-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Changes in Chinese Policies to Promote the Rational Use of Antibiotics
article has not abstract
Published in the journal: . PLoS Med 10(11): e32767. doi:10.1371/journal.pmed.1001556
Category: Health in Action
doi: https://doi.org/10.1371/journal.pmed.1001556Summary
article has not abstract
Summary Points
-
Microbial resistance to antimicrobial agents (antimicrobial resistance, AMR) is a serious public health challenge, and containment of AMR is an urgent priority, both in China and worldwide.
-
The main cause of AMR is the irrational use of antimicrobial agents, in healthcare and veterinary settings and by the general public. Actions taken by the Chinese health administrative authorities in the past 10 years have been largely unsuccessful, likely because of the lack of mandatory regulations.
-
In 2011, coupled with new healthcare reforms, the Chinese Ministry of Health changed strategy and launched a special campaign to promote the rational use of antimicrobials in healthcare settings. This mainly consisted of establishing mandatory management strategies, such as target setting, taskforce organization, and the development of audit and inspection systems.
-
The special campaign had notable achievements, with decreased antibiotic sales and a reduced percentage of prescriptions for antimicrobials for both hospitalized patients and outpatients.
-
A number of issues still need to be addressed to ensure further improvements in AMR containment. These include the unregulated use of antibiotics in animal husbandry, over-the-counter purchases of antibiotics, and elimination of economic incentives for drug sales.
Antimicrobial resistance (AMR) is a serious public health challenge and containment of AMR is a global priority. On World Health Day in April 2011, the World Health Organization appealed to all member countries to “combat drug resistance: no action today, no cure tomorrow” [1]. The implementation of new Chinese policies over the past 2 years for the rational use of antimicrobials and AMR containment is a promising response to this appeal.
The Causes of Increasing Antimicrobial Resistance in China
The prevalence of AMR is relatively high in China; the morbidity and mortality from infections caused by multidrug-resistant or pan-drug-resistant pathogens are higher in China than in other countries [2]. Data reported by the Chinese Ministry of Health (MOH) National Antimicrobial Resistance Investigation Net (Mohnarin) indicates that AMR is rising steadily. The prevalence of methicillin-resistant Staphylococcus aureus (MRSA), extended-spectrum β-lactamase-producing Escherichia coli, imipenem-resistant Pseudomonas aeruginosa, and imipenem-resistant Acinetobacter baumannii—the so-called “superbugs” in nosocomial infections—was 50.5%, 71.2%, 23.4%, and 56.8% in 2010, respectively (Figure 1). The overall prevalence of erythromycin-resistant Streptococcus pneumonia and ciprofloxacin-resistant E. coli was 94.7% and 65.7% in community settings, respectively [3],[4].
Fig. 1. Overall trends in prevalence of major antimicrobial-resistant bacteria in Chinese tertiary hospitals in 2000–2011. 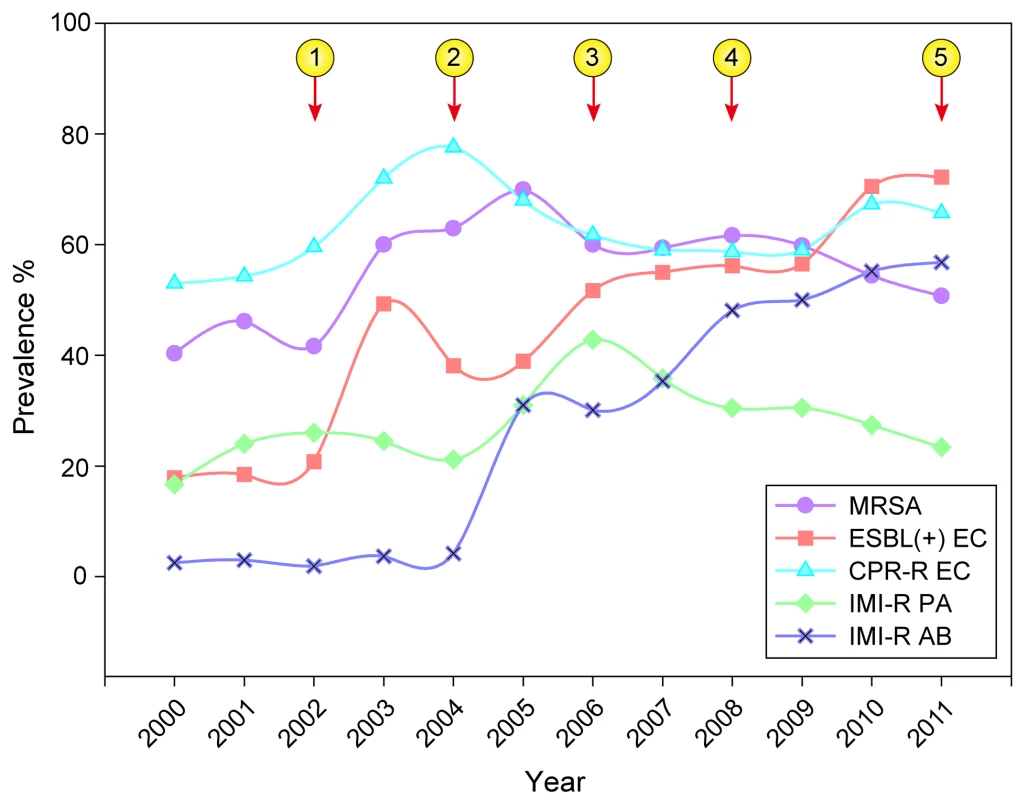
The majority of the data were adapted from Mohnarin results, which mostly represent situations involving nosocomial infections in tertiary hospitals. The numbers in circles describe the chronology of major administrative interventions taken by the Chinese Ministry of Health. indicates the issue of “temporary rules for pharmaceutical affairs in healthcare institutions” (2002); indicates the issue of “guidance for the clinical use of antimicrobials” (2004); indicates the issue of “regulations for management of nosocomial infections' (2006); indicates the issue of recommendations for enhancing the prevention and control of multidrug resistant bacterial infections (2008); and indicates the special campaign initiated in 2011. MRSA, methicillin-resistant Staphylococcus aureus; ESBL (+) EC, extended-spectrum β-lactamase-producing Escherichia coli; CPR-REC, ciprofloxacin-resistant E. coli; IMI-R PA, imipenem-resistant Pseudomonas aeruginosa; IMI-R AB, imipenem-resistant Acinetobacter baumannii. Irrational use of antimicrobial agents is the main cause of increased AMR. In China, antibiotics are considered to be a panacea by the general public and some healthcare practitioners. Over-the-counter purchase and over-reliance on antibiotics for disease therapy, infection prevention, and animal growth promotion are common phenomena in healthcare settings and veterinary practice. The percentage of prescriptions containing antibiotics in rural clinics of western China was around 50%, which is higher than in developed countries such as the US and Sweden [5]. Another important cause of the irrational use of antibiotics is the financial compensation provided to healthcare institutions for drug sales. The Chinese healthcare system consists of a government-led system with characteristics of free market financing and lower service pricing. The government's contribution to hospital budgets is less than 20% of hospital expenditure. Healthcare institutions can receive financial compensation by selling healthcare services and drugs. The government's acquiescence to the situation has stimulated, and to some extent encouraged, excessive examinations, unnecessary treatment, and overuse of medicines by routine healthcare services. Drug sales constitute about half of institutional income and most of the profit, with more than 25% being sales of antimicrobial agents [6]. At the same time, the overuse of antimicrobial agents in animal husbandry and farming has contributed to the occurrence and spread of antibiotic-resistant microbes in the environment [7],[8].
The Limited Effect of Professional Strategies for the Rational Use of Antibiotics
To control AMR, the Chinese health administrative authorities have taken a series of actions over the past 10 years, including the development of technical specifications and policies. These included the issue of guidance about antibiotic use and infection control. Mohnarin and the Chinese MOH Center for Antibacterial Surveillance (Mohcas) were established in 2006. Hospitals were required to set up a drug therapeutics committee to facilitate the rational use of drugs, and medical practitioners were required to prescribe antibiotics in a rational manner. Furthermore, nosocomial infection control measures were emphasized, such as hand hygiene and contact precautions for AMR infections (although compliance is often unsatisfactory because of heavy staff workloads and large patient populations). In addition, nationwide continuing medical education programs focusing on rational drug use and AMR control, were conducted repeatedly. All of the measures were established as part of a technical support system to promote the rational use of antibiotics, as recommended by the World Health Organization [9],[10].
However, due to strained resources, insufficient enforcement, absence of supervision and inspection, and inefficient implementation plans, these policies and strategies were not successful. Indeed, during the past decade, antimicrobials have remained the most prescribed institutional medicine, and AMR has continued to increase, in some cases dramatically (for example, imipenem-resistant Acinetobacter baumannii) (Figure 1) [3],[11],[12].
Changes in Policy to Promote the Rational Use of Antibiotics
In 2009, a new round of healthcare reforms was initiated in China with the ultimate target of eradicating the “difficulty and high price of seeing a doctor,” and to achieve basic medical security for everyone by 2020. The government increased healthcare spending and promoted healthcare insurance coverage for urban and rural residents. The aim was for the medical establishment to gradually regain its public service role. All these reforms contributed to policies promoting sustainable progress towards the rational use of antimicrobials [13].
In 2011, coupled with healthcare reforms, the Chinese MOH adjusted the reliance on the professional strategies described above and launched a special campaign to reorganize the rational use of antimicrobials in healthcare settings. The campaign protocol mainly consists of establishing mandatory administrative strategies for the rational use of antimicrobials, setting targets for antimicrobial management, organizing task forces, developing audit and inspection systems, and investigating and reassigning responsibility to hospital management staff who violate rational use policies. According to the protocol, all hospitals should have an antibiotic administrative group chaired by the president, formulary restrictions are to be enforced, prescribers have accredited prescription rights for different antibiotic classes determined by their positional titles, and antibiotic procurement should be restricted to 50 or 35 agents in secondary and tertiary hospitals, respectively. Meanwhile, targets for antibiotic prescription are set at less than 60% and 20% of all prescriptions for hospitalized patients and outpatients, respectively; prophylactic use of antibiotics in clean operations should be lowered to 30% of patients and reduced to less than 24 hours' duration; and antibiotic utilization in hospitalized patients should be less than 40 daily defined doses per 100 patient days. All the indicators are linked to hospital quality evaluation procedures and the allocation of future medical resources. Furthermore, adherence to these protocols are to be considered when appointing or dismissing hospital presidents.
To enact these protocols, the Chinese MOH and local health administration signed an administrative target responsibility agreement with major hospital authorities. The Chinese MOH also held several national medical education programs each year and conducted twice yearly inspections (every September and December). According to the protocols, hospitals that fail to meet targets would be downgraded to a lower classification level, and the leaders of the institutes involved would be dismissed. Medical staff who seriously violate the regulations could lose their accreditation to prescribe antibacterial agents, have their professional qualification revoked, or even be prosecuted if their actions have serious consequences [14].
During the past 2 years in China, these policies were enacted with extensive promotion of education and increased levels of supervision. Excellent hospitals were recognized, and failures were criticized in public. Several hospital presidents were dismissed and some clinicians were punished with economic sanctions. A few clinicians also had their prescription rights suspended by health authorities as a result of severe regulatory violations. A gradual return towards the rational use of antimicrobials has begun. According to IMS Research data, the percentage of drug sales (by value) for antimicrobials decreased to 17% in the fourth quarter of 2012 from 25% in 2011, with an associated decrease in the volume of antibiotics sold (Figure 2). Data released by the Chinese MOH indicates that the percentage of prescriptions for antimicrobials decreased from 68% to 58% for hospitalized patients and from 25% to 15% for outpatients. Antimicrobial prophylaxis use associated with clean surgical procedures also decreased from 95% to 58% of cases, with the duration of use shortened from 5 days to less than 48 hours. For example, antibiotic procurement in Tianjin City was 200 million RMB Yuan lower in 2011 than in 2010, although the numbers of outpatient visits, hospitalized patients, and operations increased by 1.4 million, 84,000, and 58,000, respectively [15].
Fig. 2. Quarterly sales volume and the proportion of antimicrobial agents sold in 2010–2012 in China. 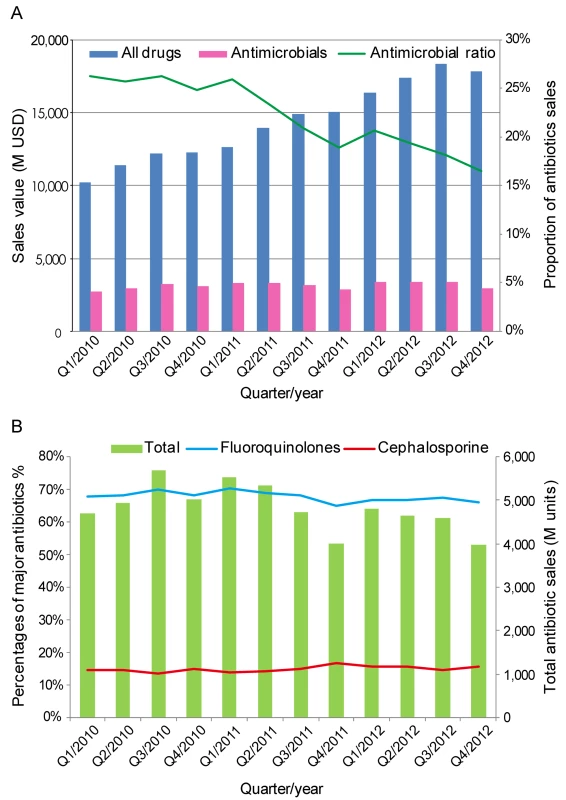
(A) The sales value of all drugs (blue bars) or antimicrobial agents (pink bars) in millions (M) of US dollars (USD) and the proportion of antimicrobial agents sold (green line). (B) The sales volume of all antimicrobial agents in minimal packaging units (green bars) and the percentage of fluoroquinolones (blue line) or cephalosporin sales (red line). Data were adapted from IMS Research. To ensure sustainable progress towards the rational use of antimicrobial agents in healthcare settings, “administrative regulations for the clinical use of antimicrobials” were issued in China in August 2012, in which the concept of “antibiotic stewardship” was integrated into the measures outlined during the special campaign [16]. The legislation considers long-term antibiotic stewardship in Chinese healthcare institutions and is expected to change the current situation in which rational antimicrobial use simply relies on incidental administrative motivation. This “administrative antibiotic stewardship” regulation is implemented by the Chinese MOH. They may also provide a valuable reference for other countries with similar healthcare systems [17].
Further Problems for the Containment of AMR
Although the special campaign launched by the MOH to promote the rational use of antibiotics in healthcare settings has had some success, several factors need to be considered to establish a long-term and nationwide framework for sustainable AMR containment in China. Firstly, several ministries share regulatory oversight of antimicrobial use. The State Food and Drug Administration is responsible for the registration, production, quality control, and distribution of antimicrobials. The Ministry of Agriculture is independently responsible for complete oversight of antibiotic use in animal feed and veterinary care. The MOH exclusively administers the use of antibiotics in healthcare settings. This power-sharing administrative system has a tendency to dilute direct responsibility. New mechanisms should be explored to provide integrated policies to promote the rational use of antibiotics and AMR containment in related fields. Secondly, medical school curricula and continuing medical education should be improved. At present, most medical students in China do not study the relevance of antibiotic therapy to AMR. Thirdly, public education should be provided to ensure that the general public are aware of the risks associated with AMR, which will likely help to reduce over-the-counter sales and self-medication of antibiotics. Finally, and critically, the government should widen the healthcare reforms and provide financial guarantees to medical institutions to ensure that economic incentives from drug sales are eliminated. This will return healthcare institutions to a not-for-profit status and aid professional standards [9],[12],[18],[19].
Zdroje
1. World Health Organization (April 2011) World Health Day-7. Available: http://wwwwhoint/world-health-day/2011/en/indexhtml Accessed 10 March 2013.
2. YezliS, LiH (2012) Antibiotic resistance amongst healthcare-associated pathogens in China. Int J Antimicrob Agents 40 : 389–397.
3. XiaoYH, GiskeCG, WeiZQ, ShenP, HeddiniA, et al. (2011) Epidemiology and characteristics of antimicrobial resistance in China. Drug Resist Updat 14 : 236–250.
4. XiaoYH, ShenP, WeiZQ, ChenYB, KongHS, et al. (2012) Mohnarin report of 2011 : monitoring of bacterial resistance in China. Chinese Journal of Nosocomiology (Zhonghua Yi Yuan Gan Ran Xue Za Zhi) 22 : 4946–4952.
5. DongL, YanH, WangD (2008) Antibiotic prescribing patterns in village health clinics across 10 provinces of Western China. J Antimicrob Chemother 62 : 410–415.
6. ReynoldsL, McKeeM (2009) Factors influencing antibiotic prescribing in China: an exploratory analysis. Health Policy 90 : 32–36.
7. TangS, MengQ, ChenL, BekedamH, EvansT, et al. (2008) Tackling the challenges to health equity in China. Lancet 372 : 1493–1501.
8. ZhuYG, JohnsonTA, SuJQ, QiaoM, GuoGX, et al. (2013) Diverse and abundant antibiotic resistance genes in Chinese swine farms. Proc Natl Acad Sci U S A 110 : 3435–3440.
9. XiaoYH (2012) Building technical support system for antibiotic rational use. Chin J Pract Intern Med 32 : 973–976.
10. World Health Organization (2002) Promoting rational use of medicines: core components. Policy Perspectives on Medicines No 5 2002 Geneva. Available: http://apps.who.int/medicinedocs/en/d/Jh3011e/. Accessed 05 May, 2013.
11. XuJ, SunZ, LiY, ZhouQ (2013) Surveillance and correlation of antibiotic consumption and resistance of Acinetobacter baumannii complex in a tertiary care hospital in northeast China, 2003–2011. Int J Environ Res Public Health 10 : 1462–1473.
12. WangH, LiN, ZhuH, XuS, LuH, et al. (2013) Prescription pattern and its influencing factors in Chinese county hospitals: a retrospective cross-sectional study. PLoS One 8: e63225 doi:10.1371/journal.pone.0063225
13. YipWC-M, HsiaoWC, ChenW, HuS, MaJ, et al. (2012) Early appraisal of China's huge and complex health-care reforms. Lancet 379 : 833–842.
14. China MoH (2011) Protocol for special campaign of antibiotic administrative in healthcare institutions. Ministry of Health, May 8, 2011Beijing.
15. China MoH (10 March 2013) Available: http://www.moh.gov.cn/mohbgt/s3582/201205/54651.shtml. News Conference on May 8, 2012.
16. DellitTH, OwensRC, McGowanJE, GerdingDN, WeinsteinRA, et al. (2007) Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 44 : 159–177.
17. XiaoY, LiL (2013) Legislation of clinical antibiotic use in China. Lancet Infect Dis 13 : 189–191.
18. GuardabassiL, LarsenJ, WeeseJ, ButayeP, BattistiA, et al. (2013) Public health impact and antimicrobial selection of meticillin-resistant staphylococci in animals. Journal of Global Antimicrobial Resistance 1 : 55–62.
19. KhachatouriansGG (1998) Agricultural use of antibiotics and the evolution and transfer of antibiotic-resistant bacteria. Can Med Assoc J 159 : 1129–1136.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 11- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Antikoagulační léčba u pacientů před operačními výkony
-
Všechny články tohoto čísla
- Antenatal Syphilis Screening Using Point-of-Care Testing in Sub-Saharan African Countries: A Cost-Effectiveness Analysis
- From Ideals to Tools: Applying Human Rights to Maternal Health
- Interactions between Non-Physician Clinicians and Industry: A Systematic Review
- Harnessing Poverty Alleviation to Reduce the Stigma of HIV in Sub-Saharan Africa
- Integrating Health Care to Meet the Needs of the Mother–Infant Pair: A Call for Papers for Year 3 of the Maternal Health Task Force–PLOS Collection
- Changes in Chinese Policies to Promote the Rational Use of Antibiotics
- Same Song, Different Audience: Pharmaceutical Promotion Targeting Non-Physician Health Care Providers
- A Gene Expression Signature for RSV: Clinical Implications and Limitations
- Global Research Priorities to Better Understand the Burden of Iatrogenic Harm in Primary Care: An International Delphi Exercise
- Measles Outbreak Response Immunization Is Context-Specific: Insight from the Recent Experience of Médecins Sans Frontières
- Global Mortality Estimates for the 2009 Influenza Pandemic from the GLaMOR Project: A Modeling Study
- When to Start Antiretroviral Therapy in Children Aged 2–5 Years: A Collaborative Causal Modelling Analysis of Cohort Studies from Southern Africa
- Burden of Depressive Disorders by Country, Sex, Age, and Year: Findings from the Global Burden of Disease Study 2010
- Role of DNA Methylation and Epigenetic Silencing of in Endometrial Cancer Development
- Characterization of Regional Influenza Seasonality Patterns in China and Implications for Vaccination Strategies: Spatio-Temporal Modeling of Surveillance Data
- Whole Blood Gene Expression Profiles to Assess Pathogenesis and Disease Severity in Infants with Respiratory Syncytial Virus Infection
- Complex Disease Dynamics and the Design of Influenza Vaccination Programs
- A Brief Patient-Reported Outcomes Quality of Life (PROQOL) Instrument to Improve Patient Care
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- A Brief Patient-Reported Outcomes Quality of Life (PROQOL) Instrument to Improve Patient Care
- Burden of Depressive Disorders by Country, Sex, Age, and Year: Findings from the Global Burden of Disease Study 2010
- From Ideals to Tools: Applying Human Rights to Maternal Health
- Role of DNA Methylation and Epigenetic Silencing of in Endometrial Cancer Development
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



