-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Harnessing Poverty Alleviation to Reduce the Stigma of HIV in Sub-Saharan Africa
article has not abstract
Published in the journal: . PLoS Med 10(11): e32767. doi:10.1371/journal.pmed.1001557
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001557Summary
article has not abstract
Summary Points
-
Poverty is an important driver of HIV stigma.
-
HIV-related morbidity undermines HIV-infected persons' ability to maintain their full economic contributions to family and community life.
-
Stigmatization and exclusion from local solidarity networks erode food and livelihood security, which undermine adherence to HIV treatment, further perpetuating this cycle.
-
HIV treatment can improve the economic, mental, and social health of HIV-infected persons, but it may not be sufficient to reduce the stigma of HIV.
-
Livelihood interventions can reduce the stigma of HIV by directly targeting poverty.
Introduction
HIV is highly stigmatized throughout sub-Saharan Africa [1],[2]. In studies conducted among general population samples, stigma has been shown to impede uptake of HIV testing and increase sexual risk-taking behavior [3],[4]. Among HIV-infected persons, stigma has also been associated with inhibited serostatus disclosure to sexual partners and potential treatment supporters, delays in HIV antiretroviral therapy (ART) initiation, and ART non-adherence [5],[6],[7]. The stigma of HIV also intensifies the poverty, stress, and insecurity endemic to many resource-limited settings [8], resulting in worsened mental health [9], itself an important determinant of AIDS-related mortality [10]. Until we can better understand how to effectively intervene to reduce the stigma of HIV, it will continue to adversely affect the well-being of HIV-infected persons and undermine both treatment and prevention efforts throughout sub-Saharan Africa.
Given the pressing need for effective intervention, in this Policy Forum article we argue that poverty alleviation should be conceptualized as a potentially powerful yet understudied tool for confronting the stigma of HIV. Beginning with a conceptual discussion of stigma, we draw on qualitative and epidemiological studies to focus our attention on the perceived disability, economic incapacity, and death associated with HIV as key determinants of stigma in numerous sub-Saharan African countries. We then explain how poverty alleviation may help reduce the stigma of HIV. In doing so we borrow from disparate lines of inquiry, including HIV research and programmatic work in sub-Saharan Africa; the medical literature on other stigmatized conditions, such as epilepsy and schizophrenia; and literature from other fields, including anthropology, economics, psychology, and sociology.
The Stigma of HIV in Sub-Saharan Africa
In many cultural contexts, the stigma of HIV is largely driven by concerns about its symbolic meanings [11]. Gilmore and Somerville [12] argue that stigma is best understood as a social process which involves the exercise of power, along the fault lines of these symbolic meanings, by one group over another. Consistent with their argument, stigma has historically been deployed in a manner that serves to reproduce inequalities that existed even prior to the HIV epidemic, thereby displacing already-marginalized groups even further downward in the status hierarchy (Box 1). For example, during the first decade of widespread awareness about the epidemic in the US, HIV was associated with marginalized groups perceived to be deviant or engaged in deviant behavior, such as injection drug users and men who have sex with men.
Box 1. The Stigma Process
-
Goffman [70] described stigma as an attribute that is “deeply discrediting” and that, in the eyes of society, reduces someone “from a whole and usual person to a tainted, discounted one” (p. 3).
-
Persons with and without the stigmatized attribute are separated into two categories: “them” vs. “us” [71],[72].
-
Internalized stigma results when stigmatized persons come to accept these inhospitable attitudes as valid, thereby developing self-defacing beliefs and perceptions about themselves [73].
-
Enacted stigma results when clandestine hostility and/or overt acts of discrimination are directed towards persons specifically because they possess the stigmatized attribute [71].
-
In such an environment, even stigmatized persons who are not directly victimized may experience fear in anticipation of being targeted (felt stigma) [74].
-
These processes are contingent on differentials in power [12],[75].
Although in some sub-Saharan African countries the stigma of HIV may be partly rooted in its association with perceived deviance, others have argued that such an account insufficiently explains persisting negative attitudes toward HIV-infected persons [13],[14],[15]. We hypothesize that an overlooked—and under-targeted—driver of HIV stigma is its powerful association with disability, economic incapacity, and death. Our hypothesis is grounded in the observation that, in settings of generalized poverty where subsistence agriculture is the norm and where social protection schemes are limited, it is a critical aspect of human sociality to be perceived as sufficiently fit to engage in physical labor [16],[17] and to be perceived as actively contributing to networks of mutual aid [18]. Economic incapacity resulting from HIV-associated morbidity, and the specter of impending premature mortality, call into question HIV-infected persons' abilities to support their households via productive labor or to engage in reciprocal exchange, thereby singling them out for social exclusion (Figure 1).
Fig. 1. Relationships between HIV, disability, and stigma. 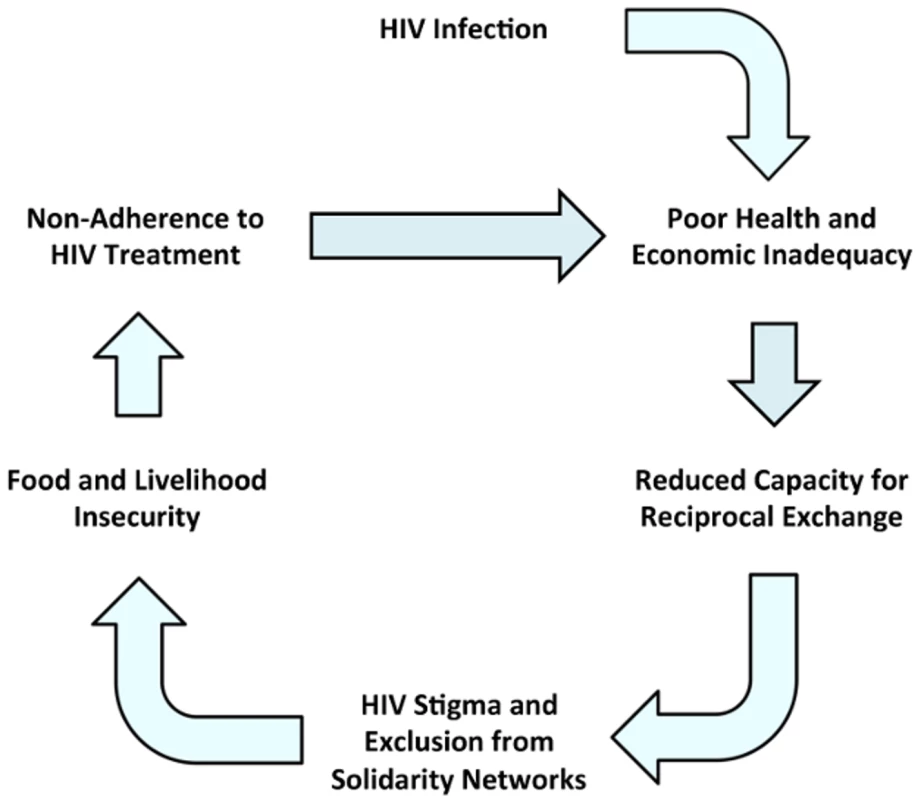
HIV infection has adverse health and economic impacts, undermining HIV-infected persons' abilities to maintain their full economic contributions to family and community life and engage in reciprocal exchange. Stigmatization and exclusion from local solidarity networks erodes their food and livelihood security, which in turn undermine their adherence to ART. Non-adherence to ART perpetuates this cycle by further compromising health and economic viability. The mechanism we describe here has been identified as a key culprit explaining the corroded social status of HIV-infected persons in different settings throughout sub-Saharan Africa [19]. Table S1 provides examples of qualitative studies from sub-Saharan Africa in which poverty and inability to engage in reciprocal exchange were cited as drivers of stigma. For example, a young man from a community sample in Zimbabwe portrayed HIV-infected persons as a drain on their communities: “Right now those who are infected are not treated as fellow human beings. They are already declared dead, and regarded as useless as a grave… They mean that these people are no longer able to do anything useful. They say they are just waiting for the day of their death” [20] (p. 2275). These attitudes are embedded in local descriptions of HIV-infected persons who have been labeled “corpses that live” [13] (p. 848). Table S2 lists other dysphemisms that have been applied to HIV-infected persons in countries throughout sub-Saharan Africa.
The conceptual discussion above describes both symbolic and instrumental drivers of stigma [11]. On the one hand, its symbolic component is derived from what HIV symbolizes in specific cultural contexts: disability, economic incapacity, and death. On the other hand, the exclusion of economically inadequate persons from participation in local solidarity networks can be viewed as instrumental, i.e., serving a utilitarian function. This view of stigma emphasizes the instrumental, rather than the symbolic, value of stigma to groups who are in a position to engage in the type of exercise of power described above. The instrumental basis for stigmatization has been elaborated from an evolutionary perspective by social psychologists who treat stigma as a behavioral adaptation designed to solve one of the central problems of human sociality: the need for long-term, cooperative, reciprocal exchange [21],[22]. Persons targeted for stigmatization are simply those who are perceived to violate the norm of reciprocity.
The stigma of HIV can also be understood using concepts borrowed from social capital theory. Persons living in settings of generalized poverty rely heavily on social capital (specifically, bonding and bridging social capital [23]) to access material resources needed for survival. These themes are prominently described in numerous qualitative studies from sub-Saharan Africa [24],[25],[26],[27],[28]. The motivating forces behind social capital are not always altruistic, however, as Portes and Sensenbrenner [29] argued. When social capital is rooted in instrumental rather than altruistic concerns, persons who do not fulfill reciprocity expectations can be excluded. Accordingly, in some communities, fear of the “social death” and exclusion resulting from an HIV diagnosis is more intense than the fear of the disease itself [30].
To date, a number of different approaches to stigma reduction have been attempted. These have largely consisted of educational interventions, aimed at the general population to correct overblown fears about casual transmission risks, or contact interventions in which study participants experience scripted interactions with HIV-infected persons in order to increase tolerance and acceptance [31]. Under the framework described above, these approaches can be thought of as addressing either symbolic or instrumental aspects of HIV stigma. Persons who are exposed to an educational intervention (that demonstrates how the risks of casual transmission are much lower than they previously thought) might be expected to revise their instrumental concerns about HIV. Similarly, persons who are exposed to HIV-infected persons through a contact intervention might be inclined to revise their symbolically grounded views about the humanity of HIV-infected persons (a process termed “recategorization” [32]). These approaches, however, do not necessarily consider the underlying functional aspects of HIV stigma.
ART Scale-Up as a Necessary but Not Sufficient Stigma Reduction Strategy
If an important driver of HIV stigma is its powerful association with disability, economic incapacity, and death, then ART might receive an alternative reading as an anti-stigma intervention. Although ART is deployed at the level of the individual, it should also be regarded as a structural intervention aimed at altering the context in which HIV-infected persons interact with their HIV-uninfected peers [33]. We conceptualize HIV treatment as increasing the perceived social value of HIV-infected persons, by detaching the perceived inevitability of death from HIV infection and by directly addressing societal assessments about one's ability to adhere to norms of reciprocity. Consistent with this hypothesis, epidemiologic and econometric studies have demonstrated that the availability of and perceived access to ART have altered general population expectancies about longevity in Malawi [34],[35] and diminished negative attitudes towards HIV-infected persons in Botswana [2]. In fact, an early argument advanced in support of ART scale-up was that doing so would reduce stigma and enhance prevention efforts [36].
For HIV-infected persons, the past decade of ART expansions has vindicated these claims. Program implementers at the non-governmental organization Partners in Health, for example, reported that after the introduction of ART in Haiti, they observed greater demand for HIV testing and counseling, and their patients reported fewer HIV-related discriminatory events and increased social integration [36],[37]. As shown in Table S1, in qualitative studies conducted in countries throughout sub-Saharan Africa, HIV-infected persons initiating ART have similarly described a constellation of benefits, including improved economic productivity, greater self-efficacy, and reduced internalized stigma [38]. These findings have been confirmed in larger-scale epidemiological studies as well [9],[39],[40],[41],[42],[43],[44].
Yet, while ART has undeniably improved the economic, mental, and social health of HIV-infected persons, two factors may hinder its ability to level stigmatizing beliefs in the general population. First, accurate knowledge about ART efficacy may not evenly follow the contours of treatment expansion. Over the past decade, with substantial investments in educational HIV-related messages promoted through radio, television, and/or print media, overall levels of accurate HIV-specific knowledge have improved slightly but remain low in general population surveys conducted throughout sub-Saharan Africa [45]. Similarly, local beliefs about ART availability or ART efficacy may also lag, thereby perpetuating the assumed association between HIV and disability, economic incapacity, and death. This could potentially explain why uptake of HIV testing throughout sub-Saharan Africa, while increasing over time, has remained persistently low despite large-scale expansions in access to ART [46]. Refusal of treatment despite eligibility has also been described [47].
Second, ART alone may not be sufficient to decrease the stigma of HIV. Despite expansions in access to ART at no charge, many patients present for treatment initiation late in the disease stage. As a result, even when they experience dramatic recovery of physical function, they may return to work at a lower intensity compared to their pre-disease state [17],[18],[48],[49]. In addition, even HIV-infected persons who are able to resume working at full capacity have nonetheless voiced difficulties in rebounding to the same overall level of economic well-being. While trying to cope with HIV-associated morbidity before treatment initiation, they may have had to adopt coping strategies such as selling off productive assets or shifting from high-return to low-return activities, while ultimately undermining their own financial viability in the long term. These themes are prominent in qualitative studies [16],[17],[19],[27],[49] and have been confirmed in larger-scale epidemiological studies [50].
“ART-Plus”: Harnessing Poverty Alleviation to Reduce the Stigma of HIV
Considering the important limitations in our current portfolio of anti-stigma interventions [31], we believe poverty alleviation—and, specifically, livelihood interventions—should also be considered in conjunction with ART to help further reduce the stigma of HIV. We recognize that the idea of “ART-plus” does not, at present, have widespread adherents. For example, a recently published Cochrane Collaboration protocol for a planned systematic review of interventions to reduce HIV stigma lists an exhaustive catalogue of educational anti-stigma interventions, including “lectures, group discussions, individual education, radio, television, print (newspapers, magazines, booklets, leaflets, posters, pamphlets), films, documentaries, billboards, folk media (such as street dramas), or a combination of these” [51] (p. 4) but does not provide any indication that livelihood interventions will be examined.
The hypotheses we describe in this article are consistent with an argument advanced by Castro and Farmer [37], who prominently called attention to the ways in which the stigma of HIV is mainly determined by large-scale social forces such as poverty and racial and gender inequality. Drawing on their programmatic and research experience with HIV-infected persons in Haiti, they write, “poverty, already representing an almost universal stigma, will be the primary reason that poor people living with HIV suffer from greater AIDS-related stigma” (p. 55). Conceptually, this line of argument suggests that HIV-related stigmatization may at least be partially conditioned on poverty, extending the cognitive and psychological models described above to emphasize how power relations and economic and other structural factors influence community responses to HIV. Qualitative studies from Brazil [52], Zambia [53], and Zimbabwe [54] have generated similar conclusions.
Non-governmental organizations have already moved forward with programs to address these issues [41],[55],[56],[57],[58]. Indeed, the summary term we have adopted here, “ART-plus,” is borrowed from a Peruvian non-governmental organization's pilot program that employed a comprehensive HIV treatment strategy with both ART and socioeconomic support [55]. Yet although the multiple lines of inquiry described in this article provide sufficient groundwork to justify the implementation of experimental or quasi-experimental studies, to date the available evidence in this area has been exclusively observational. In qualitative studies of HIV-infected persons participating in integrated livelihood intervention programs in different sub-Saharan African settings, study participants reported less stigma, increased social integration, and improved status in the community (Table S1). These changes were explicitly linked to their improved economic standing, as one program staff member observed: “Some participants…have gained [a] reputation within their communities…Because of the cow, because of the income they are getting, they have been taking on positions of responsibility in their communities, in churches, in schools, on boards…they are now getting less stigmatized in a sense… [the community] can see them managing their own issues, managing themselves, surviving…” [58] (p.e26117). In other words, by availing themselves of economic opportunities brought about through these interventions, HIV-infected persons were able to construct “positive identities” for themselves in much the same fashion as when they were first restored to health after initiating ART [54] (p. 1008).
Additional evidence comes from a longitudinal study with matched controls, in which Muñoz and colleagues [59] studied the psychosocial impacts of a comprehensive social support intervention among 120 HIV-infected persons receiving ART in Peru. At 24-month follow-up, participants in the intervention group reported less stigma and perceived greater social support. Because only ten of these actually received individually tailored microfinance assistance, there was limited ability to draw inferences about the incremental stigma-reducing effects of the microfinance assistance component of the intervention. However, studies of similar types of interventions based on participant samples unselected for HIV seropositivity have shown statistically significant impacts on mental health [60],[61] and social integration [62], thereby lending further plausibility to the effects shown by Muñoz and colleagues [59].
A simplified diagram summarizing our hypotheses about how ART-plus revises HIV-stigmatizing beliefs is shown in Figure 2. In our account, ART-plus addresses internalized stigma, by enhancing the HIV-infected person's self-efficacy and self-esteem. This aspect of our framework is most closely related to the conceptual model and empirical study by Rosenfield [63], who identified links between economic rehabilitation, self-efficacy, social status, and subjective quality of life among functionally impaired persons with mental illness in the US. Further, if the objective is “recategorization” (as described above in the context of contact interventions), ART-plus also offers a different type of recategorization to address enacted stigma, by encouraging a view of HIV-infected persons not as a net drain on their communities but rather as productive members of society who are “managing their own issues” [58] (p.e26117).
Fig. 2. Transforming HIV-stigmatizing beliefs through ART-plus. 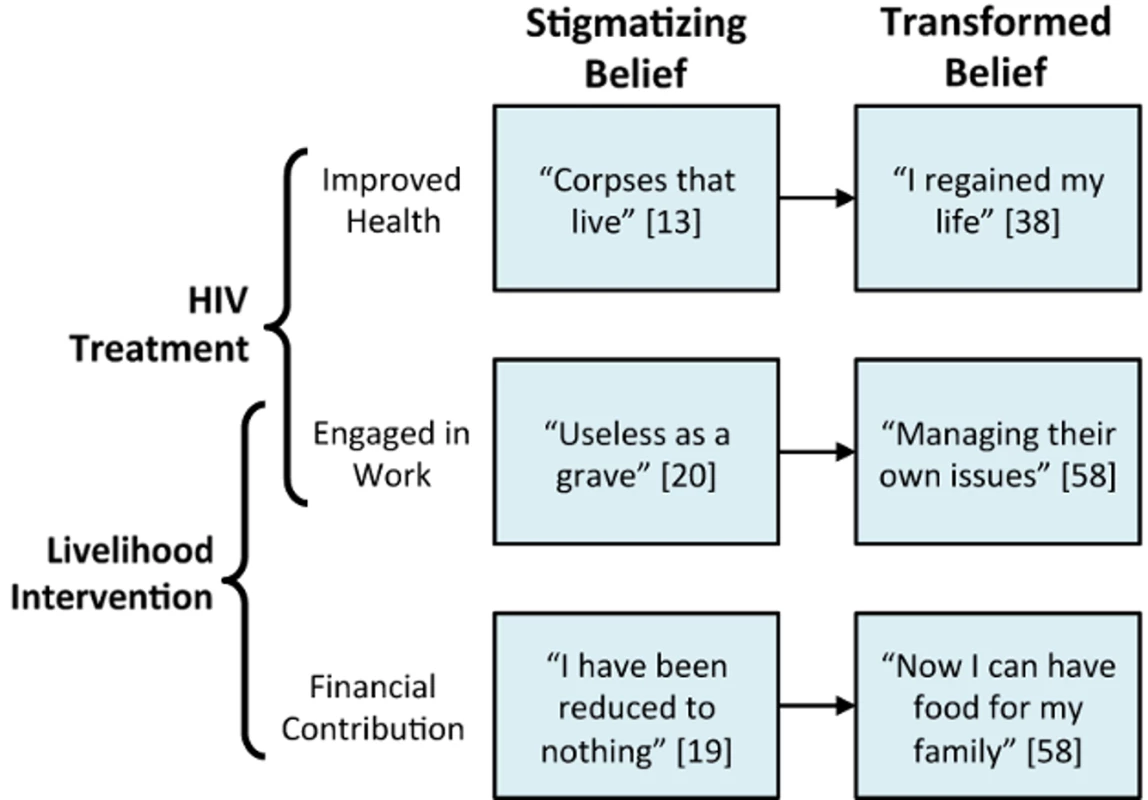
ART manages the disability incurred through HIV infection, undermining the view of HIV-infected persons as economically inadequate members of the community and permitting them to re-engage in productive activity. Livelihood interventions, such as combined financial literacy and microenterprise management programs, may additionally create new modes of engaging in productive activity, such as new trades or new enterprise development. These financial contributions are welcomed within local solidarity networks, and the norm of reciprocity is upheld. Limitations of the ART-Plus Approach
We recognize several potential pitfalls with this proposed ART-plus approach to stigma reduction. First, while we believe that the perceived association between HIV and disability, economic incapacity, and death is a primary driver of stigma, we also recognize that stigma is complex and may be driven by many other factors depending on the cultural context. Despite dramatic expansions in access to ART in urban South Africa, for example, a longitudinal study by Maughan-Brown [64] showed continued increases in symbolic stigma centered around the association of HIV with promiscuity. Similarly, a common prominent theme in several qualitative studies from Tanzania was a negative perception of HIV-infected persons that persisted specifically because of ART's effects on prolonging life [65],[66]. Study participants voiced concerns that ART changed HIV-infected persons from diseased but visibly ill and incapable of sexual risk-taking behavior, to diseased but healthy-appearing potential vectors of sexual transmission. In settings where such symbolism is a secondary but nonetheless substantial driver of stigma, even if a combined ART-plus intervention could undo the association between HIV, disability, and economic incapacity, it would still “leave the spectre of illicit sex untouched” [67] (p. 643).
A second issue that poses a dilemma for the implementation of our proposed strategy, without undermining the strategy itself, is that precisely targeting this type of intervention may be politically difficult. Making economic resources available specifically to HIV-infected persons in the context of widespread poverty may generate resentment not unlike the antipathy directed towards welfare recipients in the US beginning in the 1970s and continuing to the present day. For example, participants in a qualitative study from South Africa intimated that welfare fraud was widespread among HIV-infected persons receiving disability grants [68]. Because of these reasons, there is a consensus that broad-based targeting schemes (e.g., based on poverty and multiple vulnerability criteria) for cash transfer interventions should be used rather than procedures focused on HIV-affected status or orphanhood alone [69]. However, interventions that focus on livelihoods, such as animal husbandry training or microfinance assistance for small enterprises, may be perceived in the community to be more sustainable than interventions that provide direct food or cash transfers and therefore engender less resentment [58].
Conclusion
Taken together, these related strands of inquiry build a strong case for considering livelihood interventions as a compelling stigma reduction strategy with the potential to improve the well-being of HIV-infected persons throughout sub-Saharan Africa. Although our framework has not been rigorously tested in an experimental context, we believe the corroborating evidence from anthropology, economics, psychology, and sociology is strongly suggestive. It would be imprudent for us to suggest that prevailing approaches to stigma should be abandoned despite their uneven effectiveness to date. Future studies may find that the most effective approaches to stigma reduction adopt synergistic strategies that target both the stigmatized (through livelihood interventions) as well as the stigmatizers (through educational or contact interventions).
Supporting Information
Zdroje
1. KalichmanSC, SimbayiLC, JoosteS, ToefyY, CainD, et al. (2005) Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav 9 : 135–143.
2. WolfeWR, WeiserSD, LeiterK, StewardWT, Percy-de KorteF, et al. (2008) The impact of universal access to antiretroviral therapy on HIV stigma in Botswana. Am J Public Health 98 : 1865–1871.
3. YoungSD, HlavkaZ, ModibaP, GrayG, Van RooyenH, et al. (2010) HIV-related stigma, social norms, and HIV testing in Soweto and Vulindlela, South Africa: National Institutes of Mental Health Project Accept (HPTN 043). J Acquir Immune Defic Syndr 55 : 620–624.
4. PitpitanEV, KalichmanSC, EatonLA, CainD, SikkemaKJ, et al. (2012) AIDS-related stigma, HIV testing, and transmission risk among patrons of informal drinking places in Cape Town, South Africa. Ann Behav Med 43 : 362–371.
5. TsaiAC, BangsbergDR, KegelesSM, KatzIT, HabererJE, et al. (2013) Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Ann Behav Med 46 : 285–294.
6. MuhamadiL, NsabagasaniX, TumwesigyeMN, Wabwire-MangenF, EkstromAM, et al. (2010) Inadequate pre-antiretroviral care, stock-out of antiretroviral drugs and stigma: policy challenges/bottlenecks to the new WHO recommendations for earlier initiation of antiretroviral therapy (CD<350 cells/microL) in eastern Uganda. Health Policy 97 : 187–194.
7. KatzIT, RyuAE, OnuegbuAG, PsarosC, WeiserSD, et al. (2013) Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc 16 : 18640.
8. TsaiAC, BangsbergDR, EmenyonuN, SenkunguJK, MartinJN, et al. (2011) The social context of food insecurity among persons living with HIV/AIDS in rural Uganda. Soc Sci Med 73 : 1717–1724.
9. TsaiAC, BangsbergDR, FrongilloEA, HuntPW, MuzooraC, et al. (2012) Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med 74 : 2012–2019.
10. CookJA, GreyD, BurkeJ, CohenMH, GurtmanAC, et al. (2004) Depressive symptoms and AIDS-related mortality among a multisite cohort of HIV-positive women. Am J Public Health 94 : 1133–1140.
11. PryorJB, ReederGD, VinaccoR, KottTL (1989) The instrumental and symbolic functions of attitudes towards persons with AIDS. J Appl Soc Psychol 19 : 377–404.
12. GilmoreN, SomervilleMA (1994) Stigmatization, scapegoating and discrimination in sexually transmitted diseases: overcoming ‘them’ and ‘us’. Soc Sci Med 39 : 1339–1358.
13. NiehausI (2007) Death before dying: understanding AIDS stigma in the South Africa lowveld. J S Afr Stud 33 : 845–860.
14. Niehaus I (2009) Part 1: Bushbuckridge: Beyond treatment literacy. In: Crewe M, editor. Magic AIDS Review 2009. Pretoria: University of Pretoria. pp. 17–58.
15. Dapaah JM (2012) HIV/AIDS treatment in two Ghanaian hospitals: experiences of patients, nurses, and doctors. Leiden: African Studies Centre.
16. RussellS, SeeleyJ, EzatiE, WamaiN, WereW, et al. (2007) Coming back from the dead: living with HIV as a chronic condition in rural Africa. Health Policy Plan 22 : 344–347.
17. KalerA, AlibhaiA, KippW, RubaaleT, Konde-LuleJ (2010) “Living by the hoe” in the age of treatment: perceptions of household well-being after antiretroviral treatment among family members of persons with AIDS. AIDS Care 22 : 509–519.
18. SeeleyJ, RussellS (2010) Social rebirth and social transformation? Rebuilding social lives after ART in rural Uganda. AIDS Care 22 : 44–50.
19. Kwansa BK (2013) Safety in the midst of stigma: experiencing HIV/AIDS in two Ghanaian communities. Leiden: African Studies Centre.
20. MamanS, AblerL, ParkerL, LaneT, ChirowodzaA, et al. (2009) A comparison of HIV stigma and discrimination in five international sites: the influence of care and treatment resources in high prevalence settings. Soc Sci Med 68 : 2271–2278.
21. Neuberg SL, Smith SM, Asther T (2000) Why people stigmatize: toward a biocultural framework. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The social psychology of stigma. New York: The Guilford Press. pp. 31–61.
22. KurzbanR, LearyMR (2001) Evolutionary origins of stigmatization: the functions of social exclusion. Soc Sci Med 127 : 187–208.
23. Gittell R, Vidal A (1998) Community organizing: building social capital as a development strategy. Thousand Oaks: Sage Publications, Inc.
24. RankinWW, BrennanS, SchellE, LaviwaJ, RankinSH (2005) The stigma of being HIV-positive in Africa. PLoS Med 2: e247.
25. WareNC, IdokoJ, KaayaS, BiraroIA, WyattMA, et al. (2009) Explaining adherence success in sub-Saharan Africa: an ethnographic study. PLoS Med 6: e11.
26. IzugbaraCO, WekesaE (2011) Beliefs and practices about antiretroviral medication: a study of poor urban Kenyans living with HIV/AIDS. Sociol Health Illn 33 : 869–883.
27. SamuelsFA, RutenbergN (2011) “Health regains but livelihoods lag”: findings from a study with people on ART in Zambia and Kenya. AIDS Care 23 : 748–754.
28. GaussetQ, MogensenHO, YameogoWM, BertheA, KonateB (2012) The ambivalence of stigma and the double-edged sword of HIV/AIDS intervention in Burkina Faso. Soc Sci Med 74 : 1037–1044.
29. PortesA, SensenbrennerJ (1993) Embeddedness and immigration: notes on the social determinants of economic action. Am J Sociol 98 : 1320–1350.
30. EgrotM (2007) Renaître d'une mort sociale annoncée: recomposition du lien social des personnes vivant avec le VIH en Afrique de l'Ouest (Burkina Faso, Sénégal). Cultures et Sociétés 1 : 49–56.
31. SenguptaS, BanksB, JonasD, MilesMS, SmithGC (2011) HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav 15 : 1075–1087.
32. GaertnerSL, MannJ, MurrellA, DovidioJF (1989) Reducing intergroup bias: the benefits of recategorization. J Pers Soc Psychol 57 : 239–249.
33. TsaiAC (2012) A typology of structural approaches to HIV prevention: a commentary on Roberts and Matthews. Soc Sci Med 75 : 1562–1567; discussion 1568–1571.
34. Baranov V, Bennett D, Kohler H-P (2012) The indirect impact of antiretroviral therapy. Hanover: Northeast Universities Development Consortium Conference.
35. Baranov V, Kohler H-P (2013) The impact of AIDS treatment on savings and human capital investment in Malawi. New Orleans: Population Association of American 2013 Annual Meeting.
36. FarmerP, LeandreF, MukherjeeJS, ClaudeM, NevilP, et al. (2001) Community-based approaches to HIV treatment in resource-poor settings. Lancet 358 : 404–409.
37. CastroA, FarmerP (2005) Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. Am J Public Health 95 : 53–59.
38. Nyanzi-WakholiB, LaraAM, WateraC, MunderiP, GilksC, et al. (2009) The role of HIV testing, counselling, and treatment in coping with HIV/AIDS in Uganda: a qualitative analysis. AIDS Care 21 : 903–908.
39. Kaai S, Sarna A, Luchters S, Geibel S, Munyao P, et al.. (2007) Changes in stigma among a cohort of people on antiretroviral therapy: findings from Mombasa, Kenya. Nairobi: Population Council.
40. ThirumurthyH, ZivinJG, GoldsteinM (2008) The economic impact of AIDS treatment: labor supply in western Kenya. J Hum Resources 43 : 511–552.
41. MuñozM, FinneganK, ZeladitaJ, CaldasA, SanchezE, et al. (2010) Community-based DOT-HAART accompaniment in an urban resource-poor setting. AIDS Behav 14 : 721–730.
42. WeiserSD, GuptaR, TsaiAC, FrongilloEA, GredeN, et al. (2012) Changes in food insecurity, nutritional status, and physical health status after antiretroviral therapy initiation in rural Uganda. J Acquir Immune Defic Syndr 61 : 179–186.
43. WagnerGJ, Ghosh-DastidarB, GarnettJ, KityoC, MugyenyiP (2012) Impact of HIV antiretroviral therapy on depression and mental health among clients With HIV in Uganda. Psychosom Med 74 : 883–890.
44. TsaiAC, BangsbergDR, BwanaM, HabererJE, FrongilloEA, et al. (2013) How does antiretroviral treatment attenuate the stigma of HIV? Evidence from a cohort study in rural Uganda. AIDS Behav 17 : 2725–2731.
45. Mishra V, Agrawal P, Alva S, Gu Y, Wang S (2009) Changes in HIV-related knowledge and behaviors in sub-Saharan Africa. DHS Comparative Reports No. 24. Calverton: ICF Macro.
46. Staveteig S, Wang S, Head SK, Bradley SEK, Nybro E (2013) Demographic patterns of HIV testing uptake in sub-Saharan Africa. DHS Comparative Reports No. 30. Calverton: ICF International.
47. KatzIT, EssienT, MarindaET, GrayGE, BangsbergDR, et al. (2011) Antiretroviral therapy refusal among newly diagnosed HIV-infected adults. AIDS 25 : 2177–2181.
48. DattaD, NjugunaJ (2008) Microcredit for people affected by HIV and AIDS: insights from Kenya. SAHARA J 5 : 94–102.
49. WagnerG, RyanG, HuynhA, KityoC, MugyenyiP (2009) A qualitative analysis of the economic impact of HIV and antiretroviral therapy on individuals and households in Uganda. AIDS Patient Care STDS 23 : 793–798.
50. YamanoT, JayneTS (2004) Measuring the impact of working-age adult mortality on small-scale farm households in Kenya. World Dev 32 : 91–119.
51. Wariki WMV, Nomura S, Ota E, Mori R, Shibuya K (2013) Interventions for reduction of stigma in people with HIV/AIDS (protocol). Cochrane Database Syst Rev: Art. no. CD006735. doi: 10.1002/14651858.CD006735.
52. Abadía-BarreroCE, CastroA (2006) Experiences of stigma and access to HAART in children and adolescents living with HIV/AIDS in Brazil. Soc Sci Med 62 : 1219–1228.
53. Bond V (2006) Stigma when there is no other option: understanding how poverty fuels discrimination toward people living with HIV in Zambia. In: Gillespie S, editor. AIDS, poverty, and hunger: challenges and responses. Washington, D.C.: International Food Policy Research Institute. pp. 181–197.
54. CampbellC, SkovdalM, MadanhireC, MugurungiO, GregsonS, et al. (2011) “We, the AIDS people. . .”: how antiretroviral therapy enables Zimbabweans living with HIV/AIDS to cope with stigma. Am J Public Health 101 : 1004–1010.
55. Muñoz M, Espiritu B, Palacios E, Sebastian JL, Mestanza L, et al.. (2006) Pilot study of ART-PLUS for vulnerable HIV-positive patients in Lima, Peru. Abstract no. CDB1267. Toronto: XVI International AIDS Conference.
56. PiotP, GreenerR, RussellS (2007) Squaring the circle: AIDS, poverty, and human development. PLoS Med 4 : 1571–1575.
57. LonguetC, MachuronJL, DeschampsMM, SiniorR, BrignoliE, et al. (2009) Access to microcredit for women living with, or vulnerable to, HIV in Haiti. Field Actions Sci Rep 2 : 85–91.
58. YagerJE, KadiyalaS, WeiserSD (2011) HIV/AIDS, food supplementation and livelihood programs in Uganda: a way forward? PLoS One 6: e26117.
59. MuñozM, BayonaJ, SanchezE, ArevaloJ, SebastianJL, et al. (2011) Matching social support to individual needs: a community-based intervention to improve HIV treatment adherence in a resource-poor setting. AIDS Behav 15 : 1454–1464.
60. AhmedSM, ChowdhuryM (2001) Micro-credit and emotional well-being: experience of poor rural women from Matlab, Bangladesh. World Dev 29 : 1957–1966.
61. FernaldLC, HamadR, KarlanD, OzerEJ, ZinmanJ (2008) Small individual loans and mental health: a randomized controlled trial among South African adults. BMC Public Health 8 : 409.
62. PronykPM, HarphamT, BuszaJ, PhetlaG, MorisonLA, et al. (2008) Can social capital be intentionally generated? A randomized trial from rural South Africa. Soc Sci Med 67 : 1559–1570.
63. RosenfieldS (1992) Factors contributing to the subjective quality of life in the chronic mentally ill. J Health Soc Behav 33 : 299–315.
64. Maughan-BrownB (2010) Stigma rises despite antiretroviral roll-out: a longitudinal analysis in South Africa. Soc Sci Med 70 : 368–374.
65. RouraM, UrassaM, BuszaJ, MbataD, WringeA, et al. (2009) Scaling up stigma? The effects of antiretroviral roll-out on stigma and HIV testing. Early evidence from rural Tanzania. Sex Transm Infect 85 : 308–312.
66. EzekielMJ, TalleA, JumaJM, KleppKI (2009) “When in the body, it makes you look fat and HIV negative”: the constitution of antiretroviral therapy in local discourse among youth in Kahe, Tanzania. Soc Sci Med 68 : 957–964.
67. JohnsonJ (2012) Life with HIV: ‘stigma’ and hope in Malawi's era of ARVs. Africa (Lond) 82 : 632–653.
68. Zuberi F (2005) “Hey Miss AIDS, when are you going to receive your social grant?” The right to have access to social assistance: HIV/AIDS and disability grants. In: Viljoen F, editor. Righting stigma: exploring a rights-based approach to addressing stigma. Pretoria: University of Pretoria. pp. 116–131.
69. Adato M, Bassett L (2012) Social protection and cash transfers to strengthen families affected by HIV and AIDS. Washington, D.C.: International Food Policy Research Institute.
70. Goffman E (1963) Stigma: notes on the management of spoiled identity. Englewood Cliffs: Prentice-Hall, Inc.
71. Allport GW (1954) The nature of prejudice. Reading: Addison-Wesley Publishing Company.
72. BrewerMB (1979) In-group bias in the minimal intergroup situation: a cognitive-motivational analysis. Psychol Bull 86 : 307–324.
73. Scheff TJ (1966) Being mentally ill: a sociological theory. Chicago: Aldine Publishing Co.
74. ScamblerG, HopkinsA (1986) Being epileptic: coming to terms with stigma. Sociol Health Illn 8 : 26–43.
75. LinkBG, PhelanJC (2001) Conceptualizing stigma. Annu Rev Sociol 27 : 363–385.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 11- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
-
Všechny články tohoto čísla
- Antenatal Syphilis Screening Using Point-of-Care Testing in Sub-Saharan African Countries: A Cost-Effectiveness Analysis
- From Ideals to Tools: Applying Human Rights to Maternal Health
- Interactions between Non-Physician Clinicians and Industry: A Systematic Review
- Harnessing Poverty Alleviation to Reduce the Stigma of HIV in Sub-Saharan Africa
- Integrating Health Care to Meet the Needs of the Mother–Infant Pair: A Call for Papers for Year 3 of the Maternal Health Task Force–PLOS Collection
- Changes in Chinese Policies to Promote the Rational Use of Antibiotics
- Same Song, Different Audience: Pharmaceutical Promotion Targeting Non-Physician Health Care Providers
- A Gene Expression Signature for RSV: Clinical Implications and Limitations
- Global Research Priorities to Better Understand the Burden of Iatrogenic Harm in Primary Care: An International Delphi Exercise
- Measles Outbreak Response Immunization Is Context-Specific: Insight from the Recent Experience of Médecins Sans Frontières
- Global Mortality Estimates for the 2009 Influenza Pandemic from the GLaMOR Project: A Modeling Study
- When to Start Antiretroviral Therapy in Children Aged 2–5 Years: A Collaborative Causal Modelling Analysis of Cohort Studies from Southern Africa
- Burden of Depressive Disorders by Country, Sex, Age, and Year: Findings from the Global Burden of Disease Study 2010
- Role of DNA Methylation and Epigenetic Silencing of in Endometrial Cancer Development
- Characterization of Regional Influenza Seasonality Patterns in China and Implications for Vaccination Strategies: Spatio-Temporal Modeling of Surveillance Data
- Whole Blood Gene Expression Profiles to Assess Pathogenesis and Disease Severity in Infants with Respiratory Syncytial Virus Infection
- Complex Disease Dynamics and the Design of Influenza Vaccination Programs
- A Brief Patient-Reported Outcomes Quality of Life (PROQOL) Instrument to Improve Patient Care
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- A Brief Patient-Reported Outcomes Quality of Life (PROQOL) Instrument to Improve Patient Care
- Burden of Depressive Disorders by Country, Sex, Age, and Year: Findings from the Global Burden of Disease Study 2010
- From Ideals to Tools: Applying Human Rights to Maternal Health
- Role of DNA Methylation and Epigenetic Silencing of in Endometrial Cancer Development
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



