-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Health Aspects of the Pre-Departure Phase of Migration
article has not abstract
Published in the journal: . PLoS Med 8(5): e32767. doi:10.1371/journal.pmed.1001035
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001035Summary
article has not abstract
Summary Points
-
The local conditions and environment at the place of origin of migrants influences health during all phases of the migration process.
-
Pre-departure health characteristics are important drivers in health activities directed at migrants, such as immigration medical screening.
-
Some pre-departure health elements continue to affect migrant populations long after their arrival at their destination.
-
Improved understanding and management of pre-departure health determinants will support the development and delivery of migrant-relevant health services.
This is one article in a six-part PLoS Medicine series on Migration & Health.
Introduction
The flow of populations within and across international boundaries is an important element in today's globalized world. Recent estimates of migration patterns place the combined numbers of international migrants and internal migrants at nearly a billion people [1]. Although migrant populations are extremely diverse, the processes of migration include certain characteristics shared by all migrants. All migrants have a place of origin. Experiences and exposures at a place of origin can influence migrants' health throughout the process of mobility [2], which may include transition, temporary residence, and arrival at a destination. After arrival or settlement, some migrant cohorts may experience ongoing or return migrations that can also have health consequences. [3] As indicated in Table 1, rates of departure from origin countries are markedly different between global areas and countries, with rates in Europe, Latin America, and Oceania more than double those of Africa, Asia, and North America [4]. It is important to note, however, that even low rates of departure from highly populated countries of origin can produce large health impacts at destinations.
Tab. 1. General emigration rates for 89 destination countries (modified from reference <em class="ref">[4]</em>). ![General emigration rates for 89 destination countries (modified from reference <em class="ref">[4]</em>).](https://www.prolekare.cz/media/cache/resolve/media_object_image_small/media/image/53eed69bd27cfed3c59e02a216971a29.png)
In general, most migrants move to destination countries in the same region. A recent Organisation for Economic Co-operation and Development (OECD) analysis involving 89 reception countries [4] noted intra-regional emigration flows of 85% in Africa, 75% in Asia, 62% in Latin America, and 60% in Europe. Two other smaller patterns are observed, however, in situations where historical links (e.g., Latin America–Europe) to other regions exist, or where long-standing immigration settlement policies (e.g., Australia, Canada, United States) affect origin and destination dynamics. Global studies of emigration reveal a relative gender balance in aggregate migrant population. However, there are large differences at the continental, regional, and country level (see Figure 1). The same OECD database study indicates that women make up greater proportions of North American and European migrants, while they represent lower proportions of African migrants, especially those from North Africa.
Fig. 1. Origin of emigrants (15 years and older) residing in 89 destination countries in 2000. 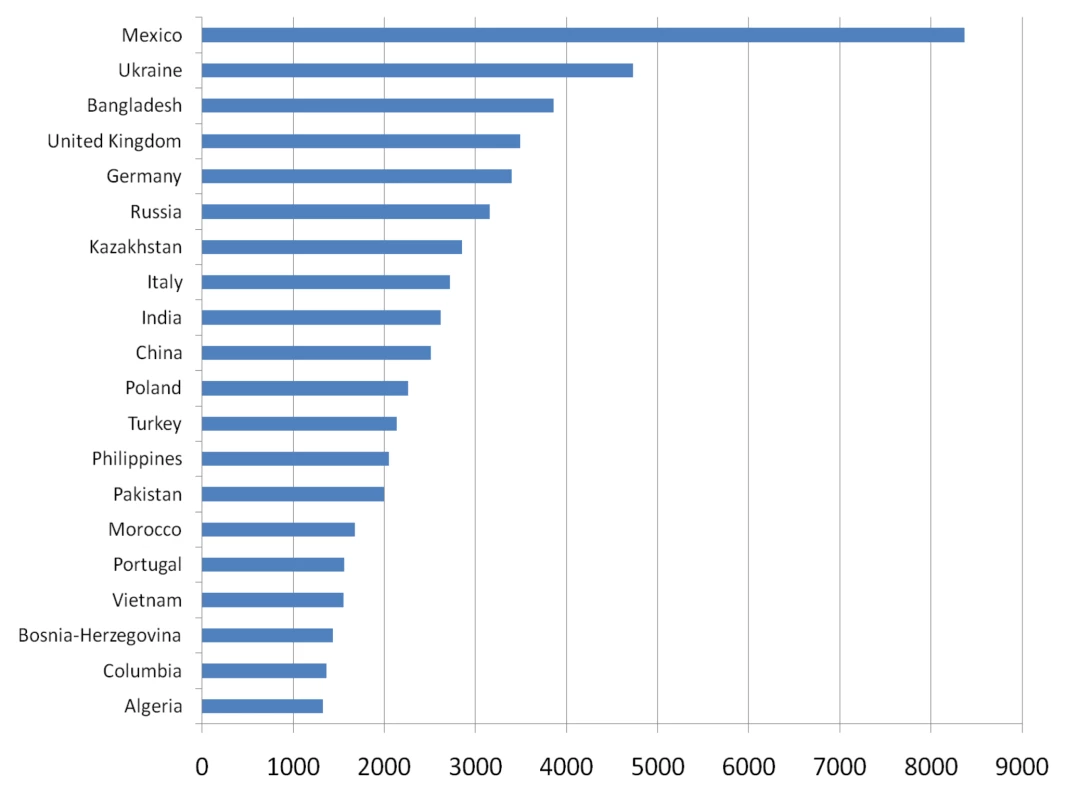
Modified from reference [4]. Migrant Health in the Context of the Pre-Migration Phase
The observation that one's origin, in terms of physical location and the determinants of health (socioeconomics, genetics and biology, behaviour, and environment), influences one's current and future response to events is widely appreciated across the spectrum of social and physical sciences [5]. In the context of migration and population mobility, the pre-departure phase can be considered as the beginning of the migration process and as such affects the rest of the migratory journey. The health characteristics of pre-departure migrant populations can be very diverse, reflecting disparities in the determinants of health at both individual and societal levels. The interaction between those pre-existing determinants of health and the forces that create migration affect many health outcomes in migrants.
Population mobility and migration are the result of a combination of “push” and “pull” factors that are inter-related and often mutually dependent. Descriptions of these factors and examples are provided in Table 2. For example, poverty and under-employment may “push” people to leave their place of residence to a destination that is at least perceived to offer wealth and job opportunities that “pull” migrants [6]. Similarly, environmental forces such as those resulting from natural disasters may generate “push” factors that force people to seek new homes. The combination of environmental and socioeconomic “push” factors such as floods or drought in areas of pre-existing areas of poverty can generate new directions in population flow. Those new patterns can be associated with different health impacts than pre-disaster migration movements. A recent example is provided by migration from Haiti where cholera, a post-2010 earthquake issue, may affect the health of potential migrants [7].
Tab. 2. Examples of determinants of health and mobility impacts. 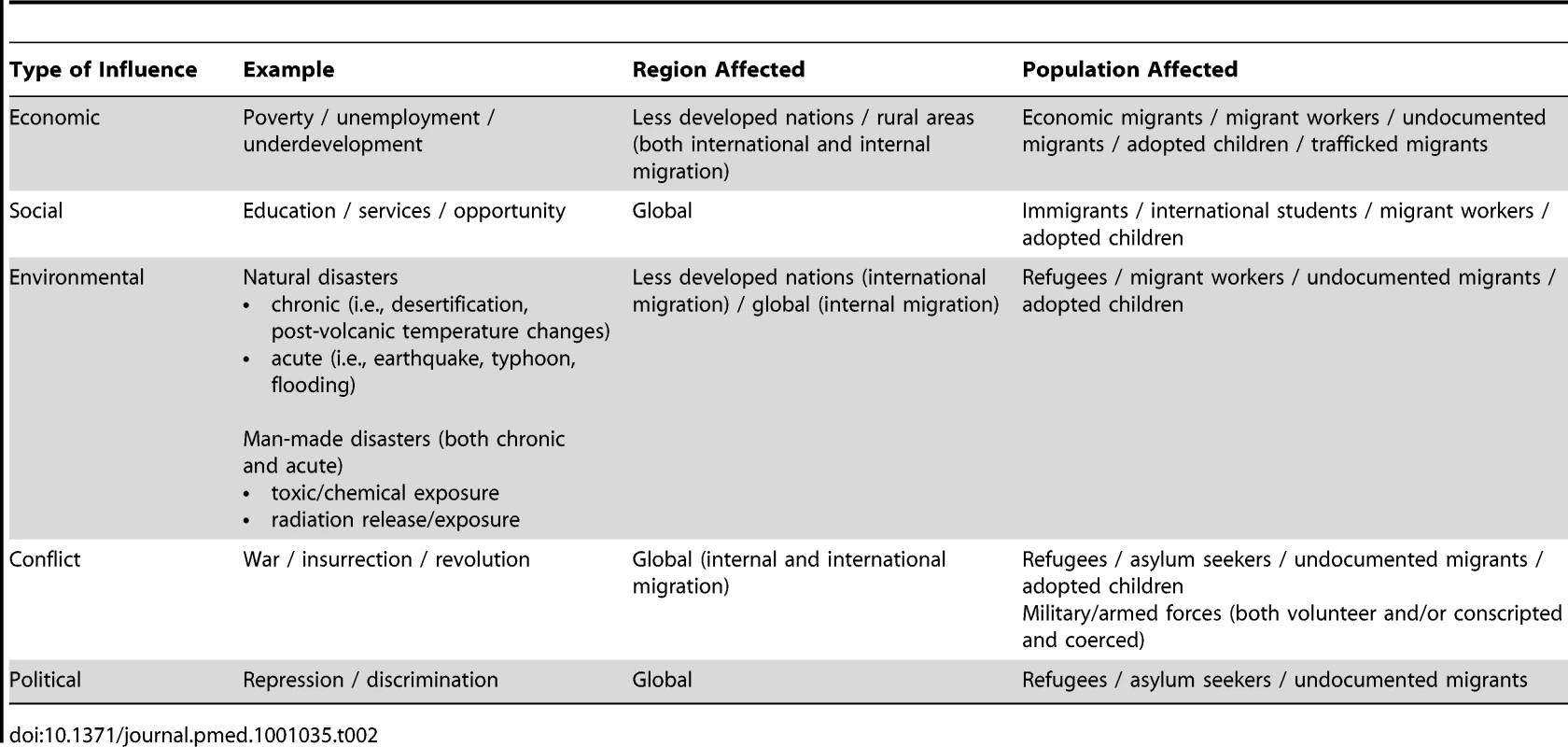
Factors Generating Migration Flows
These push and pull pressures are unequally distributed across pre-departure migrant populations, and together they both influence and affect migrant demography. An illustration is provided by comparing rural to urban migration and international migration from the same area. Rural to urban internal migration often represents the movement of workers, either with or without their families, from less affluent areas to metropolitan centers where jobs are perceived to be more plentiful. This broad pattern of migration has its own set of health issues and examples have been observed in several locations including child health in Africa, where death in those younger than 5 years old was greater for children of rural–urban migrants [8]. Other examples include the acquisition of less healthy determinants associated with urban living related to diet, activity, body weight, and access to preventive health services. Studies have noted increases in body mass index and diabetes in rural–urban migrants in India [9], increased cardiovascular risk factors in urban migrants in Latin America [10], and reduced rates of immunization in children of urban migrants [11].
Reflecting the diversity of population mobility, not all the effects of rural–urban migration are negative. For example, some studies have noted reduced rates of cardiovascular disease in non-migrant rural populations in South America compared to those in urban migrants in the same country [12]. At the same time, more affluent and educated cohorts from countries experiencing rural–urban migration move internationally as tourists, students, business travellers, and/or as permanent immigrants. For example, by the end of 2009, government estimates of rural migrant workers in China stood at 149 million [13]. Simultaneously, China is a major source of permanent immigrants and international students for nations such as Australia, Canada, the US, and Europe. Pre-migration health, social, and economic conditions will differ between each group even though they originate in the same country. The outcomes of the interaction between these push and pull factors can be important. Wealthy nations with relatively small domestic populations can provide work and residence to large numbers of migrant workers. Health characteristics and outcomes in migrants may differ from those of the domestic host population and may also impact the future health outcomes of the receiving nation.
Some migrants may be more vulnerable to adverse health outcomes. Refugees and displaced populations represent specific populations at risk [14]. In addition to their “normal” pre-migration state, their health status may have been compromised by lack of access to adequate nutrition, health care, public health programs such as routine childhood immunization, or housing during the process that made them refugees [15]. Those who are fleeing conflict may also be subject to violence and trauma, or abuse. The health characteristics of some vulnerable populations, such as permanently settled refugees, are often studied by receiving nations [16]. However, the permanently resettled (112,400 in 2009) represents only a fraction of global refugee and displaced populations (43,000,000 in 2009) [17]. The poor and those acutely displaced by catastrophe or conflict often have less access to, or support for, organized methods of migration and may turn to irregular patterns of population mobility such as illegal or illicit migration, or human smuggling and/or trafficking. By its nature irregular migration is very difficult to quantify, but crude estimates attest to its current and growing importance [18]. Attempting to enter other nations by irregular or illicit means is frequently associated with adverse health outcomes that include injury, exposure to harsh environments, violence, and death [19].
Health Outcomes in Relation to Pre-Departure Determinants
Pre-departure health status affects both individual and population health outcomes [20]. As described in Table 3, the magnitude of those influences is dependent upon the diversity (differences) and/or disparity (differences with a disadvantage) in the determinants of health and their outcomes between their new destination and those at the migrants' origin. People moving between regions of high endemicity for a disease can carry that epidemiology to low incidence, migrant-receiving nations [21]. Pre-departure differences in chronic disease epidemiology between migrant origin and destination locations can have long-term effects [22]. Over time and with sustained migration from high prevalence to low prevalence areas, migrants can come to represent specific disease risk groups in destination countries [23] for non-prevalent conditions such as tuberculosis [24], hepatitis B [25], strongliodaiasis [26], malaria [27], cystercercosis [28], South American trypanosomiasis [29], diabetes [30], renal failure [31], cardiovascular disease [32], and certain malignancies [33], among others.
Tab. 3. Pre-movement factors that influence health (modified from reference <em class="ref">[71]</em>). ![Pre-movement factors that influence health (modified from reference <em class="ref">[71]</em>).](https://www.prolekare.cz/media/cache/resolve/media_object_image_small/media/image/6e63caeaf58acf3e584e9ac94071de00.png)
Not all of the health concerns in migrants that are the consequences of geographically disparate disease epidemiology are related to infectious diseases. Health outcomes in migrants also include biological and inherited elements as well as those associated with ethnicity and social and cultural practices, as reflected in the selection of marriage partners [34]. Some genetic conditions, such as the hemoglobinopathies more common in the Levant and other areas [35], have post-immigration implications in locations where these genetic features had not evolved and were not normally distributed [36]. The introduction of sickle cell disease into the Americas [37] or the differences in malignancy incidence reflected in some migrant populations embedded in host environments [38] are examples of these impacts. Another example is provided by studies on the international movement of Helicobacter pylori [39], which has post-infection, chronic consequences, including malignancy.
Historically, there has been a tendency to consider only the adverse health risks related to migration, focusing on disease risks in migrant populations that were greater than the host population. It is important to note, however, that the consequential health outcomes for both the migrant and host population may be positive, neutral, or negative.
In several migration-receiving nations, cohorts of new arrivals often display health characteristics that are better than that those of similar cohorts of the domestic population. These observations are frequently related to lifestyle choices or chronic diseases (e.g., dietary choices, physical fitness, smoking, substance abuse) but extend to other situations (e.g., use of health services, fecundity and pregnancy outcomes). Described as the “healthy immigrant effect” [40], examples of this type are important in defining migrant factors that impact health outcomes.
Health and Health Service System Implications of the Pre-Departure Phase
Historically, the pre-departure influences affecting the health of migrants were approached in terms of the potential risks migrants were believed to pose to the domestic host population. Attempts to control the admission of epidemic diseases grew to include the medical screening of arriving migrants [41]. Practiced by nations with organized immigration selection programs, medical screening may be an element of a formal regulated process used to determine the eligibility of entry on health grounds [42]. Additional or supplemental screening is often recommended for clinical or public health benefit [43]. Screening is also a frequent component of organized migrant labor or temporary workers programs in Asia [44] and the Middle East [45].
The nature, purpose, and type of migrant medical screening for exclusion varies by nation from none at all to very detailed, proscriptive programs [46]. Those screening immigrant programs that do exist commonly include testing for communicable diseases of public health significance (e.g., tuberculosis and a small number of other infectious diseases); chronic diseases that may impact health or social services (e.g., cancer, heart disease, mental disability); or medical conditions deemed to be a social risk factor (substance abuse, mental disease). Screening of migrants may be enhanced or introduced in situations of international public health concern such as was observed in SARS [47], human infection with avian influenza, and the H1N1 (2009) influenza pandemic [48]. Screening for migrant labourers may include aspects of fitness for work.
Some nations with universal health insurance systems, such as Canada [49] and Australia [50], apply immigration screening to prevent the admission of some complex or costly diseases that could adversely affect the domestic supply of limited health services. Nations that screen migrants in terms of disease cost or service demand often waive these requirements for refugee or humanitarian migrant populations.
More recently, expanding the concept of immigration medical screening is being considered in terms of screening not for exclusion on health grounds [51], but as a tool to assess the public health fitness of the newly arriving migrant [52] and perhaps facilitate integration into the health systems at the migrants' destination. While these approaches are still being developed, some steps in this regard are being undertaken. Immunization against vaccine-preventable diseases may be required by some migrant-receiving nations [53], and special populations at risk such as refugees or adopted children may receive additional attention. Immigration screening in this context has the potential to become an integral component of public health promotion and prevention in migration receiving countries.
An additional pre-departure health element that exerts influence after a migrant's arrival is the approach to the use of health services. Models of health care delivery differ across the globe. Examples include ayurvedic and traditional Chinese medicine used by billions of individuals, which differs from Western allopathic medicine [54]. Migrants arriving from backgrounds where different medical models of care are used may use host country medical services differently [55],[56]. Those arriving from fee-for-service environments may be unaware or unfamiliar with the provision of nationally insured services, for example [57]. At the same time, fear of potential consequences, migrants' perceptions and attitudes, and provider competency may defer or delay migrants' use of medical services [58].
Policy Challenges Posed by Pre-Departure Health Factors
Migration health policies, when they exist, are frequently based on traditional considerations of immigration/emigration. Those frameworks often categorize mobile populations of increasingly diverse origin into a limited number of administratively determined immigrant categories. Health concerns in mobile populations have often been addressed in terms of traditional migrant classification (refugee, immigrant, temporary worker, visitor, etc.). While those categories may reflect historical migration flows, they are often not representative of modern migrant diversity or disparity, nor may they reflect the current reality of health differences relevant to receiving nations. An example is provided by the demographic, experiential, and personal differences present in current refugee populations. Depending on location and national practice, a wealthy, educated political refugee originating in a developed metropolitan area who filed an asylum claim versus an economically and educationally deprived laborer forced from his or her home into a refugee camp by conflict, could be administratively classified identically. Yet, their health status and needs may be significantly different.
Recommendations to consider health policies and programs for migrants in terms of the country of origin as a reference point rather than immigrant classification began in the 1980s [59]. More recently the need to expand the scope of migrant health policies to include additional parameters beyond the traditional administrative labels is also becoming better appreciated [60]. This increased appreciation of the health implications of modern migration includes national, bilateral and multilateral approaches to managing health disparities in some migrant populations. Some European nations that receive large numbers of migrants from less developed areas, including Spain and Italy, have extended municipal or national health insurance coverage for migrants [61]. In Canada, the federal government offers health coverage for refugees and refugee claimants until they qualify for provincial health insurance [62].
The repetitive, cyclic flow of migrants, such as migrant labor or migrants visiting friends and relatives in their place of origin, can create specific health challenges that exceed the capacities of traditional programs developed for uni-directional migration. Nations sharing common borders frequently crossed by migrants are developing joint projects to manage health issues in mobile populations. Examples include shared programs along the US–Mexican border that involve common health information systems and shared treatment and monitoring systems [63]. Other examples include guidelines for the assessment and management of health conditions in migrant travellers at specific risk, such at those who visit friends and relatives [64]. Globally and regionally integrated public health surveillance and monitoring of pre-departure health characteristics can provide early recognition of disease or illness in migrants and other mobile populations. Examples include surveillance and monitoring systems for tropical infections, such as TropNetEurop [65], and for travel-associated illnesses, such as GeoSentinel [66]. Through these multi-site systems, providers and laboratories report imported or travel-related diseases in an aggregated format that allows for the early identification and quantification of risks in mobile populations, including migrants. This information is used to support disease prevention activities and management activities and programs.
The cumulative implications of the pre-departure health status of migrants ultimately extend to the delivery of patient care at the destination. Cultural competency and the ability to deal with diversity are increasingly important aspects of health care in migrant-receiving locations [67]. Migrant-receiving destinations are increasingly faced with the need for linguistic and cultural services to reduce barriers to care posed by language and different cultural norms. These needs extend to the level of the clinical caregiver who, in an increasingly globalized world, requires greater awareness of pre-departure factors for migrant populations in order to accommodate specific migrant needs [68].
Conclusions
The determinants of health present during the pre-departure phase of migration are crucially important factors affecting the existing and future health outcomes of migrants and host populations. The effects of these factors extend throughout the remaining phases of the migratory process and apply at both the individual and population level. Appreciating and dealing with these issues at operational and policy levels requires global focus, rapid and flexible response to change, and current information on the composition and nature of the migrants themselves as opposed to traditional administrative migrant-classification - or disease-based paradigms. Increasingly, the challenges of dealing with migrant health are being addressed through collaborating centers of reference and experience [69],[70]. Bringing together multidisciplinary sectors that include providers, migrant communities, and educational institutions, these centers allow for the effective preparation of migrant-focused policies, programs, and services using shared knowledge, research, and resources. Collaboration of this type reduces duplication of activities, allows for the expedient extension of best practices, and supports comparative research.
Zdroje
1. UNDP 2009 Human development report 2009. Overcoming barriers: human mobility and development. United Nations Development Programme. Available: http://hdr.undp.org/en/media/HDR_2009_EN_Complete.pdf. Accessed 19 April 2011
2. MacPhersonDWGushulakBD 2001 Human mobility and population health. New approaches in a globalizing world. Perspect Biol Med 44 390 401
3. GushulakBDMacPhersonDW 2006 Migration medicine and health: principles and practice. BC Decker. Hamilton (ON)
4. DumontJ-CSpielvogelGWidmaierS 2010 International migrants in developed, emerging and developing countries: an extended profile. OECD Social, Employment and Migration Working Papers No. 114. Available: http://www.oecd.org/els/workingpapers. Accessed 19 April 2011
5. CurtisSSetiaMSQuesnel-ValleeA 2009 Socio-geographic mobility and health status: a longitudinal analysis using the National Population Health Survey of Canada. Soc Sci Med 69 1845 1853
6. TakenakaAPrenKA 2010 Leaving to get ahead: assessing the relationship between mobility and inequality in Peruvian migration. Lat Am Perspect 37 29 49
7. HarrisJBLarocqueRCCharlesRCMazumderRNKhanAIBardhanPK 2010 Cholera's western front. Lancet 376 1961 1965
8. AntaiDWedrénSBelloccoRMoradiT 2010 Migration and child health inequities in Nigeria: a multilevel analysis of contextual - and individual-level factors. Trop Med Int Health 15 1464 1474 doi:10.1111/j.1365-3156.2010.02643.x
9. EbrahimSKinraSBowenLAndersenEBen-ShlomoY 2010 Indian Migration Study group. The effect of rural-to-urban migration on obesity and diabetes in India: a cross-sectional study. PLoS Med 7 4 e1000268 doi:10.1371/journal.pmed.1000268
10. TorunBSteinADSchroederDGrajedaRConliskA 2002 Rural-to-urban migration and cardiovascular disease risk factors in young Guatemalan adults. Int J Epidemiol 31 218 226
11. KusumaYSKumariRPandavCSGuptaSK 2010 Migration and immunization: determinants of childhood immunization uptake among socioeconomically disadvantaged migrants in Delhi, India. Trop Med Int Health 15 1326 1332 doi:10.1111/j.1365-3156.2010.02628.x
12. ZamanMJde MolaCLGilmanRHSmeethLMirandaJJ 2010 The prevalence of angina symptoms and association with cardiovascular risk factors, among rural, urban and rural to urban migrant populations in Peru. BMC Cardiovasc Disord 10 50
13. National Bureau of Statistics of China 2010 National economy: recovery and posing in the good direction in 2009. January 21, 2010. Available: http://www.stats.gov.cn/was40/gjtjj_en_detail.jsp?searchword=ruralmigrantworkers&channelid=9528&record=1. Accessed 21 April 2011
14. StaufferWMWeinbergM 2009 Emerging clinical issues in refugees. Curr Opin Infect Dis 22 436 442
15. TooleMJWaldmanRJ 1997 The public health aspects of complex emergencies and refugee situations. Annu Rev Public Health 18 283 312
16. BensonJDonohueW 2007 Hepatitis in refugees who settle in Australia. Aust Fam Physician 36 719 727
17. UNHCR 2010 2009 global trends: refugees, asylum-seekers, returnees, internally displaced and stateless persons. June, 15 2010 Geneva UNHCR Available: http://www.unhcr.org/4c11f0be9.html. Accessed 18 April 2011
18. Danailova-TrainorGLaczkoF 2010 Trafficking in persons and development: towards greater policy coherence. Int Migr 48 38 83
19. GushulakBDMacPhersonDW 2000 Health issues associated with the smuggling and trafficking of migrants. J Immigr Health 2 67 78
20. ElliotPBestN 1998 Geographical patterns of disease. ArmitagePColtonT International encyclopaedia of biostatistics Chichester Wiley 1694 1701
21. SotoSM 2009 Human migration and infectious diseases. Clin Microbiol Infect 15 Suppl 1 26 28
22. GushulakBDMacPhersonDW 2006 The basic principles of migration health: population mobility and gaps in disease prevalence. Emerg Themes Epidemiol 3 3 Available: http://www.ete-online.com/content/3/1/3. Accessed 4 January 2011
23. NormanFFPérez de AyalaAPérez-MolinaJAMonge-MailloBZamarrónP 2010 Neglected tropical diseases outside the tropics. PLoS Negl Trop Dis 4 e762 doi:10.1371/journal.pntd.0000762
24. ArshadSBavanLGajariKPagetSNBaussanoI 2010 Active screening at entry for tuberculosis among new immigrants: a systematic review and meta-analysis. Eur Respir J 35 1336 1345
25. KimWR 2009 Epidemiology of hepatitis B in the United States. Hepatology 49 5 Suppl S28 S34
26. MarcosLATerashimaADupontHLGotuzzoE 2008 Strongyloides hyperinfection syndrome: an emerging global infectious disease. Trans R Soc Trop Med Hyg 102 314 318
27. NeavePEJonesCOBehrensRH 2010 A review of risk factors for imported malaria in the European African diaspora. J Travel Med 17 346 350 doi:10.1111/j.1708-8305.2010.00440.x
28. ImirizalduLMirandaLGarcía-GurtubayIGastónIUrrizaJQuesadaP 2004 [Neurocysticercosis. An emergent disease]. [Article in Spanish]. An Sist Sanit Navar 27 201 209
29. GasconJBernCPinazoMJ 2010 Chagas disease in Spain, the United States and other non-endemic countries. Acta Trop 115 22 27
30. CreatoreMIMoineddinRBoothGManuelDHDesMeulesM 2010 Age - and sex-related prevalence of diabetes mellitus among immigrants to Ontario, Canada. CMAJ 182 781 789
31. StewartJHMcCredieMRMcDonaldSP 2004 Incidence of end-stage renal disease in overseas-born, compared with Australian-born, non-indigenous Australians. Nephrology (Carlton) 9 247 252
32. BaineyKRJugduttBI 2009 Increased burden of coronary artery disease in South-Asians living in North America. Need for an aggressive management algorithm. Atherosclerosis 204 1 10
33. Garcés-PalacioICScarinciIC 2010 Factors associated with perceived susceptibility to cervical cancer among Latina immigrants in Alabama. Matern Child Health J E-pub ahead of print 29 December 2010. doi:10.1007/s10995-010-0737-x
34. RotimiCNJordeLB 2010 Ancestry and disease in the age of genomic medicine. N Engl J Med 363 1551 1558
35. HendersonSTimbsAMcCarthyJGallienneAVan MourikM 2009 Incidence of haemoglobinopathies in various populations - the impact of immigration. Clin Biochem 42 1745 1756
36. BainBJ 2009 Neonatal/newborn haemoglobinopathy screening in Europe and Africa. J Clin Pathol 62 53 56
37. JohnsonCS 1985 Landmark perspective. Sickle cell anemia. JAMA 254 1958 1963
38. ParkinDMKhlatM 1996 Studies of cancer in migrants: rationale and methodology. Eur J Cancer 32A 761 771
39. YamaokaY 2009 Helicobacter pylori typing as a tool for tracking human migration. Clin Microbiol Infect 15 829 834
40. McDonaldJTKennedyS 2004 Insights into the ‘healthy immigrant effect’: health status and health service use of immigrants to Canada. Soc Sci Med 59 1613 1627
41. YewE 1980 Medical inspection of immigrants at Ellis Island, 1891–1924. Bull N Y Acad Med 56 488 510
42. KeaneVPGushulakBD 2001 The medical assessment of migrants: current limitations and future potential. Int Migr 39 29 42
43. StaufferWMKamatDWalkerPF 2002 Screening of international immigrants, refugees, and adoptees. Prim Care 29 879 905
44. SrisupanantMWiwanitkitV 2008 Prevalence of hepatitis B seropositivity among Thai workers in screening program before going abroad. Ann Hepatol 7 389
45. AkhtarSMohammadHG 2008 Nonlinear pattern of pulmonary tuberculosis among migrants at entry in Kuwait: 1997–2006. BMC Public Health 8 264
46. CDC 2010 Introduction and background. Technical instructions for medical examination of aliens. Available: http://www.cdc.gov/immigrantrefugeehealth/exams/ti/panel/technical-instructions/panel-physicians/introduction-background.html. Accessed 18 April 2011
47. St JohnRKKingAde JongDBodie-CollinsMSquiresSG 2005 Border screening for SARS. Emerging Infect Dis 11 6 10
48. KrautAM 2010 Immigration, ethnicity, and the pandemic. Public Health Rep 125 Suppl 3 123 133
49. Citizenship and Immigration Canada 2009 Handbook for designated medical practitioners Ottawa Citizenship and Immigration Canada Available: http://www.cic.gc.ca/english/pdf/pub/dmp-handbook.pdf. Accessed 18 April 2011
50. Australian Department of Immigration and Citizenship 2011 Fact sheet 22–the health requirement. Available: http://www.immi.gov.au/media/fact-sheets/22health.htm Accessed 18 April 2011
51. MaloneyS 2005 Shifting the paradigm from exclusion to inclusion. Health and migration: bridging the gap. International dialog on migration #6. PP65–67 Geneva IOM Available: http://www.iom.int/jahia/webdav/site/myjahiasite/shared/shared/mainsite/published_docs/serial_publications/RedBook6_eng.pdf. Accessed 19 April 2011
52. GreenawayCDongierPBoivinJFTapieroBMillerM 2007 Susceptibility to measles, mumps, and rubella in newly arrived adult immigrants and refugees. Ann Intern Med 146 20 24
53. CDC 2011 2009 technical instructions for panel physicians for vaccinations. Available: http://www.cdc.gov/immigrantrefugeehealth/exams/ti/panel/vaccination-panel-technical-instructions.html. Accessed 19 April 2011
54. PatwardhanBWarudeDPushpangadanPBhattN 2005 Ayurveda and traditional Chinese medicine: a comparative overview. Evid Based Complement Alternat Med 2 465 473
55. NgEWilkinsRGendronFBerthelotJ-M 2005 Dynamics of immigrants' health in Canada: Evidence from the National Population Health Survey Ottawa Statistics Canada Available: http://www.statcan.ca/english/research/82-618-MIE/82-618-MIE2005002.htm. Accessed 19 April 2011
56. ChiuT 2003 Logitudinal survey of immigrants to Canada: process, progress and prospects. Document 89-611-XIE Ottawa Statistics Canada
57. HargreavesSHolmesAHSaxenaSLe FeuvrePFarahW 2008 Charging systems for migrants in primary care: the experiences of family doctors in a high-migrant area of London. J Travel Med 15 13 18
58. ScheppersEvan DongenEDekkerJGeertzenJDekkerJ 2006 Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract 23 325 348 doi:10.1093/fampra/cmi113
59. CollegeM 1986 Migration and health. Report of a WHO consultation in The Hague, 1983 Geneva WHO
60. LassetterJHCallisterLC 2009 The impact of migration on the health of voluntary migrants in western societies. J Transcult Nurs 20 93 104
61. PadillaBPortugalRInglebyDDe FreitasCLebasJ 2009 Good practices on health and migration in the EU. Health and migration in the European Union: better health for all in an inclusive society Lisbon Instituto Nacional de Saude Doutor Ricardo Jorge
62. Citizenship and Immigration Canada 2011 Resettlement from outside Canada: arriving—health care. Available: http://www.cic.gc.ca/english/refugees/outside/arriving-healthcare.asp. Accessed 19 April 2011
63. United States–Mexico Border Health Commission 2011 United States–Mexico Border Health Commission Web site. Available: http://www.borderhealth.org/. Accessed 18 April 2011
64. BarnettEDMacPhersonDWStaufferWMLoutanLHatzCF 2010 The visiting friends or relatives traveler in the 21st century: time for a new definition. J Travel Med 7 163 170
65. European Network on Imported Infectious Disease Surveillance (TropNetEurop) 2011 About TropNetEurop. Available: http://www.tropnet.net/about/about_index.html. Accessed 18 April 2011
66. ISTM, CDC 2011 GeoSentinel. Available: http://www.istm.org/geosentinel/objectiv.html. Accessed 18 April 2011
67. OhmansPGarrettCTreichelC 1996 Cultural barriers to health care for refugees and immigrants. Providers' perceptions. Minn Med 79 26 30
68. WalkerPF 2010 Practising medicine in the global village: use of guidelines and virtual networks. CMAJ E-pub ahead of print 7 June 2010. doi:10.1503/cmaj.100625
69. Consortium on Health and Mobility 2011 Consortium on Health and Mobility. Available: http://healthandmobility.org/Health_and_Mobility/Welcome.html. Accessed 18 April 2011
70. UK Health Protection Agency 2011 HPA migrant health guide. Available: http://www.hpa.org.uk/migranthealthguide. Accessed 19 April 2011
71. GushulakBDMacPhersonDW 2004 Population mobility and health: an overview of the relationships between movement and population health. J Travel Med 11 171 178
Štítky
Interní lékařství
Článek The Transit Phase of Migration: Circulation of Malaria and Its Multidrug-Resistant Forms in AfricaČlánek If You Could Only Choose Five Psychotropic Medicines: Updating the Interagency Emergency Health Kit
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2011 Číslo 5- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Antikoagulační léčba u pacientů před operačními výkony
-
Všechny články tohoto čísla
- Primary Prevention of Gestational Diabetes Mellitus and Large-for-Gestational-Age Newborns by Lifestyle Counseling: A Cluster-Randomized Controlled Trial
- Meta-analyses of Adverse Effects Data Derived from Randomised Controlled Trials as Compared to Observational Studies: Methodological Overview
- Effectiveness of Early Antiretroviral Therapy Initiation to Improve Survival among HIV-Infected Adults with Tuberculosis: A Retrospective Cohort Study
- Characterizing the Epidemiology of the 2009 Influenza A/H1N1 Pandemic in Mexico
- The Joint Action and Learning Initiative: Towards a Global Agreement on National and Global Responsibilities for Health
- Let's Be Straight Up about the Alcohol Industry
- Advancing Cervical Cancer Prevention Initiatives in Resource-Constrained Settings: Insights from the Cervical Cancer Prevention Program in Zambia
- The Transit Phase of Migration: Circulation of Malaria and Its Multidrug-Resistant Forms in Africa
- Health Aspects of the Pre-Departure Phase of Migration
- Aripiprazole in the Maintenance Treatment of Bipolar Disorder: A Critical Review of the Evidence and Its Dissemination into the Scientific Literature
- Threshold Haemoglobin Levels and the Prognosis of Stable Coronary Disease: Two New Cohorts and a Systematic Review and Meta-Analysis
- If You Could Only Choose Five Psychotropic Medicines: Updating the Interagency Emergency Health Kit
- Migration and Health: A Framework for 21st Century Policy-Making
- Maternal Influenza Immunization and Reduced Likelihood of Prematurity and Small for Gestational Age Births: A Retrospective Cohort Study
- The Impact of Retail-Sector Delivery of Artemether–Lumefantrine on Malaria Treatment of Children under Five in Kenya: A Cluster Randomized Controlled Trial
- Medical Students' Exposure to and Attitudes about the Pharmaceutical Industry: A Systematic Review
- Estimates of Outcomes Up to Ten Years after Stroke: Analysis from the Prospective South London Stroke Register
- Low-Dose Adrenaline, Promethazine, and Hydrocortisone in the Prevention of Acute Adverse Reactions to Antivenom following Snakebite: A Randomised, Double-Blind, Placebo-Controlled Trial
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Low-Dose Adrenaline, Promethazine, and Hydrocortisone in the Prevention of Acute Adverse Reactions to Antivenom following Snakebite: A Randomised, Double-Blind, Placebo-Controlled Trial
- Effectiveness of Early Antiretroviral Therapy Initiation to Improve Survival among HIV-Infected Adults with Tuberculosis: A Retrospective Cohort Study
- Medical Students' Exposure to and Attitudes about the Pharmaceutical Industry: A Systematic Review
- Estimates of Outcomes Up to Ten Years after Stroke: Analysis from the Prospective South London Stroke Register
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



