nervous system and ourselves.
Zdroje
1. Rowitch DH. Glial specification in the vertebrate neural tube. Nat Rev Neurosci. 2004;5 : 409–419. 15100723
2. Jessen K, Mirsky R. The origin and development of glial cells in peripheral nerves. Nat Rev Neurosci. 2005;6.
3. Weider M, Wegener A, Schmitt C, Küspert M, Hillgärtner S, Bösl MR, et al. Elevated In Vivo Levels of a Single Transcription Factor Directly Convert Satellite Glia into Oligodendrocyte-like Cells. PLoS Genet. 2015;11: e1005008. doi: 10.1371/journal.pgen.1005008 25680202
4. Zawadzka M, Rivers L, Fancy S, Zhao C, Tripathi R, Jamen F, et al. CNS-resident glial progenitor/stem cells produce Schwann cells as well as oligodendrocytes during repair of CNS demyelination. Cell stem cell. 2010;6.
5. Kucenas S, Takada N, Park H-C, Woodruff E, Broadie K, Appel B. CNS-derived glia ensheath peripheral nerves and mediate motor root development. Nature neuroscience. 2008;11.
6. Smith CJ, Morris AD, Welsh TG, Kucenas S. Contact-mediated inhibition between oligodendrocyte progenitor cells and motor exit point glia establishes the spinal cord transition zone. PLoS biology. 2014;12.
7. Clark J, O’Keefe A, Mastracci T, Sussel L, Matise M, Kucenas S. Mammalian Nkx2.2(+) perineurial glia are essential for motor nerve development. Developmental dynamics: an official publication of the American Association of Anatomists. 2014.
8. Rowitch DH, Kriegstein AR. Developmental genetics of vertebrate glial-cell specification. Nature. 2010;468 : 214–222. doi: 10.1038/nature09611 21068830
9. Najm FJ, Lager AM, Zaremba A, Wyatt K, Caprariello AV, Factor DC, et al. Transcription factor-mediated reprogramming of fibroblasts to expandable, myelinogenic oligodendrocyte progenitor cells. Nat Biotechnol. 2013;31 : 426–433. doi: 10.1038/nbt.2561 23584611
10. Yang N, Zuchero JB, Ahlenius H, Marro S, Ng YH, Vierbuchen T, et al. Generation of oligodendroglial cells by direct lineage conversion. Nat Biotechnol. 2013;31 : 434–439. doi: 10.1038/nbt.2564 23584610
11. Cai J, Qi Y, Hu X, Tan M, Liu Z, Zhang J, et al. Generation of oligodendrocyte precursor cells from mouse dorsal spinal cord independent of Nkx6 regulation and Shh signaling. Neuron. 2005;45 : 41–53. 15629701
Štítky
Genetika Reprodukční medicína
Článek Retraction: Astakine 2—the Dark Knight Linking Melatonin to Circadian Regulation in CrustaceansČlánek Genomic Location of the Major Ribosomal Protein Gene Locus Determines Global Growth and InfectivityČlánek Spatial Fluctuations in Expression of the Heterocyst Differentiation Regulatory Gene in FilamentsČlánek Genome-Wide Negative Feedback Drives Transgenerational DNA Methylation Dynamics in ArabidopsisČlánek Systematic Dissection of the Sequence Determinants of Gene 3’ End Mediated Expression ControlČlánek The Chromatin Remodeler CHD8 Is Required for Activation of Progesterone Receptor-Dependent EnhancersČlánek Selection against Heteroplasmy Explains the Evolution of Uniparental Inheritance of MitochondriaČlánek The DNA Helicase Recql4 Is Required for Normal Osteoblast Expansion and Osteosarcoma FormationČlánek Dual-Specificity Anti-sigma Factor Reinforces Control of Cell-Type Specific Gene Expression in
Článek vyšel v časopisePLOS Genetics
Nejčtenější tento týden
2015 Číslo 4- Akutní intermitentní porfyrie
- Farmakogenetické testování pomáhá předcházet nežádoucím efektům léčiv
- Růst a vývoj dětí narozených pomocí IVF
- Pilotní studie: stres a úzkost v průběhu IVF cyklu
- Vliv melatoninu a cirkadiálního rytmu na ženskou reprodukci
-
Všechny články tohoto čísla
- Retraction: Astakine 2—the Dark Knight Linking Melatonin to Circadian Regulation in Crustaceans
- Adventures in Wonderland
- Experimental Swap of 's Assortative Mating Preferences Demonstrates Key Role of X-Chromosome Divergence Island in Incipient Sympatric Speciation
- Chromosome Replacement and Deletion Lead to Clonal Polymorphism of Berry Color in Grapevine
- The Protein Quality Control Machinery Regulates Its Misassembled Proteasome Subunits
- Genome-Wide Association Study Identifies as a Critical Gene for Susceptibility to Noise-Induced Hearing Loss
- Genomic Location of the Major Ribosomal Protein Gene Locus Determines Global Growth and Infectivity
- Viable Neuronopathic Gaucher Disease Model in Medaka () Displays Axonal Accumulation of Alpha-Synuclein
- Multi-locus Analysis of Genomic Time Series Data from Experimental Evolution
- The Genetic Legacy of the Expansion of Turkic-Speaking Nomads across Eurasia
- Lack of GDAP1 Induces Neuronal Calcium and Mitochondrial Defects in a Knockout Mouse Model of Charcot-Marie-Tooth Neuropathy
- The Pif1 Helicase, a Negative Regulator of Telomerase, Acts Preferentially at Long Telomeres
- Inhibiting K63 Polyubiquitination Abolishes No-Go Type Stalled Translation Surveillance in
- SYD-1C, UNC-40 (DCC) and SAX-3 (Robo) Function Interdependently to Promote Axon Guidance by Regulating the MIG-2 GTPase
- Spatial Fluctuations in Expression of the Heterocyst Differentiation Regulatory Gene in Filaments
- Synergistic and Independent Actions of Multiple Terminal Nucleotidyl Transferases in the 3’ Tailing of Small RNAs in Arabidopsis
- Host Genetic Variation Influences Gene Expression Response to Rhinovirus Infection
- Contribution of Large Region Joint Associations to Complex Traits Genetics
- Volatility of Mutator Phenotypes at Single Cell Resolution
- Proteolysis of Virulence Regulator ToxR Is Associated with Entry of into a Dormant State
- Genome-Wide Negative Feedback Drives Transgenerational DNA Methylation Dynamics in Arabidopsis
- A Multi-layered Protein Network Stabilizes the FtsZ-ring and Modulates Constriction Dynamics
- Systematic Dissection of the Sequence Determinants of Gene 3’ End Mediated Expression Control
- Genome Sequencing of the Perciform Fish Provides Insights into Molecular and Genetic Mechanisms of Stress Adaptation
- Natural Variant E610G Is a Semi-dominant Suppressor of IAP-Induced RNA Processing Defects
- The Alkaline Response Pathway: Identification of a Novel Rim Pathway Activator
- Transgenerational Inheritance of Diet-Induced Genome Rearrangements in Drosophila
- A Single Nucleotide Polymorphism Uncovers a Novel Function for the Transcription Factor Ace2 during Hyphal Development
- DNA Damage Response and Spindle Assembly Checkpoint Function throughout the Cell Cycle to Ensure Genomic Integrity
- The Functional Interplay Between the t(9;22)-Associated Fusion Proteins BCR/ABL and ABL/BCR in Philadelphia Chromosome-Positive Acute Lymphatic Leukemia
- Extreme Recombination Frequencies Shape Genome Variation and Evolution in the Honeybee,
- Beyond Glycolysis: GAPDHs Are Multi-functional Enzymes Involved in Regulation of ROS, Autophagy, and Plant Immune Responses
- Comprehensive Profiling of Amino Acid Response Uncovers Unique Methionine-Deprived Response Dependent on Intact Creatine Biosynthesis
- Windpipe Controls Intestinal Homeostasis by Regulating JAK/STAT Pathway via Promoting Receptor Endocytosis and Lysosomal Degradation
- Ataxin-2 Regulates Translation in a New BAC-SCA2 Transgenic Mouse Model
- Cross-Population Joint Analysis of eQTLs: Fine Mapping and Functional Annotation
- The Power of Gene-Based Rare Variant Methods to Detect Disease-Associated Variation and Test Hypotheses About Complex Disease
- The Chromatin Remodeler CHD8 Is Required for Activation of Progesterone Receptor-Dependent Enhancers
- Competition between VanU Repressor and VanR Activator Leads to Rheostatic Control of Vancomycin Resistance Operon Expression
- A Missense Change in the Gene Links Aberrant Autophagy to a Neurodegenerative Vacuolar Storage Disease
- Simultaneous Discovery, Estimation and Prediction Analysis of Complex Traits Using a Bayesian Mixture Model
- Selection against Heteroplasmy Explains the Evolution of Uniparental Inheritance of Mitochondria
- Genome-Destabilizing Effects Associated with Top1 Loss or Accumulation of Top1 Cleavage Complexes in Yeast
- Imputation-Based Population Genetics Analysis of Malaria Parasites
- Heterozygosity for a Hypomorphic Polβ Mutation Reduces the Expansion Frequency in a Mouse Model of the Fragile X-Related Disorders
- Neto-Mediated Intracellular Interactions Shape Postsynaptic Composition at the Neuromuscular Junction
- Ndd1 Turnover by SCF Is Inhibited by the DNA Damage Checkpoint in
- Frameshift Variant Associated with Novel Hoof Specific Phenotype in Connemara Ponies
- The DNA Helicase Recql4 Is Required for Normal Osteoblast Expansion and Osteosarcoma Formation
- Spastin Binds to Lipid Droplets and Affects Lipid Metabolism
- Maintenance of Glia in the Optic Lamina Is Mediated by EGFR Signaling by Photoreceptors in Adult Drosophila
- Auxin Influx Carriers Control Vascular Patterning and Xylem Differentiation in
- Dual-Specificity Anti-sigma Factor Reinforces Control of Cell-Type Specific Gene Expression in
- The Lowe Syndrome Protein OCRL1 Is Required for Endocytosis in the Zebrafish Pronephric Tubule
- Postnatal Loss of Hap1 Reduces Hippocampal Neurogenesis and Causes Adult Depressive-Like Behavior in Mice
- CAPER Is Vital for Energy and Redox Homeostasis by Integrating Glucose-Induced Mitochondrial Functions via ERR-α-Gabpa and Stress-Induced Adaptive Responses via NF-κB-cMYC
- Distinct and Cooperative Activities of HESO1 and URT1 Nucleotidyl Transferases in MicroRNA Turnover in
- The Evolutionary Origination and Diversification of a Dimorphic Gene Regulatory Network through Parallel Innovations in and
- MAPK Signaling Pathway Alters Expression of Midgut ALP and ABCC Genes and Causes Resistance to Cry1Ac Toxin in Diamondback Moth
- Spatio-temporal Remodeling of Functional Membrane Microdomains Organizes the Signaling Networks of a Bacterium
- Asymmetric Transcript Discovery by RNA-seq in . Blastomeres Identifies , a Gene Important for Anterior Morphogenesis
- A Stress-Induced Small RNA Modulates Alpha-Rhizobial Cell Cycle Progression
- Systematic Profiling of Poly(A)+ Transcripts Modulated by Core 3’ End Processing and Splicing Factors Reveals Regulatory Rules of Alternative Cleavage and Polyadenylation
- The UPR Branch IRE1- in Plants Plays an Essential Role in Viral Infection and Is Complementary to the Only UPR Pathway in Yeast
- A Non-canonical RNA Silencing Pathway Promotes mRNA Degradation in Basal Fungi
- Co-chaperone p23 Regulates . Lifespan in Response to Temperature
- Re-replication of a Centromere Induces Chromosomal Instability and Aneuploidy
- Shade Avoidance Components and Pathways in Adult Plants Revealed by Phenotypic Profiling
- Lipid-Induced Epigenomic Changes in Human Macrophages Identify a Coronary Artery Disease-Associated Variant that Regulates Expression through Altered C/EBP-Beta Binding
- PLOS Genetics
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Lack of GDAP1 Induces Neuronal Calcium and Mitochondrial Defects in a Knockout Mouse Model of Charcot-Marie-Tooth Neuropathy
- Proteolysis of Virulence Regulator ToxR Is Associated with Entry of into a Dormant State
- Frameshift Variant Associated with Novel Hoof Specific Phenotype in Connemara Ponies
- Ataxin-2 Regulates Translation in a New BAC-SCA2 Transgenic Mouse Model
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



