-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaThe effect of transversus abdominis plane block on post-operative pain relief: a prospective audit
TAP blok a pooperační bolest – prospektivní audit
Cíl studie:
“Transversus abdominis plane” (TAP) blok je relativně nová regionální technika, která poskytuje analgezii po výkonech břišní chirurgie. Lokální anestetikum je aplikováno do prostoru mezi m. transversus abdominis a m. obliquus internus abdominis. TAP blok může být proveden buď podle anatomických orientačních bodů, nebo pomocí ultrazvuku. Cílem bylo zhodnocení kvality pooperační analgezie po výkonech břišní chirurgie u pacientů, u nichž byl proveden TAP blok, jejich spokojenost a komplikace spojené s technikou.Typ studie:
Prospektivní audit.Typ pracoviště:
Anesteziologické oddělení výukové oblastní nemocnice.Materiál a metoda:
Pacientům, kteří byli zahrnuti v auditu, byl aplikován TAP blok. Pacienti byli sledováni na pooperačním oddělení a 24 hodin po výkonu. Dostali standardní peroperační a pooperační analgezii.Výsledky:
Audit celkově zahrnul 63 pacientů. U 1 pacienta nebyla vrácena kompletní data. Jednu pacientku nebylo možné vyhodnotit, protože byla pooperačně ventilována na JIP. Spokojeno nebo velmi spokojeno s kvalitou pooperační analgezie bylo 89 % pacientů. Padesát devět pacientů popsalo žádnou nebo pouze mírnou bolest na pooperačním oddělení a 52 pacientů uvedlo žádnou nebo mírnou bolest 24 hodin po výkonu. Žádná komplikace jako důsledek TAP bloku se nevyskytla.Závěr:
TAP blok je bezpečná a účinná metoda v komplexní léčbě pooperační bolesti po výkonech břišní chirurgie a je dobře tolerován ze strany pacientů.Klíčová slova:
transversus abdominis plane blok – laparotomie – laparoskopické operace – ulrazvukem naváděná regionální anestezie
Authors: P. Mcaleavey Francis 1; Michálek Pavel 1,2; Pokorný Lukáš 1; Periketi Dayakar 1
Authors place of work: Department of Anaestetics, Antrim Area Hospital, 45 Bush Road, Antrim, United Kingdom/Northern Ireland 1; 3. lékařská fakulta Univerzity Karlovy, Praha 2
Published in the journal: Anest. intenziv. Med., 21, 2010, č. 2, s. 85-90
Category: Anesteziologie - Původní práce
Summary
Objective:
The tranversus abdominis plane (TAP) block is a relatively new regional anaesthesia technique for provision of analgesia following abdominal surgery. Local anaesthetic is injected into the plane between transversus abdominis and the internal oblique muscles. The TAP block can be performed employing either a landmark technique or with ultrasound guidance. The goal of this audit was to ascertain the quality of postoperative analgesia following abdominal surgery in patients in whom the TAP block had been employed, patient satisfaction with analgesia and complication rate of the technique.Design:
Prospective audit.Settings:
Department of Anaesthetics, Regional Teaching Hospital.Material and methods:
Patients included in the audit were administered TAP blocks, either by landmark or ultrasound guided technique. These patients were then reviewed in recovery ward and at 24 hours postoperatively. Patients received standard intraoperative and post-operative analgesia in addition to the TAP blocks.Results:
63 patients were included in the audit. 1 patient had incomplete information returned. 1 patient was unable to be assessed as she required ventilation in ICU. 89% of patients were satisfied or very satisfied with the quality of postoperative analgesia. 59 patients reported no pain or mild pain in recovery ward and 52 patients reported no pain or mild pain at 24 hours. No patient suffered a complication as the result of a TAP block.Conclusion:
TAP block appears to be a safe and effective adjunct in the management of pain following abdominal surgery. It is well tolerated by patients.Keywords:
transversus abdominis plane block – laparotomy – major laparoscopic surgery – ultrasound-guided regional anaesthesiaIntroduction
Pain is an undesirable result of abdominal surgery. It has been previously demonstrated that a large portion of the pain associated with abdominal surgery derives from incision of the abdominal wall [1]. The abdominal wall itself comprises of three layers of muscle, the external oblique, the internal oblique and the transversus abdominis along with their associated fascial sheaths. Centrally, the abdominal wall includes the rectus abdominis muscles and their sheath. Innervation of the abdominal wall is via the branches of intercostal nerves which run through the transversus abdominis neuro-fascial plane [2].
Various strategies have been adopted for the control of pain in the postoperative period. These include nurse controlled analgesia (NCA) [3], patient controlled analgesia (PCA) [4], epidural analgesia [5], intrathecal opioid administration [6], and more recently, abdominal field blocks [7].
Although promising, the utility of abdominal field blocks is limited by their unpredictability, which may be in part due to the inability of the clinician to be certain of anatomical landmarks and needle tip position within tissue planes. For this reason, and based on previous work of Rafi [8], McDonnell et al. [9] sought a novel, reliable approach to blockade of abdominal wall nerve afferents – they named this block the “transversus abdominis plane (TAP) block”.
Interest in the TAP block has been demonstrated in several articles and in a variety of fields from elective abdominal surgery, paediatric and obstetric surgery [10, 11, 12]. The aim of this prospective audit study was to assess the efficacy of TAP block as a part of multimodal analgesia regimen across the spectrum of patients presenting for elective and emergency procedures in a teaching district general hospital.
Methods
Following to approval by the Trust Audit Committee, prospective 3 months collection of data was undertaken. Patient confidentiality was strictly preserved. A data sheet was used to collect per-operative information on the patients, and facilitated their review at 24 hours. Information on each individual was collected by the clinician who performed the anaesthesia. Data collected included the patients’ age, ASA classification, procedure scheduled and duration of the procedure. The patients’ reported level of pain was recorded along with their satisfaction with their analgesia regimen. The patients were then reviewed at 24 hours post operatively, whereupon their level of subjective pain was assessed, the amount of analgesia required was recorded, and the patients were asked to quantify their level of satisfaction with their post-operative analgesia. The results were then collated anonymously on a spreadsheet. Outcomes in which we were interested were reported pain in recovery ward and 24 hours, patient satisfaction with their analgesic regimen and the presence or otherwise of any complications from their analgesic regimen.
Pain was reported by the patients subjectively as mild, moderate or severe on a three point scale. Patient satisfaction was recorded on a five point scale ranging from extremely dissatisfied to very satisfied.
Patients’ consent for TAP block was sought pre-operatively. The TAP block was administered following induction of anaesthesia and before commencement of surgery, except in cases where surgery could not be delayed, for example, in the event of an emergency caesarean section. The TAP block was administered in accordance with the technique described by McDonnell et al. [9].
The iliac crests were palpated from anterior to posterior until the border of latissimus dorsi could be appreciated. The triangle of Petit could then be identified, as it is just anterior to the latissimus dorsi muscle (Fig. 1). We used a blunt needle to administer the local anaesthetic, either a 22G regional block needle or an 18G Tuohy needle depending on the operator. The needle was held perpendicular to the skin in a coronal plane and then advanced until resistance was felt. Further gentle advancement of the needle elicited an appreciable “click” which indicated that the needle tip had passed into the plane between the internal and external oblique muscles. A second “click” was elicited upon cautious advancement of the needle, at which point the tip was in the transversus abdominis plane. Inadvertent vascular puncture was excluded by careful aspiration before injection of local anaesthetic. Typically, 20 ml of 0.375% levobupivacaine was injected up to a dose of 1 mg . kg-1, however where this would have led to use of a small volume of local anaesthetic, some operators chose to use 0.25% levobupivacaine. In situations where surgical incision crossed the midline, the technique was repeated on the patient’s opposite side.
Fig. 1. Anatomical landmarks for transversus abdominis plane block 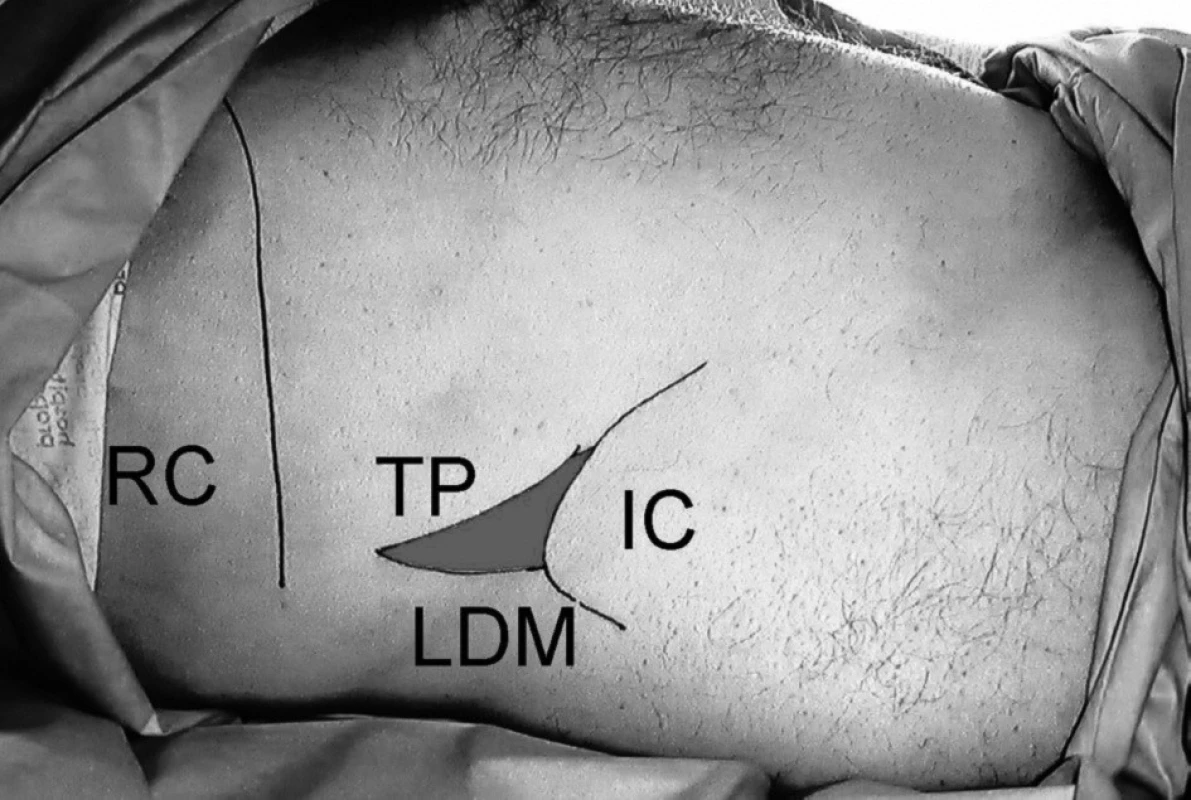
Legend: TP – triangle of Petit, IC – iliac crest, LDM – latissimus dorsi muscle, RC – lower border of rib cage Sixteen patients had their TAP block guided by ultrasound. A high-frequency linear ultrasound probe (HFL 38x, Sonosite Ltd., Hitchin, UK) was placed at the triangle of Petit, perpendicularly to the iliac crest. The 18-G Tuohy epidural needle was then directed into the transversus abdominis plane using “in-plane” (IP) technique (Fig. 2, Fig. 3). Ultrasound usage was dictated by operator preference and experience. Time to entry of the tranversus abdominis plane was not recorded. The dose of local anaesthetic used was the same regardless of the use of ultrasound, at 1 mg . kg-1 bilaterally.
Fig. 2. Ultrasonographic image for TAP block using in plane (IP) technique 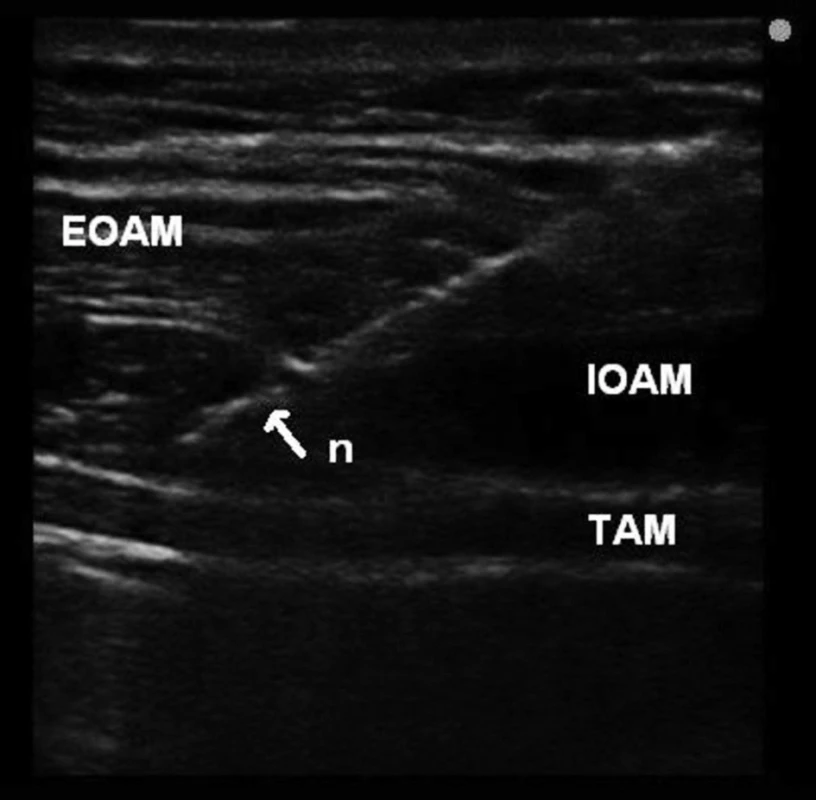
Legend: EOAM – external oblique abdominis muscle, IOAM – internal oblique abdominis muscle, TAM – transversus abdominis muscle, n – needle Fig. 3. Distribution of local anaesthetic solution in transversus abdominis plane between the internal oblique abdominis and transversus abdominis muscles 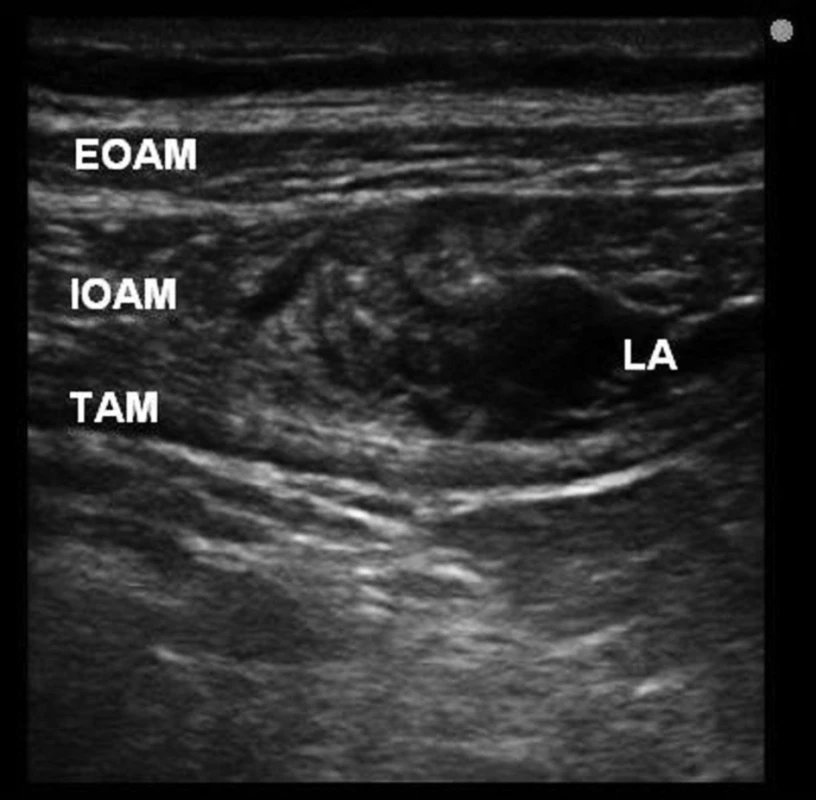
Legend: EOAM – external oblique abdominis muscle, IOAM – internal oblique abdominis muscle, TAM – transversus abdominis muscle, LA – local anaesthetic Results
63 patients were included in the audit. Information was generally well recorded, however, 1 form was incomplete. Of the 63 patients, 28 were male and 35 were female. The age range of the patients was from 8 to 86 years of age (mean = 51.4 years, median = 52 years, interquartile range = 35.5 years). The surgical specialties involved were gynaecology and general surgery, and encompassed open and laparoscopic surgery. The range of procedure duration was from 30 to 360 minutes (mean = 117 min, median = 90 min, interquartile range 105 min).
Of the 63 patients recorded, 19 (30%) had a unilateral TAP block performed, for instance in the case of appendicectomy or inguinal hernia repair. 44 patients (70%) had a bilateral TAP block performed. Ultrasound guidance was employed in 16 cases (25%). All patients received up to 1 mcg . kg-1 of fentanyl at induction, and all patients were administered additional intraoperative morphine sulphate of up to 0.1 mg . kg-1. All patients were administered intravenous paracetamol per-operatively, and 14 patients were administered non-steroidal analgesics.
Of the 63 patients, 37 (59%) were prescribed post-operative patient-controlled analgesia (PCA) with morphine sulphate, and the remainder were prescribed nurse-controlled opioid in addition to intravenous paracetamol and non-steroidal analgesics.
59 patients (94%) reported no or mild pain in recovery ward. No patient reported severe pain in the recovery ward and one patient’s pain was unable to be assessed as she was transferred to intensive care for post-operative care.
After 24 hours, 52 patients (83%) reported only no pain or mild pain. 8 patients (12.5%) reported moderate pain, while one patient (1.5%), whose laparoscopic procedure required conversion to an open procedure reported severe pain. We were unable to assess 2 patients’ (3%) post-operative pain because their forms were incomplete.
Post-operative opioids were required for most patients, however 4 patients (6%) required no post-operative opioid. Two of these patients had undergone major laparoscopic bowel surgery, one had undergone a laparotomy and the fourth had undergone a laparoscopic cholecystectomy. The majority of patients (44–70%) required less than 20mg of morphine in the first 24 hours (Graph 1). All patients received their prescribed non-opioid analgesics regularly.
Graph 1. Post-operative opioid requirements in patients given TAP block. (PCAS – Patient Controlled Analgesia System, NCAS – Nurse Controlled Analgesia) 
Patient satisfaction levels with post-operative analgesia were very high. 56 patients (89%) reported that they were satisfied or very satisfied with their pain management. 4 (6%) patients were ambivalent, 1 (1.5%) was rather unsatisfied, and the data was incomplete for two patients (Graph 2).
Graph 2. Graph 2. Reported patient satisfaction with post-operative analgesia 
Twelve of the 63 patients (19%) in the audit underwent major laparoscopic surgery. Five patients reported no pain in the immediate post operative period, and these patients went on to report no pain at 24 hours. Two patients who reported mild pain in recovery ward reported no pain once 24 hours had elapsed. One patient reported severe pain. This patient’s procedure had been noted as difficult, and required conversion to an open operation. All except this patient were satisfied (6 patients) or very satisfied (5 patients) with their analgesia.
Opioid use in this group was generally low. All patients were prescribed a PCA in addition to non-opioid analgesics. All patients except one used less than 40 mg of morphine in the first 24 hours, and 2 patients used no morphine in that time (Graph 3).
Graph 3. Post operative opioid requirements following major laparoscopic surgery 
Complications
No patients suffered a complication as the result of TAP block. 2 patients (3%) reported severe post-operative nausea and vomiting.
Discussion
Our results showed that in our group of patients, TAP block was a well tolerated and safe method of providing postoperative analgesia following abdominal surgery. Only one of 63 patients was dissatisfied with their postoperative analgesia. Reported pain levels and opioid requirements in the recovery period and first 24 hours were lower than we had expected. Of our 63 patients, the vast majority (59 patients) reported no pain or mild pain in recovery ward, and 52 patients reported no pain or mild pain in the first 24 hours post-operatively.
Opioid usage compared favourably to other work which had studied opioid requirements following major abdominal surgery. For example, Reeves and colleagues [13] found that the mean amount of morphine administered via PCA systems following major abdominal surgery in a group of 35 patients was 71 mg over 24 hours. The mean amount of morphine administered via PCA in our group of patients was 22.5 mg, although our group of patients did include those undergoing intermediate surgery.
Mukhtar and Singh reported the use of TAP blocks for intermediate laparoscopic surgery in five patients [14]. They felt that TAP blocks appeared to be a useful adjunct in the management of postoperative pain. Our audit showed that TAP blockade appears to be useful in major abdominal laparoscopic surgery. Of the 63 patients in our audit, 12 underwent major laparoscopic surgery. Reported pain levels and opioid usage in this group were generally low, except from one patient who required conversion to an open procedure. This could be due to injection of the local anaesthetic in the incorrect plane, or that the spread of local anaesthetic is insufficient to cover the upper pole of a large midline incision. In one study to determine spread of injectate following ultrasound-guided TAP block, it was found that segmental nerves T10, T11, T12 and L1 were likely to be involved, the implication being that the utility of the TAP block is limited to lower abdominal surgery [15].
Tab. 1. Breakdown of patients by type of operation 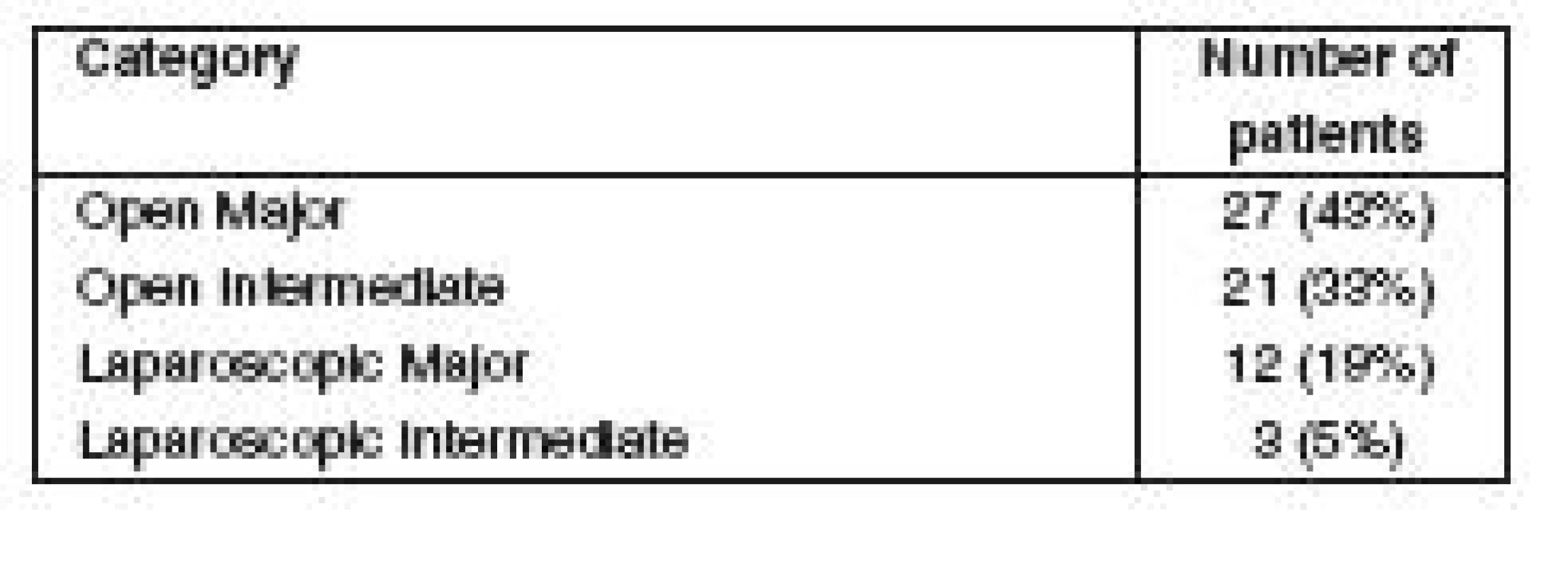
None of the patients in our audit suffered a complication as the result of TAP block. However, it has to be mentioned that one case of liver trauma associated with blind technique of TAP block has been described [16]. Employing an ultrasound-guided technique may improve the safety of TAP block placement.
We also noted that administration of prescribed simple and non-steroidal analgesics in addition to PCA was invariably regular and appreciate that this may have contributed to the high levels of patient satisfaction with analgesia.
We appreciate that our ability to evaluate patients’ pain and satisfaction in this audit is limited. Our patients were a heterogenous, unmatched group with no blinding, randomisation or control group, and pain was assessed by a number of different individuals. Nonetheless, we feel that TAP blocks may be a safe and useful adjunct in a multimodal approach to the control of postoperative pain following abdominal surgery.
Tab. 2. Opioid (morphine) requirements in the first 24 hours postoperatively 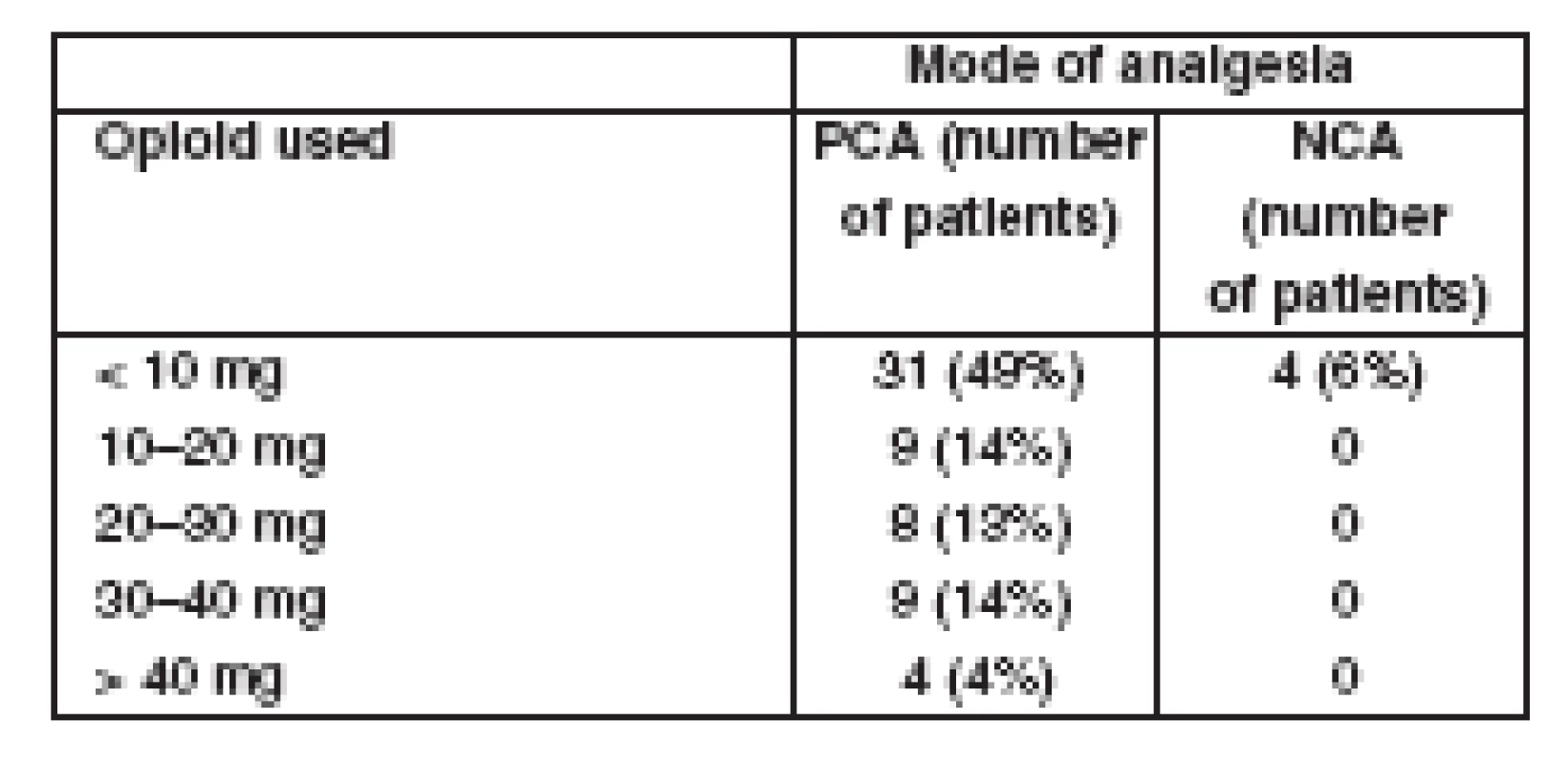
We would like to remark on some other points arising from this audit. For patients undergoing extensive laparotomies some other regional anaesthesia technique covering upper abdominal segments should probably be employed. Hebbard recommended performing additional subcostal TAP blocks in extensive laparotomies [17].
We have already started to supplement classical TAP block with a bilateral subcostal TAP technique for these laparotomies. One must be careful not to exceed maximal doses of local anaesthetics. For this reason, a suitable dilute preparation of local anaesthetic, for example, 0.2% of levobupivacaine should be used.
Ultrasound guidance seems to be useful adjunct to TAP blockade. It allows a real-time evaluation of the needle passage [18], local anaesthetic distribution and, potentially, facilitates TAP catheter placement for continuous postoperative analgesia.
We are planning to establish a research project evaluating the efficacy of subcostal TAP blocks in extensive and upper laparotomies. We have already started a prospective randomized study comparing blind and ultrasound-guided techniques (NCT00972920, www.clinicaltrials.gov).
Conclusion
Based on the results of our audit, we would like to conclude that TAP block may be a reliable and safe technique for provision of analgesia for patients undergoing laparotomy or other abdominal wall procedures. Future directions should focus on ultrasound guidance for this block and on RCTs comparing this method with epidural analgesia and PCA.
Adresa pro korespondenci:
Dr Francis McAleavey
Dept of Anaesthetics, Antrim Area Hospital
45 Bush Road, Antrim
BT41 4RD United Kingdom, Northern Ireland
e-mail: frankiemca@aol.com
Zdroje
1. Wall, P. D., Melzack, R. Pain measurements in persons in pain. In: Wall, P. D., Melzack, R., eds. Textbook of Pain. 4th ed. Edinburgh, UK: Churchill Livingstone, 1999, p. 409–426.
2. Abrahams, P. H., Marks, S. C., Hutchings, R. T. Abdomen and Pelvis. In Abrahams, P. H., Marks, S. C., Hutchings, R. T. McMinn’s Colour Atlas of Human Anatomy. 5th ed. Edinburgh, UK: Elsevier Science Ltd, 2003, p. 221–284.
3. Everett, B., Salamonson, Y. Differences in postoperative opioid consumption in patients prescribed patient-controlled analgesia versus intramuscular injection. Pain Manag. Nurs., 2005, 6, p. 137–144.
4. Werawatganon, T., Charuluxananan, S. Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database of Systematic Reviews 2005, Issue 1. Art. No.: CD004088. DOI: 10.1002/14651858.CD004088.pub2.
5. Pouzeratte, Y., Delay, J. M., Brunat, G., Boccara, G., Vergne, C., Jaber, S., Fabre, J. M., Colson, P., Mann, C. Patient-controlled epidural analgesia after abdominal surgery: ropivacaine versus bupivacaine. Anesth. Analg., 2001, 93, p. 1587–1592.
6. Lim, P. C., MacIntyre, P. E. An audit of intrathecal morphine analgesia for non-obstetric postsurgical patients in an adult tertiary hospital. Anaesth. Intensive Care, 2006, 34, p. 776–781.
7. Dierking, G. W., Dahl, J. B., Kanstrup, J., Dahl, A., Kehlet, H. Effect of pre - vs postoperative inguinal field blockade on postoperative pain after herniorrhaphy. Br. J. Anaesth., 1992, 68, p. 344–348.
8. Rafi, A. N. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia, 2001, 56, p. 1024–1026.
9. McDonnell, J. G., O’Donnell, B., Curley, G., Heffernan, A., Power, C., Laffey, J. G. The analgesic efficacy of tranversus abdominis plane block after abdominal surgery: a prospective randomised controlled trial. Anesth. Analg., 2007, 104, p. 193–197.
10. Cooke, A., O’ Neill, O., Shields, M., Mulholland, D. Transversus abdominis blocks in elective abdominal surgery. Reg. Anesth. Pain Med., 2008, 33, p. e98.
11. Ludot, H., Testard, A., Ferrand, I., Sennah, C., Labrousse, M., Malinovsky, J. Transversus abdominis plane block (TAPB) and continuous psoas compartment block (CPCB) : efficacy in pediatric complex pelvic osteotomy. Reg. Anesth. Pain Med., 2008, 33, p. e98.
12. McDonnell, J. G., Curley, G., Carney, J., Benton, A., Costello, J., Maharaj, C. H., Laffey, J. G. The analgesic efficacy of transversus abdominis plane block after caesarean delivery: a randomised controlled trial. Anesth. Analg., 2008, 106, p. 186–191.
13. Reeves, M., Lindholm, D. E., Myles, P. S., Fletcher, H., Hunt, J. O. Adding ketamine to morphine for patient controlled analgesia after major abdominal surgery: a double-blinded, randomized controlled trial. Anesth. Analg., 2001, 93, p. 116–120.
14. Mukhtar, K., Singh, S. Transversus abdominis plane block for laparoscopic surgery. Br. J. Anaesth., 2009, 102, p. 143–144.
15. Tran, T. M. N., Ivanusic, J. J., Hebbard, P., Barrington, M. J. Determination of spread of injectate after ultrasound-guided transversus abdominis plane block: a cadaveric study. Br. J. Anaesth., 2009, 102, p. 123–127.
16. Farooq, M., Carey, M. A case of liver trauma with a blunt regional anesthesia needle while performing transversus abdominis plane block. Reg. Anesth. Pain Med., 2008, 33, p. 274–275.
17. Hebbard, P. Subcostal transversus abdominis plane block under ultrasound guidance. Anesth. Analg., 2008, 106, p. 274–275.
18. El-Dawlatly, A. A., Turkistani, A., Kettner, S. C., Machata, A. M., Delvi, M. B., Thallaj, A., Kapral, S., Marhofer, P. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br. J. Anaesth., 2009, 102, p. 763–767.
Štítky
Anesteziologie a resuscitace Intenzivní medicína
Článek vyšel v časopiseAnesteziologie a intenzivní medicína
Nejčtenější tento týden
2010 Číslo 2- Jak souvisí postcovidový syndrom s poškozením mozku?
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
- Neodolpasse je bezpečný přípravek v krátkodobé léčbě bolesti
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Metamizol a jeho pozice v léčbě bolesti
-
Všechny články tohoto čísla
- Multimodal monitoring in neurointensive care of severe traumatic brain injury
- Tomas Kadlic Memorial – Ass. Prof. Tomas Kadlic, M. D.
- Programové prohlášení výboru na období 2009-2012
- Prohlášení Sekce pro ultrazvukové metody ČSARIM
- Zápis ze zasedání Akreditační komise oboru Anesteziologie a resuscitace ze dne 18.11.2009
- Rozhodování o přechodu z intenzivní na paliativní péči u pacientů s postupujícím a nezvratným multiorgánovým selháváním – konsenzuální stanovisko
- Registr pacientů s infekcí H1N1 hospitalizovaných na odděleních typu ARO/JIP 18. 11. 2009
- Zápis z jednání výboru č. 4/2009
- Přínos Johna W. Severinghause anesteziologii a intenzivní medicíně
- John W. Severinghaus – fyzik, elektronik, lékař, vědec
- Translating Basic Science to Clinical Care
- Úspěch na Postgraduate Assembly of Anesthesiology
- Influence of age on the pharmacodynamic parameters of cisatracurium, rocuronium and vecuronium in males during total intravenous anaesthesia – a prospective study
- The effect of transversus abdominis plane block on post-operative pain relief: a prospective audit
- First Aid Courses (basic life support) for parents of pre-term newborns – a retrospective analysis of questionnaires
- Kritéria pro zahájení venovenózního ECMO u pacientů s respiračním selháním na základě infekce virem H1N1, platné v Kardiocentru VFN Praha
- Coupled plasma filtration adsorption in experimental septic shock
- Anesteziologie a intenzivní medicína
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- The effect of transversus abdominis plane block on post-operative pain relief: a prospective audit
- Rozhodování o přechodu z intenzivní na paliativní péči u pacientů s postupujícím a nezvratným multiorgánovým selháváním – konsenzuální stanovisko
- Multimodal monitoring in neurointensive care of severe traumatic brain injury
- Kritéria pro zahájení venovenózního ECMO u pacientů s respiračním selháním na základě infekce virem H1N1, platné v Kardiocentru VFN Praha
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



