-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Solitary cerebellar metastasis of uterine cervical carcinoma
Solitární cerebelární metastáza uterinního cervikálního karcinomu
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manu script met the ICMJE “uniform requirements” for biomedical papers.
Authors: M. B. Onal 1; A. Kircelli 2; E. Civelek 3; O. Aydin 4
Authors place of work: Vocational School of Health Sciences, Acibadem University, Istanbul, Turkey 1; Department of Neurosurgery, Istanbul Research Hospital, Baskent University, Istanbul, Turkey 2; Department of Neurosurgery, Gaziosmanpasa Taksim Education and Research Hospital, University of Health Sciences, Istanbul, Turkey 3; Department of Pathology, Acıbadem University, Istanbul, Turkey 4
Published in the journal: Cesk Slov Neurol N 2018; 81(6): 714-715
Category: Dopisy redakci
doi: https://doi.org/10.14735/amcsnn2018714Summary
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manu script met the ICMJE “uniform requirements” for biomedical papers.
Dear Editor,
Uterine cervical cancer is one of the leading cancers in women as it is the second most common cancer worldwide. It causes approximately 275,000 female deaths yearly [1]. Nevertheless, CNS metastasis of uterine cervical carcinoma are uncommon [2,3]. Cervical cancer metastasis potential is very low (< 10%), and there is a tendency to enter retroperitoneal lymph nodes, lungs and bone [4]. Cerebral metastasis occurs as part of a disseminated disease with systemic involvement, which has an incidence of 0.5% to 1.2% [5]. The cerebellum is a very unusual site for metastasis. The most common histopathology is shown to be a squamous cell tumor [2].
A 65-year-old woman suffering from vaginal bleeding was referred to a gynecology clinic. Pelvic examination resulted in abdominal ultrasonography which revealed a 35 × 33 × 48 mm tumor of the cervix with parametrial invasion. Thorax and upper abdominal tomography were normal. Cervical biopsy was performed. Pathology showed a moderately differentiated invasive squamous cell carcinoma. The disease was staged 2b according to The International Federation of Gynecology and Obstetrics (FIGO) staging, so the patient underwent adjuvant radiation therapy and concurrent cisplatin containing chemotherapy. The patient was symptom free for 6 months. Then, she started to complain of nausea and dizziness. PET did not reveal any metastasis but the symptoms remained, so head tomography was performed, which revealed an occupying lesion in the left cerebellum with a mass effect on the fourth ventricle causing hydrocephalus and increasing intracranial pressure. The patient underwent a midline occipital craniotomy and total excision of the mass (Fig. 1), which histologically proved to be squamous cell carcinoma metastasis (Fig. 2). Intraoperatively, the tumor had a medium hardness. It was encapsulated with well-defined planes and soon after the capsule was opened, a grayish yellow mucoid fluid was seen.
Fig. 1. MRI of the brain demonstrates the lesion in the left cerebellar hemisphere with a heterogeneous postcontrast enhancement in axial (A) and sagittal (B) T1-weighted images. Postoperative T1-weighted postcontrast axial (C) and sagittal (D) images reveal the total excision of the tumor.
Obr. 1. Předoperační MR mozku zobrazuje lézi v levé cerebelární hemisféře s heterogenním postkontrastním enhancementem v axiálním (A) a sagitálním (B) T1 váženém obrazu. Pooperační T1 vážené postkontrastní axiální (C) a sagitální (D) obrazy zobrazují úplnou excizi nádoru.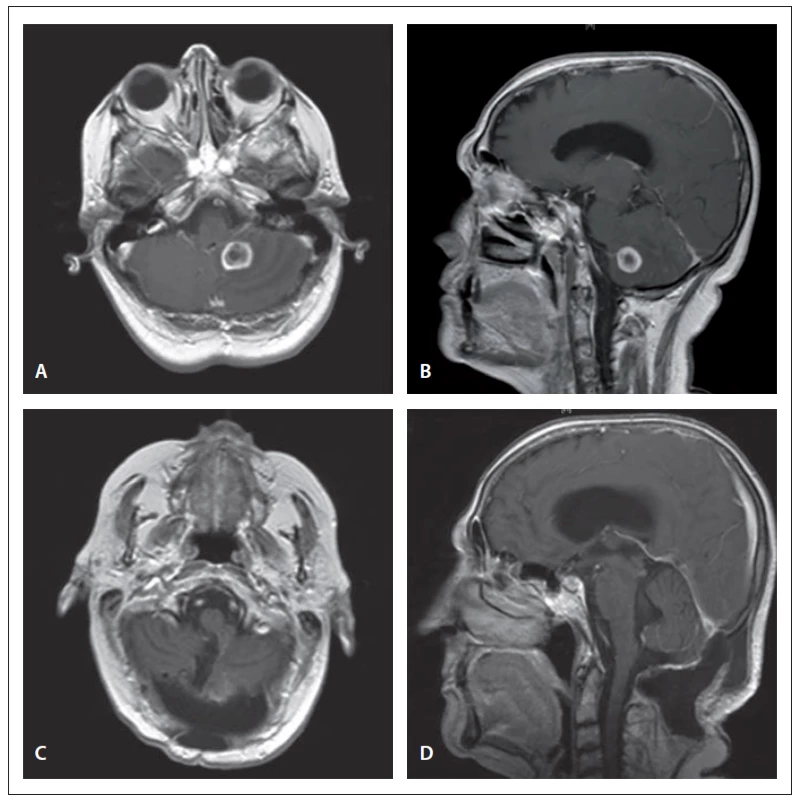
Fig. 2. Paraffin section showing a metastatic squamous cell carcinoma (hematoxylin and eosin).
Obr. 2. Parafinový řez ukazující metastatický karcinom skvamózních buněk (hematoxylin a eosin).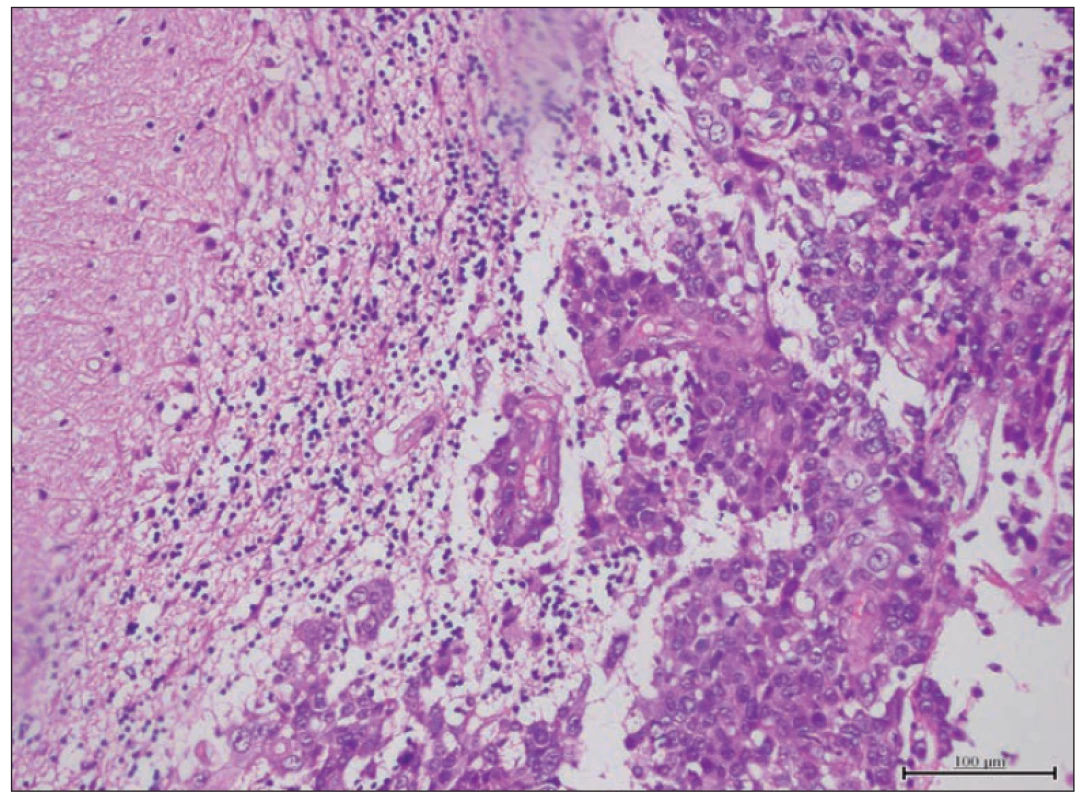
She received radiotherapy to the brain 1 month post-surgery. At the end of the 10th radiation therapy, she started vomiting and displayed cerebellar syndrome. Medical treatment showed no recovery. She was sleepy and unconscious. Brain MRI revealed total excision of the left cerebellar metastasis but also tetraventricular hydrocephalus with transependymal cerebrospinal fluid pass. After pressure measurement by lumbar puncture, she underwent surgery for ventriculoperitoneal shunting. She recovered after the procedure. Eight months after cerebellar resection, the patient was dead. Before her death, she had multiple metastases to the lungs and bones.
Henriksen first reported cerebral metastasis of cervical carcinoma in 1949 in an autopsy study [6]. Cervical carcinomas similar to other gynecologic malignancies have a lower tendency to metastasize to the brain, with a rate of 0.4– 1.2%. Generally, headache and hemiplegia are the most significant symptoms of brain metastasis; however, dizziness and nausea were the most common complaints of our patient. In the literature, the time from initial diagnosis to metastasis has been reported in a various range of 5 weeks to 8 years [7]. In our patient, metastasis was discovered 6 months after diagnosis. In the literature, brain involvement without systemic involvement of the cervical carcinoma is very rare [8].
The treatment of brain metastasis includes radiation or surgery combined with postoperative radiation therapy. Solitary metastasis and life-threatening masses are some of the surgical indications. The median survival is longer with surgery combined with radiotherapy, which is more effective than radiotherapy treatment alone. Palliative therapy is recommended in multiple intracranial lesions with systemic dissemination [8]. It is reported that surgical resection followed by whole brain radiotherapy is the best choice in solitary brain metastasis cases [5].
Similar case reports in the literature have shown that comorbidities such as lung metastasis, are generally determined at the time of diagnosis. In our opinion, surgical resection should be performed in solitary cerebellum metastasis of cervical cancer, in the absence of another organ metastasis. Otherwise, palliative management should be chosen. Although there are several treatment modalities are available, the prognosis of cerebral metastasis from cervical cancer is still very poor.
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Accepted for review: 15. 6. 2018
Accepted for print: 30. 10. 2018
Atilla Kırcelli, MD.
Department of Neurosurgery
Istanbul Research Hospital
Baskent University
Altunizade Mahallesi
7, Kısıklı Caddesi, Oymacı Sk.
34662 Üsküdar/İstanbul
Turkey
Zdroje
1. Oaknin A, de Corcuera ID, Rodríguez-Freixinós V et al. SEOM guidelines for cervical cancer. Clin Trans Oncol 2012; 14(7): 516– 519. doi: 10.1007/ s12094-012-0834-y.
2. Cormio G, Pellegrino A, Landoni F et al. Brain metastases from cervical carcinoma. Tumori 1996; 82(4): 394– 396.
3. Dadlani R, Ghosal N, Hegde AS. Solitary cerebellous metastasis after prolonged remission in a case of uterine cervical adenocarcinoma. J Neurosci Rural Pract 2012; 3(2): 185– 187. doi: 10.4103/ 0976-3147.98234.
4. Tajran D, Berek J. Surgical resection of solitary brain metastasis from cervical cancer. Int J Gynecol Cancer 2003; 13(3): 368– 370.
5. El Omari-Alaoui H, Gaye P, Kebdani T et al. Cerebellous metastases in patients with uterine cervical cancer. Two cases reports and review of the literature. Cancer Radiother 2003; 7(5): 317– 320.
6. Henriksen E. The lymphatic spread of carcinoma of the cervix and of the body of the uterus: a study of 420 necropsies. Am J Obstetrics Gynecol 1949; 58(5): 924– 942.
7. Peters P, Bandi H, Efendy J et al. Rapid growth of cervical cancer metastasis in the brain. J Clinical Neurosci 2010; 17(9): 1211– 1212. doi: 10.1016/ j.jocn.2010.01.021.
8. Ikeda SI, Yamada T, Katsumata N et al. Cerebral metastasis in patients with uterine cervical cancer. Jpn J Clin Oncol 1998; 28(1): 27– 29.
Štítky
Dětská neurologie Neurochirurgie Neurologie
Článek vyšel v časopiseČeská a slovenská neurologie a neurochirurgie
Nejčtenější tento týden
2018 Číslo 6- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Magnosolv a jeho využití v neurologii
- Zolpidem může mít širší spektrum účinků, než jsme se doposud domnívali, a mnohdy i překvapivé
- Nejčastější nežádoucí účinky venlafaxinu během terapie odeznívají
-
Všechny články tohoto čísla
- Diagnostics, symptomatology and findings in diseases and disorders of the autonomic nervous system in neurology
- Patients with extensive early changes (ASPECTS < 5) – recanalization YES
- Patients with extensive early changes (ASPECTS < 5) – recanalization NO
-
Pacient s rozsiahlymi skorými zmenami (ASPECTS < 5) – rekanalizácia
Komentár ku kontroverziám - Pragnancy and multiple sclerosis from a neurologist’s point of view
- Quality of life of caregivers of patients with progressive neurological disease
- New-onset refractory status epilepticus and considered spectrum disorders (NORSE/ FIRES)
- The efficacy of cochlear implantation in adult patients with profound hearing loss
- Clinical results of cervical discectomy and fusion with anchored cage – prospective study with a 24-month follow-up
- A comparison of mini-invasive percutaneous versus classic open pedicle screw fixation of thoracolumbar fractures – retrospective analysis
- Dural reconstruction with usage of xenogenic biomaterial
- Fingolimod attenuates harmaline-induced passive avoidance memory and motor impairments in a rat model of essential tremor
- Comment to the article N. Dahmardeh et al. Fingolimod attenuates harmaline-induced passive avoidance memory and motor impairments in a rat model of essential tremor
- Evaluation of systolic and diastolic cardiac functions and heart rate variability in patients with juvenile myoclonic epilepsy
- Reconstruction of the anterior skull base with free muscle flap after iatrogenic injury
- A Bulgarian family with epileptic seizures as a first manifestation of familial cerebral cavernous malformations
- Meningococcal meningitis with Chiari malformation (type I)
- Solitary cerebellar metastasis of uterine cervical carcinoma
- Abstrakta přednášek, které odezněly na XI. neuromuskulárním kongresu Brno, 10.–11. května 2018
- Analýza dat v neurologii
- Komentář k článku autorů Voháňka et al Anestezie a nervosvalová onemocnění Cesk Slov Neurol N 2018; 81/114(4): 501–514.
- Recenze knih
- Prof. MUDr. Ivan Rektor, CSc., FCMA, FANA, FEAN slaví významné životní jubileum
- Prof. MU Dr. Martin Bareš, Ph.D., padesátiletý
- Výroční kongres České neurochirurgické společnosti
- Česká a slovenská neurologie a neurochirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Diagnostics, symptomatology and findings in diseases and disorders of the autonomic nervous system in neurology
- New-onset refractory status epilepticus and considered spectrum disorders (NORSE/ FIRES)
- Clinical results of cervical discectomy and fusion with anchored cage – prospective study with a 24-month follow-up
- Pragnancy and multiple sclerosis from a neurologist’s point of view
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



