-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Intimate Partner Violence and Population Mental Health: Why Poverty and Gender Inequities Matter
article has not abstract
Published in the journal: . PLoS Med 10(5): e32767. doi:10.1371/journal.pmed.1001440
Category: Perspective
doi: https://doi.org/10.1371/journal.pmed.1001440Summary
article has not abstract
Linked Research Article
This Perspective discusses the following new study published in PLOS Medicine:
Devries KM, Mak J, Bacchus L, Child J, Falder G, et al. (2013) Intimate Partner Violence and Incident Depressive Symptoms and Suicide Attempts: A Systematic Review of Longitudinal Studies. PLoS Med 10(5): e1001439. doi:10.1371/journal.pmed.1001439
Karen Devries and colleagues conduct a systematic review of longitudinal studies to evaluate the direction of association between symptoms of depression and intimate partner violence.
Steven Pinker [1] suggests that the world is becoming less violent. Yet, although it has been nearly two decades since the United Nations issued its Declaration on the Elimination of Violence against Women, the global burden of violence against women still remains alarmingly high [2]. Violence commonly results in physical injury, and other serious physical or psychological sequelae may also result, compounding its contribution to the overall global burden of disease [3]. The systematic review and meta-analysis by Karen Devries and colleagues [4] in this week's PLOS Medicine brings us one step closer toward understanding the mental health liabilities associated with violence against women. The public health impact of their contribution is substantial, given the lack of resources devoted to the prevention and treatment of mental disorders worldwide [5],[6],[7].
Their article is not the first to summarize the impacts of various forms of violence and abuse against women on mental health [8],[9],[10] (Table 1). Karen Devries and colleagues [4] contribute to this body of literature reviews by restricting their focus to longitudinal studies, thereby examining the temporal relationship between intimate partner violence and depression. Although the literature contained few studies examining the impacts of violence on incident depressive disorders, the authors identified enough studies to support a conclusion that violence was associated with incident symptoms of depression. They had intended to also examine the association between victimization and depression among men, but lack of data limited their ability to draw firm conclusions.
Tab. 1. Peer-reviewed journal articles summarizing the literature on intimate partner violence and mental health. 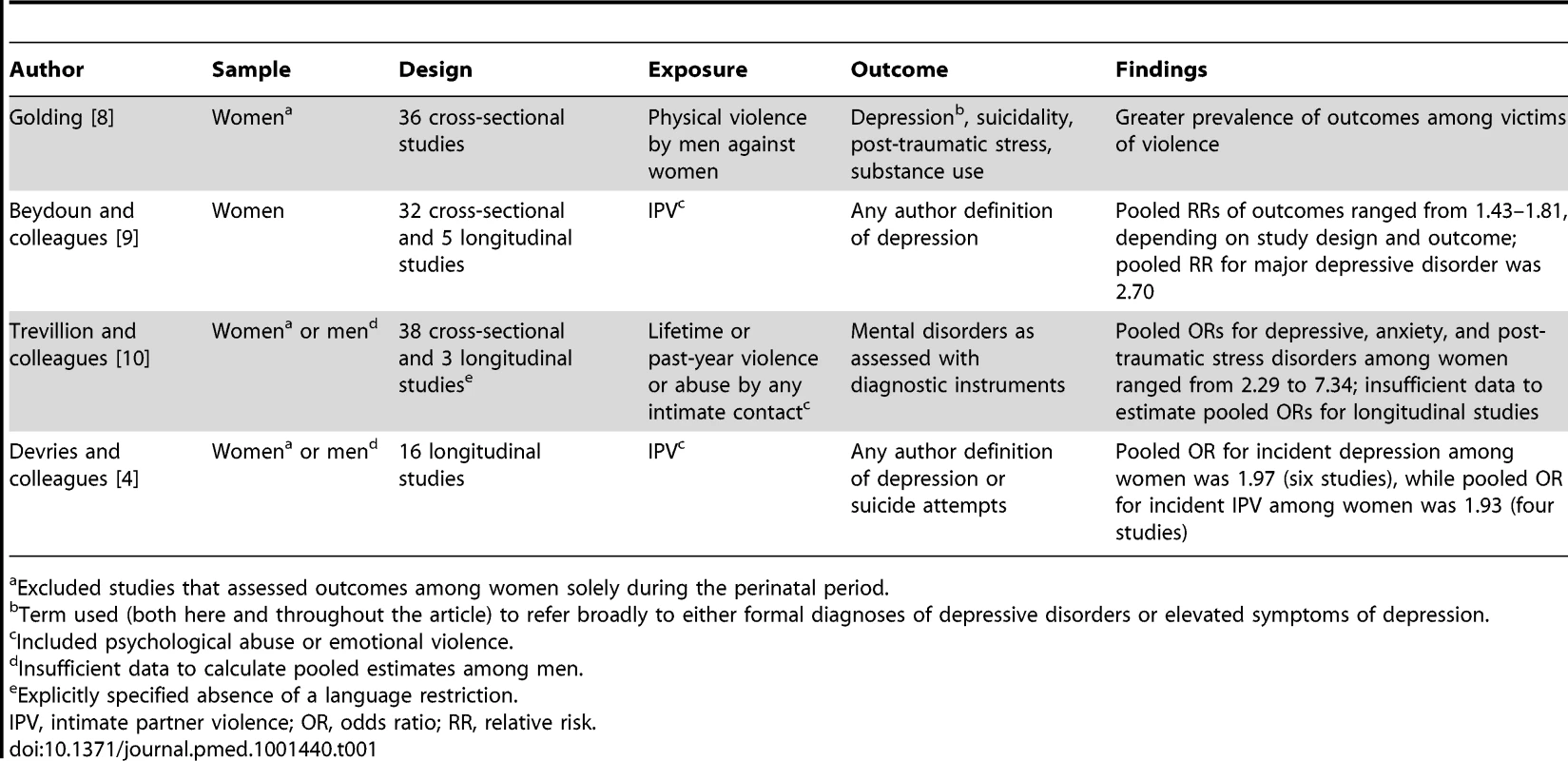
Excluded studies that assessed outcomes among women solely during the perinatal period. Notably, Karen Devries and colleagues [4] also found that, among women, symptoms of depression were associated with incident experiences of violence. Whether the relationship between violence and depression is truly causal in both directions is unknown. For example, in examining the association between exposure to intimate partner violence during adulthood and incident symptoms of depression, an unmeasured confounder preceding both variables such as childhood abuse—not measured in most of the studies—could be causally related to both irrespective of their temporal relationship with each other, inducing a spurious association that could be mistakenly interpreted as bidirectional. Statistical adjustment for baseline depression symptom severity, which was done in most of the studies, could potentially help with this problem if it is a key pathway through which the confounding effects of childhood abuse are transmitted.
So what do these findings suggest for clinical practice, programming, or policies to prevent violence against women? If depression is causally related to violence, one might consider evidence-based collaborative care management of depression [11],[12] in order to prevent subsequent experiences of violence. If violence is causally related to depression, one might suggest counseling interventions for women with histories of partner abuse in order to prevent subsequent episodes of depression, but high-quality randomized controlled trials have shown mixed results [13],[14],[15],[16]. The only randomized trial of universal screening for intimate partner violence yielded null findings [17]. It is possible that screening may exert substantive benefits only in settings where providers also have the ability to refer their clients to a broad array of services (e.g., case management, crisis services, legal advocacy, emergency shelters, transitional housing, and/or parenting and childcare support) [18], but the effectiveness of such a multipronged approach is as of yet unknown.
This particular gap in the literature redirects our attention to more systemic determinants of the excess burden of violence and depression among women. The simplified conceptual model depicted in Figure 1, informed in part by previously published work [19],[20], suggests not only that violence against women is a consequence of gendered norms about the use violence against intimate partners and power relations [21],[22], but also that its direct and indirect effects serve to reproduce these norms and power relations 23,24,25. The extent to which exposure to violence results in poor mental health outcomes is modified by gendered norms governing how men and women safely negotiate situations of potential danger [26],[27] as well as by biological differences in physical strength. And finally, poverty offers a hospitable environment for gender-unequal norms [28], violence against women [22],[29],[30], and psychological distress [31],[32] to thrive.
Fig. 1. Conceptual framework depicting connections between intimate partner violence and mental health, in the context of poverty, gender relations, and biological differences between men and women. 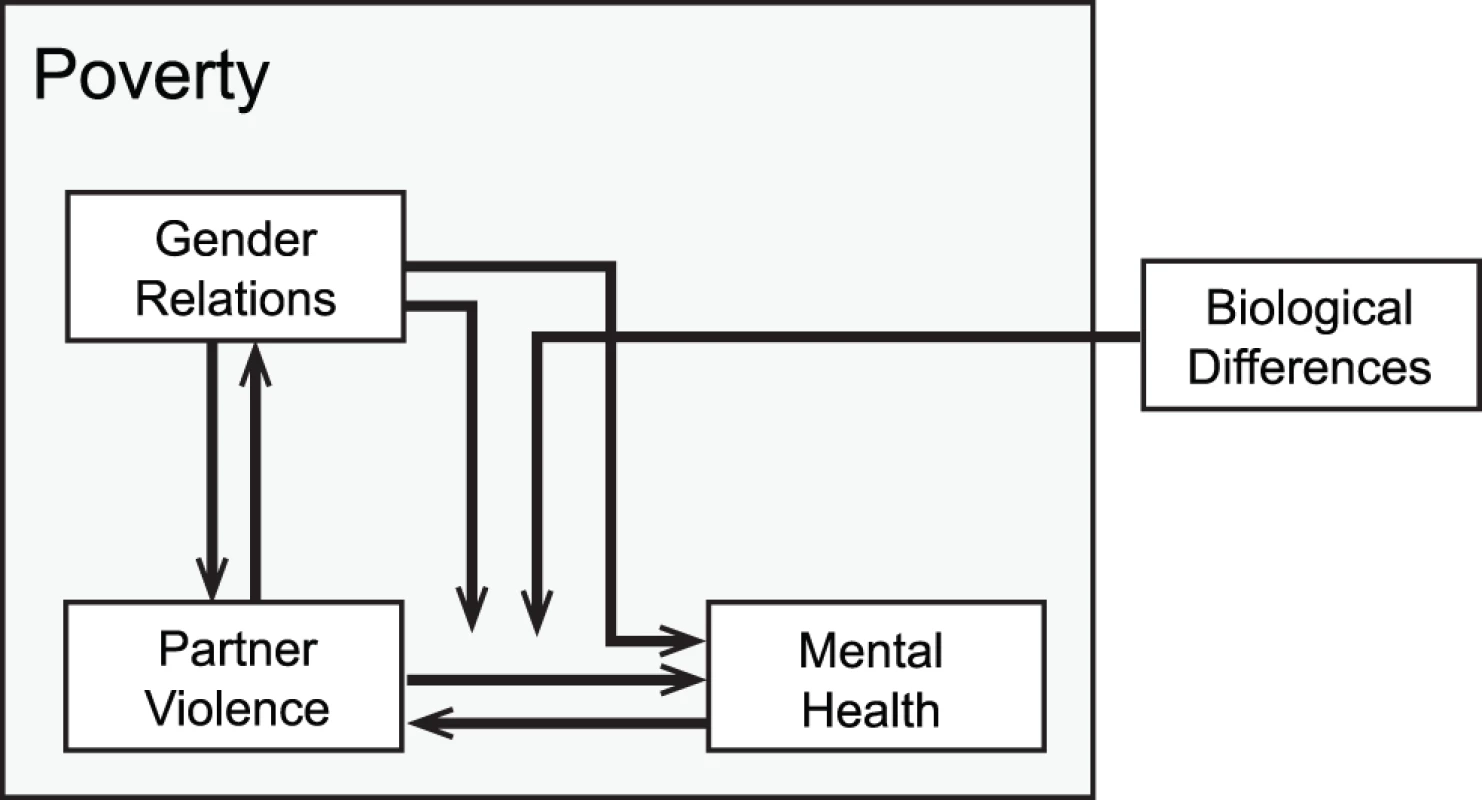
A reduced form of this model might not be obtainable, but at the very least this model suggests that: (a) violence against women may have direct adverse effects on mental health, as suggested by Karen Devries and colleagues [4]; and, simultaneously, (b) both violence and depression are partly rooted in gender-unequal relations and the unremitting strain of poverty. Meeting this formidable challenge will require complex interventions operating at multiple levels [33],[34]. As the epidemiologist Geoffrey Rose succinctly stated in his now-classic work, “Mass diseases and mass exposures require mass remedies” [35] (p.129). Rose argued that interventions aimed at shifting the entire distribution of disease (rather than interventions aimed at preventing disease in “high-risk” individuals) would yield substantive benefits for population health even if they carry little benefit for a given individual [36],[37]. This approach emphasizes the societal changes needed to curtail the production and unequal distribution of violence against women.
With regard to the conceptual model depicted in Figure 1, effective structural interventions would target the conditions that shape women's risks for these co-occurring problems. For example, in one randomized controlled trial conducted in rural South Africa, partnered women who took part in a microfinance intervention experienced a statistically significant decline in intimate partner violence [38]. While the intervention might be considered an “agentic” type of structural intervention that targets individual behavior change [39],[40], it is plausible that participation led to environmental changes on a micro scale, such as improvements in women's bargaining power vis-à-vis their intimate partners. Thus the findings of that study [38] hint at the possibilities for change on a macro scale. Consistent with their findings, an analysis of macroeconomic data from the US showed that changes in labor market conditions favoring women led to reductions in domestic violence [41]. Related work in India showed that a policy change increasing the number of women in political leadership positions had the effect of weakening stereotypes about gender roles [42] and raising parental aspirations for their daughters' educational attainment [43].
It would be imprudent to suggest that Rose's “high-risk” strategy [37] has no place in violence prevention. The review by Karen Devries and colleagues [4] reveals major gaps in research on intimate partner violence and depression, including lack of adjustment for childhood sexual abuse or other trauma. A life course perspective, which is missing from much of the research on determinants of violence in general [44],[45], would greatly enrich the field by helping intervention programs better address histories of child abuse and/or family violence in identifying targets for secondary prevention. As we continue to advance the science of developing and testing structural interventions, we should remain vigilant for potential synergies to emerge. Quite likely, the most effective approaches will involve interventions targeting high-risk individuals, complemented with population-based approaches focused on shifting the entire frequency distribution. At this time, the effectiveness of such a combination approach may be speculative. What is clear is that we cannot sit idly by while awaiting Pinker [1]'s long arc of history to avert the persistent psychological scars of violence.
Zdroje
1. Pinker S (2011) The better angels of our nature: why violence has declined. New York: Viking Penguin.
2. LimSS, VosT, FlaxmanAD, DanaeiG, ShibuyaK, et al. (2013) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 : 2224–2260.
3. ResnickHS, AciernoR, KilpatrickDG (1997) Health impact of interpersonal violence. 2: Medical and mental health outcomes. Behav Med 23 : 65–78.
4. DevriesK, MakJ, BacchusLJ, ChildJC, FalderG, et al. (2013) Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med 10: e1001439 doi:10.1371/journal.pmed.1001439.
5. TomlinsonM, RudanI, SaxenaS, SwartzL, TsaiAC, et al. (2009) Setting priorities for global mental health research. Bull World Health Organ 87 : 438–446.
6. TomlinsonM, LundC (2012) Why does mental health not get the attention it deserves? An application of the Shiffman and Smith framework. PLoS Med 9: e1001178 doi:10.1371/journal.pmed.1001178.
7. SaxenaS, ThornicroftG, KnappM, WhitefordH (2007) Resources for mental health: scarcity, inequity, and inefficiency. Lancet 370 : 878–889.
8. GoldingJM (1999) Intimate partner violence as a risk factor for mental disorders: a meta-analysis. J Fam Viol 14 : 99–132.
9. BeydounHA, BeydounMA, KaufmanJS, LoB, ZondermanAB (2012) Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: a systematic review and meta-analysis. Soc Sci Med 75 : 959–975.
10. TrevillionK, OramS, FederG, HowardLM (2012) Experiences of domestic violence and mental disorders: a systematic review and meta-analysis. PLoS One 7: e51740.
11. GilbodyS, BowerP, FletcherJ, RichardsD, SuttonAJ (2006) Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med 166 : 2314–2321.
12. TsaiAC, MortonSC, MangioneCM, KeelerEB (2005) A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care 11 : 478–488.
13. KielyM, El-MohandesAA, El-KhorazatyMN, BlakeSM, GantzMG (2010) An integrated intervention to reduce intimate partner violence in pregnancy: a randomized controlled trial. Obstet Gynecol 115 : 273–283.
14. El-MohandesAA, KielyM, JosephJG, SubramanianS, JohnsonAA, et al. (2008) An intervention to improve postpartum outcomes in African-American mothers: a randomized controlled trial. Obstet Gynecol 112 : 611–620.
15. TaftAJ, SmallR, HegartyKL, WatsonLF, GoldL, et al. (2011) Mothers' AdvocateS In the Community (MOSAIC)–non-professional mentor support to reduce intimate partner violence and depression in mothers: a cluster randomised trial in primary care. BMC Public Health 11 : 178.
16. TiwariA, FongDY, YuenKH, YukH, PangP, et al. (2010) Effect of an advocacy intervention on mental health in Chinese women survivors of intimate partner violence: a randomized controlled trial. JAMA 304 : 536–543.
17. MacMillanHL, WathenCN, JamiesonE, BoyleMH, ShannonHS, et al. (2009) Screening for intimate partner violence in health care settings: a randomized trial. JAMA 302 : 493–501.
18. SpangaroJ, ZwiAB, PoulosR (2009) The elusive search for definitive evidence on routine screening for intimate partner violence. Trauma Violence Abuse 10 : 55–68.
19. KriegerN (2003) Genders, sexes, and health: what are the connections–and why does it matter? Int J Epidemiol 32 : 652–657.
20. JewkesR (2002) Intimate partner violence: causes and prevention. Lancet 359 : 1423–1429.
21. ShannonK, LeiterK, PhaladzeN, HlanzeZ, TsaiAC, et al. (2012) Gender inequity norms are associated with increased male-perpetrated rape and sexual risks for HIV infection in Botswana and Swaziland. PLoS One 7: e28739.
22. Bourgois P (1996) In search of respect: selling crack in El Barrio. 1st ed. Cambridge: Cambridge University Press.
23. TsaiAC, SubramanianSV (2012) Proximate context of gender-unequal norms and women's HIV risk in sub-Saharan Africa. AIDS 26 : 381–386.
24. HungKJ, ScottJ, RicciottiHA, JohnsonTR, TsaiAC (2012) Community-level and individual-level influences of intimate partner violence on birth spacing in sub-saharan Africa. Obstet Gynecol 119 : 975–982.
25. PallittoCC, O'CampoP (2005) Community level effects of gender inequality on intimate partner violence and unintended pregnancy in Colombia: testing the feminist perspective. Soc Sci Med 60 : 2205–2216.
26. Connell RW (1987) Gender and power. Palo Alto: Stanford University Press.
27. BlancAK (2001) The effect of power in sexual relationships on sexual and reproductive health: an examination of the evidence. Stud Fam Plann 32 : 189–213.
28. UthmanOA, MoradiT, LawokoS (2009) The independent contribution of individual-, neighbourhood-, and country-level socioeconomic position on attitudes towards intimate partner violence against women in sub-Saharan Africa: a multilevel model of direct and moderating effects. Soc Sci Med 68 : 1801–1809.
29. TsaiAC, LeiterK, WolfeWR, HeislerM, ShannonK, et al. (2011) Prevalence and correlates of forced sex perpetration and victimization in Botswana and Swaziland. Am J Pub Health 101 : 1068–1074.
30. CunradiCB, CaetanoR, ClarkC, SchaferJ (2000) Neighborhood poverty as a predictor of intimate partner violence among White, Black, and Hispanic couples in the United States: a multilevel analysis. Ann Epidemiol 10 : 297–308.
31. LundC, BreenA, FlisherAJ, KakumaR, CorrigallJ, et al. (2010) Poverty and common mental disorders in low and middle income countries: A systematic review. Soc Sci Med 71 : 517–528.
32. RileyED, MooreK, SorensenJL, TulskyJP, BangsbergDR, et al. (2011) Basic subsistence needs and overall health among human immunodeficiency virus-infected homeless and unstably housed women. Am J Epidemiol 174 : 515–522.
33. KriegerN (2008) Proximal, distal, and the politics of causation: what's level got to do with it? Am J Public Health 98 : 221–230.
34. KriegerN (1994) Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med 39 : 887–903.
35. Rose G (2008) Rose's strategy of preventive medicine. New York: Oxford University Press, Inc.
36. RoseG (1985) Sick individuals and sick populations. Int J Epidemiol 14 : 32–38.
37. RoseG (1981) Strategy of prevention: lessons from cardiovascular disease. Br Med J (Clin Res Ed) 282 : 1847–1851.
38. PronykPM, HargreavesJR, KimJC, MorisonLA, PhetlaG, et al. (2006) Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet 368 : 1973–1983.
39. McLarenL, McIntyreL, KirkpatrickS (2010) Rose's population strategy of prevention need not increase social inequalities in health. Int J Epidemiol 39 : 372–377.
40. TsaiAC (2012) A typology of structural approaches to HIV prevention: a commentary on Roberts and Matthews. Soc Sci Med 75 : 1562–1567 discussion 1568–1571.
41. AizerA (2010) The gender wage gap and domestic violence. Am Econ Rev 100 : 1847–1859.
42. BeamanL, ChattopadhyayR, DufloE, PandeR, TopalovaP (2009) Powerful women: does exposure reduce bias? Q J Econ 124 : 1497–1540.
43. BeamanL, DufloE, PandeR, TopalovaP (2012) Female leadership raises aspirations and educational attainment for girls: a policy experiment in India. Science 335 : 582–586.
44. GiordanoPC, SchroederRD, CernkovichSA (2007) Emotions and crime over the life coruse: a neo-Meadian perspective on criminal continuity and change. Am J Sociol 112 : 1603–1661.
45. EhrensaftMK, CohenP, BrownJ, SmailesE, ChenH, JohnsonJG (2003) Intergenerational transmission of partner violence: a 20-year prospective study. J Consult Clin Psychol 71 : 741–753.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 5- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Antikoagulační léčba u pacientů před operačními výkony
-
Všechny články tohoto čísla
- Measuring Coverage in MNCH: Challenges and Opportunities in the Selection of Coverage Indicators for Global Monitoring
- Measuring Coverage in MNCH: Tracking Progress in Health for Women and Children Using DHS and MICS Household Surveys
- Measuring Coverage in MNCH: Population HIV-Free Survival among Children under Two Years of Age in Four African Countries
- Tobacco Company Efforts to Influence the Food and Drug Administration-Commissioned Institute of Medicine Report An Analysis of Documents Released through Litigation
- Irreconcilable Conflict: The Tobacco Industry and the Public Health Challenge of Tobacco Use
- Providing Impetus, Tools, and Guidance to Strengthen National Capacity for Antimicrobial Stewardship in Viet Nam
- Measuring Coverage in MNCH: New Findings, New Strategies, and Recommendations for Action
- Grand Challenges: Integrating Maternal Mental Health into Maternal and Child Health Programmes
- Measuring Coverage in MNCH: Challenges in Monitoring the Proportion of Young Children with Pneumonia Who Receive Antibiotic Treatment
- Measuring Coverage in MNCH: Current Indicators for Measuring Coverage of Diarrhea Treatment Interventions and Opportunities for Improvement
- Measuring Coverage in MNCH: Evaluation of Community-Based Treatment of Childhood Illnesses through Household Surveys
- Measuring Coverage in MNCH: Accuracy of Measuring Diagnosis and Treatment of Childhood Malaria from Household Surveys in Zambia
- Grand Challenges: Integrating Mental Health Care into the Non-Communicable Disease Agenda
- Integrating Global and National Knowledge to Select Medicines for Children: The Ghana National Drugs Programme
- Grand Challenges: Integrating Mental Health Services into Priority Health Care Platforms
- Disability Transitions and Health Expectancies among Adults 45 Years and Older in Malawi: A Cohort-Based Model
- Comparative Efficacy of Seven Psychotherapeutic Interventions for Patients with Depression: A Network Meta-Analysis
- Measuring Coverage in MNCH: Design, Implementation, and Interpretation Challenges Associated with Tracking Vaccination Coverage Using Household Surveys
- Measuring Coverage in MNCH: A Prospective Validation Study in Pakistan and Bangladesh on Measuring Correct Treatment of Childhood Pneumonia
- Contribution of and Smoking Trends to US Incidence of Intestinal-Type Noncardia Gastric Adenocarcinoma: A Microsimulation Model
- Carriage of in the Upper Respiratory Tract of Symptomatic and Asymptomatic Children: An Observational Study
- Setting Research Priorities to Reduce Mortality and Morbidity of Childhood Diarrhoeal Disease in the Next 15 Years
- Grand Challenges: Improving HIV Treatment Outcomes by Integrating Interventions for Co-Morbid Mental Illness
- Gene Expression Classification of Colon Cancer into Molecular Subtypes: Characterization, Validation, and Prognostic Value
- Domestic Violence and Perinatal Mental Disorders: A Systematic Review and Meta-Analysis
- Intimate Partner Violence and Incident Depressive Symptoms and Suicide Attempts: A Systematic Review of Longitudinal Studies
- Effect of Facilitation of Local Maternal-and-Newborn Stakeholder Groups on Neonatal Mortality: Cluster-Randomized Controlled Trial
- Intimate Partner Violence and Population Mental Health: Why Poverty and Gender Inequities Matter
- Assessing Population Aging and Disability in Sub-Saharan Africa: Lessons from Malawi?
- The Paradox of Mental Health: Over-Treatment and Under-Recognition
- Measuring Coverage in MNCH: Determining and Interpreting Inequalities in Coverage of Maternal, Newborn, and Child Health Interventions
- Measuring Coverage in MNCH: Total Survey Error and the Interpretation of Intervention Coverage Estimates from Household Surveys
- Measuring Coverage in MNCH: Indicators for Global Tracking of Newborn Care
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Gene Expression Classification of Colon Cancer into Molecular Subtypes: Characterization, Validation, and Prognostic Value
- Domestic Violence and Perinatal Mental Disorders: A Systematic Review and Meta-Analysis
- Intimate Partner Violence and Incident Depressive Symptoms and Suicide Attempts: A Systematic Review of Longitudinal Studies
- Measuring Coverage in MNCH: Challenges in Monitoring the Proportion of Young Children with Pneumonia Who Receive Antibiotic Treatment
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



