-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Reduction in Infection Rates after Mandatory Hospital Public Reporting: Findings from a Longitudinal Cohort Study in Canada
Background:
The role of public reporting in improving hospital quality of care is controversial. Reporting of hospital-acquired infection rates has been introduced in multiple health care systems, but its relationship to infection rates has been understudied. Our objective was to determine whether mandatory public reporting by hospitals is associated with a reduction in hospital rates of Clostridium difficile infection.Methods and Findings:
We conducted a longitudinal, population-based cohort study in Ontario (Canada's largest province) between April 1, 2002, and March 31, 2010. We included all patients (>1 y old) admitted to 180 acute care hospitals. Using Poisson regression, we developed a model to predict hospital - and age-specific monthly rates of C. difficile disease per 10,000 patient-days prior to introduction of public reporting on September 1, 2008. We then compared observed monthly rates of C. difficile infection in the post-intervention period with rates predicted by the pre-intervention predictive model. In the pre-intervention period there were 33,634 cases of C. difficile infection during 39,221,113 hospital days, with rates increasing from 7.01 per 10,000 patient-days in 2002 to 10.79 in 2007. In the first calendar year after the introduction of public reporting, there was a decline in observed rates of C. difficile colitis in Ontario to 8.92 cases per 10,000 patient-days, which was significantly lower than the predicted rate of 12.16 (95% CI 11.35–13.04) cases per 10,000 patient-days (p<0.001). Over this period, public reporting was associated with a 26.7% (95% CI 21.4%–31.6%) reduction in C. difficile cases, or a projected 1,970 cases averted per year (95% CI 1,476–2,500). The effect was specific to C. difficile, with rates of community-acquired gastrointestinal infections and urinary tract infections unchanged. A limitation of our study is that this observational study design cannot rule out the influence of unmeasured temporal confounders.Conclusions:
Public reporting of hospital C. difficile rates was associated with a substantial reduction in the population burden of this infection. Future research will be required to discern the direct mechanism by which C. difficile infection rates may have been reduced in response to public reporting.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 9(7): e32767. doi:10.1371/journal.pmed.1001268
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001268Summary
Background:
The role of public reporting in improving hospital quality of care is controversial. Reporting of hospital-acquired infection rates has been introduced in multiple health care systems, but its relationship to infection rates has been understudied. Our objective was to determine whether mandatory public reporting by hospitals is associated with a reduction in hospital rates of Clostridium difficile infection.Methods and Findings:
We conducted a longitudinal, population-based cohort study in Ontario (Canada's largest province) between April 1, 2002, and March 31, 2010. We included all patients (>1 y old) admitted to 180 acute care hospitals. Using Poisson regression, we developed a model to predict hospital - and age-specific monthly rates of C. difficile disease per 10,000 patient-days prior to introduction of public reporting on September 1, 2008. We then compared observed monthly rates of C. difficile infection in the post-intervention period with rates predicted by the pre-intervention predictive model. In the pre-intervention period there were 33,634 cases of C. difficile infection during 39,221,113 hospital days, with rates increasing from 7.01 per 10,000 patient-days in 2002 to 10.79 in 2007. In the first calendar year after the introduction of public reporting, there was a decline in observed rates of C. difficile colitis in Ontario to 8.92 cases per 10,000 patient-days, which was significantly lower than the predicted rate of 12.16 (95% CI 11.35–13.04) cases per 10,000 patient-days (p<0.001). Over this period, public reporting was associated with a 26.7% (95% CI 21.4%–31.6%) reduction in C. difficile cases, or a projected 1,970 cases averted per year (95% CI 1,476–2,500). The effect was specific to C. difficile, with rates of community-acquired gastrointestinal infections and urinary tract infections unchanged. A limitation of our study is that this observational study design cannot rule out the influence of unmeasured temporal confounders.Conclusions:
Public reporting of hospital C. difficile rates was associated with a substantial reduction in the population burden of this infection. Future research will be required to discern the direct mechanism by which C. difficile infection rates may have been reduced in response to public reporting.
: Please see later in the article for the Editors' SummaryIntroduction
The past decade has witnessed a remarkable global surge in the incidence and severity of Clostridium difficile infection [1]–[4]. This pathogen has long been among the most burdensome hospital-acquired infections, but has now become a leading contributor to infectious disease morbidity and mortality in developed countries [5]. The majority of C. difficile infections are acquired in hospital, and many of these are potentially preventable through strategies aimed at minimizing transmission between patients or decreasing patient susceptibility, primarily by reducing inappropriate antibiotic use [6].
Mandating public reporting of quality care metrics has been one vehicle used by health care payers to incentivize improvements in hospital care at a system level. Several theories have been put forth for how public reporting might improve patient outcomes: public reporting could encourage patients and their agents to select higher performing institutions (selection pathway), it could allow hospitals to identify areas of poor performance to target for improvement (change pathway), or it could motivate institutions to avoid the shame of a bad performance report and seek the pride of a good report (reputation pathway) [7],[8]. Most evidence, including a recent randomized trial of public reporting of cardiac quality indicators, suggests that the potential benefit is largely in stimulating quality improvement efforts [9]. However, the benefits and hazards of public reporting systems may vary depending on the specific clinical context (identification of appropriate measurements and responsible providers, and the need for risk adjustment) [7],[10],[11], and public reporting is particularly understudied in the domain of hospital-acquired infections [12].
In Ontario, Canada, the Ontario Ministry of Health and Long-Term Care (MOHLTC) selected C. difficile rates as the first among a slate of hospital patient safety indicators to be subject to mandatory monthly public reporting starting September 1, 2008 [13]. Hospitals were obligated to collect their own data on hospital-acquired C. difficile infections, and report the data monthly to the MOHLTC for posting on a publicly accessible website. No additional hospital-level incentives or disincentives were initially implemented, but there was acknowledgment that hospital global budgets and hospital executive compensation could eventually be linked to hospital performance [14].
The objective of our investigation was to utilize population-based health care data in Ontario, Canada, as an independent means to rigorously evaluate the impact of a public reporting system on province-wide, hospital-specific rates of this burdensome pathogen.
Methods
Ethics Statement
The study was approved by the research ethics board of Sunnybrook Health Sciences Centre.
General Study Design
We conducted a retrospective, longitudinal population-based cohort study of all patients (>1 y old) admitted to acute care hospitals in Ontario between April 1, 2002, and March 31, 2010. Poisson regression analysis was used to develop a high-fidelity predictive model of hospital rates of C. difficile infection prior to public reporting, to allow an assessment of the change in provincial hospital-specific rates of C. difficile infection following the introduction of mandatory public reporting (introduced September 2008).
Data Sources
The cohort was derived from a linkage of well-validated, province-wide health care administrative databases housed at the Institute for Clinical Evaluative Sciences [15],[16]. The Registered Persons Database contains demographic data for all of Ontario's 12.2 million residents; the Ontario Health Insurance Plan database includes physician billing claims for all visits and procedures performed within Ontario's universal single-payer health care system; the Canadian Institute for Health Information Discharge Abstract Database details all hospitalization events; the Ontario Drug Benefit database contains comprehensive and accurate (>99% concordant with chart review) outpatient drug information for Ontario's 1.2 million elderly residents [16].
C. difficile rates from health care administrative data were validated against rates reported by individual institutions via the mandatory public reporting system. Given that these reporting data are only available (by definition) from the period after the program was initiated, and given that they are aggregated at the hospital level (without any risk adjustment), they cannot be directly used to evaluate the impact of the program. Hospitals reported all cases of C. difficile diagnosed at their institution, using a standardized case definition, and were required to classify the origin of cases as (i) nosocomial acquisition from their institution, (ii) nosocomial acquisition from another institution, or (iii) community acquisition or unknown/indeterminate source. Only those cases deemed by the institution to have been acquired in their own hospital are incorporated into the numerator of monthly publicly reported rates. However, for this study we had access to overall C. difficile rates, including cases assigned to any of the three categories.
Patient Selection Criteria
We identified all patients admitted to an acute care hospital in Ontario between April 1, 2002, and March 31, 2010. We excluded infants as well as patients admitted to psychiatry, rehabilitation, and complex continuing care institutions, given low expected event rates, and the fact that admissions to these non-acute-care centers are recorded in separate, less well validated databases. The use of broad inclusion criteria was intended to generate population-based data, and avoid the selection bias that is inherent in clinical surveillance networks. In total, data from 180 acute care hospitals contributed to the analysis during the 8-y study period, including 165 which contributed data to the public reporting period (September 1, 2008, to March 31, 2010). Individual hospitals were included even if they were in existence for only part of the pre-intervention and/or post-intervention period(s), because even with hospital openings, closures, and mergers during the 9-y study period, the net population at risk was considered to be all Ontario patients admitted to acute care hospital beds.
Primary Predictor
The primary predictor in this study was the date of initiation of mandatory public reporting of hospital C. difficile rates, which was implemented by the MOHLTC on September 1, 2008.
Outcome Definition
The primary outcome was the hospital - and age-specific monthly rates of C. difficile disease per 10,000 hospital patient-days. C. difficile disease is captured in the hospital database, through a single International Classification of Diseases (ICD) code (ICD-10 code A047). Two prior validation studies in the United States have indicated that ICD codes are sensitive (71%–88%) and specific (>99%) for the diagnosis of C. difficile infection [17],[18]. It is less clear whether administrative databases can accurately distinguish the source of C. difficile acquisition, and so we included all cases rather than just those that were labelled as post-admission diagnoses [19].
Validation of C. difficile Rates in the Administrative Datasets
For additional indirect validation of ICD-10 codes in the local context, data from September 1, 2008, to March 31, 2010 (the period of public reporting), were used to compare hospital-level C. difficile counts in the administrative data to publicly reported counts. Pearson correlation coefficients (weighted for hospital bed-days) were calculated for overall C. difficile cases and nosocomial C. difficile cases across the institutions subject to public reporting.
Risk Strata
Hospitalized patients were grouped into monthly, age group, and hospital-specific strata. Hospitalized patients were separated into nine age strata: 1–18, 19–30, 31–40, 41–50, 51–60, 61–70, 71–80, 81–90, and >90 y old. In total there were 124,740 potential strata in the pre-intervention period (77 mo×nine age groups×180 institutions), and 30,780 potential strata in the post-intervention period (19 mo×nine age groups×180 institutions). The actual number of strata was slightly lower (133,418), given that not all age strata were represented in all hospital-months, and some hospitals were not in existence for the entire study duration.
Statistical Analysis
Primary analysis
We first computed C. difficile rates by age group, month, and hospital strata prior to September 1, 2008, to visually inspect temporal trends, overall and by hospital. The numerator was the number of C. difficile cases in each stratum; the denominator was the at-risk hospitalized population in each stratum (10,000 patient-days). In the primary analysis, we examined whether the introduction of public reporting of C. difficile rates in September 2008 was associated with a significant decline in hospital-specific C. difficile rates.
To model the temporal patterns of C. difficile infections, we used generalized estimating equations for clustered count data to account for correlations among outcomes within hospitals over time, using an auto-regressive correlation structure with a period of 3 mo [20]. The unit of analysis was the hospital, month, and age group stratum. The dependent variable was the number of C. difficile infections in each stratum; the offset parameter was the number of patient-days in each stratum. All models included age group, pre-reporting calendar month (to account for seasonal trends), hospital facility type (acute teaching, large community, or small community), concurrent and 1 - to 12-mo lagged provincial monthly rates of prescriptions of antimicrobials, and indicator variables for each post-reporting month, coded as the difference between the specific post-reporting month and the corresponding pre-reporting calendar month. The exponentiated post-month regression coefficients thus represent the relative difference between the observed post-month and the predicted post-month based on the pre-reporting trends. We planned to model longitudinal trend with both linear and non-linear functions. Model fit was assessed through graphical inspection of observed and predicted rates over the pre-intervention period, as well as through deviance and Pearson chi-square statistics.
We used 6.5 y of data to model pre-reporting trends, and projected these trends to the post-reporting period after September 1, 2008, to obtain predicted rates in the absence of reporting. The predicted cases and 95% confidence intervals for a calendar month after public reporting were computed as the observed number of cases for that month divided by the corresponding relative rates from the model, as in previous work [21]. The overall relative difference in infection rates in the calendar year 2009 was obtained as the exponentiated weighted average of the regression coefficients corresponding to that period, weighting by log person-days. Averted cases were computed as the difference between predicted and observed cases in post-reporting months. The decrease in hospital C. difficile rates was computed for the overall population, as well as for hospital facility subtypes. In a sensitivity analysis, to test the robustness of our results and to ensure that findings were not being driven by coding practices in a few large institutions, we excluded hospitals with discordant rates of C. difficile in the public reporting and administrative datasets.
Tracer analyses
To test the specificity of our findings, we examined tracer outcomes that should not be impacted by C. difficile public reporting. First, we inspected hospital admissions for other bacterial gastrointestinal pathogens. These pathogens (Salmonella, Shigella, Campylobacter, Listeria, and Yersinia, among others) are almost universally community-acquired, to the extent that microbiology laboratory guidelines recommend against testing for these pathogens when infections arise more than 72 h post-admission [22]. We also inspected urinary tract infections as a tracer outcome; although a fraction of urinary tract infections are hospital-acquired, they are not yet subject to public reporting, and the primary means of preventing nosocomial urinary tract infections (e.g., urinary catheter avoidance) differ from the prevention strategies for C. difficile [6],[23].
Analyses were performed using STATA procedure XTGEE. Patient confidentiality was maintained via encrypted health card numbers using Institute for Clinical Evaluative Sciences protocols.
Results
Cross-Validation of C. difficile Rates in Public Reporting and Administrative Datasets
The total number of C. difficile cases publicly reported by each Ontario hospital between September 1, 2008, and March 31, 2010, was compared to the corresponding number of cases recorded in the provincial administrative datasets. There was an excellent concordance for overall C. difficile cases (Figure 1A; weighted Pearson's correlation coefficient 0.92), and nosocomial C. difficile cases (Figure 1B; weighted Pearson's correlation coefficient 0.91) across these institutions.
Fig. 1. Correlation of aggregate hospital C. difficile cases in administrative datasets and public reporting statistics. 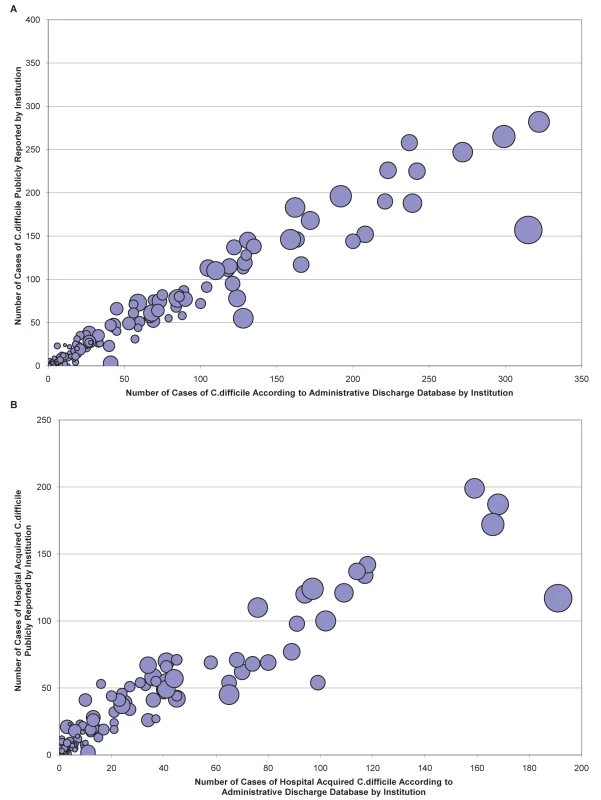
C. difficile cases in the administrative data are plotted against cases from the public reporting database, for the total public reporting period between September 1, 2008, and March 31, 2010. Each bubble represents a distinct institution (n = 165), and bubble sizes reflect hospital sizes (in patient-days). There was an excellent correlation for overall C. difficile cases (A) (weighted Pearson's correlation coefficient 0.92), and hospital-acquired C. difficile cases (B) (weighted Pearson's correlation coefficient 0.91). C. difficile Rates in Ontario prior to the Introduction of Public Reporting
There were a total of 6,068,777 acute care hospital admissions, and 39,221,113 hospital days at risk for C. difficile infection in the pre-intervention period between April 1, 2002, and August 31, 2008. During this time there were 33,634 cases of C. difficile infection, corresponding to a rate of 5.54 per 1,000 hospitalizations or 8.58 per 10,000 patient-days. Of these cases, 14,956 (44.5%) were recorded as post-admission complications, corresponding to a rate of 2.46 nosocomial cases per 1,000 hospitalizations or 3.81 per 10,000 patient-days.
Provincial monthly rates per 10,000 patient-days did not differ by sex (data not shown), but did increase markedly in older age groups: 4.86 infections per 10,000 patient-days for 1–18 y olds, 2.88 for 19–30, 3.31 for 31–40, 5.84 for 41–50, 6.97 for 51–60, 8.55 for 61–70, 10.84 for 71–80, 12.05 for 81–90, and 12.46 for >90 y olds. C. difficile rates were highest in large community hospitals (8.97 per 10,000 patient-days), followed by academic teaching hospitals (8.01) and small community hospitals (7.88).
There was marked seasonal variation in C. difficile rates, with yearly peaks in winter months (Figure 2). In addition, crude C. difficile rates increased over this pre-intervention period, from 7.01 per 10,000 patient-days in 2002, to 6.39 in 2003, 8.14 in 2004, 9.5 in 2005, 8.23 in 2006, and 10.79 in 2007. The overall burden of antibiotic use in Ontario (as measured by outpatient antibiotic prescriptions to elderly individuals) also exhibited seasonal peaks preceding C. difficile peaks, and increased over the pre-intervention period (Figure 2). The yearly antibiotic consumption increased from 2,110,184 prescriptions in 2003, to 2,323,006 in 2008, and 2,426,138 in 2009. The final predictive model incorporated age, hospital type, calendar month, and burden of antibiotic use in current and 12 lagged months. In this model there was no statistically significant longitudinal time trend prior to public reporting (the increase in pre-intervention rates was predicted by the combination of other covariates).
Fig. 2. Longitudinal trends in C. difficile infection rates and antibiotic prescription rates in Ontario prior to the introduction of mandatory public reporting. 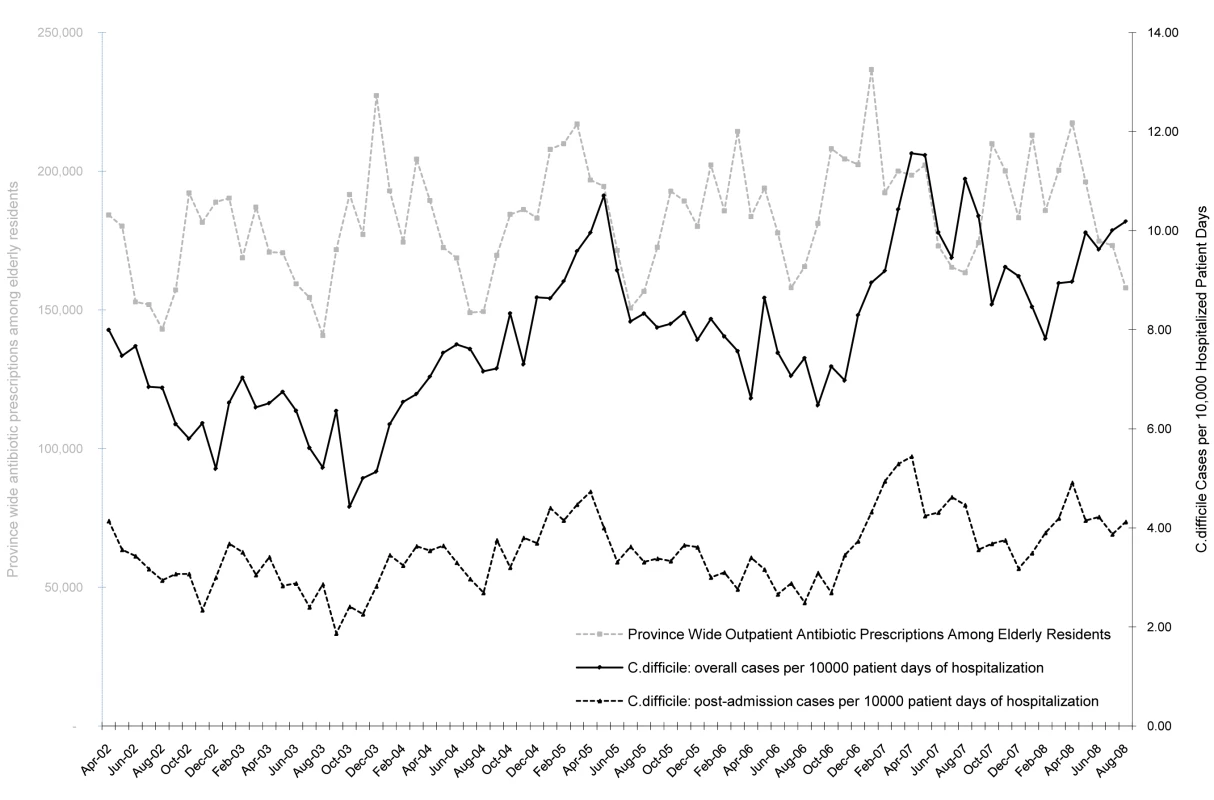
Seasonal variations in overall C. difficile infection rates (black solid line) and post-admission C. difficile infection rates (black dashed line) per 10,000 patient-days appear to follow seasonal changes in the overall monthly population burden of antibiotic prescriptions measured by the number of prescriptions in the Ontario Drug Benefit database (grey dashed line). Predictors of Monthly C. difficile Rates
As compared to the reference age group of 61–70 y olds, all younger age groups had a reduced incidence rate ratio of C. difficile infection, while all older age groups had an increased incidence (Table 1). Infection rates were lower in small community hospitals, as compared to academic teaching hospitals. Higher C. difficile monthly rates were associated with higher total outpatient elderly antibiotic prescriptions in Ontario in the preceding months, with time lags up to 9 mo (Table 1).
Tab. 1. Predictors of monthly hospital-specific C. difficile infection rates in a multivariate Poisson model of the period prior to public reporting. 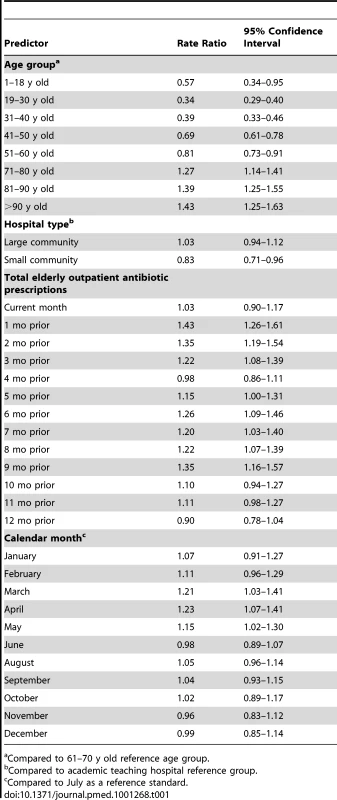
Compared to 61–70 y old reference age group. C. difficile Rates in Ontario following the Introduction of Public Reporting
After the introduction of public reporting, there was a gradual decline in age-specific hospital rates of C. difficile colitis in Ontario (Figure 3). The observed post-intervention rates diverged from predicted rates based on the pre-reporting-period trends: rates were forecasted to continue to rise during this period (Figure 3). There were 8,787 cases of C. difficile in Ontario during the 19-mo post-intervention period, as compared to 11,392 predicted by the Poisson model. In 2009, the first full calendar year after public reporting was instituted, there were only 5,417 cases (8.92 per 10,000 patient-days) as compared to 7,327 predicted by the Poisson model (12.16 per 10,000 patient-days, 95% CI 11.35–13.04 cases per 10,000 patient-days) (p<0.001). This corresponded to a 26.7% reduction in C. difficile cases (95% CI 21.4%–31.6%). Predicted rates were higher than observed rates across all facility types, including large community hospitals (12.9 versus 10.1 per 10,000 patient-days), small community hospitals (10.1 versus 5.4 per 10,000 patient-days), and acute teaching hospitals (11.1 versus 7.5 per 10,000 patient-days). Public reporting was associated with a projected 1,970 cases averted in the first calendar year after introduction (95% CI 1,476–2,500 cases) (Table 2). Findings were similar in a sensitivity analysis excluding two large hospitals with the greatest discordance between C. difficile rates in the publicly reported and administrative datasets (data not shown).
Fig. 3. Reduced rates of C. difficile infection associated with the introduction of public reporting. 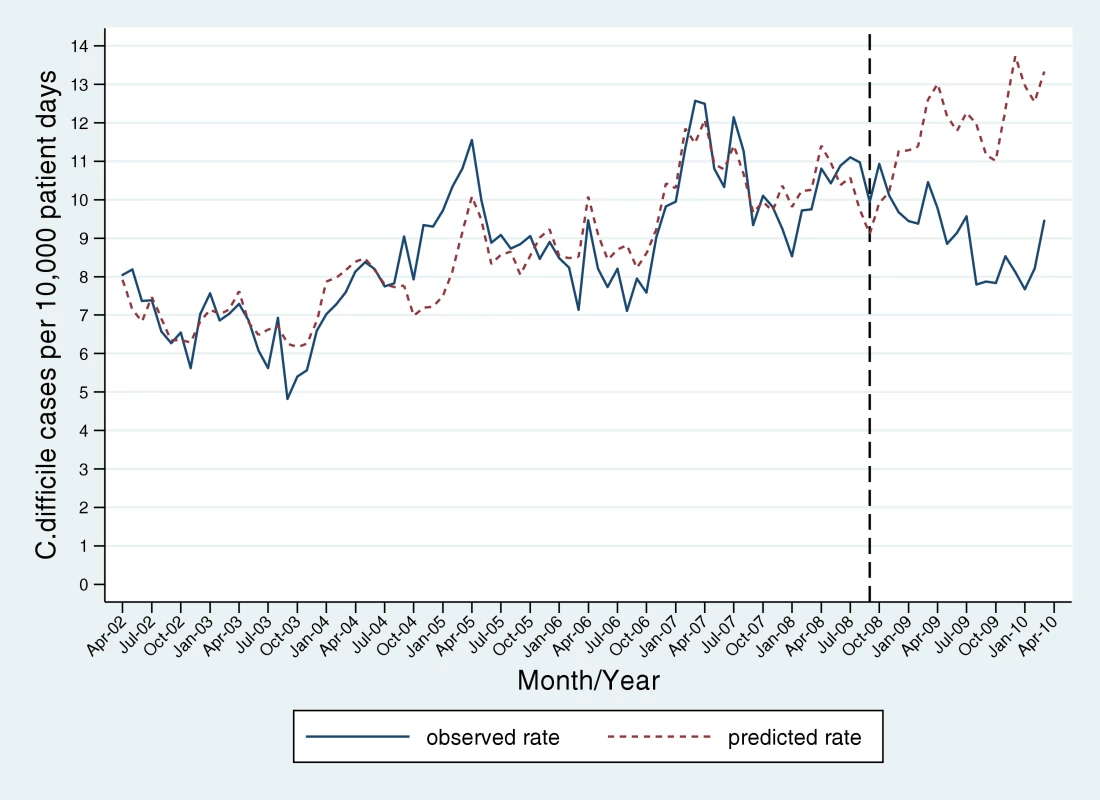
Observed monthly rates of C. difficile infection in Ontario (solid blue line) were generally increasing prior to the introduction of public reporting in September 2008 (identified by black dotted line), and declined after this intervention. Post-intervention rates were significantly lower than rates predicted by a Poisson model (red dashed line) derived from pre-intervention data points and adjusted for age and hospital strata, and overall burden of community antibiotic use (with 0- to 12-mo lags). Tab. 2. Cases of C. difficile averted by public reporting based on differences in observed and expected monthly case counts. 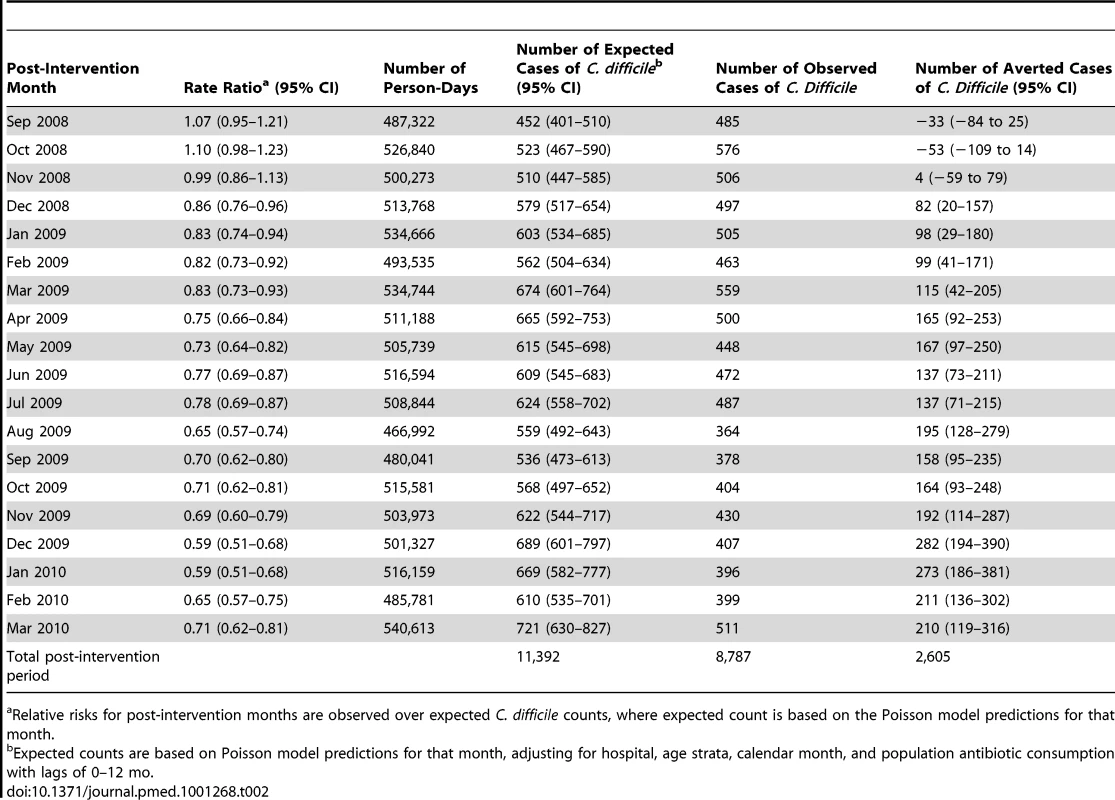
Relative risks for post-intervention months are observed over expected C. difficile counts, where expected count is based on the Poisson model predictions for that month. Tracer Outcomes Not Expected to Be Impacted by C. difficile Public Reporting
During the study period (April 1, 2002 to March 31, 2010) there were 6,545 hospital admissions for other leading bacterial gastrointestinal pathogens, corresponding to a rate of 0.87 per 1,000 hospital admissions, or 1.34 per 10,000 patient-days. The rate of these predominantly community-acquired infections did not change after the introduction of C. difficile public reporting (Figure 4A).
Fig. 4. Tracer analyses evaluating longitudinal time trends of infections not expected to be impacted by hospital public reporting of C. difficile infection rates. 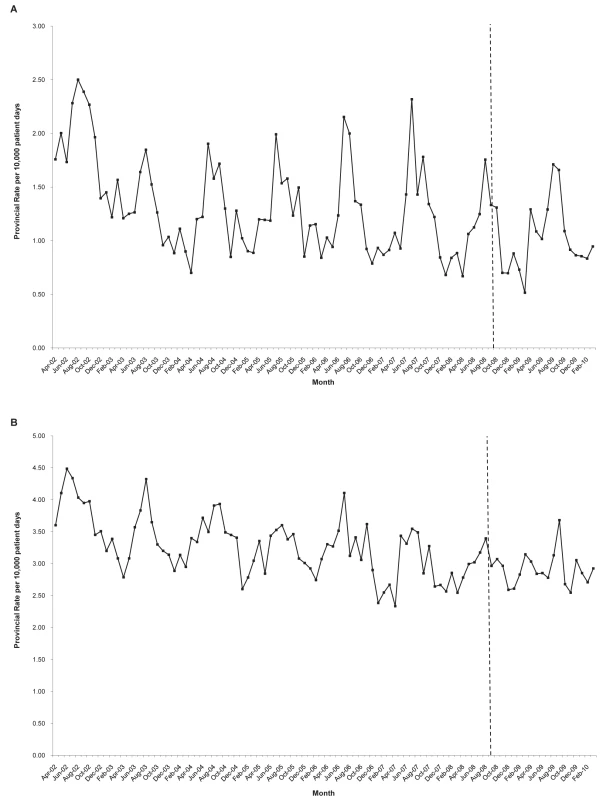
Neither community-acquired bacterial gastrointestinal infections (A) nor urinary tract infections (B) exhibited a change in incidence concurrent with the introduction of C. difficile infection public reporting in September 2008. There were 16,601 hospital admissions involving urinary tract infections, corresponding to a rate of 2.21 per 1,000 admissions, or 3.40 per 10,000 patient-days. Longitudinal trends in urinary tract infections did not change after the introduction of C. difficile public reporting (Figure 4B).
Discussion
This longitudinal population-based cohort study has confirmed an immense burden of C. difficile infection in Ontario, while heralding mandatory hospital reporting as one potential means to reduce this burden. C. difficile infections affected more than 6,000 patients per year in Ontario, were more than twice as common as all other bacterial gastrointestinal and urinary tract infections combined, and increased over the 6.5-y pre-intervention period. However, with the introduction of public reporting in September 2008, C. difficile infections declined by 26% across Ontario, resulting in over 1,900 cases averted per year.
A number of jurisdictions in the United States, Canada, and the United Kingdom have introduced mandatory public reporting of hospital-acquired infections, including C. difficile colitis, and some have reported reductions in rates [24],[25]. However, our study represents the first attempt, to our knowledge, to measure population-based rates in a dataset that is independent from the public reporting system. In fact, a prior systematic review identified no rigorous studies investigating changes in health care–associated infection as an outcome of public reporting [12]. Therefore, our findings provide important confirmation that public reporting can be associated with reductions in health care–associated infections on a broad scale.
Although we did not explore the mechanisms by which public reporting influenced C. difficile rates in this case, prior research suggests that the selection pathway (i.e., patients selecting higher performing institutions) is least likely to have impacted C. difficile rates in Ontario. A recent review suggests that the impact of public reports on consumers is related to the accessibility and ease of understanding the messages of the report [26]. However, in Ontario the reports are quite deeply buried on a MOHLTC website [27]. So, even though the universal health care system in Ontario does not constrain individuals from choosing their own providers and institutions, it is unlikely that these reports led to shifts in patient selection of hospitals. It is more likely that public reporting elevated C. difficile to greater prominence on hospital quality improvement agendas, and motivated hospitals to adhere more closely to best practices in C. difficile prevention. Such practices, ranging from patient isolation to environmental cleaning, are well described in general infectious diseases society guidelines [6], and analogous Ontario guidelines were distributed to all hospitals. No financial incentives or disincentives were initially linked to C. difficile public reporting in Ontario, but hospitals may have anticipated that at some future point high rates could influence hospital reimbursement, akin to the US Centers for Medicare & Medicaid Services' denial of hospital reimbursement for avoidable patient complications such as infection (termed “never events”) [28]. In fact, subsequent legislation in Ontario has now mandated that executive compensation be linked to achieving quality improvement targets, including for C. difficile rates, starting in 2012 [14].
This investigation confirmed prior findings that higher C. difficile rates are strongly associated with older patient age [1],[29], large community hospitals [30], and winter (respiratory virus) season [30],[31]. Although prior antibiotic exposure is widely recognized as a cause of C. difficile colitis for individual patients (by disrupting normal intestinal flora) [1],[32], we report a novel finding that population-level outpatient antimicrobial consumption is predictive of hospital C. difficile rates across a broad geographic region. Overall antibiotic prescription rates predicted C. difficile rates at lags of up to 9 mo. Seasonal increases in antibiotic use in winter appear to drive seasonal increases in C. difficile disease, and likely mediate the reported association between influenza and C. difficile seasonality [31]. Intriguingly, the apparent increases in C. difficile rates in Ontario between 2002 and 2008 are also potentially explained by corresponding increases in population antibiotic utilization. This finding provides strong support for the “antibiotic stewardship” movement, aimed at reducing unnecessary antibiotic use within institutional and community settings [33].
Although study strengths include a population-based assessment of a system-level intervention with no loss to follow-up, as an observational study using health administrative data our study has some limitations. Our study findings may be influenced by misclassification of C. difficile outcome status in the administrative databases. However, the accuracy of these diagnostic codes are supported by patient-level validation studies in other jurisdictions [17],[18], as well as our own hospital-level cross-validation with Ontario public reporting statistics. Without a prospective, randomized trial we cannot be certain that C. difficile rates in Ontario were not influenced by some other temporal confounder, such as changes in C. difficile strain prevalence or antibiotic stewardship practices unrelated to C. difficile public reporting. However, the causal inference is strengthened by the duration of our longitudinal cohort (crude rates were rising for 6.5 y and then dropped coinciding with the intervention), the inclusion of crucial predictors of C. difficile (age and antibiotic utilization), and the assessment of control infectious diseases. Although public reporting could prompt some hospitals to underestimate the proportion of cases that were nosocomial, these hospitals are not likely to have underestimated the overall number of cases, since these figures were not subject to public reporting, and because ignoring cases or reducing laboratory testing of C. difficile could potentially lead to increased transmission of infection and more dramatic outbreaks. Nevertheless, given the potential for “gaming” of reported rates, and the potential for more thorough reporting in higher performing institutions, we utilized a data source for hospital C. difficile rates that was independent of the public reporting system itself.
This study provides to our knowledge the first population-based, rigorous evaluation of a public reporting system for hospital-acquired infection using an independent data source. In doing so, it provides support for ongoing public reporting of hospital C. difficile rates as a means of reducing the large population burden of this preventable disease. Future research will be required to discern the direct mechanism by which C. difficile infection rates are reduced in response to public reporting.
Zdroje
1. KellyCPLaMontJT 2008 Clostridium difficile—more difficult than ever. N Engl J Med 359 1932 1940
2. McDonaldLCOwingsMJerniganDB 2006 Clostridium difficile infection in patients discharged from US short-stay hospitals, 1996–2003. Emerg Infect Dis 12 409 415
3. GravelDMillerMSimorATaylorGGardamM 2009 Health care-associated Clostridium difficile infection in adults admitted to acute care hospitals in Canada: a Canadian Nosocomial Infection Surveillance Program Study. Clin Infect Dis 48 568 576
4. PepinJValiquetteLCossetteB 2005 Mortality attributable to nosocomial Clostridium difficile-associated disease during an epidemic caused by a hypervirulent strain in Quebec. CMAJ 173 1037 1042
5. KwongJCCrowcroftNSCampitelliMRatnasingamSDanemanN 2010 Ontario burden of infectious diseases study Toronto Institute for Clinical Evaluative Sciences
6. DubberkeERGerdingDNClassenDAriasKMPodgornyK 2008 Strategies to prevent clostridium difficile infections in acute care hospitals. Infect Control Hosp Epidemiol 29 Suppl 1 S81 S92
7. FungCHLimYWMattkeSDambergCShekellePG 2008 Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med 148 111 123
8. HibbardJH 2008 What can we say about the impact of public reporting? Inconsistent execution yields variable results. Ann Intern Med 148 160 161
9. TuJVDonovanLRLeeDSWangJTAustinPC 2009 Effectiveness of public report cards for improving the quality of cardiac care: the EFFECT study: a randomized trial. JAMA 302 2330 2337
10. MarshallMNShekellePGLeathermanSBrookRH 2000 The public release of performance data: what do we expect to gain? A review of the evidence. JAMA 283 1866 1874
11. SchaufflerHHMordavskyJK 2001 Consumer reports in health care: do they make a difference? Annu Rev Public Health 22 69 89
12. McKibbenLFowlerGHoranTBrennanPJ 2006 Ensuring rational public reporting systems for health care-associated infections: systematic literature review and evaluation recommendations. Am J Infect Control 34 142 149
13. Ontario Hospital Association 2009 Public reporting of Clostridium difficile frequently asked questions Toronto Ontario Hospital Association
14. 2010 Excellent Care for All Act, 2010. Legislative Assembly of Ontario Bill 46. Available: http://www.ontla.on.ca/web/bills/bills_detail.do?locale=en&Intranet=&BillID=2326. Accessed 8 June 2012
15. National Ambulatory Care Reporting System 2007 CIHI data quality study of Ontario emergency department visits for 2004–2005—executive summary Ottawa Canadian Institute for Health Information
16. LevyARO'BrienBJSellorsCGrootendorstPWillisonD 2003 Coding accuracy of administrative drug claims in the Ontario Drug Benefit database. Can J Clin Pharmacol 10 67 71
17. DubberkeERReskeKAMcDonaldLCFraserVJ 2006 ICD-9 codes and surveillance for Clostridium difficile-associated disease. Emerg Infect Dis 12 1576 1579
18. ScheurerDBHicksLSCookEFSchnipperJL 2007 Accuracy of ICD-9 coding for Clostridium difficile infections: a retrospective cohort. Epidemiol Infect 135 1010 1013
19. DubberkeERButlerAMYokoeDSMayerJHotaB 2010 Multicenter study of surveillance for hospital-onset Clostridium difficile infection by the use of ICD-9-CM diagnosis codes. Infect Control Hosp Epidemiol 31 262 268
20. ZegerSLLiangKY 1986 Longitudinal data analysis for discrete and continuous outcomes. Biometrics 42 121 130
21. SchullMJStukelTAVermeulenMJZwarensteinMAlterDA 2007 Effect of widespread restrictions on the use of hospital services during an outbreak of severe acute respiratory syndrome. CMAJ 176 1827 1832
22. GilliganPHJandaJMKarmaliMAMillerJM 1992 Laboratory diagnosis of bacterial diarrhea. NolteFS Cumitech 12A: laboratory diagnosis of bacterial diarrhea Washington (District of Columbia) American Society of Microbiology
23. LoENicolleLClassenDAriasKMPodgornyK 2008 Strategies to prevent catheter-associated urinary tract infections in acute care hospitals. Infect Control Hosp Epidemiol 29 Suppl 1 S41 S50
24. Ministère de la Santé et Services Sociaux du Québec 2009 Surveillance, prevention et controle des infections nosocomiales Quebec City Ministère de la Santé et Services Sociaux du Québec
25. Health Protection Agency 2012 March 15 Quarterly epidemiological commentary: mandatory MRSA, MSSA and E.coli bacteraemia, and C. difficile infection data (up to October–December 2011) London Health Protection Agency
26. FaberMBoschMWollersheimHLeathermanSGrolR 2009 Public reporting in health care: how do consumers use quality-of-care information? A systematic review. Med Care 47 1 8
27. Ontario Ministry of Health and Long-Term Care 2010 Patient safety indicator reporting [database]. Available: http://patientsafetyontario.net/Reporting/en/searchselection.aspx. Accessed 18 June 2012
28. Centers for Medicare and Medicaid Services 2008 August 4 CMS improves patient safety for Medicare and Medicaid by addressing never events Baltimore Centers for Medicare and Medicaid Services
29. MillerMGravelDMulveyMTaylorGBoydD 2010 Health care-associated Clostridium difficile infection in Canada: patient age and infecting strain type are highly predictive of severe outcome and mortality. Clin Infect Dis 50 194 201
30. GilcaRHubertBFortinEGaulinCDionneM 2010 Epidemiological patterns and hospital characteristics associated with increased incidence of Clostridium difficile infection in Quebec, Canada, 1998–2006. Infect Control Hosp Epidemiol 31 939 947
31. PolgreenPMYangMBohnettLCCavanaughJE 2010 A time-series analysis of clostridium difficile and its seasonal association with influenza. Infect Control Hosp Epidemiol 31 382 387
32. PoutanenSMSimorAE 2004 Clostridium difficile-associated diarrhea in adults. CMAJ 171 51 58
33. DellitTHOwensRCMcGowanJEJrGerdingDNWeinsteinRA 2007 Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 44 159 177
Štítky
Interní lékařství
Článek Risk of Venous Thromboembolism in Patients with Cancer: A Systematic Review and Meta-AnalysisČlánek The Co-Management of Tuberculosis and Diabetes: Challenges and Opportunities in the Developing WorldČlánek Researching New Methods of Screening for Adverse Pregnancy Outcome: Lessons from Pre-eclampsiaČlánek HIV Treatment as Prevention: Models, Data, and Questions—Towards Evidence-Based Decision-MakingČlánek United States Private-Sector Physicians and Pharmaceutical Contract Research: A Qualitative Study
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2012 Číslo 7- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
-
Všechny články tohoto čísla
- HIV Treatment as Prevention: Issues in Economic Evaluation
- Risk of Venous Thromboembolism in Patients with Cancer: A Systematic Review and Meta-Analysis
- HIV Treatment as Prevention: Natural Experiments Highlight Limits of Antiretroviral Treatment as HIV Prevention
- HIV Treatment as Prevention: Optimising the Impact of Expanded HIV Treatment Programmes
- Reduction in Infection Rates after Mandatory Hospital Public Reporting: Findings from a Longitudinal Cohort Study in Canada
- Medical Device Regulation: Time to Improve Performance
- Averting an Impending Storm: Can We Reengineer Health Systems to Meet the Needs of Aging Populations?
- Thinking Forward: The Quicksand of Appeasing the Food Industry
- The Co-Management of Tuberculosis and Diabetes: Challenges and Opportunities in the Developing World
- Community Mobilization in Mumbai Slums to Improve Perinatal Care and Outcomes: A Cluster Randomized Controlled Trial
- Researching New Methods of Screening for Adverse Pregnancy Outcome: Lessons from Pre-eclampsia
- Social Entrepreneurship for Sexual Health (SESH): A New Approach for Enabling Delivery of Sexual Health Services among Most-at-Risk Populations
- Lessons from Agriculture for the Sustainable Management of Malaria Vectors
- HIV Treatment as Prevention: Modelling the Cost of Antiretroviral Treatment—State of the Art and Future Directions
- HIV Treatment as Prevention: Considerations in the Design, Conduct, and Analysis of Cluster Randomized Controlled Trials of Combination HIV Prevention
- Antiretroviral Therapy for Prevention of Tuberculosis in Adults with HIV: A Systematic Review and Meta-Analysis
- The Effectiveness of Emergency Obstetric Referral Interventions in Developing Country Settings: A Systematic Review
- Digital Humanitarianism: Collective Intelligence Emerging
- The Ethics of Switch/Simplify in Antiretroviral Trials: Non-Inferior or Just Inferior?
- “Big Food,” the Consumer Food Environment, Health, and the Policy Response in South Africa
- Plasma Phospholipid Fatty Acid Concentration and Incident Coronary Heart Disease in Men and Women: The EPIC-Norfolk Prospective Study
- HIV Treatment as Prevention: The Utility and Limitations of Ecological Observation
- How Does Medical Device Regulation Perform in the United States and the European Union? A Systematic Review
- HIV Treatment as Prevention: Models, Data, and Questions—Towards Evidence-Based Decision-Making
- Risk Factors for Death among Children Less than 5 Years Old Hospitalized with Diarrhea in Rural Western Kenya, 2005–2007: A Cohort Study
- United States Private-Sector Physicians and Pharmaceutical Contract Research: A Qualitative Study
- HIV Treatment as Prevention: Debate and Commentary—Will Early Infection Compromise Treatment-as-Prevention Strategies?
- HIV Treatment as Prevention: Principles of Good HIV Epidemiology Modelling for Public Health Decision-Making in All Modes of Prevention and Evaluation
- Effect of a Community-Based Nursing Intervention on Mortality in Chronically Ill Older Adults: A Randomized Controlled Trial
- Surveillance of Infection Severity: A Registry Study of Laboratory Diagnosed
- Consequences of Gestational Diabetes in an Urban Hospital in Viet Nam: A Prospective Cohort Study
- Integrating Mental Health and Development: A Case Study of the BasicNeeds Model in Nepal
- Treatment of Young Children with HIV Infection: Using Evidence to Inform Policymakers
- The Impact of Transnational “Big Food” Companies on the South: A View from Brazil
- HIV Treatment as Prevention: Systematic Comparison of Mathematical Models of the Potential Impact of Antiretroviral Therapy on HIV Incidence in South Africa
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- HIV Treatment as Prevention: Issues in Economic Evaluation
- HIV Treatment as Prevention: Modelling the Cost of Antiretroviral Treatment—State of the Art and Future Directions
- HIV Treatment as Prevention: The Utility and Limitations of Ecological Observation
- Consequences of Gestational Diabetes in an Urban Hospital in Viet Nam: A Prospective Cohort Study
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



