-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Pleiotropic Effects of Immune Responses Explain Variation in the Prevalence of Fibroproliferative Diseases
Many diseases are differentially distributed among human populations. Differential selection on genetic variants in ancestral environments that coincidentally predispose to disease can be an underlying cause of these unequal prevalence patterns. Selected genes may be pleiotropic, affecting multiple phenotypes and resulting in more than one disease or trait. Patterns of pleiotropy may be helpful in understanding the underlying causes of an array of conditions in a population. For example, several fibroproliferative diseases are more prevalent and severe in populations of sub-Saharan ancestry. We propose that this disparity is due to selection for an enhanced Th2 response that confers resistance to helminthic infections, and concurrently increases susceptibility to fibrosis due to the profibrotic action of Th2 cytokines. Many studies on selection of Th2-related genes for host resistance to helminths have been reported, but the pleiotropic impact of this selection on the distribution of fibrotic disorders has not been explicitly investigated. We discuss the disproportionate occurrence of fibroproliferative diseases in individuals of African ancestry and provide evidence that adaptation of the immune system has shaped the genetic structure of these human populations in ways that alter the distribution of multiple fibroproliferative diseases.
Published in the journal: . PLoS Genet 11(11): e32767. doi:10.1371/journal.pgen.1005568
Category: Review
doi: https://doi.org/10.1371/journal.pgen.1005568Summary
Many diseases are differentially distributed among human populations. Differential selection on genetic variants in ancestral environments that coincidentally predispose to disease can be an underlying cause of these unequal prevalence patterns. Selected genes may be pleiotropic, affecting multiple phenotypes and resulting in more than one disease or trait. Patterns of pleiotropy may be helpful in understanding the underlying causes of an array of conditions in a population. For example, several fibroproliferative diseases are more prevalent and severe in populations of sub-Saharan ancestry. We propose that this disparity is due to selection for an enhanced Th2 response that confers resistance to helminthic infections, and concurrently increases susceptibility to fibrosis due to the profibrotic action of Th2 cytokines. Many studies on selection of Th2-related genes for host resistance to helminths have been reported, but the pleiotropic impact of this selection on the distribution of fibrotic disorders has not been explicitly investigated. We discuss the disproportionate occurrence of fibroproliferative diseases in individuals of African ancestry and provide evidence that adaptation of the immune system has shaped the genetic structure of these human populations in ways that alter the distribution of multiple fibroproliferative diseases.
Prevalence of Fibroproliferative Diseases in Individuals of African Ancestry
Fibroproliferation is a response to tissue injury in which fibroblast-like cells under the influence of immune modulators proliferate and produce extracellular matrix components to heal a wound. Aberrant regulation may result in excessive accumulation of matrix components, i.e., fibrosis. This pathological process, which can occur in multiple tissues, is a common response to injury that leads to scarring and dysfunction of injured tissue and sometimes death [1]. Dermal fibrosis can result in keloids or other types of hypertrophic scars; fibrosis in the kidney, liver, and lung can result in end-stage disease. Fibrosis is also seen in autoimmune diseases, including scleroderma, sarcoidosis, systemic lupus, and in airway remodeling in asthma. Disorders whose pathophysiology is characterized by an exaggerated response to injury are referred to as fibroproliferative diseases. An increased incidence of fibrosis has been widely observed in black populations and has been termed a fibroid [2] or fibroplastic diathesis [3–5]. Fibroid diathesis is used to describe processes in which growth is an essential characteristic, and it depends for the most part on changes caused by inflammation. As a rule, the starting point is tissue injury. “As the element of heredity seems to enter largely into these changes, perhaps the term fibroid diathesis may be admissible as expressing the inherent tendency to this class of changes” [2].
In a series of articles, Anthony P. Polednak suggested that adaptation to the tropical environment in Africa may have involved a tendency toward connective tissue overgrowth as well as hyperpigmentation, and that both tendencies may affect susceptibility to several chronic diseases and response to disease or drug therapies [6–8]. A subset of fibroproliferative disorders that occur at higher frequency and/or with more severe manifestations in people of African ancestry is listed in Table 1. These include keloids [9], glaucoma [10,11], hypertension [12,13], nephrosclerosis [14], scleroderma [15], sarcoidosis [16], uterine fibroma [17], and allergic diseases, including asthma [18–21].
Tab. 1. Relative frequencies of certain fibroproliferative diseases in black and white populations. 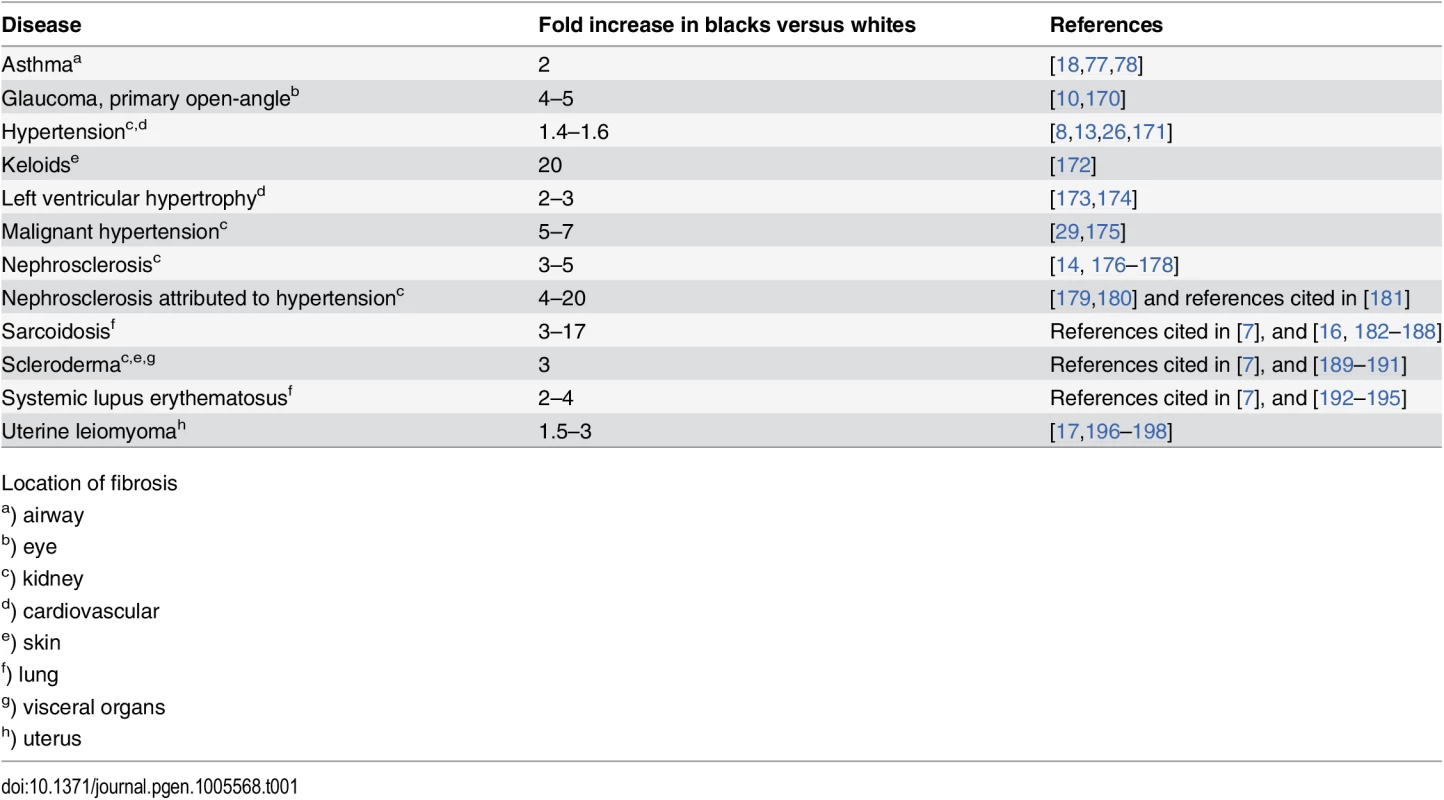
Location of fibrosis Not all fibrotic disorders show increased prevalence in blacks; such inconsistencies are probably due to a variety of etiologies. In the subset of fibrotic disorders listed in Table 1, different organ systems are affected. In keloids, the dermis alone is involved, whereas in scleroderma there is life-threatening fibrosis of skin and visceral organs with a higher prevalence of renal crisis in African Americans [22]; in sarcoidosis any organ system may be involved but severe pulmonary fibrosis is more prevalent in individuals of African descent [23].
There is strong evidence for a genetic role in fibroproliferative disorders, although in most cases they are genetically complex. Genome-wide linkage studies and targeted genome scans have implicated common loci for several fibroproliferative diseases that may have been selected in a similar environment [24]. We [25], and others [7,14,26–29], have suggested that a common etiopathology may operate in these diseases, and common genetic factors may account for their unusual distribution. We propose that the increased prevalence of fibroproliferative diseases in individuals of African ancestry is due to selective pressure for an elevated Th2 response that confers resistance to helminthic infections and concomitantly increases susceptibility to fibrosis.
Cytokine Profile for Fibrosis
In the late 1980s it was shown, using a panel of mouse CD4+ T cells, that two groups of T helper (Th) lymphocytes produced distinct cytokine patterns [30]. Early evidence that Th2 cytokines were profibrotic came from experiments in which administration of IL12, a cytokine that primes Th1 immunity and blocks Th2 immunity, prevented fibrosis in a mouse model of schistosomiasis [31]. The role these cytokines played in the fibrotic response was further supported in studies using mouse models that polarized to either a Th1 or Th2 response to wounding. Using inbred strains of mice that differed in sensitivity to murine leishmaniasis—a Th1-responsive disorder caused by the intracellular trypanosomatid protozoan Leishmania chagasi—it was found that polarization of the immune response toward Th1 or Th2 is under genetic control (reviewed in [32,33]). In C57BL/6 mice that are resistant to leishmanial infection, the Th1 cell population expanded and produced IFNγ, whereas susceptible BALB/c mice exhibited a Th2 response characterized by production of IL4. As seen in Table 2, several different exposures induced a fibrotic phenotype in BALB/c but not in C57BL/6 mice.
Tab. 2. Response to exposure by mouse strain. 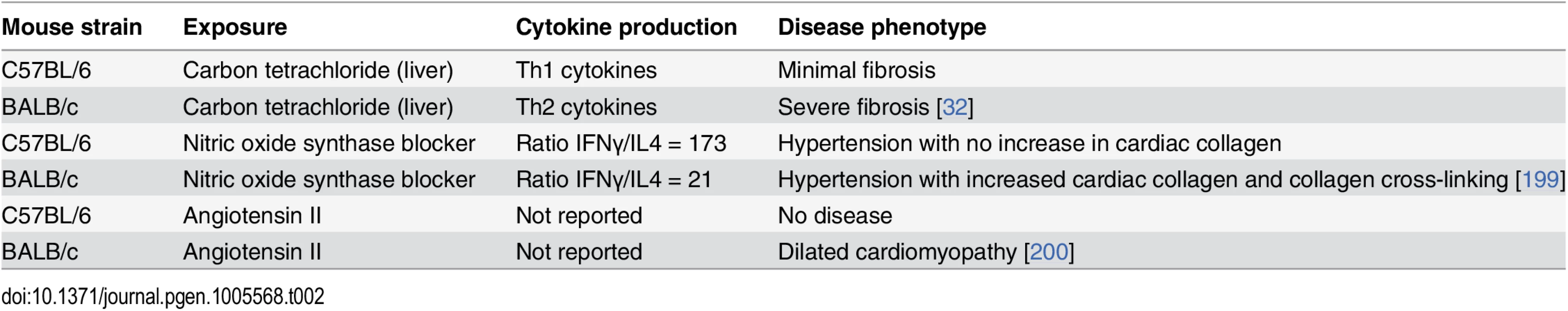
In the carbon tetrachloride study, strains of mice that lacked IFNγ defaulted to a Th2 response and developed fibrosis, whereas treatment with anti-IL4 or IFNγ prevented fibrosis, even in BALB/c mice [32]. When the immune response to infection with Schistosoma mansoni or to injection with soluble egg antigen was compared between wild type C57BL/6 mice and mice genetically engineered to be deficient in Th1 or Th2 cytokines and/or Th10, Th2 cytokines were profibrotic while Th1 cytokines were inflammatory. Mortality due to either Th1 - or Th2-related pathologies was regulated by IL10, which suppressed the production of both type 1 and type 2 cytokines [34]. Gene expression profiling in liver [35] and lung [36] revealed similar results: Th2-polarized mice overexpressed genes involved in fibrogenesis and wound repair, whereas Th1-polarized mice overexpressed genes associated with inflammation-induced tissue damage.
Th2 cytokines also play an important role in human fibrosis [1,37,38]. IL4 and IL13 increase collagen synthesis in human fibroblasts [39–43]; they also promote fibrocyte differentiation from a subset of peripheral blood monocytes. In contrast, the antifibrotic Th1 cytokines IFNγ and IL12 inhibit fibrocyte differentiation [44]. Increased levels of type 2 cytokines have been observed in patients with pulmonary fibrosis [45,46] and hepatic fibrosis [47,48]. Decreased levels of the antifibrotic Th1 cytokines IFNγ and IFNα have been reported for African Americans with keloids compared to those without keloids [49]. While Th2 cytokines were not measured in this study, an increased level of IL6 was observed; IL6 has been shown to promote Th2 differentiation and inhibit Th1 differentiation [50]. An enhanced Th2 response in keloid patients is also supported by: (1) an increased keloid incidence in high school students with allergies [51]; (2) a reduction in collagen synthesis in keloid and scleroderma fibroblasts by Tranilast, a drug developed to control allergies [52,53]; and (3) a correlation of excessive scar formation with IgE levels [54]. Patients with progressive systemic sclerosis also exhibit a predominant type 2 response, which accounts for the endothelial cell injury, fibrosis, and autoantibody production in this disease [55,56]. Mutations in IL13Rα2, a decoy receptor that serves as an off-signal for IL13 [57,58], are associated with systemic sclerosis [59].
Immunity to Helminths
Helminths are parasitic worms that cause the most common infectious diseases of humans in developing countries. It is estimated that one billion people in developing areas of sub-Saharan Africa are infected with at least one helminth (Fig 1) [60]. These worms represent a highly diverse group of multicellular eukaryotic parasites, consisting of two phyla, Nematoda, and Platyhelminthes. Infection by any of these parasitic worms, including schistosomes, hookworms, and ascaris, induces a Th2 immune response [60,61]. This response includes the production of cytokines IL4, IL5, and IL13, antibody isotypes IgG1, IgG4, and IgE, and expanded populations of eosinophils, basophils, mast cells, and IL4 - and IL13-activated (alternatively activated or M2) macrophages (Fig 1) [61,62]. The adaptive Th2 response mirrors a range of innate helper cell responses that occur upon parasite invasion of epithelium [62]. Interestingly, helminth diversity was observed to correlate with 3,478 gene variants in more than 800 genes in complex networks centered around Th2 cytokines [63]. Th2 immunity is enhanced in environments with a high prevalence of helminthic infection, and may have evolved to isolate and encapsulate the organism and resolve localized extracellular damage [64]. This process can result in tissue injury due to an excess deposition of extracellular matrix, i.e., fibrosis [62,64].
Fig. 1. Helminth exposure selects for a protective Th2 immune response that simultaneously increases risk for fibrosis. 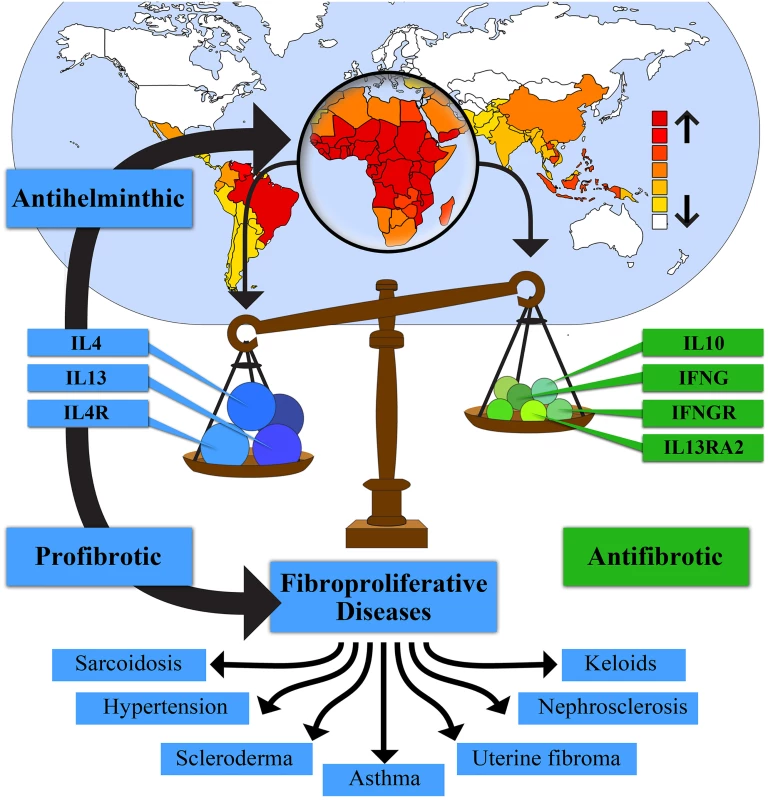
The high prevalence of helminths in Africa has selected for genotypes favoring an enhanced Th2 immune response characterized by increased levels of interleukin 4 (IL4), interleukin 13 (IL13), and interleukin 4 receptor (IL4R), and other Th2 factors. This selection also decreases Th1 factors, such as interferon gamma (IFNG) and interferon gamma receptor (IFNGR), and Th2 regulatory factors, such as IL10 and interleukin 13 receptor alpha 2 (IL13RA2). These genotypes increase resistance to helminthic infection and contribute to a subset of fibroproliferative diseases that are more common and/or more severe in individuals of African ancestry. Global distribution of helminth species in upper part of figure adapted from Lustigman et al. [168]. Controlling the Th2 response is imperative to avoid excessive host scarring and other pathological effects. It may also benefit the parasite by damping the immune response, thereby permitting the chronic nature of most helminthic infections. Helminthic infections promote down-regulation of the immune response by expanding populations of immune regulatory cells, including alternatively activated macrophages, Treg cells, and regulatory B cells, by production of IL10 and TGFβ, and by suppression of Th17 [65–68].
The immune response to helminths shares key features with the allergic response. Both are characterized by high levels of IL4, IL5, and IL13, eosinophilia, and abundant IgE production. Several investigators have proposed that a genotype that confers resistance to helminths increases susceptibility to diseases such as allergies, asthma, and autoimmune disease when helminths are not present [69–74]. This is supported by the observation that the geographic distribution of helminth parasitism and allergic disease are complementary [69,75,76], in contrast to the coincident distribution of sickle cell disease and malaria. The prevalence and severity of allergic airway disease are both disproportionately high among African Americans, even after adjustment for demographic and socioeconomic factors [18–21,77,78]. Also consistent are reports of a higher prevalence of atopic dermatitis and elevated IgE levels in individuals of African descent compared with European descent [21,79,80].
During chronic infection, mechanisms that down-regulate both Th1 and Th2 immunity reduce allergic and autoimmune reactions and other pathological effects of the Th2 response, including fibrosis [65–68,81]. Therefore, what we and others argue has been selected historically to deal with parasites may produce an increased fibrotic disease burden in a relatively helminth-free environment where the muted response does not occur. Thus, in the absence of helminthic control mechanisms, individuals genetically predisposed to an increased Th2/Th1 ratio might produce a damaging excess of Th2 cytokines and demonstrate increased incidence and severity of fibroproliferative disease. While direct evidence that helminth infection impacts fibrosis is lacking—save for the complementary distribution of helminth parasitism and asthma (a fibroproliferative disease)—our hypothesis should stimulate research to determine whether this is indeed the case.
Considerable emphasis has been placed on identifying Th2-related genes common to host resistance against helminths and asthma [82–84], but association of such genes with fibrotic disorders that occur with disproportionately high frequency in individuals of African ancestry is lacking. Yet there is support for the notion that Th2 immunity evolved as a rapid repair mechanism in response to extracellular pathogens [64], and that an increased ratio of Th2 to Th1 cytokine responses after injury leads to fibrosis. Moreover, asthma itself is a fibroproliferative disease. As asthma becomes more severe, the airway environment is similar to a chronic wound characterized by secretion of growth factors that induce smooth muscle proliferation, angiogenesis and fibrosis [85,86]. Numerous studies have shown that increased airway wall thickening that includes subepithelial fibrosis results in increased disease severity, including near-fatal and fatal asthma (references cited in [86]).
Genetics of Resistance to Helminthic Infections
Epidemiological studies in the late 20th century showed that susceptibility to helminthic infection, as defined by worm burden, is a heritable trait with the proportion of variance attributed to genetic effects varying from 0.21–0.44 (reviewed in [70]). Evidence for a genetic predisposition to infection was also provided by ethnic variation in susceptibility, familial aggregation, and individual variation. Differences in susceptibility to helminth infection between ethnic groups was noted early in the 20th century in studies in the southern United States, where a much higher prevalence and intensity of hookworm infection was observed in people of European than African ancestry [87–89]. Additional evidence came from studies that separated effects of relatedness and shared households by statistically analyzing large pedigrees across many households [90].
Identification of specific genes that associate with infection susceptibility provided evidence that immune-related, and especially Th2-related genes, tended to associate with helminth infection. The first genome scans for a parasitic disease associated a major locus that mapped to chromosome region 5q31-q33 with resistance to S. mansoni infection. This region is rich in Th2 cytokine and Th2 cytokine-related genes [91–93]. A genome study of ascaris infection intensity identified two chromosomal regions, 13q32-q34 and 1p32. TNFSF13B, which encodes B lymphocyte stimulator protein and hence is a player in the Th2 response, is in the 13q32-q34 region; this locus also associates with total IgE levels (cited in [70]).
Analysis of Schistosoma haematobium infection in Mali revealed that in chromosomal region 5q31-q33, polymorphisms in the IL13 gene promoter at −1055 and −591 were associated with the infection rate: alleles −1055C and −591A were preferentially transmitted to children with the 10% highest infection rate, whereas −1055T associated with the lowest infection levels [94]. The protective −1055T allele associated with increased IL13 transcription [95,96] and with resistance to reinfection in a Kenyan cohort [97]. In the latter study, it was also found that the IL4 −590T allele associated with high IgE, and the IFNγ +874T allele associated with high IFNγ production; both increased resistance. Another study in Mali revealed an association between a single-nucleotide polymorphism in the STAT6 gene at 12q13.3 and intensity of infection by S. haematobium; this polymorphism had an additive effect with IL13 −1055 [98].
While most genetic studies of susceptibility to helminth infection have focused on infection intensity, variation in pathology has also been reported, even in the absence of differences in infection intensity. Differences in severity of schistosomal pathology between people of African and European ancestry have been observed in Brazil, with individuals of European ancestry showing increased susceptibility to severe, inflammation-induced pathology [99,100]. A 5-fold increased risk of hepatosplenic disease was observed, despite similar egg counts [101]. Severe hepatosplenism in humans is associated with high levels of Th1 cytokines and low levels of the Th2 cytokine IL5 [102]. Severe disease has been reported more recently to involve elevated levels of the proinflammatory and profibrotic cytokine IL17, produced by Th17 cells [103,104]. However, mutations in the gene encoding the antifibrotic Th1 cytokine IFNγ or its receptor may be important in combating other immunopathological effects caused by Th2 cytokines [105–107]. Individuals with low levels of IFNγ have been reported to be susceptible to severe fibrosis, whereas high levels correlated with reduced fibrosis [107]. Studies in a Sudanese population supported the presence of a major codominant gene controlling hepatic fibrosis in schistosomiasis. Severe hepatic fibrosis due to S. mansoni infection was also associated with variation at 6q22-23, close to the gene for the IFNγ receptor α chain (IFNGR1) [108]. Two polymorphisms (+2109A/G and +3810A/G) in intron 3 of the IFNγ gene were associated with periportal fibrosis: the 2109G allele with severe fibrosis, and 3810A with protection from fibrosis. Other studies indicate that 2109G decreases IFNγ expression, whereas 3810A increases it [106].
Evidence for an Immune Adaptation for Resistance to Helminths in Individuals of African Ancestry
As hypothesized by Le Souef et al. [72], “Modern man’s ancestors lived in an environment where infectious tropical diseases would have been endemic.” They postulated that, in this hostile environment, genetic selection for increased Th2 immune responses occurred. In more temperate areas, these pronounced responses would have been less important (and selected against) due to increased mortality from overly vigorous responses to harmless or less common environmental agents. They reviewed evidence that alleles resulting in a heightened Th2 response in several genes, such as IL4, IL4R, and the IgE receptor, are more prevalent in populations with long-term tropical ancestry than in those with long-term residence in temperate regions.
Little has been done to directly determine whether healthy Africans or African Americans exhibit a Th2-biased response. In one small study comparing healthy African children and adults from the Gabonese rain forest to healthy European children and adults from Austria, Wilfing et al. reported an increased frequency of both Th1 - and Th2-cytokine-producing T cells in African versus European adults; however, whereas CD4+ cells expressing the type 1 cytokines IL2 and IFNγ expanded in both African and European adults, CD4+ cells expressing the type 2 cytokines IL4 and IL13 expanded only in African adults [109]. Although these data are consistent with our hypothesis, more extensive studies are needed to determine whether healthy individuals with African ancestry skew toward a Th2 immune response relative to Th1 and Th17 responses.
More recent studies of a subset of genes, and population studies such as 1,000 Genomes [110] and HapMap [111], have supported increased prevalence of alleles associated with resistance to helminths and concomitant susceptibility to fibrosis in West African (YRI), and African American (ASW) populations relative to individuals of Northern European descent (CEU). Of particular interest are polymorphisms in IL4, IL4R, IL13, IL13RA1, IL13RA2, IFNG, IFNGR1, and IL10, described below and in Table 3, which occur with higher frequency in the recent African descent populations. We also note that allele frequencies in Th2 genes differ more on average between West African and European populations than do differences genome-wide (Fig 2A), supporting the hypothesis that these loci have been exposed to different patterns of selection. Of note, these differences are more pronounced than differences between Th1 genes and the genomic background (Fig 2B and 2C). The frequencies of polymorphisms in East Africa (LWK) seen in 1,000 Genomes are generally similar to YRI. Many of these similarities are also observed in Asian descent populations (S2 Table). Most variants in Th2 and Th1 genes also differ more among these human populations than the genomic background (S1 Fig). However, except for evidence of increased keloid formation in these populations, data on prevalence of fibroproliferative diseases and/or helminthic infection prevalence are too limited to extend our hypothesis beyond Western Africans and African Americans.
Tab. 3. Population-specific allele frequencies (1,000 Genomes, 16 October 2014 release). 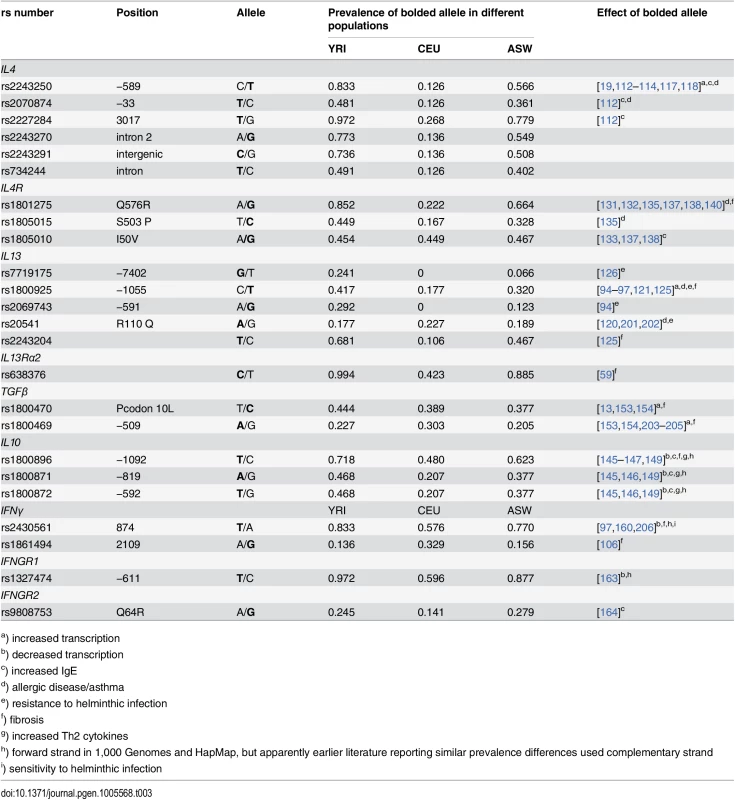
a) increased transcription Fig. 2. Pattern of differences between YRI and CEU HapMap populations, as determined by Fst between SNPs. 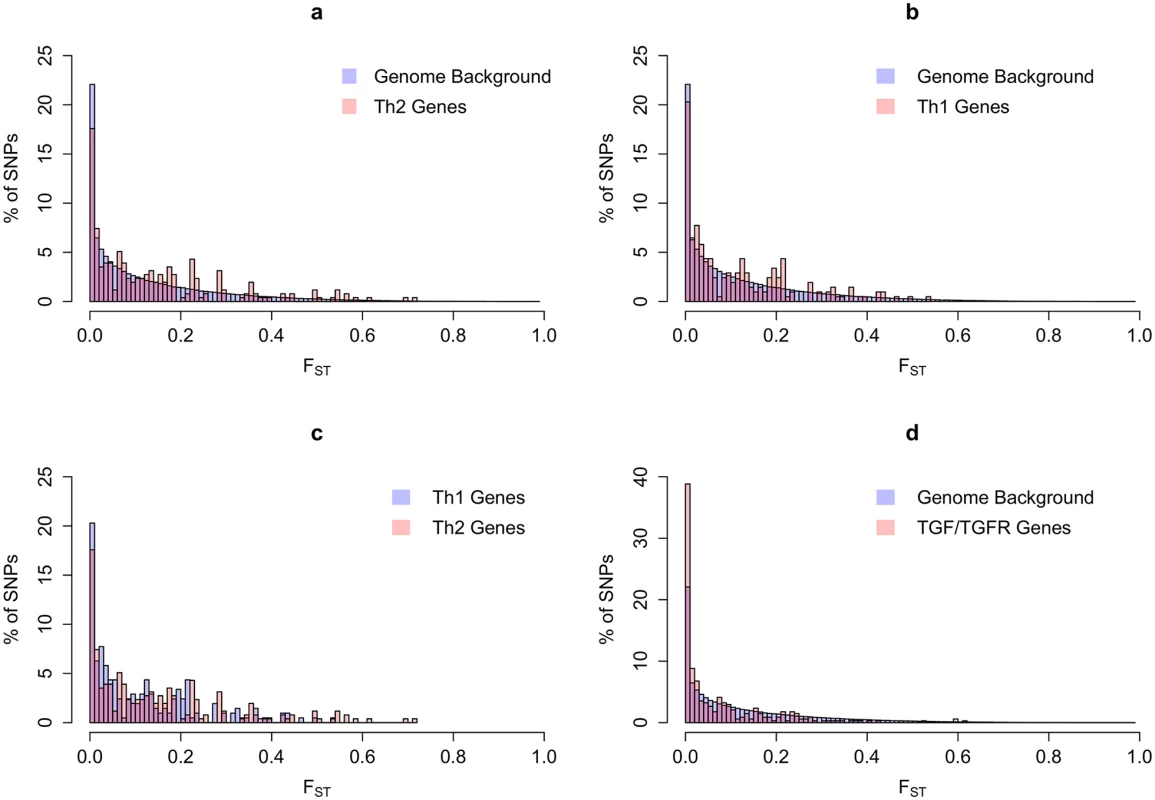
(A) Th2 variants compared to background (18 genes and 256 SNPs); (B) Th1 variants compared to background (14 genes and 207 SNPs); (C) A comparison of Fst values for Th2 as compared to Th1 SNPs); (D) TGFβ and TGFβ-receptor variants, as compared to background (6 genes and 340 SNPs). Fst was calculated using the method of Weir and Cockerham [169] and varies from zero (when two populations have identical allele frequencies of a given SNP) to one (when they are fixed for different alleles). Genes used for these analyses are listed in S1 Table. Interleukin 4
IL4 plays a major role in Th2 differentiation. It induces immature T cells to assume a Th2 phenotype and represses Th1-inducing signals. As a downstream effector, it acts on B cells to produce IgE. Polymorphisms in IL4 have been associated with increased total serum IgE levels, atopy, and asthma in some populations, but not in others [112–114]. Importantly, IL4 polymorphisms that associate with asthma severity and elevated IgE in individuals of European descent are more frequent in African Americans than in European Americans (Table 3) [18,19,114,115]. Recent studies have also pointed to a role for private IL4 mutations in African Americans that may be associated with asthma susceptibility [116]. Somewhat surprisingly, three of the most well-studied of these polymorphisms, at −33, −589, and +3017, associate with asthma and/or elevated IgE in individuals of European descent but not in African populations (Table 3) [19,112–114]; the lack of association at −589T and +3017 in African populations may be due to their high frequency in these populations. Because −589T also associates with expression variation, it provides a putative mechanism to explain the variable patterns of association [117–119]. For example, −589T contributes to lower baseline values of forced expiratory volume (FEV) and higher IgE levels observed in individuals of African descent [21,79,80] and probably the increased prevalence of fibroproliferative disease.
Interleukin 13
IL13 plays a major role in promoting fibrosis in asthma and schistosomiasis [94,96,97,120,121]. It signals through a common pathway with IL4 [122,123]. Polymorphisms in IL13 and IL13Rα1 have been associated with asthma and elevated IgE [57,120,121]. The decoy receptor IL13Rα2 down-regulates IL13 signaling and reduces fibrosis [57,58,124]. As indicated above, −1055T in the IL13 gene promoter (rs1800925) correlates with different rates of infection in Mali and Kenya [94,97]. This allele, which is associated with lowest infection levels, has also been associated with allergic inflammation, an increased rate of IL13 transcription [95,121], and systemic sclerosis in individuals of European descent [125]. As seen in Table 3, the T allele is more common in YRI and ASW than in CEU. Also protective against schistosomiasis and occurring at higher frequency in populations of African ancestry is a G allele at a second promoter site (rs771975). These two SNPs are in linkage disequilibrium (LD), making a mechanistic conclusion difficult [126], but haplotype analysis revealed that homozygotes for the doubly protective haplotype TG were less likely to be infected than other subjects. The G allele of a third polymorphism in the IL13 promoter at −591A/G (−646), rs2069743, was also protective and is present at 33% and 12.3% in YRI and ASW 1,000 Genomes populations, respectively, but is not seen in populations of European descent [94]. A fourth polymorphism, located in the 3’UTR of IL13, rs2243204, has been associated with systemic sclerosis in individuals of European ancestry [125]; here too, the risk allele T occurs at higher frequency in African and African-American populations (Table 3). In addition to polymorphisms in IL13, a polymorphism in IL13Rα2 associated with systemic sclerosis in individuals of European ancestry [59] occurs with higher frequency in individuals of African ancestry (Table 3).
IL4 Receptor
Both IL4 and IL13 signal through a common pathway by binding to the heterodimeric IL4 receptor (IL4R) composed of the IL4Rα chain and either the common γc chain or the IL13Rα chain. Signaling via IL4Rα plays a critical role in the pathogenesis of asthma [127], with more than a dozen polymorphisms in the gene contributing to asthma risk [128–135]. Several of these susceptibility alleles are more common in African Americans [136–139]. Of particular interest is rs1801275, which causes a glutamine to arginine change at position 576 in the receptor α chain. Arginine at this position is associated with altered IL4 signaling, a shift of the Th1/Th2 balance toward Th2, and susceptibility to asthma and several connective tissue disorders, including systemic lupus and scleroderma [139,140]. The risk allele has a 68% frequency in African Americans but only 20% in populations of European ancestry [137]. Other data demonstrate this allele frequency difference (Table 3) [138]. A nearby variant, rs1805015, which causes a serine to proline change at position 501 associated with atopy [141], is also more prevalent in African Americans, but a third atopy-associated allele (rs1805010) is not (Table 3). While individual alleles are pathogenic, susceptibility is increased by multiple mutations in the IL4Rα gene, creating risk haplotypes that are more prevalent in African Americans [138]; these interact with other mutations that influence Th1/Th2 activity, such as those that occur with increased frequency in IL13 [141].
Interleukin 10
IL10 is a major immunoregulatory cytokine that downregulates both Th1 and Th2 activity [68,142]. It is effective in preventing fibrosis in several model systems, and suppresses synthesis of procollagen by human scar-derived fibroblasts (cited in [37]). Overexpression of IL10 promotes scarless wound-healing in adult mice [143]. In studies of S. mansoni infection, severe periportal fibrosis is associated with low concentrations of IL10 and IFNγ [144]. IL10 promoter haplotypes that include polymorphisms at −1082, −819, and −592 have altered rates of transcription. Alleles causing low IL10 expression are associated with elevated IgE [145] and increased Th2 cytokines [146]. Allele −1082A is predictive of increased periportal fibrosis in S. mansoni infection [147]. Population studies have revealed significant differences in the proportion of high or low producer genotypes in populations of European descent versus African Americans [148,149]. A study by Delaney et al. yielded similar results [150]. The combined frequency of low-expression genotypes was significantly higher in African Americans than in European Americans, while the frequency of high expression genotypes in African Americans was less than half that in European Americans. Recently, 1,000 Genomes data confirmed the increased abundance of alleles at promoter sites −1082, −819, and −592 that decrease transcription of IL10 in YRI and ASW compared to CEU (Table 3). These data support a major role for IL10 in preventing fibrosis by down-regulating Th2 cytokines. Thus, the increased frequency of low IL10 expression genotypes in individuals of African ancestry supports selection for an enhanced Th2 response in this population.
Transforming Growth Factor β
Increased TGFβ is a component of helminth-mediated down-regulation of the Th2 response [65,71]. While muting the response might be expected to reduce Th2-mediated fibrosis, TGFβ itself promotes a variety of fibrotic conditions [151,152]. Two polymorphisms in TGFβ1, −509, and +869, which elevate plasma levels of TGFβ1, increase the severity of cystic fibrosis [153] and familial pulmonary hypertension [154]. It has been hypothesized that overexpression of TGFβ1 contributes to increased morbidity in African Americans [155]. Plasma levels of TGFβ1 in hypertension and end-stage renal disease are higher in African Americans [13,14], and higher levels of TGFβ1 have been reported in normotensive African Americans than in normotensive European Americans. In these studies the +869 variant, encoding a proline, was associated with higher levels of TGFβ1 mRNA and protein, and was initially reported to be more frequent in African Americans [13]. However, increased prevalence was not observed in the 1,000 Genomes database (Table 3). Moreover, the −509 polymorphism associated with increased TGFβ1 is more common in CEU than ASW or YRI (Table 3) [156]. While the TGFβ1 promoter is highly polymorphic, frequencies of different polymorphisms do not differ among racial groups [157]. Several rare variants are present only in individuals with African ancestry but their effects on expression have not been determined [157]. The failure to observe racial differences in frequency of TGFβ polymorphisms and the presence of two common polymorphisms in TGFβ1 that increase expression but are not more prevalent in individuals with African ancestry suggest that, while TGFβ1 contributes to fibrosis in multiple populations, increased expression does not directly account for the higher incidence of fibroproliferative diseases in African Americans.
Interferon γ
Several antifibrotic effects have been attributed to IFNγ, the prototypic Type 1 cytokine. It inhibits fibroblast proliferation and collagen deposition, promotes fibroblast apoptosis, and inhibits the production and profibrotic action of TGFβ (reviewed in [38]). It inhibits development of fibrosis in vivo [158], and reduces the extracellular matrix in animal models of fibrosis [159]. Decreased levels of IFNγ have been observed in the blood of keloid patients [49]. In a Sudanese population infected with S. mansoni, low levels of IFNγ were associated with severe fibrosis, whereas high levels correlated with reduced fibrosis [107]. However, high levels of IFNγ have been reported to be protective against infection with S. mansoni [97].
In 1999, Pravica et al. identified a polymorphism in intron 1 at position +874 of IFNγ, and found that the A allele at this position correlated with a higher copy number of CA repeats that altered an NFkβ binding site, resulting in decreased IFNγ production [160]. Several studies reported that African Americans have a higher frequency of the allele that decreases production than do European Americans (Table 3) [148,150,161,162]. In Delaney et al. [150], the risk allele frequency was 0.804 in an African American population and 0.61 in a European American population, and was also higher in YRI and ASW (Table 3). As described previously, two polymorphisms, +2109A/G (rs1861494) and +3810A/G, in intron 3 of the IFNγ gene associated with periportal fibrosis in a Sudanese population: the 2109G allele decreased IFNγ expression and correlated with severe fibrosis, whereas 3810A increased IFNγ expression and protected from fibrosis [106]. Somewhat surprisingly, the 2109G allele that associated with low IFNγ production was more frequent in CEU (0.33) than in YRI (0.14) or ASW (0.16) (Table 3). The effect of these alleles on resistance to infection has not been reported; however, high levels of IFNγ have been associated with resistance to infection, suggesting that the low prevalence of the 2109G fibrosis risk allele in African populations may be protective against infection [97].
IFNγ Receptor (IFNGR)
IFNGR is a heterodimer consisting of two chains—IFNGR1 encoded on chromosome 6 and IFNGR2 on chromosome 21. Mutations in IFNGR1 have been reported to affect fibrosis. Studies in a Sudanese population indicated that a major codominant locus controlling hepatic fibrosis in schistosomiasis was at 6q22-q23, close to the gene for the IFNGR1 chain [108]. Six polymorphisms in the IFNGR1 promoter region associated with pulmonary mycobacterial disease [163]. Two (−611 and −56) were polymorphic in all study populations, which included African Americans, Europeans, and Koreans. The −611 polymorphism associated with decreased IFNGR1 expression was approximately 1.5 times more common in African Americans than in European Americans. Similar differences in frequency among YRI, ASW, and CEU were seen in 1,000 Genomes (Table 3). A polymorphic allele in IFNGR2 associated with increased IgE was also more common in Africans and African Americans than in Europeans (Table 3) [164].
Differentiation between African and European Populations with Respect to Th2, Th1 and TGFβ Genes
As documented above, selection has enhanced Th2 gene expression in populations from sub-Saharan Africa that, we argue, is in response to a greater burden of helminthic infections. As a further consequence of this selection, we predict that Th2 alleles will vary more between sub-Saharan populations and European populations than the genomic background. We tested this assumption using the metric, Fst, which represents a measure of genetic differentiation (Fig 2). Consistent with our hypothesis, Th2 gene SNPs represent an enrichment of variants that differ more between sub-Saharan and European populations than does the genetic background (Fig 2A). Differentiation among Th1 gene SNPs appears to follow more closely the genome-wide patterns (Fig 2B and 2C). This comparison includes all SNPs in Th1 and Th2 genes without considering their function. In contrast to the findings for Th2 and to a lesser extent for Th1 genes, differentiation of TGFβ genes and their receptors between populations appears to be identical to the genomic background (Fig 2D).
In summary, individuals of African ancestry have an increased incidence of fibrotic disorders. While the distribution of these diseases supports a genetic contribution, the disorders themselves do not confer a selective advantage. We argue that this pattern of variation can be explained by selection for resistance to diseases caused by helminthic worms prevalent in sub-Saharan Africa. Resistance is achieved by a shift in the immune system toward an enhanced Th2 response to injury that coincidentally results in fibrosis. The exaggerated response to tissue injury resulting in fibrosis can be accounted for in large part by genes that cause increased expression or functionality of Th2 cytokines and their receptors, decreased expression of IL10, and decreased activity of antifibrotic cytokines and receptors of the Th1 system. The allelic distribution of variants that affect the Th2 response are highly concordant with this hypothesis; there is greater differentiation in variants in Th2-related genes compared to the genetic background between African and non-African populations, an observation consistent with selection favoring Th2 enrichment in Africa. While the fibrotic side effects of an increased Th2/Th1 cytokine ratio are a serious consequence, in regions where helminths are common, these side effects are less dangerous than the diseases they protect against. Moreover, chronic helminth infections mute the Th2 response, limiting the fibrotic side effects. Recent migration out of Africa to regions with fewer helminths has, therefore, resulted in a less regulated Th2 pattern, in which frequency and severity of many Th2-related diseases are increased in African Americans.
We hypothesize that genotypes that favor a skewed Th2 response in individuals of African ancestry account for the pattern of multiple fibroproliferative diseases. The increased prevalence of Th2 genotypes that increase resistance to helminthic infection and the increased frequency and severity of a subset of fibrotic disorders in individuals of African ancestry are consistent with a skewed Th2 response; however, more research is needed to determine whether healthy Africans and African Americans exhibit a skewed Th2 response.
Other immunologic differences selected in response to bacterial, viral, and other parasitic challenges in Africa also exist. For example, differences in response to evoked inflammation [165], TLR signaling [166], and stimulation of Th17 expression [167] have been reported which may contribute to increased inflammation and/or fibrosis in African Americans. Our hypothesis is not meant to explain all prevalence differences seen even in the disorders listed in Table 1. However, the high likelihood that helminthic selection for an enhanced Th2 profile contributes to all of the diseases mentioned is based, to a large extent, on the global distribution of helminths, as shown in Fig 1, and the strong evidence for an ancestral genotype that promotes high Th2 expression, decreased IL10 expression, and variably decreased Th1 expression in individuals of African ancestry. This hypothesis, which is testable, is a reasonable starting point for further study.
Supporting Information
Zdroje
1. Wynn TA, Ramalingam TR (2012) Mechanisms of fibrosis: therapeutic translation for fibrotic disease. Nat Med 18 : 1028–1040. doi: 10.1038/nm.2807 22772564
2. Balloch EA (1893) Relative frequency of fibroid processes in the dark skinned races. News XLVI: 29–35.
3. Rosser C (1925) Rectal pathology in the Negro. J Am Med Assoc LXXXIV: 93–97.
4. Rosser C (1923) Proctologic peculiarities of the Negro: the fibroplastic diathesis.Am J Surg 37 : 265.
5. Moehlig RC (1937) The mesoderm of the negro. Amer J of Phys Anthropol XXII: 297–314.
6. Polednak AP (1974) Connective tissue responses in Negroes in relation to disease. Am J Phys Anthropol 41 : 49–57. 4601999
7. Polednak AP (1987) Connective tissue responses in blacks in relation to disease: further observations. Am J Phys Anthropol 74 : 357–371. 3322033
8. Polednak AP (1989) Various chronic disorders and other conditions. Racial and Ethnic Differences in Disease. New York: Oxford University press. pp. 228–229, 246–247.
9. Niessen FB, Spauwen PH, Schalkwijk J, Kon M (1999) On the nature of hypertrophic scars and keloids: a review. Plast Reconstr Surg 104 : 1435–1458. 10513931
10. Racette L, Wilson MR, Zangwill LM, Weinreb RN, Sample PA (2003) Primary open-angle glaucoma in blacks: a review. Surv Ophthalmol 48 : 295–313. 12745004
11. Morris DA, Peracha MO, Shin DH, Kim C, Cha SC, et al. (1999) Risk factors for early filtration failure requiring suture release after primary glaucoma triple procedure with adjunctive mitomycin. Arch Ophthalmol 117 : 1149–1154. 10496386
12. Dustan HP (1992) Growth factors and racial differences in severity of hypertension and renal diseases. Lancet 339 : 1339–1340. 1350001
13. Suthanthiran M, Li B, Song JO, Ding R, Sharma VK, et al. (2000) Transforming growth factor-beta 1 hyperexpression in African-American hypertensives: A novel mediator of hypertension and/or target organ damage. Proc Natl Acad Sci U S A 97 : 3479–3484. 10725360
14. August P, Suthanthiran M (2003) Transforming growth factor beta and progression of renal disease. Kidney Int Suppl: S99–104. 14531781
15. Mayes MD, Lacey JV Jr., Beebe-Dimmer J, Gillespie BW, Cooper B, et al. (2003) Prevalence, incidence, survival, and disease characteristics of systemic sclerosis in a large US population. Arthritis Rheum 48 : 2246–2255. 12905479
16. Rybicki BA, Maliarik MJ, Major M, Popovich J Jr., Iannuzzi MC (1998) Epidemiology, demographics, and genetics of sarcoidosis. Semin Respir Infect 13 : 166–173. 9764947
17. Flake GP, Andersen J, Dixon D (2003) Etiology and pathogenesis of uterine leiomyomas: a review. Environ Health Perspect 111 : 1037–1054. 12826476
18. Nickel R, Beck LA, Stellato C, Schleimer RP (1999) Chemokines and allergic disease. J Allergy Clin Immunol 104 : 723–742. 10518815
19. Barnes KC, Grant AV, Hansel NN, Gao P, Dunston GM (2007) African Americans with asthma: genetic insights. Proc Am Thorac Soc 4 : 58–68. 17202293
20. Newth CJ, Meert KL, Clark AE, Moler FW, Zuppa AF, et al. (2012) Fatal and Near-Fatal Asthma in Children: The Critical Care Perspective. J Pediatr 161 : 214–221.e3. doi: 10.1016/j.jpeds.2012.02.041 22494876
21. Lester LA, Rich SS, Blumenthal MN, Togias A, Murphy S, et al. (2001) Ethnic differences in asthma and associated phenotypes: collaborative study on the genetics of asthma. J Allergy Clin Immunol 108 : 357–362. 11544453
22. Prisant LM, Loebl DH, Mulloy LL (2003) Scleroderma renal crisis. J Clin Hypertens (Greenwich) 5 : 168–170, 176.
23. Swigris JJ, Olson AL, Huie TJ, Fernandez-Perez ER, Solomon J, et al. (2011) Sarcoidosis-related mortality in the United States from 1988 to 2007. Am J Respir Crit Care Med 183 : 1524–1530. doi: 10.1164/rccm.201010-1679OC 21330454
24. Arrindell S, Russell SB (2009) Genetics of Skin Diseases. In: Kelly PA, Taylor SC, editors. Dermatology for Skin of Color: McGraw Hill. pp. 96–104.
25. Smith JC, Boone BE, Opalenik SR, Williams SM, Russell SB (2008) Gene profiling of keloid fibroblasts shows altered expression in multiple fibrosis-associated pathways. J Invest Dermatol 128 : 1298–1310. 17989729
26. Dustan HP (1995) Does keloid pathogenesis hold the key to understanding black/white differences in hypertension severity? Hypertension 26 : 858–862. 7490140
27. Freedman BI, Morrow MA, Tuttle AB, Igwemezie BM, Rich SS, et al. (1998) Keloids and end-stage renal disease. Nephron 80 : 244–246. 9736834
28. Shriver MD, Stroup B, and Thompson P. (1997) Genetic factors common to keloids and hypertension. Am J Hum Gen 61: A321.
29. August P, Leventhal B, Suthanthiran M (2000) Hypertension-induced organ damage in African Americans: transforming growth factor-beta(1) excess as a mechanism for increased prevalence. Curr Hypertens Rep 2 : 184–191. 10981147
30. Mosmann TR, Cherwinski H, Bond MW, Giedlin MA, Coffman RL (1986) Two types of murine helper T cell clone. I. Definition according to profiles of lymphokine activities and secreted proteins. J Immunol 136 : 2348–2357. 2419430
31. Wynn TA, Cheever AW, Jankovic D, Poindexter RW, Caspar P, et al. (1995) An IL-12-based vaccination method for preventing fibrosis induced by schistosome infection. Nature 376 : 594–596. 7637808
32. Shi Z, Wakil AE, Rockey DC (1997) Strain-specific differences in mouse hepatic wound healing are mediated by divergent T helper cytokine responses. Proc Natl Acad Sci U S A 94 : 10663–10668. 9380692
33. Reiner SL, Locksley RM (1995) The regulation of immunity to Leishmania major. Annu Rev Immunol 13 : 151–177. 7612219
34. Hoffmann KF, James SL, Cheever AW, Wynn TA (1999) Studies with double cytokine-deficient mice reveal that highly polarized Th1 - and Th2-type cytokine and antibody responses contribute equally to vaccine-induced immunity to Schistosoma mansoni. J Immunol 163 : 927–938. 10395689
35. Hoffmann KF, McCarty TC, Segal DH, Chiaramonte M, Hesse M, et al. (2001) Disease fingerprinting with cDNA microarrays reveals distinct gene expression profiles in lethal type 1 and type 2 cytokine-mediated inflammatory reactions. Faseb J 15 : 2545–2547. 11641263
36. Sandler NG, Mentink-Kane MM, Cheever AW, Wynn TA (2003) Global gene expression profiles during acute pathogen-induced pulmonary inflammation reveal divergent roles for Th1 and Th2 responses in tissue repair. J Immunol 171 : 3655–3667. 14500663
37. Wynn TA (2004) Fibrotic disease and the T(H)1/T(H)2 paradigm. Nat Rev Immunol 4 : 583–594. 15286725
38. Sime PJ, O'Reilly KM (2001) Fibrosis of the lung and other tissues: new concepts in pathogenesis and treatment. Clin Immunol 99 : 308–319. 11358425
39. Postlethwaite AE, Holness MA, Katai H, Raghow R (1992) Human fibroblasts synthesize elevated levels of extracellular matrix proteins in response to interleukin 4. J Clin Invest 90 : 1479–1485. 1401080
40. Oriente A, Fedarko NS, Pacocha SE, Huang SK, Lichtenstein LM, et al. (2000) Interleukin-13 modulates collagen homeostasis in human skin and keloid fibroblasts. J Pharmacol Exp Ther 292 : 988–994. 10688614
41. Atamas SP, White B (2003) Cytokine regulation of pulmonary fibrosis in scleroderma. Cytokine Growth Factor Rev 14 : 537–550. 14563355
42. Kaufman J, Sime PJ, Phipps RP (2004) Expression of CD154 (CD40 ligand) by human lung fibroblasts: differential regulation by IFN-gamma and IL-13, and implications for fibrosis. J Immunol 172 : 1862–1871. 14734771
43. Jinnin M, Ihn H, Yamane K, Tamaki K (2004) Interleukin-13 stimulates the transcription of the human alpha2(I) collagen gene in human dermal fibroblasts. J Biol Chem 279 : 41783–41791. 15271999
44. Shao DD, Suresh R, Vakil V, Gomer RH, Pilling D (2008) Pivotal Advance: Th-1 cytokines inhibit, and Th-2 cytokines promote fibrocyte differentiation. J Leukoc Biol 83 : 1323–1333. doi: 10.1189/jlb.1107782 18332234
45. Murray LA, Argentieri RL, Farrell FX, Bracht M, Sheng H, et al. (2008) Hyper-responsiveness of IPF/UIP fibroblasts: interplay between TGFbeta1, IL-13 and CCL2. Int J Biochem Cell Biol 40 : 2174–2182. doi: 10.1016/j.biocel.2008.02.016 18395486
46. Park SW, Ahn MH, Jang HK, Jang AS, Kim DJ, et al. (2009) Interleukin-13 and its receptors in idiopathic interstitial pneumonia: clinical implications for lung function. J Korean Med Sci 24 : 614–620. doi: 10.3346/jkms.2009.24.4.614 19654941
47. de Jesus AR, Magalhaes A, Miranda DG, Miranda RG, Araujo MI, et al. (2004) Association of type 2 cytokines with hepatic fibrosis in human Schistosoma mansoni infection. Infect Immun 72 : 3391–3397. 15155645
48. Weng HL, Liu Y, Chen JL, Huang T, Xu LJ, et al. (2009) The etiology of liver damage imparts cytokines transforming growth factor beta1 or interleukin-13 as driving forces in fibrogenesis. Hepatology 50 : 230–243. doi: 10.1002/hep.22934 19441105
49. McCauley RL, Chopra V, Li YY, Herndon DN, Robson MC (1992) Altered cytokine production in black patients with keloids. J Clin Immunol 12 : 300–308. 1512303
50. Diehl S, Rincon M (2002) The two faces of IL-6 on Th1/Th2 differentiation. Mol Immunol 39 : 531–536. 12431386
51. Smith CJ, Smith JC, Finn MC (1987) The possible role of mast cells (allergy) in the production of keloid and hypertrophic scarring. J Burn Care Rehabil 8 : 126–131. 3647037
52. Yamada H, Tajima S, Nishikawa T, Murad S, Pinnell SR (1994) Tranilast, a selective inhibitor of collagen synthesis in human skin fibroblasts. J Biochem (Tokyo) 116 : 892–897.
53. Suzawa H, Ichikawa K, Kikuchi S, Yamada K, Tsuchiya O, et al. (1992) [Effect of tranilast, an anti-allergic drug, on carrageenin-induced granulation and capillary permeability in rats]. Nippon Yakurigaku Zasshi 99 : 241–246. 1376712
54. Placik OJ, Lewis VL Jr. (1992) Immunologic associations of keloids. Surg Gynecol Obstet 175 : 185–193. 1636146
55. Mavalia C, Scaletti C, Romagnani P, Carossino AM, Pignone A, et al. (1997) Type 2 helper T-cell predominance and high CD30 expression in systemic sclerosis. Am J Pathol 151 : 1751–1758. 9403725
56. Salmon-Ehr V, Serpier H, Nawrocki B, Gillery P, Clavel C, et al. (1996) Expression of interleukin-4 in scleroderma skin specimens and scleroderma fibroblast cultures. Potential role in fibrosis. Arch Dermatol 132 : 802–806. 8678573
57. Chiaramonte MG, Mentink-Kane M, Jacobson BA, Cheever AW, Whitters MJ, et al. (2003) Regulation and function of the interleukin 13 receptor alpha 2 during a T helper cell type 2-dominant immune response. J Exp Med 197 : 687–701. 12642601
58. Mentink-Kane MM, Cheever AW, Thompson RW, Hari DM, Kabatereine NB, et al. (2004) IL-13 receptor alpha 2 down-modulates granulomatous inflammation and prolongs host survival in schistosomiasis. Proc Natl Acad Sci U S A 101 : 586–590. 14699044
59. Granel B, Allanore Y, Chevillard C, Arnaud V, Marquet S, et al. (2006) IL13RA2 gene polymorphisms are associated with systemic sclerosis. J Rheumatol 33 : 2015–2019. 16981293
60. Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, et al. (2008) Helminth infections: the great neglected tropical diseases. J Clin Invest 118 : 1311–1321. doi: 10.1172/JCI34261 18382743
61. Diaz A, Allen JE (2007) Mapping immune response profiles: the emerging scenario from helminth immunology. Eur J Immunol 37 : 3319–3326. 18000958
62. Allen JE, Maizels RM (2011) Diversity and dialogue in immunity to helminths. Nat Rev Immunol 11 : 375–388. doi: 10.1038/nri2992 21610741
63. Fumagalli M, Pozzoli U, Cagliani R, Comi GP, Bresolin N, et al. (2010) The landscape of human genes involved in the immune response to parasitic worms. BMC Evol Biol 10 : 264. doi: 10.1186/1471-2148-10-264 20807397
64. Allen JE, Wynn TA (2011) Evolution of Th2 immunity: a rapid repair response to tissue destructive pathogens. PLoS Pathog 7: e1002003. doi: 10.1371/journal.ppat.1002003 21589896
65. Smits HH, Everts B, Hartgers FC, Yazdanbakhsh M (2010) Chronic helminth infections protect against allergic diseases by active regulatory processes. Curr Allergy Asthma Rep 10 : 3–12. doi: 10.1007/s11882-009-0085-3 20425508
66. Walsh KP, Brady MT, Finlay CM, Boon L, Mills KH (2009) Infection with a helminth parasite attenuates autoimmunity through TGF-beta-mediated suppression of Th17 and Th1 responses. J Immunol 183 : 1577–1586. doi: 10.4049/jimmunol.0803803 19587018
67. Hartmann W, Haben I, Fleischer B, Breloer M (2011) Pathogenic nematodes suppress humoral responses to third-party antigens in vivo by IL-10-mediated interference with Th cell function. J Immunol 187 : 4088–4099. doi: 10.4049/jimmunol.1004136 21900178
68. Hoffmann KF, Cheever AW, Wynn TA (2000) IL-10 and the dangers of immune polarization: excessive type 1 and type 2 cytokine responses induce distinct forms of lethal immunopathology in murine schistosomiasis. J Immunol 164 : 6406–6416. 10843696
69. Yazdanbakhsh M, Kremsner PG, van Ree R (2002) Allergy, parasites, and the hygiene hypothesis. Science 296 : 490–494. 11964470
70. Quinnell RJ (2003) Genetics of susceptibility to human helminth infection. Int J Parasitol 33 : 1219–1231. 13678637
71. Maizels RM, Yazdanbakhsh M (2003) Immune regulation by helminth parasites: cellular and molecular mechanisms. Nat Rev Immunol 3 : 733–744. 12949497
72. Le Souef PN, Goldblatt J, Lynch NR (2000) Evolutionary adaptation of inflammatory immune responses in human beings. Lancet 356 : 242–244. 10963213
73. Elliott DE, Weinstock JV Helminth-host immunological interactions: prevention and control of immune-mediated diseases. Ann N Y Acad Sci 1247 : 83–96. doi: 10.1111/j.1749-6632.2011.06292.x 22239614
74. Maizels RM, Yazdanbakhsh M (2008) T-cell regulation in helminth parasite infections: implications for inflammatory diseases. Chem Immunol Allergy 94 : 112–123. doi: 10.1159/000154944 18802342
75. Flohr C, Quinnell RJ, Britton J (2009) Do helminth parasites protect against atopy and allergic disease? Clin Exp Allergy 39 : 20–32. doi: 10.1111/j.1365-2222.2008.03134.x 19128351
76. Masters S, Barrett-Connor E (1985) Parasites and asthma—predictive or protective? Epidemiol Rev 7 : 49–58. 4054238
77. Gold DR, Wright R (2005) Population disparities in asthma. Annu Rev Public Health 26 : 89–113. 15760282
78. Nelson DA, Johnson CC, Divine GW, Strauchman C, Joseph CL, et al. (1997) Ethnic differences in the prevalence of asthma in middle class children. Ann Allergy Asthma Immunol 78 : 21–26. 9012615
79. Grundbacher FJ, Massie FS (1985) Levels of immunoglobulin G, M, A, and E at various ages in allergic and nonallergic black and white individuals. J Allergy Clin Immunol 75 : 651–658. 4008794
80. Vergara C, Murray T, Rafaels N, Lewis R, Campbell M, et al. (2013) African ancestry is a risk factor for asthma and high total IgE levels in African admixed populations. Genet Epidemiol 37 : 393–401. doi: 10.1002/gepi.21702 23554133
81. D'Elia R, Behnke JM, Bradley JE, Else KJ (2009) Regulatory T cells: a role in the control of helminth-driven intestinal pathology and worm survival. J Immunol 182 : 2340–2348. doi: 10.4049/jimmunol.0802767 19201888
82. Hopkin J (2009) Immune and genetic aspects of asthma, allergy and parasitic worm infections: evolutionary links. Parasite Immunol 31 : 267–273. doi: 10.1111/j.1365-3024.2009.01104.x 19388947
83. Barnes KC, Grant AV, Gao P (2005) A review of the genetic epidemiology of resistance to parasitic disease and atopic asthma: common variants for common phenotypes? Curr Opin Allergy Clin Immunol 5 : 379–385. 16131910
84. Moller M, Gravenor MB, Roberts SE, Sun D, Gao P, et al. (2007) Genetic haplotypes of Th-2 immune signalling link allergy to enhanced protection to parasitic worms. Hum Mol Genet 16 : 1828–1836. 17519224
85. Holgate ST (2012) Innate and adaptive immune responses in asthma. Nat Med 18 : 673–683. doi: 10.1038/nm.2731 22561831
86. Shifren A, Witt C, Christie C, Castro M (2012) Mechanisms of remodeling in asthmatic airways. J Allergy (Cairo) 2012 : 316049.
87. Smillie WG, Augustine DL (1925) Intensity of hookworm infestation in Alabama. Its relationship to residence, occupation, age, sex and race. J Am Med Assoc 85 : 1958–1963.
88. Keller AE, Leather WS, Knox JC,. (1937) The present status of hookworm infestation in North Carolina. Am J Hyg 26 : 437–454.
89. Coelho PRP, McGuire RA (2006) Racial differences in disease susceptibilities: intestinal worm infection in the early twentieth-century American south. Soc Hist Med 19 : 461–482.
90. Williams-Blangero S, Subedi J, Upadhayay RP, Manral DB, Rai DR, et al. (1999) Genetic analysis of susceptibility to infection with Ascaris lumbricoides. Am J Trop Med Hyg 60 : 921–926. 10403321
91. Abel L, Demenais F, Prata A, Souza AE, Dessein A (1991) Evidence for the segregation of a major gene in human susceptibility/resistance to infection by Schistosoma mansoni. Am J Hum Genet 48 : 959–970. 1902058
92. Marquet S, Abel L, Hillaire D, Dessein H, Kalil J, et al. (1996) Genetic localization of a locus controlling the intensity of infection by Schistosoma mansoni on chromosome 5q31-q33. Nat Genet 14 : 181–184. 8841190
93. Muller-Myhsok B, Stelma FF, Guisse-Sow F, Muntau B, Thye T, et al. (1997) Further evidence suggesting the presence of a locus, on human chromosome 5q31-q33, influencing the intensity of infection with Schistosoma mansoni. Am J Hum Genet 61 : 452–454. 9311752
94. Kouriba B, Chevillard C, Bream JH, Argiro L, Dessein H, et al. (2005) Analysis of the 5q31-q33 locus shows an association between IL13-1055C/T IL-13-591A/G polymorphisms and Schistosoma haematobium infections. J Immunol 174 : 6274–6281. 15879126
95. Cameron L, Webster RB, Strempel JM, Kiesler P, Kabesch M, et al. (2006) Th2 cell-selective enhancement of human IL13 transcription by IL13-1112C>T, a polymorphism associated with allergic inflammation. J Immunol 177 : 8633–8642. 17142763
96. van der Pouw Kraan TC, van Veen A, Boeije LC, van Tuyl SA, de Groot ER, et al. (1999) An IL-13 promoter polymorphism associated with increased risk of allergic asthma. Genes Immun 1 : 61–65. 11197307
97. Gatlin MR, Black CL, Mwinzi PN, Secor WE, Karanja DM, et al. (2009) Association of the gene polymorphisms IFN-gamma +874, IL-13–1055 and IL-4–590 with patterns of reinfection with Schistosoma mansoni. PLoS Negl Trop Dis 3: e375. doi: 10.1371/journal.pntd.0000375 19190772
98. He H, Isnard A, Kouriba B, Cabantous S, Dessein A, et al. (2008) A STAT6 gene polymorphism is associated with high infection levels in urinary schistosomiasis. Genes Immun 9 : 195–206. doi: 10.1038/gene.2008.2 18273035
99. Bethony JM, Quinnell RJ (2008) Genetic epidemiology of human schistosomiasis in Brazil. Acta Trop 108 : 166–174. doi: 10.1016/j.actatropica.2007.11.008 18207118
100. Prata A (1992) Influence of the host related factors in the development of the hepatosplenic form of schistosomiasis mansoni. Mem Inst Oswaldo Cruz 87 Suppl 4 : 39–44. 1343924
101. Bina JC, Tavares-Neto J, Prata A, Azevedo ES (1978) Greater resistance to the development of severe schistosomiasis in Brazilian negroes. Hum Biol 50 : 41–49. 649103
102. Mwatha JK, Kimani G, Kamau T, Mbugua GG, Ouma JH, et al. (1998) High levels of TNF, soluble TNF receptors, soluble ICAM-1, and IFN-gamma, but low levels of IL-5, are associated with hepatosplenic disease in human schistosomiasis mansoni. J Immunol 160 : 1992–1999. 9469463
103. Mbow M, Larkin BM, Meurs L, Wammes LJ, de Jong SE, et al. (2013) T-helper 17 cells are associated with pathology in human schistosomiasis. J Infect Dis 207 : 186–195. doi: 10.1093/infdis/jis654 23087431
104. Rutitzky LI, Stadecker MJ (2011) Exacerbated egg-induced immunopathology in murine Schistosoma mansoni infection is primarily mediated by IL-17 and restrained by IFN-gamma. Eur J Immunol 41 : 2677–2687. doi: 10.1002/eji.201041327 21660933
105. Abath FG, Morais CN, Montenegro CE, Wynn TA, Montenegro SM (2006) Immunopathogenic mechanisms in schistosomiasis: what can be learnt from human studies? Trends Parasitol 22 : 85–91. 16380294
106. Chevillard C, Moukoko CE, Elwali NE, Bream JH, Kouriba B, et al. (2003) IFN-gamma polymorphisms (IFN-gamma +2109 and IFN-gamma +3810) are associated with severe hepatic fibrosis in human hepatic schistosomiasis (Schistosoma mansoni). J Immunol 171 : 5596–5601. 14607968
107. Henri S, Chevillard C, Mergani A, Paris P, Gaudart J, et al. (2002) Cytokine regulation of periportal fibrosis in humans infected with Schistosoma mansoni: IFN-gamma is associated with protection against fibrosis and TNF-alpha with aggravation of disease. J Immunol 169 : 929–936. 12097398
108. Dessein AJ, Hillaire D, Elwali NE, Marquet S, Mohamed-Ali Q, et al. (1999) Severe hepatic fibrosis in Schistosoma mansoni infection is controlled by a major locus that is closely linked to the interferon-gamma receptor gene. Am J Hum Genet 65 : 709–721. 10441577
109. Wilfing A, Winkler S, Schrattbauer K, Willheim M, Baier K, et al. (2001) African-European differences in the capacity of T-cell cytokine production. Am J Trop Med Hyg 65 : 504–509. 11716105
110. Abecasis GR, Auton A, Brooks LD, DePristo MA, Durbin RM, et al. (2012) An integrated map of genetic variation from 1,092 human genomes. Nature 491 : 56–65. doi: 10.1038/nature11632 23128226
111. Altshuler DM, Gibbs RA, Peltonen L, Altshuler DM, Gibbs RA, et al. (2010) Integrating common and rare genetic variation in diverse human populations. Nature 467 : 52–58. doi: 10.1038/nature09298 20811451
112. Basehore MJ, Howard TD, Lange LA, Moore WC, Hawkins GA, et al. (2004) A comprehensive evaluation of IL4 variants in ethnically diverse populations: association of total serum IgE levels and asthma in white subjects. J Allergy Clin Immunol 114 : 80–87. 15241348
113. Nie W, Zhu Z, Pan X, Xiu Q (2013) The interleukin-4 -589C/T polymorphism and the risk of asthma: a meta-analysis including 7,345 cases and 7,819 controls. Gene 520 : 22–29. doi: 10.1016/j.gene.2013.02.027 23454622
114. Burchard EG, Silverman EK, Rosenwasser LJ, Borish L, Yandava C, et al. (1999) Association between a sequence variant in the IL-4 gene promoter and FEV(1) in asthma. Am J Respir Crit Care Med 160 : 919–922. 10471619
115. Donfack J, Schneider DH, Tan Z, Kurz T, Dubchak I, et al. (2005) Variation in conserved non-coding sequences on chromosome 5q and susceptibility to asthma and atopy. Respir Res 6 : 145. 16336695
116. Haller G, Torgerson DG, Ober C, Thompson EE (2009) Sequencing the IL4 locus in African Americans implicates rare noncoding variants in asthma susceptibility. J Allergy Clin Immunol 124 : 1204–1209 e1209. doi: 10.1016/j.jaci.2009.09.013 19910025
117. Rockman MV, Hahn MW, Soranzo N, Goldstein DB, Wray GA (2003) Positive selection on a human-specific transcription factor binding site regulating IL4 expression. Curr Biol 13 : 2118–2123. 14654003
118. Rosenwasser LJ, Borish L (1997) Genetics of atopy and asthma: the rationale behind promoter-based candidate gene studies (IL-4 and IL-10). Am J Respir Crit Care Med 156: S152–155. 9351597
119. Akkad DA, Arning L, Ibrahim SM, Epplen JT (2007) Sex specifically associated promoter polymorphism in multiple sclerosis affects interleukin 4 expression levels. Genes Immun 8 : 703–706. 17855802
120. Heinzmann A, Mao XQ, Akaiwa M, Kreomer RT, Gao PS, et al. (2000) Genetic variants of IL-13 signalling and human asthma and atopy. Hum Mol Genet 9 : 549–559. 10699178
121. Hummelshoj T, Bodtger U, Datta P, Malling HJ, Oturai A, et al. (2003) Association between an interleukin-13 promoter polymorphism and atopy. Eur J Immunogenet 30 : 355–359. 14641544
122. Doucet C, Brouty-Boye D, Pottin-Clemenceau C, Canonica GW, Jasmin C, et al. (1998) Interleukin (IL) 4 and IL-13 act on human lung fibroblasts. Implication in asthma. J Clin Invest 101 : 2129–2139. 9593769
123. Hershey GK (2003) IL-13 receptors and signaling pathways: an evolving web. J Allergy Clin Immunol 111 : 677–690; quiz 691. 12704343
124. Wilson MS, Elnekave E, Mentink-Kane MM, Hodges MG, Pesce JT, et al. (2007) IL-13Ralpha2 and IL-10 coordinately suppress airway inflammation, airway-hyperreactivity, and fibrosis in mice. J Clin Invest 117 : 2941–2951. 17885690
125. Granel B, Chevillard C, Allanore Y, Arnaud V, Cabantous S, et al. (2006) Evaluation of interleukin 13 polymorphisms in systemic sclerosis. Immunogenetics 58 : 693–699. 16832637
126. Isnard A, Kouriba B, Doumbo O, Chevillard C (2011) Association of rs7719175, located in the IL13 gene promoter, with Schistosoma haematobium infection levels and identification of a susceptibility haplotype. Genes Immun 12 : 31–39. doi: 10.1038/gene.2010.43 20861864
127. Chatila TA (1998) Genetics of atopic diseases. Curr Opin Pediatr 10 : 584–587. 9848017
128. Deichmann K, Bardutzky J, Forster J, Heinzmann A, Kuehr J (1997) Common polymorphisms in the coding part of the IL4-receptor gene. Biochem Biophys Res Commun 231 : 696–697. 9070874
129. Hackstein H, Hecker M, Kruse S, Bohnert A, Ober C, et al. (2001) A novel polymorphism in the 5' promoter region of the human interleukin-4 receptor alpha-chain gene is associated with decreased soluble interleukin-4 receptor protein levels. Immunogenetics 53 : 264–269. 11491529
130. Bergin AM, Balder B, Kishore S, Sward K, Hahn-Zoric M, et al. (2006) Common variations in the IL4R gene affect splicing and influence natural expression of the soluble isoform. Hum Mutat 27 : 990–998. 16917945
131. Hershey GK, Friedrich MF, Esswein LA, Thomas ML, Chatila TA (1997) The association of atopy with a gain-of-function mutation in the alpha subunit of the interleukin-4 receptor. N Engl J Med 337 : 1720–1725. 9392697
132. Rosa-Rosa L, Zimmermann N, Bernstein JA, Rothenberg ME, Khurana Hershey GK (1999) The R576 IL-4 receptor alpha allele correlates with asthma severity. J Allergy Clin Immunol 104 : 1008–1014. 10550746
133. Mitsuyasu H, Yanagihara Y, Mao XQ, Gao PS, Arinobu Y, et al. (1999) Cutting edge: dominant effect of Ile50Val variant of the human IL-4 receptor alpha-chain in IgE synthesis. J Immunol 162 : 1227–1231. 9973373
134. Wjst M, Kruse S, Illig T, Deichmann K (2002) Asthma and IL-4 receptor alpha gene variants. Eur J Immunogenet 29 : 263–268. 12047364
135. Kruse S, Japha T, Tedner M, Sparholt SH, Forster J, et al. (1999) The polymorphisms S503P and Q576R in the interleukin-4 receptor alpha gene are associated with atopy and influence the signal transduction. Immunology 96 : 365–371. 10233717
136. Wu X, Di Rienzo A, Ober C (2001) A population genetics study of single nucleotide polymorphisms in the interleukin 4 receptor alpha (IL4RA) gene. Genes Immun 2 : 128–134. 11426321
137. Caggana M, Walker K, Reilly AA, Conroy JM, Duva S, et al. (1999) Population-based studies reveal differences in the allelic frequencies of two functionally significant human interleukin-4 receptor polymorphisms in several ethnic groups. Genet Med 1 : 267–271. 11258628
138. Ober C, Leavitt SA, Tsalenko A, Howard TD, Hoki DM, et al. (2000) Variation in the interleukin 4-receptor alpha gene confers susceptibility to asthma and atopy in ethnically diverse populations. Am J Hum Genet 66 : 517–526. 10677312
139. Tachdjian R, Mathias C, Al Khatib S, Bryce PJ, Kim HS, et al. (2009) Pathogenicity of a disease-associated human IL-4 receptor allele in experimental asthma. J Exp Med 206 : 2191–2204. doi: 10.1084/jem.20091480 19770271
140. Youn J, Hwang SH, Cho CS, Min JK, Kim WU, et al. (2000) Association of the interleukin-4 receptor alpha variant Q576R with Th1/Th2 imbalance in connective tissue disease. Immunogenetics 51 : 743–746. 10941846
141. Battle NC, Choudhry S, Tsai HJ, Eng C, Kumar G, et al. (2007) Ethnicity-specific gene-gene interaction between IL-13 and IL-4Ralpha among African Americans with asthma. Am J Respir Crit Care Med 175 : 881–887. 17303794
142. Couper KN, Blount DG, Riley EM (2008) IL-10: the master regulator of immunity to infection. J Immunol 180 : 5771–5777. 18424693
143. Peranteau WH, Zhang L, Muvarak N, Badillo AT, Radu A, et al. (2008) IL-10 overexpression decreases inflammatory mediators and promotes regenerative healing in an adult model of scar formation. J Invest Dermatol 128 : 1852–1860. doi: 10.1038/sj.jid.5701232 18200061
144. Booth M, Mwatha JK, Joseph S, Jones FM, Kadzo H, et al. (2004) Periportal fibrosis in human Schistosoma mansoni infection is associated with low IL-10, low IFN-gamma, high TNF-alpha, or low RANTES, depending on age and gender. J Immunol 172 : 1295–1303. 14707108
145. Grant AV, Araujo MI, Ponte EV, Oliveira RR, Cruz AA, et al. (2011) Polymorphisms in IL10 are associated with total Immunoglobulin E levels and Schistosoma mansoni infection intensity in a Brazilian population. Genes Immun 12 : 46–50. doi: 10.1038/gene.2010.50 20927126
146. Hayden CM, Zhang G, Judge PK, Khoo SK, Laing IA, et al. (2011) Regulatory role of IL10 genetic variations in determining allergen-induced T(H)2 cytokine responses in children. J Allergy Clin Immunol 128 : 237–239 e238. doi: 10.1016/j.jaci.2011.02.032 21439624
147. Silva PC, Gomes AV, de Souza TK, Coelho MR, Cahu GG, et al. (2014) Association of SNP (-G1082A) IL-10 with Increase in Severity of Periportal Fibrosis in Schistosomiasis, in the Northeast of Brazil. Genet Test Mol Biomarkers 18 : 646–52. doi: 10.1089/gtmb.2014.0098 25079344
148. Hoffmann SC, Stanley EM, Cox ED, DiMercurio BS, Koziol DE, et al. (2002) Ethnicity greatly influences cytokine gene polymorphism distribution. Am J Transplant 2 : 560–567. 12118901
149. Smith AJ, Humphries SE (2009) Cytokine and cytokine receptor gene polymorphisms and their functionality. Cytokine Growth Factor Rev 20 : 43–59. doi: 10.1016/j.cytogfr.2008.11.006 19038572
150. Delaney NL, Esquenazi V, Lucas DP, Zachary AA, Leffell MS (2004) TNF-alpha, TGF-beta, IL-10, IL-6, and INF-gamma alleles among African Americans and Cuban Americans. Report of the ASHI Minority Workshops: Part IV. Hum Immunol 65 : 1413–1419. 15603866
151. Ihn H (2002) Pathogenesis of fibrosis: role of TGF-beta and CTGF. Curr Opin Rheumatol 14 : 681–685. 12410091
152. Border WA, Noble NA (1994) Transforming growth factor beta in tissue fibrosis. N Engl J Med 331 : 1286–1292. 7935686
153. Drumm ML, Konstan MW, Schluchter MD, Handler A, Pace R, et al. (2005) Genetic modifiers of lung disease in cystic fibrosis. N Engl J Med 353 : 1443–1453. 16207846
154. Phillips JA 3rd, Poling JS, Phillips CA, Stanton KC, Austin ED, et al. (2008) Synergistic heterozygosity for TGFbeta1 SNPs and BMPR2 mutations modulates the age at diagnosis and penetrance of familial pulmonary arterial hypertension. Genet Med 10 : 359–365. doi: 10.1097/GIM.0b013e318172dcdf 18496036
155. Eiser AR (2010) Does over-expression of transforming growth factor-beta account for the increased morbidity in African-Americans: Possible clinical study and therapeutic implications. Medical Hypotheses 75 : 418–421. doi: 10.1016/j.mehy.2010.04.009 20457494
156. August P, Sharma V, Ding R, Schwartz JE, Suthanthiran M (2009) Transforming growth factor beta and excess burden of renal disease. Trans Am Clin Climatol Assoc 120 : 61–72. 19768163
157. Shah R, Rahaman B, Hurley CK, Posch PE (2006) Allelic diversity in the TGFB1 regulatory region: characterization of novel functional single nucleotide polymorphisms. Hum Genet 119 : 61–74. 16369764
158. Oldroyd SD, Thomas GL, Gabbiani G, El Nahas AM (1999) Interferon-gamma inhibits experimental renal fibrosis. Kidney Int 56 : 2116–2127. 10594787
159. Giri SN, Hyde DM, Marafino BJ Jr. (1986) Ameliorating effect of murine interferon gamma on bleomycin-induced lung collagen fibrosis in mice. Biochem Med Metab Biol 36 : 194–197. 2430600
160. Pravica V, Asderakis A, Perrey C, Hajeer A, Sinnott PJ, et al. (1999) In vitro production of IFN-gamma correlates with CA repeat polymorphism in the human IFN-gamma gene. Eur J Immunogenet 26 : 1–3. 10068907
161. Hassan MI, Aschner Y, Manning CH, Xu J, Aschner JL (2003) Racial differences in selected cytokine allelic and genotypic frequencies among healthy, pregnant women in North Carolina. Cytokine 21 : 10–16. 12668154
162. Upperman JS, Pillage G, Siddiqi MQ, Zeevi A, Kelly N, et al. (2005) Dominance of high-producing interleukin 6 and low-producing interleukin 10 and interferon gamma alleles in glucose-6-phosphate dehydrogenase-deficient trauma patients. Shock 23 : 197–201. 15718915
163. Rosenzweig SD, Schaffer AA, Ding L, Sullivan R, Enyedi B, et al. (2004) Interferon-gamma receptor 1 promoter polymorphisms: population distribution and functional implications. Clin Immunol 112 : 113–119. 15207788
164. Gao PS, Mao XQ, Jouanguy E, Pallier A, Doffinger R, et al. (1999) Nonpathogenic common variants of IFNGR1 and IFNGR2 in association with total serum IgE levels. Biochem Biophys Res Commun 263 : 425–429. 10491309
165. Ferguson JF, Patel PN, Shah RY, Mulvey CK, Gadi R, et al. (2013) Race and gender variation in response to evoked inflammation. J Transl Med 11 : 63. doi: 10.1186/1479-5876-11-63 23497455
166. Lyn-Cook BD, Xie C, Oates J, Treadwell E, Word B, et al. (2014) Increased expression of Toll-like receptors (TLRs) 7 and 9 and other cytokines in systemic lupus erythematosus (SLE) patients: ethnic differences and potential new targets for therapeutic drugs. Mol Immunol 61 : 38–43. doi: 10.1016/j.molimm.2014.05.001 24865418
167. Ye CJ, Feng T, Kwon HK, Raj T, Wilson MT, et al. (2014) Intersection of population variation and autoimmunity genetics in human T cell activation. Science 345 : 1254665. doi: 10.1126/science.1254665 25214635
168. Lustigman S, Prichard RK, Gazzinelli A, Grant WN, Boatin BA, et al. (2012) A research agenda for helminth diseases of humans: the problem of helminthiases. PLoS Negl Trop Dis 6: e1582. doi: 10.1371/journal.pntd.0001582 22545164
169. Weir BS, Cockerham C (1984) Estimating F-statistics for the analysis of population structure. Evolution 38 : 1358–1370.
170. Tielsch JM, Sommer A, Katz J, Royall RM, Quigley HA, et al. (1991) Racial variations in the prevalence of primary open-angle glaucoma. The Baltimore Eye Survey. JAMA 266 : 369–374. 2056646
171. (2005) Racial/ethnic disparities in prevalence, treatment, and control of hypertension—United States, 1999–2002. MMWR Morb Mortal Wkly Rep 54 : 7–9.
172. Barrett J (1973) Keloid. In: Bergsma D, editor. Birth Defect Compendium. Baltimore: Williams and Wilkens Company. pp. 553.
173. Drazner MH, Dries DL, Peshock RM, Cooper RS, Klassen C, et al. (2005) Left ventricular hypertrophy is more prevalent in blacks than whites in the general population: the Dallas Heart Study. Hypertension 46 : 124–129. 15939807
174. Kizer JR, Arnett DK, Bella JN, Paranicas M, Rao DC, et al. (2004) Differences in left ventricular structure between black and white hypertensive adults: the Hypertension Genetic Epidemiology Network study. Hypertension 43 : 1182–1188. 15123573
175. Lackland DT, Keil J.E (1996) Epidemiology of hypertension in African Americans. Semin Nephrol 16 : 63–70. 8668862
176. Ferguson R, Grim CE, Opgenorth TJ (1987) The epidemiology of end-state renal disease: the six-year South-Central Los Angeles experience, 1980–85. Am J Public Health 77 : 864–865. 3592045
177. Tracy RE, Bhandaru SY, Oalmann MC, Guzman MA, Newmann WP 3rd (1991) Blood pressure and nephrosclerosis in black and white men and women aged 25 to 54. Mod Pathol 4 : 602–609. 1758872
178. Freedman BI, Bowden DW, Rich SS, Valis CJ, Sale MM, et al. (2005) A genome scan for all-cause end-stage renal disease in African Americans. Nephrol Dial Transplant 20 : 712–718. 15701670
179. (USRDS) URDS (1998) 1998 Annual Data Report. Bethesda, MD: The National Institutes of Health, National Institute of Diabetes Digestive, and Kidney Diseases.
180. System URD (2003) USRDS 2003 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
181. Toto RB (2003) Hypertensive nephrosclerosis in African Americans. Kidney Int 64 : 2331–2341. 14633170
182. Terris M, Chaves AD (1966) An epidemiologic study of sarcoidosis. Am Rev Respir Dis 94 : 50–55. 5945340
183. Keller AZ (1971) Hospital, age, racial, occupational, geographical, clinical and survivorship characteristics in the epidemiology of sarcoidosis. Am J Epidemiol 94 : 222–230. 5093653
184. Sartwell PE, Edwards LB (1974) Epidemiology of sarcoidosis in the U.S. Navy. Am J Epidemiol 99 : 250–257. 4818715
185. Rybicki BA, Harrington D, Major M, Simoff M, Popovich J Jr., et al. (1996) Heterogeneity of familial risk in sarcoidosis. Genet Epidemiol 13 : 23–33. 8647376
186. Rybicki BA, Major M, Popovich J Jr., Maliarik MJ, Iannuzzi MC (1997) Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. Am J Epidemiol 145 : 234–241. 9012596
187. Kucera GP, Rybicki BA, Kirkey KL, Coon SW, Major ML, et al. (2003) Occupational risk factors for sarcoidosis in African-American siblings. Chest 123 : 1527–1535. 12740270
188. Iannuzzi MC, Rybicki BA, Teirstein AS (2007) Sarcoidosis. N Engl J Med 357 : 2153–2165. 18032765
189. Masi AT, D'Angelo WA (1967) Epidemiology of fatal systemic sclerosis (diffuse scleroderma). A 15-year survey in Baltimore. Ann Intern Med 66 : 870–883. 6025228
190. Arnett FC, Cho M, Chatterjee S, Aguilar MB, Reveille JD, et al. (2001) Familial occurrence frequencies and relative risks for systemic sclerosis (scleroderma) in three United States cohorts. Arthritis Rheum 44 : 1359–1362. 11407695
191. Mayes MD (2003) Scleroderma epidemiology. Rheum Dis Clin North Am 29 : 239–254. 12841293
192. Siegel M, Holley HL, Lee SL (1970) Epidemiologic studies on systemic lupus erythematosus. Comparative data for New York City and Jefferson County, Alabama, 1956–1965. Arthritis Rheum 13 : 802–811. 5495391
193. Wilson WA, Hughes GR (1979) Rheumatic disease in Jamaica. Ann Rheum Dis 38 : 320–325. 315207
194. Hochberg MC (1997) The epidemiology of systemic lupus erythematosus. In: Wallace DJ, Hahn B.H., Quismorio F.P., editor. Dubois' lupus erythematosus. Baltimore: Williams and Wilkins. pp. 49–65.
195. Rus VHA (2001) Systemic lupus erythematosus. In: Silman AJHM, editor. Epidemiology of rheumatic diseases: Oxford University Press. pp. 123–140.
196. Marshall LM, Spiegelman D, Barbieri RL, Goldman MB, Manson JE, et al. (1997) Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynecol 90 : 967–973. 9397113
197. Christopherson WM, Nealon NA (1981) Uterine cancer: a comparative study of black and white women. Prog Clin Biol Res 53 : 185–195. 7465586
198. Day Baird D, Dunson DB, Hill MC, Cousins D, Schectman JM (2003) High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol 188 : 100–107. 12548202
199. Yu Q, Horak K, Larson DF (2006) Role of T lymphocytes in hypertension-induced cardiac extracellular matrix remodeling. Hypertension 48 : 98–104. 16735642
200. Peng H, Yang XP, Carretero OA, Nakagawa P, D'Ambrosio M, et al. (2011) Angiotensin II-induced dilated cardiomyopathy in Balb/c but not C57BL/6J mice. Exp Physiol 96 : 756–764. doi: 10.1113/expphysiol.2011.057612 21602297
201. DeMeo DL, Lange C, Silverman EK, Senter JM, Drazen JM, et al. (2002) Univariate and multivariate family-based association analysis of the IL-13 ARG130GLN polymorphism in the Childhood Asthma Management Program. Genet Epidemiol 23 : 335–348. 12432502
202. Grant AV, Araujo MI, Ponte EV, Oliveira RR, Gao P, et al. (2012) Functional polymorphisms in IL13 are protective against high Schistosoma mansoni infection intensity in a Brazilian population. PLoS One 7: e35863. doi: 10.1371/journal.pone.0035863 22574126
203. Shah R, Hurley CK, Posch PE (2006) A molecular mechanism for the differential regulation of TGF-beta1 expression due to the common SNP -509C-T (c. -1347C > T). Hum Genet 120 : 461–469. 16896927
204. Grainger DJ, Heathcote K, Chiano M, Snieder H, Kemp PR, et al. (1999) Genetic control of the circulating concentration of transforming growth factor type beta1. Hum Mol Genet 8 : 93–97. 9887336
205. Silverman ES, Palmer LJ, Subramaniam V, Hallock A, Mathew S, et al. (2004) Transforming growth factor-beta1 promoter polymorphism C-509T is associated with asthma. Am J Respir Crit Care Med 169 : 214–219. 14597484
206. Awad M, Pravica V, Perrey C, El Gamel A, Yonan N, et al. (1999) CA repeat allele polymorphism in the first intron of the human interferon-gamma gene is associated with lung allograft fibrosis. Hum Immunol 60 : 343–346. 10363726
Štítky
Genetika Reprodukční medicína
Článek A Hereditary Enteropathy Caused by Mutations in the Gene, Encoding a Prostaglandin TransporterČlánek Exocyst-Dependent Membrane Addition Is Required for Anaphase Cell Elongation and Cytokinesis inČlánek Spindle-F Is the Central Mediator of Ik2 Kinase-Dependent Dendrite Pruning in Sensory Neurons
Článek vyšel v časopisePLOS Genetics
Nejčtenější tento týden
2015 Číslo 11- Akutní intermitentní porfyrie
- Farmakogenetické testování pomáhá předcházet nežádoucím efektům léčiv
- Růst a vývoj dětí narozených pomocí IVF
- Pilotní studie: stres a úzkost v průběhu IVF cyklu
- Vliv melatoninu a cirkadiálního rytmu na ženskou reprodukci
-
Všechny články tohoto čísla
- Agricultural Genomics: Commercial Applications Bring Increased Basic Research Power
- Ernst Rüdin’s Unpublished 1922-1925 Study “Inheritance of Manic-Depressive Insanity”: Genetic Research Findings Subordinated to Eugenic Ideology
- Convergent Evolution During Local Adaptation to Patchy Landscapes
- The Locus Controls Age at Maturity in Wild and Domesticated Atlantic Salmon ( L.) Males
- A Hereditary Enteropathy Caused by Mutations in the Gene, Encoding a Prostaglandin Transporter
- Absence of Maternal Methylation in Biparental Hydatidiform Moles from Women with Maternal-Effect Mutations Reveals Widespread Placenta-Specific Imprinting
- Calibrating the Human Mutation Rate via Ancestral Recombination Density in Diploid Genomes
- Anaplastic Lymphoma Kinase Acts in the Mushroom Body to Negatively Regulate Sleep
- Connecting Replication and Repair: YoaA, a Helicase-Related Protein, Promotes Azidothymidine Tolerance through Association with Chi, an Accessory Clamp Loader Protein
- UFBP1, a Key Component of the Ufm1 Conjugation System, Is Essential for Ufmylation-Mediated Regulation of Erythroid Development
- Mosaic and Intronic Mutations in Explain the Majority of TSC Patients with No Mutation Identified by Conventional Testing
- Members of the Epistasis Group Contribute to Mitochondrial Homologous Recombination and Double-Strand Break Repair in
- QTL Mapping of Sex Determination Loci Supports an Ancient Pathway in Ants and Honey Bees
- Genetic Interactions Implicating Postreplicative Repair in Okazaki Fragment Processing
- Genomics of Cancer and a New Era for Cancer Prevention
- Adaptation to High Ethanol Reveals Complex Evolutionary Pathways
- Dynamics of Transcription Factor Binding Site Evolution
- Exocyst-Dependent Membrane Addition Is Required for Anaphase Cell Elongation and Cytokinesis in
- Enhancer Runaway and the Evolution of Diploid Gene Expression
- Cattle Sex-Specific Recombination and Genetic Control from a Large Pedigree Analysis
- Drosophila Mutants Model Cornelia de Lange Syndrome in Growth and Behavior
- Pleiotropic Effects of Immune Responses Explain Variation in the Prevalence of Fibroproliferative Diseases
- Leaderless Transcripts and Small Proteins Are Common Features of the Mycobacterial Translational Landscape
- Tissue-Specific Effects of Reduced β-catenin Expression on Mutation-Instigated Tumorigenesis in Mouse Colon and Ovarian Epithelium
- Genus-Wide Comparative Genomics of Delineates Its Phylogeny, Physiology, and Niche Adaptation on Human Skin
- Mapping of Craniofacial Traits in Outbred Mice Identifies Major Developmental Genes Involved in Shape Determination
- Conserved Genetic Interactions between Ciliopathy Complexes Cooperatively Support Ciliogenesis and Ciliary Signaling
- Metabolomic Quantitative Trait Loci (mQTL) Mapping Implicates the Ubiquitin Proteasome System in Cardiovascular Disease Pathogenesis
- DNA Repair Cofactors ATMIN and NBS1 Are Required to Suppress T Cell Activation
- Spindle-F Is the Central Mediator of Ik2 Kinase-Dependent Dendrite Pruning in Sensory Neurons
- Ernst Rüdin and the State of Science
- ABCs of Insect Resistance to Bt
- Epigenetic Control of O-Antigen Chain Length: A Tradeoff between Virulence and Bacteriophage Resistance
- Encodes Dual Oxidase, Which Acts with Heme Peroxidase Curly Su to Shape the Adult Wing
- The Fanconi Anemia Pathway Protects Genome Integrity from R-loops
- Controls Quantitative Variation in Maize Kernel Row Number
- Genome-Wide Association Study of Golden Retrievers Identifies Germ-Line Risk Factors Predisposing to Mast Cell Tumours
- Insect Resistance to Toxin Cry2Ab Is Conferred by Mutations in an ABC Transporter Subfamily A Protein
- A Cytosine Methytransferase Modulates the Cell Envelope Stress Response in the Cholera Pathogen
- Conserved piRNA Expression from a Distinct Set of piRNA Cluster Loci in Eutherian Mammals
- The Multi-allelic Genetic Architecture of a Variance-Heterogeneity Locus for Molybdenum Concentration in Leaves Acts as a Source of Unexplained Additive Genetic Variance
- The lncRNA Controls Cryptococcal Morphological Transition
- Sae2 Function at DNA Double-Strand Breaks Is Bypassed by Dampening Tel1 or Rad53 Activity
- A Tandem Duplicate of Anti-Müllerian Hormone with a Missense SNP on the Y Chromosome Is Essential for Male Sex Determination in Nile Tilapia,
- Ectodysplasin/NF-κB Promotes Mammary Cell Fate via Wnt/β-catenin Pathway
- The QTL within the Complex Involved in the Control of Tuberculosis Infection in Mice Is the Classical Class II Gene
- Identifying Loci Contributing to Natural Variation in Xenobiotic Resistance in
- Variation in Rural African Gut Microbiota Is Strongly Correlated with Colonization by and Subsistence
- A Flexible, Efficient Binomial Mixed Model for Identifying Differential DNA Methylation in Bisulfite Sequencing Data
- Competition between Heterochromatic Loci Allows the Abundance of the Silencing Protein, Sir4, to Regulate Assembly of Heterochromatin
- PLOS Genetics
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- UFBP1, a Key Component of the Ufm1 Conjugation System, Is Essential for Ufmylation-Mediated Regulation of Erythroid Development
- Metabolomic Quantitative Trait Loci (mQTL) Mapping Implicates the Ubiquitin Proteasome System in Cardiovascular Disease Pathogenesis
- Genus-Wide Comparative Genomics of Delineates Its Phylogeny, Physiology, and Niche Adaptation on Human Skin
- Encodes Dual Oxidase, Which Acts with Heme Peroxidase Curly Su to Shape the Adult Wing
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



