-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaTo Be or Not IIb: A Multi-Step Process for Epstein-Barr Virus Latency Establishment and Consequences for B Cell Tumorigenesis
article has not abstract
Published in the journal: . PLoS Pathog 11(3): e32767. doi:10.1371/journal.ppat.1004656
Category: Pearls
doi: https://doi.org/10.1371/journal.ppat.1004656Summary
article has not abstract
Epstein-Barr virus (EBV), a γ-herpesvirus, was the first human tumor virus discovered fifty years ago in endemic Burkitt lymphoma [1]. Surprisingly, EBV was subsequently recognized to be a ubiquitous virus infecting greater than 90% of adults worldwide. In healthy children, primary EBV infection is typically asymptomatic because of a robust T cell immune response. However, infection during adolescence or later can result in infectious mononucleosis. Regardless of the severity of primary infection, EBV establishes a lifelong latent infection in the peripheral blood memory B cell compartment [2]. Immune suppression, genetic predisposition, or environmental factors can all serve to promote EBV-driven tumors, which are primarily of B cell, but also of epithelial and NK or T cell origin.
Early studies demonstrated that EBV infection in vitro transformed resting B cells into immortalized lymphoblastoid cell lines (LCL), providing a strong link to EBV-associated B cell cancers [3,4]. These pioneering studies stimulated intense investigation over the ensuing decades into the viral requirements and temporal cascade of gene expression triggering physiological cell changes associated with B cell proliferation and survival. The model that emerged indicates that B cell transformation in vitro is a latent infection including expression of a discrete set of nine proteins and many noncoding RNAs collectively called Latency III [2]. In this model, all of the Latency III gene products are expressed prior to the first cell division in the absence of lytic virus replication. However, this in vitro model does not account for the viral gene expression programs found in most EBV-positive B cell tumors or in the B cell compartment in vivo following natural infection. Moreover, a recent resurgence in studies of the earliest events following B cell infection combined with an appreciation of the heterogeneity of EBV latent gene expression during natural infection and in tumors provides the rationale for revisiting how this ubiquitous virus establishes latency and causes B cell malignancies.
Early B cell infection: Prelatency, the Epstein-Barr Nuclear Antigen (EBNA) transcriptional unit, and induction of proliferation
The initial events following EBV entry into B cells include deposition of the viral DNA into the nucleus and circularization of the linear genome followed by chromatinization and initial viral latent gene expression [2]. Recent work has refined these earlier studies to define a period after infection, but before cell division, of promiscuous viral gene expression where many lytic cycle mRNAs are produced in the absence of lytic DNA replication [5–8]. This transient burst of lytic gene expression is concomitant with transcription from the initial EBV latency promoter, the W promoter (Wp), to produce the first so-called latency associated proteins [9]. Together, this period of gene expression before cell division and up to the very first cell division is called the prelatent phase (Fig. 1). As the lytic mRNAs wane, the viral Epstein-Barr Nuclear Antigen 2 (EBNA2) and EBNA-LP proteins accumulate and directly activate the major upstream EBV latency C promoter (Cp) at ~48–72 hours postinfection [10]. Prior to the first cell division, at approximately 84 hours postinfection, the viral EBNA3A, 3B, 3C, and EBNA1 proteins are all expressed [10,11]. EBNA3s antagonize tumor suppressors while EBNA1 facilitates EBV genome replication and persistence. Concomitant with EBNA expression, viral BART and BHRF1 miRNAs are expressed as well as the pol III-driven short noncoding EBER RNAs [2]. Recently, it has become appreciated that the viral BCL-2 homolog, BHRF1, is expressed and peaks upon initial infection and is then continuously expressed at low levels from Wp through long-term outgrowth [12].
Fig. 1. EBV latency gene expression in different latency states. 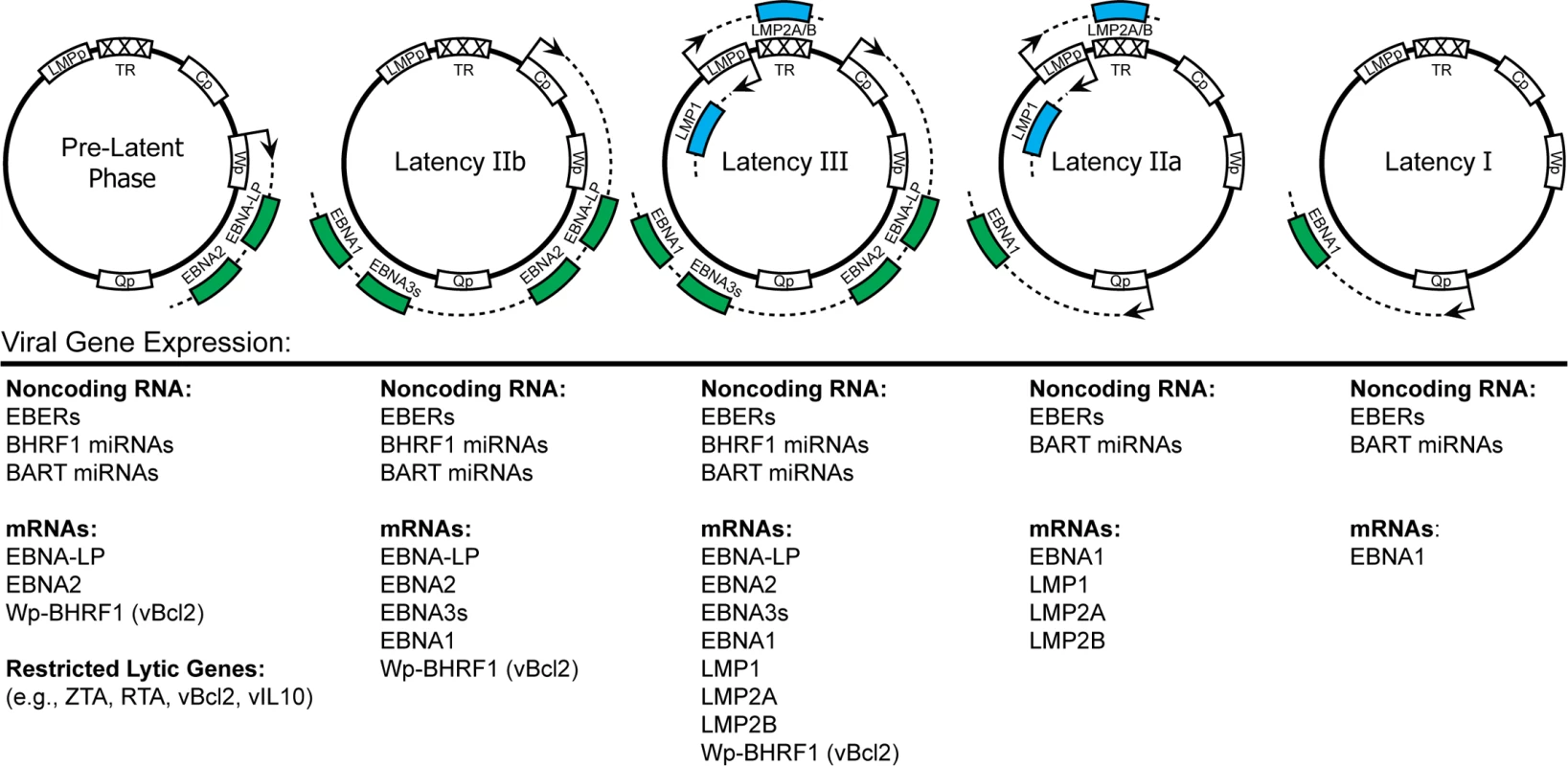
This figure depicts, from left to right, the theoretical progression of EBV latency gene expression from initial infection to true latency. The EBV genome is shown in episomal form closed at the terminal repeats (TR). Promoters are shown as white boxes and include the EBNA promoters Cp, Wp, and Qp as well as the bidirectional LMPp. Primary mRNA transcripts are shown as dotted lines, while coding regions have been simplified as colored boxes. An expanded list of viral genes expressed in each latency state is listed directly underneath the representative schematic. The first four cell divisions following infection are fast, on the order of 8–12 hours per cycle [11]. This rapid cycling mimics the behavior of centroblasts of the germinal center (GC). As a consequence of this rapid proliferation, EBV-infected blasts are susceptible to growth arrest due to a hyperproliferation-associated DNA damage response [11,13]. Infected cells that attenuate their proliferation rate will become immortalized in vitro. Interestingly, these early-infected cells express all of the EBNA proteins, but only minimally express the latent membrane proteins, or LMPs, 1, 2A, and 2B [14]. This cell state has been referred to as Latency IIb and may represent a clinically relevant feature of EBV-associated lymphomas as will be addressed below.
Transition to Latency III: Expression of the viral EBNAs and LMPs in LCLs in vitro and lymphomas in the setting of immune suppression
The full Latency III viral gene expression program, also known as the growth program, is characterized by the expression of all of the EBNAs as well as the LMPs (Fig. 1). The least restrictive of all the latency states, Latency III is observed in LCLs generated in vitro and in lymphomas in the setting of immune suppression, such as post-transplant or HIV/AIDS [2]. Latency III cells are characterized by high activity of the host NFκB pathway, which is primarily imparted by the viral LMP1 protein, a constitutively active mimic of the host CD40 costimulatory molecule [15]. LCLs and Latency III-expressing EBV lymphomas depend on high levels of NFκB activity for their survival [16,17]. Given that LMP1-induced NFκB activity is low during the first two weeks after infection [8,14], how these early-infected cells survive is an important unresolved question in the field of EBV biology.
Despite the canonical role for LMP1 in promoting survival, high level expression of LMP1 and NFκB activity might be deleterious to infected lymphoblasts in vivo. In Burkitt lymphoma, it was discovered that high levels of c-Myc transcriptional activity and a lack of NFκB imposed a nonimmunogenic phenotype due to low levels of major histocompatibility complex (MHC) class I expression and antigen presentation [18]. Furthermore, high levels of MHC class I-restricted immunogenicity was restored when c-Myc was attenuated and the cellular growth phenotype was converted to Latency III (i.e., high NFκB) [18]. Consistent with this dichotomy, Latency III gene expression in EBV-infected cells in vivo is mostly observed in settings of T cell immune suppression such as following organ transplant or HIV/AIDS [2,17].
Restricted EBV Latency IIa in germinal centers and Hodgkin lymphoma
While the progression of EBV latent infection in vitro culminates with a Latency III-expressing LCL, in vivo the establishment of latency is likely to proceed through a more complex route. It is known that EBV-infected cells express Latency III proteins at some point during natural infection, because EBV-specific cytotoxic T lymphocytes (CTLs) recognize immunodominant epitopes found in the EBNA3s [19]. Indeed, it is likely selective pressure from EBV-specific CTLs, in part, that promotes the transition from Latency III to more restricted forms of latency. Latency IIa has been detected in GC cells of healthy individuals as well as in EBV-positive Hodgkin lymphoma [20]. This form of latency is characterized by the lack of EBNA expression from Cp or Wp, retained expression of LMP1 and LMP2A, the expression of EBNA1 from a unique promoter (Qp), and the expression of EBER RNAs and BART miRNAs (Fig. 1). Precisely how the transition to this restricted latency state occurs is not well understood. However, recent work implicates T cell secreted cytokines, including IL-21, in down-regulation of Cp and EBNA expression [21].
Latency IIa-expressing cells are also thought to be precursors of EBV-associated Hodgkin lymphomas. These tumors often contain crippled immunoglobulin genes, which are likely to have been rescued through the mimicry of CD40 and B cell Receptor (BCR) signaling by LMP1 and LMP2A, respectively [22]. During natural infection, the LMP-mediated survival of GC B cells may promote entry into the mature memory pool in the periphery. However, whether antigen-driven BCR signaling is required for this process remains to be determined.
True latency: Latency 0/I in resting memory B cells and Burkitt lymphoma
In vivo, the major pool of EBV latently-infected B cells are resting, peripheral blood class-switched memory cells [23]. No viral proteins are expressed in these cells (Latency 0) except during cell division, when EBNA1 is expressed from Qp (Latency I) (Fig. 1). Interestingly, EBV ncRNAs including EBERs and BART miRNAs are expressed in these cells [2]. Therefore, these cells are poorly recognized by the T cell immune response. It is unclear what regulates viral gene expression in these truly latent cells; perhaps the lack of proliferation-associated transcription factors prevents activation of the EBNA and LMP promoters. The post-GC ontogeny, poor immunogenicity, and restricted latent gene expression of these cells are also reflected in EBV-associated Burkitt lymphomas.
The prevalence and newly appreciated importance of Latency IIb (EBNA+/LMP-) during latency establishment and in tumors
Latency IIb is a form of latency that was first observed following primary infection of B cells derived from patients with chronic lymphocytic leukemia [24]. It was named Latency IIb by Eva Klein because the EBNA2+/LMP1 - gene expression phenotype is directly opposite of the EBNA2-/LMP1+ phenotype observed in Latency IIa [25]. Recent work has demonstrated that this latent gene expression state is also observed after EBV infects peripheral blood B cells and lasts for approximately two weeks before transitioning to the full Latency III state found in LCLs [14].
A subset of EBV-associated malignancies including HIV-associated lymphomas and post-transplant lymphomas display heterogeneous expression of Latency IIb in addition to Latency III [17,25–27]. These findings are based on single cell analysis of tumor sections using immunohistochemistry and contrast the dogma based upon bulk expression analysis that characterized these malignancies as Latency III [2]. These single cell data, coupled with the aforementioned finding of Latency IIb during early primary B cell infection suggests that this form of latency may contribute to EBV pathogenesis [14,25]. Indeed, heterogeneous expression of Latency IIb with other latency types was also observed in tonsils of acute infectious mononucleosis (IM) patients [28]. A summary of latency types observed in EBV-infected B cells in vitro and in vivo is presented as Fig. 2.
Fig. 2. EBV latency types found in EBV-driven malignancies. 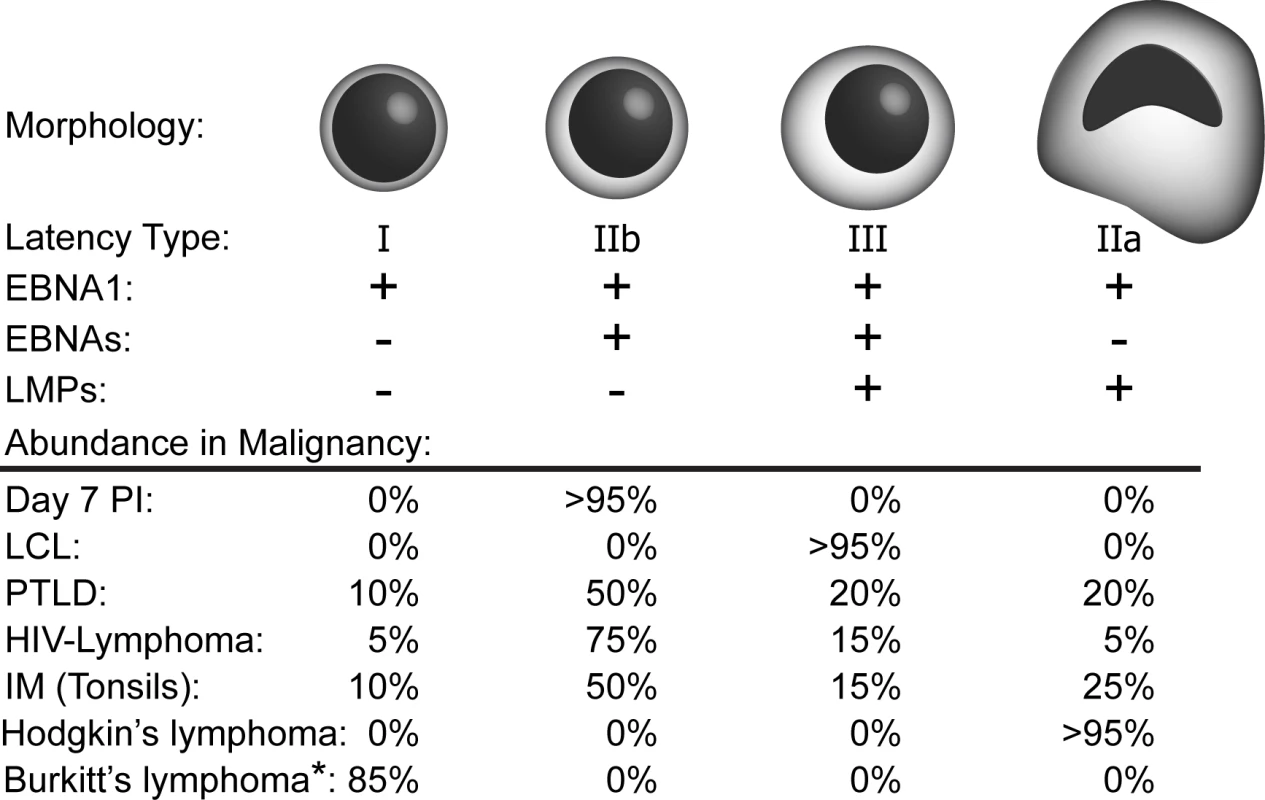
Cell morphology (including cellular size and classic Reed–Sternberg-like nuclear morphology in the case of Latency IIa cells) that is associated with various EBV latency types is depicted. In heterogeneous malignancies, the relative percentage of cells displaying each latency type as shown by tumor cross-sections and immunohistochemistry are shown below (Relevant citations: Day 7 post infection [14], Post-Transplant Lymphoproliferative Disease (PTLD) [26,27], HIV-Lymphoma [26], IM [28], all others [2]). *Of note, approximately 15% of Burkitt lymphomas carry a mutant EBV genome containing a deleted EBNA2 gene, resulting in expression of the EBNA3s and Wp-BHRF1 (vBcl2), as well as EBNA1. The prevalence of cells expressing Latency IIb within tumors is hypothesized to be due to the highly immunogenic state conferred by LMP1 within Latency III. Indeed, in humanized mouse model systems of EBV infection with functional adaptive responses, the ability of T cells to specifically kill EBV-infected B cells selects for Latency IIb-expressing tumors [29]. In recent cell line studies, Latency III-expressing LCLs were found to cycle through a wide range of expression of LMP1, which correlated with MHC I surface levels such that only cells expressing the highest amount of LMP1, and consequently MHC I, were efficiently killed by CTLs [30]. These data beg the important question of whether the LMP1–MHC I connection is also observed in vivo; will tumor cells displaying a Latency III expression pattern be killed by CTLs while those displaying a Latency IIb program be spared? A related question is whether CD4+ T cells or NK cells might play a more important role in controlling Latency IIb expressing cells in vivo. The answers to these questions will be critical for defining the mechanisms of EBV latency establishment and B cell tumorigenesis in the immunodeficient and the immunocompetent host.
Zdroje
1. Epstein M, Achong B, Barr Y (1964) Virus particles in cultured lymphoblasts from Burkitt's lymphoma. Lancet 28 : 702–703.
2. Longnecker RM, Kieff E, Cohen JI (2013) Epstein-Barr virus In: Knipe DM, Howley PM, editors. Fields Virology. 6th ed. Philadelphia: Lippincott, Williams, and Wilkins. pp. 1898–1959.
3. Henle W, Diehl V, Kohn G, Zur Hausen H, Henle G (1967) Herpes-type virus and chromosome marker in normal leukocytes after growth with irradiated Burkitt cells. Science 157 : 1064–1065. 6036237
4. Pope JH, M., and Scott W. (1968) Transformation of huiman foetal leukocytes in vitro by filtrates of a human leukaemic line containing Herpes-like virus. International Journal of Cancer 3 : 857–866. 4894385
5. Halder S, Murakami M, Verma SC, Kumar P, Yi F, et al. (2009) Early events associated with infection of Epstein-Barr virus infection of primary B-cells. PLoS One 4: e7214. doi: 10.1371/journal.pone.0007214 19784370
6. Wen W, Iwakiri D, Yamamoto K, Maruo S, Kanda T, et al. (2007) Epstein-Barr virus BZLF1 gene, a switch from latency to lytic infection, is expressed as an immediate-early gene after primary infection of B lymphocytes. Journal of Virology 81 : 1037–1042. 17079287
7. Altmann M, Hammerschmidt W (2005) Epstein-Barr virus provides a new paradigm: a requirement for the immediate inhibition of apoptosis. PLoS Biol 3: e404. 16277553
8. Price AM, Luftig MA (2014) Dynamic Epstein-Barr virus gene expression on the path to B-cell transformation. Adv Virus Res 88 : 279–313. doi: 10.1016/B978-0-12-800098-4.00006-4 24373315
9. Woisetschlaeger M, Strominger JL, Speck SH (1989) Mutually exclusive use of viral promoters in Epstein-Barr virus latently infected lymphocytes. Proc Natl Acad Sci U S A 86 : 6498–6502. 2549539
10. Alfieri C, Birkenbach M, Kieff E (1991) Early events in Epstein-Barr virus infection of human B lymphocytes. Virology 181 : 595–608. 1849678
11. Nikitin PA, Yan CM, Forte E, Bocedi A, Tourigny JP, et al. (2010) An ATM/Chk2-mediated DNA damage-responsive signaling pathway suppresses Epstein-Barr virus transformation of primary human B cells. Cell Host Microbe 8 : 510–522. doi: 10.1016/j.chom.2010.11.004 21147465
12. Kelly GL, Long HM, Stylianou J, Thomas WA, Leese A, et al. (2009) An Epstein-Barr virus anti-apoptotic protein constitutively expressed in transformed cells and implicated in burkitt lymphomagenesis: the Wp/BHRF1 link. PLoS Pathog 5: e1000341. doi: 10.1371/journal.ppat.1000341 19283066
13. Nikitin PA, Price AM, McFadden K, Yan CM, Luftig MA (2014) Mitogen-induced B-cell proliferation activates Chk2-dependent G1/S cell cycle arrest. PLoS One 9: e87299. doi: 10.1371/journal.pone.0087299 24498068
14. Price AM, Tourigny JP, Forte E, Salinas RE, Dave SS, et al. (2012) Analysis of Epstein-Barr Virus-Regulated Host Gene Expression Changes through Primary B-Cell Outgrowth Reveals Delayed Kinetics of Latent Membrane Protein 1-Mediated NF-kappaB Activation. J Virol 86 : 11096–11106. 22855490
15. Mosialos G, Birkenbach M, Yalamanchili R, VanArsdale T, Ware C, et al. (1995) The Epstein-Barr virus transforming protein LMP1 engages signaling proteins for the tumor necrosis factor receptor family. Cell 80 : 389–399. 7859281
16. Cahir-McFarland ED, Davidson DM, Schauer SL, Duong J, Kieff E (2000) NF-kappa B inhibition causes spontaneous apoptosis in Epstein-Barr virus-transformed lymphoblastoid cells. Proc Natl Acad Sci U S A 97 : 6055–6060. 10811897
17. Cesarman E (2014) Gammaherpesviruses and lymphoproliferative disorders. Annu Rev Pathol 9 : 349–372. doi: 10.1146/annurev-pathol-012513-104656 24111911
18. Staege MS, Lee SP, Frisan T, Mautner J, Scholz S, et al. (2002) MYC overexpression imposes a nonimmunogenic phenotype on Epstein-Barr virus-infected B cells. Proc Natl Acad Sci U S A 99 : 4550–4555. 11917131
19. Hislop AD, Taylor GS, Sauce D, Rickinson AB (2007) Cellular responses to viral infection in humans: lessons from Epstein-Barr virus. Annu Rev Immunol 25 : 587–617. 17378764
20. Thorley-Lawson DA, Gross A (2004) Persistence of the Epstein-Barr virus and the origins of associated lymphomas. N Engl J Med 350 : 1328–1337. 15044644
21. Kis LL, Salamon D, Persson EK, Nagy N, Scheeren FA, et al. (2010) IL-21 imposes a type II EBV gene expression on type III and type I B cells by the repression of C - and activation of LMP-1-promoter. Proc Natl Acad Sci U S A 107 : 872–877. doi: 10.1073/pnas.0912920107 20080768
22. Kanzler H, Kuppers R, Hansmann ML, Rajewsky K (1996) Hodgkin and Reed-Sternberg cells in Hodgkin's disease represent the outgrowth of a dominant tumor clone derived from (crippled) germinal center B cells. J Exp Med 184 : 1495–1505. 8879220
23. Babcock GJ, Decker LL, Volk M, Thorley-Lawson DA (1998) EBV persistence in memory B cells in vivo. Immunity 9 : 395–404. 9768759
24. Doyle MG, Catovsky D, Crawford DH (1993) Infection of leukaemic B lymphocytes by Epstein Barr virus. Leukemia 7 : 1858–1864. 8231253
25. Klein E, Nagy N, Rasul AE (2013) EBV genome carrying B lymphocytes that express the nuclear protein EBNA-2 but not LMP-1: Type IIb latency. Oncoimmunology 2: e23035. 23526738
26. Brink AA, Dukers DF, van den Brule AJ, Oudejans JJ, Middeldorp JM, et al. (1997) Presence of Epstein-Barr virus latency type III at the single cell level in post-transplantation lymphoproliferative disorders and AIDS related lymphomas. J Clin Pathol 50 : 911–918. 9462239
27. Oudejans JJ, Jiwa M, van den Brule AJ, Grasser FA, Horstman A, et al. (1995) Detection of heterogeneous Epstein-Barr virus gene expression patterns within individual post-transplantation lymphoproliferative disorders. Am J Pathol 147 : 923–933. 7573368
28. Niedobitek G, Hamilton-Dutoit S, Herbst H, Finn T, Vetner M, et al. (1989) Identification of Epstein-Barr virus-infected cells in tonsils of acute infectious mononucleosis by in situ hybridization. Hum Pathol 20 : 796–799. 2545594
29. Ma SD, Hegde S, Young KH, Sullivan R, Rajesh D, et al. (2011) A new model of Epstein-Barr virus infection reveals an important role for early lytic viral protein expression in the development of lymphomas. J Virol 85 : 165–177. doi: 10.1128/JVI.01512-10 20980506
30. Brooks JM, Lee SP, Leese AM, Thomas WA, Rowe M, et al. (2009) Cyclical expression of EBV latent membrane protein 1 in EBV-transformed B cells underpins heterogeneity of epitope presentation and CD8+ T cell recognition. J Immunol 182 : 1919–1928. doi: 10.4049/jimmunol.0713607 19201845
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek A Phospholipase Is Involved in Disruption of the Liver Stage Parasitophorous Vacuole MembraneČlánek Host ESCRT Proteins Are Required for Bromovirus RNA Replication Compartment Assembly and FunctionČlánek Enhanced CD8 T Cell Responses through GITR-Mediated Costimulation Resolve Chronic Viral Infection
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2015 Číslo 3- Stillova choroba: vzácné a závažné systémové onemocnění
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
- Diagnostika virových hepatitid v kostce – zorientujte se (nejen) v sérologii
- Jak souvisí postcovidový syndrom s poškozením mozku?
- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
-
Všechny články tohoto čísla
- To Be or Not IIb: A Multi-Step Process for Epstein-Barr Virus Latency Establishment and Consequences for B Cell Tumorigenesis
- Is Antigenic Sin Always “Original?” Re-examining the Evidence Regarding Circulation of a Human H1 Influenza Virus Immediately Prior to the 1918 Spanish Flu
- The Great Escape: Pathogen Versus Host
- Coping with Stress and the Emergence of Multidrug Resistance in Fungi
- Catch Me If You Can: The Link between Autophagy and Viruses
- Bacterial Immune Evasion through Manipulation of Host Inhibitory Immune Signaling
- Evidence for Ubiquitin-Regulated Nuclear and Subnuclear Trafficking among Matrix Proteins
- BILBO1 Is a Scaffold Protein of the Flagellar Pocket Collar in the Pathogen
- Production of Anti-LPS IgM by B1a B Cells Depends on IL-1β and Is Protective against Lung Infection with LVS
- Virulence Regulation with Venus Flytrap Domains: Structure and Function of the Periplasmic Moiety of the Sensor-Kinase BvgS
- α-Hemolysin Counteracts the Anti-Virulence Innate Immune Response Triggered by the Rho GTPase Activating Toxin CNF1 during Bacteremia
- Induction of Interferon-Stimulated Genes by IRF3 Promotes Replication of
- Intracellular Growth Is Dependent on Tyrosine Catabolism in the Dimorphic Fungal Pathogen
- HCV Induces the Expression of Rubicon and UVRAG to Temporally Regulate the Maturation of Autophagosomes and Viral Replication
- Spatiotemporal Analysis of Hepatitis C Virus Infection
- Subgingival Microbial Communities in Leukocyte Adhesion Deficiency and Their Relationship with Local Immunopathology
- Interaction between the Type III Effector VopO and GEF-H1 Activates the RhoA-ROCK Pathway
- Attenuation of Tick-Borne Encephalitis Virus Using Large-Scale Random Codon Re-encoding
- Establishment of HSV1 Latency in Immunodeficient Mice Facilitates Efficient Reactivation
- XRN1 Stalling in the 5’ UTR of Hepatitis C Virus and Bovine Viral Diarrhea Virus Is Associated with Dysregulated Host mRNA Stability
- γδ T Cells Confer Protection against Murine Cytomegalovirus (MCMV)
- Rhadinovirus Host Entry by Co-operative Infection
- A Phospholipase Is Involved in Disruption of the Liver Stage Parasitophorous Vacuole Membrane
- Dermal Neutrophil, Macrophage and Dendritic Cell Responses to Transmitted by Fleas
- Elucidation of Sigma Factor-Associated Networks in Reveals a Modular Architecture with Limited and Function-Specific Crosstalk
- A Conserved NS3 Surface Patch Orchestrates NS2 Protease Stimulation, NS5A Hyperphosphorylation and HCV Genome Replication
- Host ESCRT Proteins Are Required for Bromovirus RNA Replication Compartment Assembly and Function
- Disruption of IL-21 Signaling Affects T Cell-B Cell Interactions and Abrogates Protective Humoral Immunity to Malaria
- Compartmentalized Replication of R5 T Cell-Tropic HIV-1 in the Central Nervous System Early in the Course of Infection
- Diminished Reovirus Capsid Stability Alters Disease Pathogenesis and Littermate Transmission
- Characterization of CD8 T Cell Differentiation following SIVΔnef Vaccination by Transcription Factor Expression Profiling
- Visualization of HIV-1 Interactions with Penile and Foreskin Epithelia: Clues for Female-to-Male HIV Transmission
- Sensing Cytosolic RpsL by Macrophages Induces Lysosomal Cell Death and Termination of Bacterial Infection
- PKCη/Rdx-driven Phosphorylation of PDK1: A Novel Mechanism Promoting Cancer Cell Survival and Permissiveness for Parvovirus-induced Lysis
- Metalloprotease NleC Suppresses Host NF-κB/Inflammatory Responses by Cleaving p65 and Interfering with the p65/RPS3 Interaction
- Immune Antibodies and Helminth Products Drive CXCR2-Dependent Macrophage-Myofibroblast Crosstalk to Promote Intestinal Repair
- Adenovirus Entry From the Apical Surface of Polarized Epithelia Is Facilitated by the Host Innate Immune Response
- The RNA Template Channel of the RNA-Dependent RNA Polymerase as a Target for Development of Antiviral Therapy of Multiple Genera within a Virus Family
- Neutrophils: Between Host Defence, Immune Modulation, and Tissue Injury
- CD169-Mediated Trafficking of HIV to Plasma Membrane Invaginations in Dendritic Cells Attenuates Efficacy of Anti-gp120 Broadly Neutralizing Antibodies
- Japanese Encephalitis Virus Nonstructural Protein NS5 Interacts with Mitochondrial Trifunctional Protein and Impairs Fatty Acid β-Oxidation
- Yip1A, a Novel Host Factor for the Activation of the IRE1 Pathway of the Unfolded Protein Response during Infection
- TRIM26 Negatively Regulates Interferon-β Production and Antiviral Response through Polyubiquitination and Degradation of Nuclear IRF3
- Parallel Epigenomic and Transcriptomic Responses to Viral Infection in Honey Bees ()
- A Crystal Structure of the Dengue Virus NS5 Protein Reveals a Novel Inter-domain Interface Essential for Protein Flexibility and Virus Replication
- Enhanced CD8 T Cell Responses through GITR-Mediated Costimulation Resolve Chronic Viral Infection
- Exome and Transcriptome Sequencing of Identifies a Locus That Confers Resistance to and Alters the Immune Response
- The Role of Misshapen NCK-related kinase (MINK), a Novel Ste20 Family Kinase, in the IRES-Mediated Protein Translation of Human Enterovirus 71
- Chitin Recognition via Chitotriosidase Promotes Pathologic Type-2 Helper T Cell Responses to Cryptococcal Infection
- Activates Both IL-1β and IL-1 Receptor Antagonist to Modulate Lung Inflammation during Pneumonic Plague
- Persistence of Transmitted HIV-1 Drug Resistance Mutations Associated with Fitness Costs and Viral Genetic Backgrounds
- An 18 kDa Scaffold Protein Is Critical for Biofilm Formation
- Early Virological and Immunological Events in Asymptomatic Epstein-Barr Virus Infection in African Children
- Human CD8 T-cells Recognizing Peptides from () Presented by HLA-E Have an Unorthodox Th2-like, Multifunctional, Inhibitory Phenotype and Represent a Novel Human T-cell Subset
- Decreased HIV-Specific T-Regulatory Responses Are Associated with Effective DC-Vaccine Induced Immunity
- RSV Vaccine-Enhanced Disease Is Orchestrated by the Combined Actions of Distinct CD4 T Cell Subsets
- Concerted Activity of IgG1 Antibodies and IL-4/IL-25-Dependent Effector Cells Trap Helminth Larvae in the Tissues following Vaccination with Defined Secreted Antigens, Providing Sterile Immunity to Challenge Infection
- Structure of the Low pH Conformation of Chandipura Virus G Reveals Important Features in the Evolution of the Vesiculovirus Glycoprotein
- PPM1A Regulates Antiviral Signaling by Antagonizing TBK1-Mediated STING Phosphorylation and Aggregation
- Lipidomic Analysis Links Mycobactin Synthase K to Iron Uptake and Virulence in .
- Roles and Programming of Arabidopsis ARGONAUTE Proteins during Infection
- Impact of Infection on Host Macrophage Nuclear Physiology and Nucleopore Complex Integrity
- The Impact of Host Diet on Titer in
- Antimicrobial-Induced DNA Damage and Genomic Instability in Microbial Pathogens
- Herpesviral G Protein-Coupled Receptors Activate NFAT to Induce Tumor Formation via Inhibiting the SERCA Calcium ATPase
- The Causes and Consequences of Changes in Virulence following Pathogen Host Shifts
- Small GTPase Rab21 Mediates Fibronectin Induced Actin Reorganization in : Implications in Pathogen Invasion
- Positive Role of Promyelocytic Leukemia Protein in Type I Interferon Response and Its Regulation by Human Cytomegalovirus
- NEDDylation Is Essential for Kaposi’s Sarcoma-Associated Herpesvirus Latency and Lytic Reactivation and Represents a Novel Anti-KSHV Target
- β-HPV 5 and 8 E6 Disrupt Homology Dependent Double Strand Break Repair by Attenuating BRCA1 and BRCA2 Expression and Foci Formation
- An O Antigen Capsule Modulates Bacterial Pathogenesis in
- Variable Processing and Cross-presentation of HIV by Dendritic Cells and Macrophages Shapes CTL Immunodominance and Immune Escape
- Probing the Metabolic Network in Bloodstream-Form Using Untargeted Metabolomics with Stable Isotope Labelled Glucose
- Adhesive Fiber Stratification in Uropathogenic Biofilms Unveils Oxygen-Mediated Control of Type 1 Pili
- Vaccinia Virus Protein Complex F12/E2 Interacts with Kinesin Light Chain Isoform 2 to Engage the Kinesin-1 Motor Complex
- Modulates Host Macrophage Mitochondrial Metabolism by Hijacking the SIRT1-AMPK Axis
- Human T-Cell Leukemia Virus Type 1 (HTLV-1) Tax Requires CADM1/TSLC1 for Inactivation of the NF-κB Inhibitor A20 and Constitutive NF-κB Signaling
- Suppression of RNAi by dsRNA-Degrading RNaseIII Enzymes of Viruses in Animals and Plants
- Spatiotemporal Regulation of a T4SS Substrate by the Metaeffector SidJ
- Antigenic Properties of the Human Immunodeficiency Virus Envelope Glycoprotein Gp120 on Virions Bound to Target Cells
- Dependence of Intracellular and Exosomal microRNAs on Viral Oncogene Expression in HPV-positive Tumor Cells
- Identification of a Peptide-Pheromone that Enhances Escape from Host Cell Vacuoles
- Impaired Systemic Tetrahydrobiopterin Bioavailability and Increased Dihydrobiopterin in Adult Falciparum Malaria: Association with Disease Severity, Impaired Microvascular Function and Increased Endothelial Activation
- Transgenic Expression of the Dicotyledonous Pattern Recognition Receptor EFR in Rice Leads to Ligand-Dependent Activation of Defense Responses
- Comprehensive Antigenic Map of a Cleaved Soluble HIV-1 Envelope Trimer
- Low Doses of Imatinib Induce Myelopoiesis and Enhance Host Anti-microbial Immunity
- Impaired Systemic Tetrahydrobiopterin Bioavailability and Increased Oxidized Biopterins in Pediatric Falciparum Malaria: Association with Disease Severity
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Bacterial Immune Evasion through Manipulation of Host Inhibitory Immune Signaling
- BILBO1 Is a Scaffold Protein of the Flagellar Pocket Collar in the Pathogen
- Antimicrobial-Induced DNA Damage and Genomic Instability in Microbial Pathogens
- Attenuation of Tick-Borne Encephalitis Virus Using Large-Scale Random Codon Re-encoding
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



