-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
The effect of clonidine on desfluraneconsumption using bispectral index monitoring during general anaesthesia: Randomised, double--blind, placebo controlled study
Efekt klonidinu na spotřebu desfluranu u celkové anestezie s monitorováním bispektrálního indexu
Cíl:
Cílem této randomizované, dvojitě slepé, placebem kontrolované studie je prokázat hypotézu, zda clonidin prohloubí anestezii, jejíž hloubka je měřená bispektrálním indexem, aby došlo ke snížení spotřeby desfluranu.Typ studie:
Randomizovná, dvojitě slepá, placebem kontrolovaná studie.Typ pracoviště:
Oddělení anesteziologie a intenzivní péče oblastní nemocnice.Materiál a metoda:
50 pacientů (23 mužů a 27 žen), kteří podstoupili celkovou anestezii pro elektivní totální endoprotézu kyčle či kolene, bylo náhodně rozděleno do dvou skupin. Pacientům z první skupiny byl 10 minut před úvodem do anestezie aplikován intravenózně klonidin v dávce 2 μg . kg-1, pacientům z druhé skupiny bylo podáno placebo. Hloubka anestezie byla udržována dle BIS s cílovou úrovní mezi 40 až 60. Po ukončení anestezie byla měřena spotřeba desfluranu. Po ukončení podávání desfluranu na konci operace byla měřena doba návratu vědomí. Pro statistické zpracování výsledků byl použit nepátový t-test.Výsledky:
Celkem bylo zařazeno 25 pacientů s klonidinem a 25 pacientů s placebem. Spotřeba desfluranu byla signifikantně nižší ve skupině s klonidinem (33,1 ± 5,0 g) oproti skupině s placebem (44,5 ± 10,6 g (p < 0,001). Nebyl pozorován rozdíl v době návratu vědomí, který činil 6,4 ± 3,8 min ve skupině s klonidinem a 6,2 ± 3,7 min ve skupině s placebem (p = 0,822).Závěr:
Intravenózně podaný clonidin snižuje spotřebu desfluranu během celkové anestezie. Tento šetřící efekt není spojen s prodloužením doby návratu vědomí.Klíčová slova:
klonidin – desfluran – BIS – celková anestezie
Authors: Nováček Martin 1,2; Sanders Graeme 3
Authors place of work: Consultant Anaesthetist, Department of Anaesthesia and Intensive Care, Regional Hospital in Kolin, Kolin, Czech Republic 1; Locum Consultant Anaesthetist, Department of Anaesthesia and Critical Care, Medway Maritime Hospital, Gillingham, Kent, United Kingdom 2; Consultant Anaesthetist, Department of Anaesthesia and Critical Care, Medway Maritime Hospital, Gillingham, Kent, United Kingdom 3
Published in the journal: Anest. intenziv. Med., 25, 2014, č. 6, s. 409-417
Category: Anesteziologie - Původní práce
Summary
Objective:
This study was designed to test the hypothesis that clonidine deepens general anaesthesia as measured by the bispectral index (BIS) and allows the dose of desflurane to be reduced.Design:
Randomised, double-blind, placebo controlled study.Setting:
Department of Anaesthesia and Intensive Care of Regional and District General Hospital.Materials and methods:
Fifty patients undergoing general anaesthesia for elective total hip or total knee replacement were randomly allocated into two groups. The treatment group had 2 μg . kg-1 clonidine administered intravenously 10 minutes before general anaesthesia induction and the control group was given an intravenous placebo. Depth of anaesthesia was guided by BIS with a target level between 40 and 60. The consumption of desflurane during anaesthesia was measured. After stopping desflurane administration at the end of surgery, time to return of consciousness (ROC) was recorded. Unpaired t-test was used for statistical analyses.Results:
Twenty five patients with clonidine and 25 with placebo were enrolled. The consumption of desflurane was significantly lower in the clonidine group - 33.1 ± 5.0 g, vs. the placebo group -44.5 ± 10.6 g (p < 0.001).No difference was found in the average time to ROC. This was 6.4 ± 3.8 min in the clonidine group vs. 6.2 ± 3.7 min in the placebo group (p = 0.822).Conclusion:
Intravenous clonidine decreases the consumption of desflurane during general anaesthesia. This sparing effect is not associated with increased time to ROC.Keywords:
clonidine – desflurane – BIS – general anaesthesiaBACKGROUND
Clonidine is usually used in anaesthetic practise as premedication, for deliberate hypotension or to treat hypertension during anaesthesia. It is a centrally acting alpha-2 receptor agonist with a variety of beneficial effects during and after anaesthesia [1]. Alpha-2 adrenoreceptor agonists blunt peri-operative stress responses, including haemodynamic responses to laryngoscopy and intubation of the trachea [2]. After emergence from general anaesthesia with the use of potent volatile agent, patients may show a hyperdynamic haemodynamic profile that can be attenuated with alpha-2 agonists [1].
Intravenous clonidine results in a decrease in bispectral index (BIS) during propofol anaesthesia and allows reduction of the target concentration of propofol in order to maintain a certain BIS level [3,4]. Clonidine affects the electroencephalogram (EEG) in a variety of ways: it increases slow-wave activity (delta) and attenuates the physiological alpha fluctuations. Although no data exist regarding the specific effect of clonidine on the BIS, clonidine causes sedation and therefore may also affect the BIS. Anaesthesia guided by BIS can reduce the anaesthetic requirement and decrease the incidence of observed awareness [5]. Several studies have demonstrated that alpha-2 adrenoreceptor agonists reduce the minimal alveolar concentration (MAC) and consumption of inhalational anaesthetics [6,7]. However, we could not find any published study on their effect on desflurane consumption.
The main aim of the study was to ascertain whether clonidine can decrease the consumption of desflurane during general anaesthesia for major joint replacement. Due to the sedative effect of clonidine, an extended time to return of consciousness (ROC) might be expected. Therefore, as a secondary aim, we evaluated the effect of clonidine on ROC following general anaesthesia.
METHODS
The study was approved by the East Kent Local Research Ethics Committee (Ref: 06/Q1803/45) and registered at clinicaltrialsregister.eu (EudraCT number 2006-003139-65). A pilot study was carried out at the Medway Maritime Hospital, Gillingham, Kent, United Kingdom when seven patients were enrolled. The second part of the study was completed after regional committee approval at the General Hospital in Kolin, Czech Republic (Ref: EK/8/2012), where a principal investigator was appointed. Day before the procedure after written informed consent had been obtained, 57 patients of American Society of Anesthesiologists’ status (ASA) I, II or III, undergoing general anaesthesia for elective total hip or total knee replacement lasting at least 45 min were randomly allocated into two groups. Sealed envelope method was used for randomisation. One group had clonidine administered 10 min before general anaesthesia induction, and the other was given an intravenous placebo.
The study exclusion criteria were patients with serious co-morbidities (defined as ASA IV), age less than 18 years, renal or hepatic disease, those on digoxin or beta-blocker treatment, preoperative blood pressure less than 100 mmHg systolic, patients taking medication known to alter the MAC (chronic use of sedative drugs, alcoholism), hypersensitivity to clonidine, sick sinus syndrome, AV block, bradycardia, congestive heart failure, acute myocardial infarction in the past, Raynaud’s syndrome or other occlusive peripheral vascular disease and depression.
All the patients received midazolam 7.5 mg orally 60 minutes before anaesthesia as premedication. Placebo (0.9% sodium chloride 100ml) or clonidine 2 µg . kg-1 in 100 ml 0.9% sodium chloride was given intravenously over 10 min before induction. The appropriate solution of clonidine or placebo was prepared by a person not participating in the study to ensure the double-blind character of the trial.
Following 3 minutes of preoxygenation with O2 8 l . min-1, propofol 2–2.5 mg . kg-1 and sufentanil 0.15 µg . kg-1 were used for anaesthesia induction. Rocuronium 0.6 mg . kg-1 intravenous was given to facilitate tracheal intubation with a cuffed tube. Anaesthesia was maintained with desflurane in a mixture of oxygen and air, with an oxygen inspired fraction titrated to 0.5. Volume Control ventilation was standard ventilatory mode. Tidal volume was calculated at 6 ml . kg-1 of ideal body weight. Ventilation was adjusted to maintain an end-tidal CO2 between 4.5 and 5 kPa. Analgesia was provided with sufentanil boluses 5–10 µg in incremental doses. Fresh gas flow was 4 l . min-1 for the first 10 minutes following induction, then low flow anaesthesia was commenced and fresh gas flow was standardised at 1 l . min-1. Desflurane was titrated to maintain the BIS in the range of 40 to 60. Desflurane was stopped on completion of skin suturing and ventilation with O2 8 l . min-1 was provided until extubation of the trachea. The temperature of the patient was maintained between 36 and 37 degrees C with a forced air warming blanket and intravenous fluid warmer.
Along with standard anaesthesia monitoring, BIS monitoring with Quatro® sensors (Covidien) was commenced before induction of anaesthesia. BIS level, non-invasive blood pressure and heart rate were recorded every 5 min. The data collection started one minute before the anaesthesia induction (Time 0 in figures). The consumption of desflurane during anaesthesia was calculated by weighing the desflurane vaporiser before and after anaesthesia. A high resolution weighing scale SI-132 Excell (Excell Precision Ltd) was used. The time from stopping desflurane to return of consciousness was measured. The consumption of sufentanil and rocuronium was also measured. The duration of anaesthesia from intravenous induction to termination of desflurane administration was recorded in minutes. Demographic data of patients such as ASA status, gender, weight, height and body mass index (BMI) were collected. The use of emergency drugs such as atropine, ephedrine or metoprolol because of bradycardia, hypotension or hypertension was collected as well.
For statistical analysis statistical software SPSS 20 was used. Patients’ individual data for normally distributed variables (BIS, HR, systolic and diastolic BP) were averaged every five minutes, Kolmogorov Smirnov test was used. Data is presented as means (SD). Statistical analysis was performed using the unpaired t-test for differences between the clonidine and the placebo group. Use of emergency drugs such as atropine, ephedrine and metoprolol was analysed using Fisher’s exact test. ASA score was analysed using the chi-square test. Significance level was set at 5%.
RESULTS
57 patients were studied, 7 patients from the pilot study were excluded and 50 patients (23 male and 27 female) were included in the statistical analysis. The demographic data are presented in Table 1. No significant differences in patients’ weight, height and BMI were found. The clonidine group involved significantly younger patients 60.3 (10.6) years compare to 65.6 (7.0) years in placebo group (p = 0.043). Mean duration of anaesthesia was similar in both groups (Table 2): 69.0 (9.5) min in the clonidine group and 71.9 (15.9) min in the placebo group (p = 0.435). A very similar level of depth of anaesthesia was maintained in both groups (Table 2, Fig.1), BIS 44.7 (5.1) in clonidine group and 44.3 (5.6) in placebo group (p = 0.824). A statistically significant decrease in desflurane consumption in the clonidine group was observed 33.1 (5.0) g versus 44.5 (10.6) g in placebo group(p < 0.001), as shown in Table 3. Fig. 2 shows a significant decrease in systolic blood pressure in the clonidine group 109.0 (13.7) mmHg versus 117.6 (15.9) mmHg in the placebo group (p = 0.047). Diastolic blood pressure was also lower in clonidine group 69.1 (13.8) mmHg versus 75.7 (12.1) mmHg in placebo group but not significantly (p = 0.078) as shown in Fig. 3.
Tab. 1. Characteristic of demographic data in clonidine or placebo group in patients undergoing total hip or knee replacement 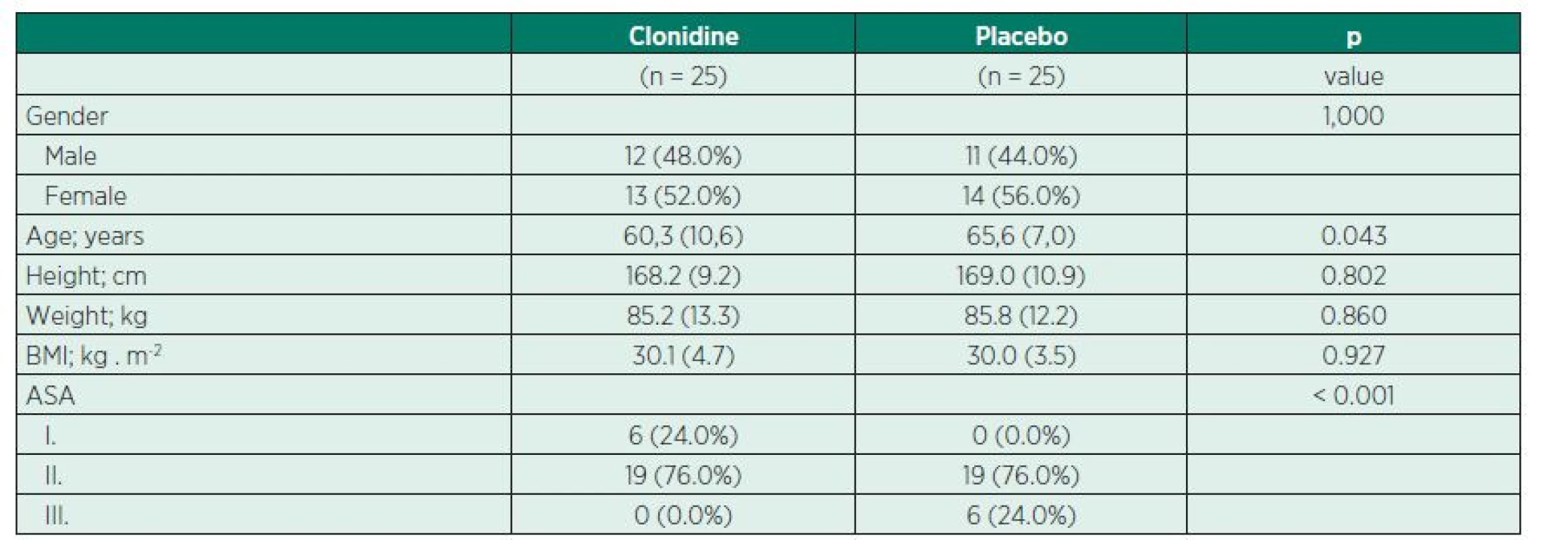
Data are presented as number (proportion) or mean (SD). Tab. 2. Summary of intraoperative BIS, haemodynamic variable, time of anaesthesia and time of return of consciousness (ROC) in clonidine or placebo group 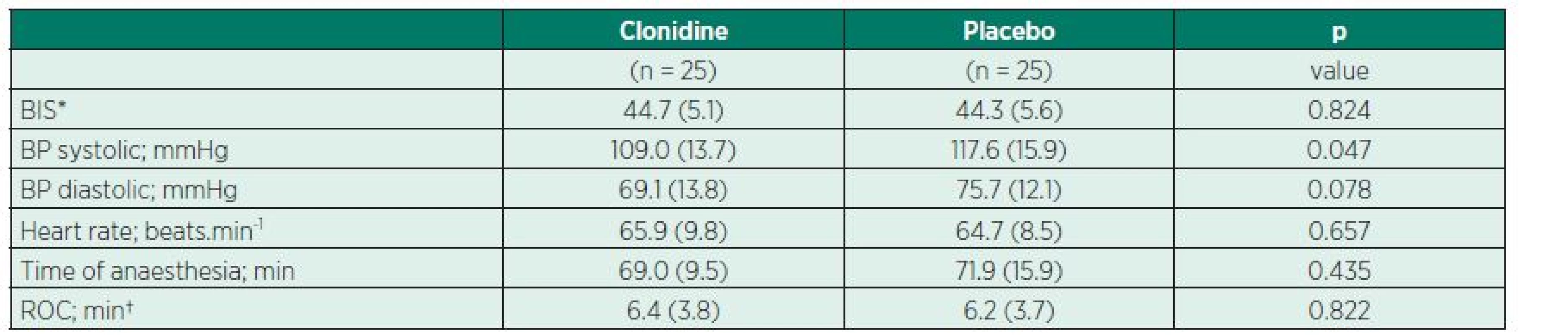
* BIS; bispectral index † ROC; return of consciousness Values are presented as mean (SD). Fig. 1 BIS levels during general anaesthesia in patients receiving clonidine or placebo. No significant difference between groups. 
Fig. 2 Systolic blood pressure during general anaesthesia in patients receiving clonidine or placebo. Significant decrease of systolic blood pressure in clonidine group (p = 0.047). 
Fig. 3 Diastolic blood pressure during general anaesthesia in patients receiving clonidine or placebo. No significant difference between groups. 
No difference in time to ROC was found (Table 2). Time to ROC was 6.4 (3.8) minutes in the clonidine group versus 6.2 (3.7) minutes in the placebo group (p = 0.822).
Heart rate (Fig. 4), consumption of sufentanil and consumption of rocuronium did not change significantly after clonidine administration (Table 3). There was a slightly increased requirement for atropine administration in the clonidine group, but this did not reach significance(p = 0.463). The need for ephedrine administra-tion was higher in the placebo group, but was not statistically significant (Table 4).
Tab. 3. Consumption of anaesthetic drugs in clonidine or placebo group 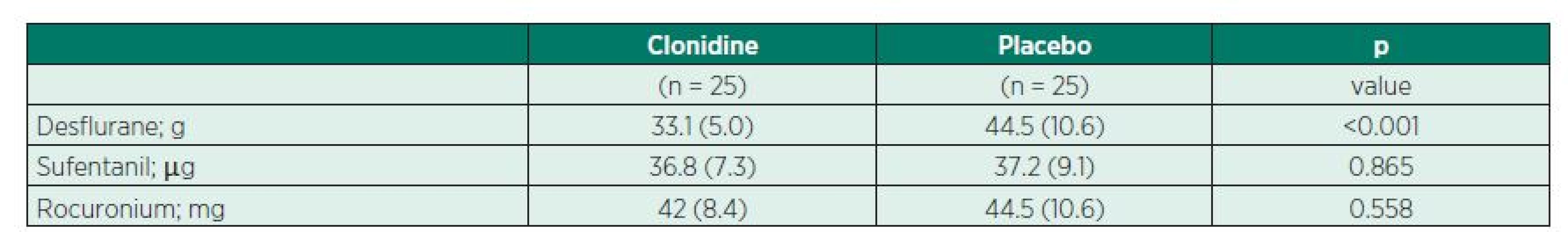
Values are presented as mean (SD). Tab. 4. Use of emergency drugs in clonidine or placebo group 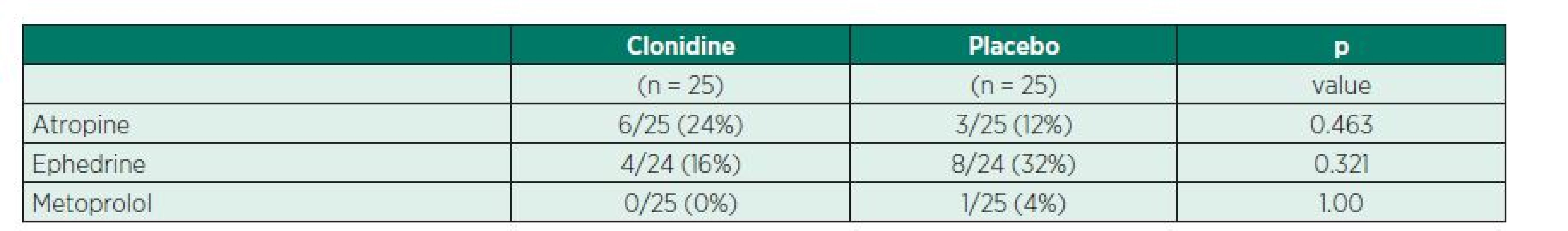
Values are presented as number (proportion). Fig. 4 Heart rate during general anaesthesia in patients receiving clonidine or placebo. No significant difference between groups. 
DISCUSSION
Intravenous clonidine significantly decreases the consumption of desflurane during general anaesthesia. The consumption of desflurane was 25.5% lower compared to the placebo group. The reduction of consumption of volatile agent fol-lowing clonidine administration varies in studies. The first published report demonstrated a reduction of halothane requirements following clonidine by 42% in an experimental dog model [7]. Another study showed clonidine had a dose related effect decreasing the minimal alveolar concentration (MAC) of isoflurane during BIS guided general anaesthesia [6]. On the other hand, no influence of clonidine on sevoflurane requirement was reported by De Deyne group [8]. Volatile agent sparing properties of the alpha 2 adrenoreceptors may be related to their sedative and analgesic properties. This action is mainly at the spinal cord level. There is good evidence that the MAC of volatile agent is related to their action at the spinal rather than cerebral level [9]. Reduction of intravenous anaesthetic drugs administration is documented as well. Propofol requirements following clonidine administration is decreased by nearly 20% [3]. Plasma propofol concentration in the clonidine group was 10% less than in the placebo group during lower extremity vascular surgery [4].In our study there was no difference in time from stopping the volatile agent to emergence (ROC) in the two groups. This may be related to BIS guided depth of anaesthesia. Titration of volatile agent according to BIS facilitates recovery after anaesthesia [10]. We use a modest dose of clonidine pre-treatment 2 µg . kg-1 intravenous compared to other studies, where doses up to 10 µg . kg-1 were used. Larger dose of clonidine may allow greater reduction in anaesthetic drug use, but may lengthen the time required for recovery from anaesthesia [11]. Another study showed no effect of clonidine on ROC [3].
Despite the analgesic effect of clonidine, no difference in consumption of sufentanil was observed. This is similar to the results of another study, describing similar opioid requirements during aortic surgery [12]. Other studies show a reduction in fentanyl consumption during general anaesthesia for cardiac surgery following clonidine administration [13,14].
A significant decrease by 7.5% in systolic bloodpressure was observed in the clonidine group and a non-significant decrease in diastolic blood pres-sure. This is similar to other works and can be explained by clonidine’s hypotensive effect.
Mean heart rate was similar in both groups. In similar studies, there is a clear dose dependent relationship. The higher the dose of clonidine, lower the heart rate. One report showed a decrease in heart rate of 20% with a clonidine dose of 6 µg . kg-1 [7].A more frequent need for bradycardia treatment was observed in the clonidine group, but this was not statistically significant. Surprisingly, ephedrine was administered more often in the placebo group for hypotension treatment but without reaching statistical significance.
Depth of anaesthesia is very important in anaesthetic practise. Estimation of depth of anaesthesia without proper measurement can be inaccurate. The routine monitoring of visual signs of awareness such as lacrimation, sweating and movements has been used for decades but is unreliable as an indicator of depth of anaesthesia. Different tools to measure the depth of anaesthesia are available nowadays. The most commonly used is the BIS system. It is estimated, that approximately 17% of surgical procedures under general anaesthesia or deep sedation in the United States are monitored with the use of BIS system [15] but only 1.8% in the United Kingdom [16]. Intraoperative awareness has a reported incidence of 0.1–0.2% [17,19] and can subsequently cause psychological symptoms [20]. Latest research from the UK shows lower incidence of awarenessof 1 : 15 414 [15]. Many trials have been published evaluating whether BIS can reduce or exclude awareness during general anaesthesia, but results are still inconclusive. The most recent studies do not demonstrate the superiority of a BIS protocol over an end tidal anaesthetic agent concentration based protocol [21,22].
The relationship between the ASA grade and risk of awareness is demonstrated, higher ASA grades showing a higher incidence of awareness [22].The addition of drugs with potential influence on brain metabolic activity and reduction of EEG activity could be useful to decrease the consumption of volatile agents. Lidocaine administered intravenously reduces propofol consumption during total intravenous anaesthesia [23]. In contrast aminophylline was demonstrated to increase BIS in sevoflurane and propofol anaesthesia [24]. It was demonstrated that BIS monitoring could reduce the anaesthetic drug administration and facilitate recovery [10].
BIS guided anaesthesia can slightly reduce sevoflurane consumption by about 5% [25]. BIS guided anesthesia significantly decreased consumption of desflurane in morbidly obese patient compared with anaesthesia without BIS monitoring (by about 19%) [26]. Opioids which are a normal part of anaesthesia reduce the MAC of volatile agents, but there is a ceiling effect. Regardless of the dose of opioid, about 0.3 MAC of volatile agents is required to prevent awareness [27].The measurement of total consumption of volatile agent during anaesthesia is not routinely used, although some anaesthetic machines are equipped with appropriate software. The total amount of volatile agent administered during general anaesthesia to the patient is related to several factors. Fresh gas flow (FGF) is the most important. Minute Ventilation and body weight are other important factors. The medical and financial points of view do meet here. Use of low-flow techniques for delivery of FGF is routine in clinical practice. Automated control of end-tidal inhalational anaesthetic concentration is now pos-sible. When combined with low-flow anaesthesia you can significantly decrease the consumption of volatile agent [28].
From the financial point of view, clonidine is inexpensive (£0.29 (€0.34/{INPUT}.44) per 150 µg ampoule) and desflurane is expensive (£63.3 (€74/.6) per 240 ml). If clonidine reduces desflurane consumption by 25%, we save about £2.00 (€2.3/) per patient.
A very short time to ROC in both groups (6.4 min in clonidine group vs. 6.2 min in placebo) was observed. This could be caused by desflurane use for anaesthesia maintenance. Desflurane is a volatile agent with unique properties. Because it has the lowest blood-gas coefficient compared to the other inhaled agents, it has the fastest onset and emergence. Especially in bariatric surgery some studies show the much faster recovery times in patients anesthetised with desflurane than with sevoflurane [30]. Compared with sevoflurane, desflurane produced deeper anaesthesia measured by BIS at 1 MAC [29]. A major disadvantage of desflurane is the bronchoconstriction described in some studies (particularly in smokers) [27]. This was not observed in either group.
The main limitation of our study is when we consider the distribution of age and ASA grades in both groups. The group with clonidine involved younger and healthier ASA I and II patients. The placebo group involved older, ASA II and III pa-tients. Post hoc power analysis for primary outcome (desflurane consumption) showed sufficient number of patients in our study (power of the test 0.96). A lower anaesthetic requirement for older and more seriously ill patients should be considered.
CONCLUSION
Our trial confirmed that clonidine decreases the consumption of desflurane during general anaesthesia for hip and knee replacement. The expected decrease of blood pressure caused by clonidine was observed only with the systolic blood pressure. ROC from anaesthesia was not significantly longer in the clonidine group compared to the placebo group.
Acknowledgements
We would like to thank Dr A. Makowski and Dr B. Misztal for their initial help with the pilot study.
Competing interest
No external funding and no competing interest declared.
This study was presented at 32nd Congress of the Scandinavian Society of Anaesthesiology and Intensive Care Medicine, Turku, Finland, 26th August 2013
Do redakce došlo dne 17. 6. 2014.
Do tisku přijato dne 25. 9. 2014.
Adresa pro korespondenci:
MUDr. Martin Nováček
ARO Oblastní nemocnice Kolín, a. s.
Žižkova 146
280 02 Kolin
e-mail: martinnovacek@email.cz
Zdroje
1. Kamibayashi, T., Maze, M. Clinical uses of α2-adrenergic agonists. Anesthesiology., 2000, 93, p. 1345–1349.
2. Kulka, P. J., Tryba, M., Zenz, M. Dose-response effects of intravenous clonidine on stress response during induction of anesthesia in coronary artery bypass graft patients. Anesth. Analg., 1995, 80, p. 263–268.
3. Fehr, S. B., Zalunardo, M. P., Seifert, B. et al. Clonidine decreases propofol requirements during anaesthesia: effect on bispectral index. Br. J. Anaesth., 2001, 86, p. 627–632.
4. Morris, J., Acheson, M., Reeves, M., Myles, P. S. Effect of clonidine pre-medication on propofol requirements during lower extremity vascular surgery: a randomised controlled trial. Br. J. Anaesth., 2005, 95, p. 183–188.
5. Johansen, J. W., Sebel, P. S. Development and clinical application of electroencephalographic bispectrum monitoring. Anesthesiology., 2000, 93, p. 1336–1344.
6. El-Kerdawy, H. M. M., Van Zalingen, E. E., Bovill, J. G. The influence of α2-adrenoceptor agonist, clonidine, on the EEG and on the MAC of isoflurane. Eur. Journal Anaesthesiol., 2000, 17, p. 105–110.
7. Bloor, B. C., Flacke, W. E. Reduction in halothane anesthetic requirement by clonidine, an alpha-adrenergic agonist. Anesth. Analg., 1982, 61, p. 741–745.
8. De Deyne, C., Struys, M., Heylen, R. et al. Influence of intravenous clonidine pretreatment on anesthetic requirements during bispectral EEG-Guided sevoflurane anesthesia. J. Clin. Anaesth., 2000, 12, p. 52–57.
9. Rampil, I. J., King, B. S. Volatile anesthetics depress spinal motor neurons. Anesthesiology, 1996, 85, p. 129–134.
10. Song, D., Joshi, G. P., White, P. F. Titration of volatile anesthetics using bispectral index facilitates recovery after ambulatory anesthesia. Anesthesiology, 1997, 87, p. 3–10.
11. Goyagi, T., Tanaka, M., Nishikawa, T. Oral clonidine premedication reduces induction dose and prolongs awakening time from propofol-nitrous oxide anesthesia. Can. J. Anaesth., 1999, 46, p. 894–896.
12. Engelman, E., Lipszyc, M., Gilbart, E. et al. Effects of clonidine on anesthetic drug requirements and hemodynamic response during aortic surgery. Anesthesiology, 1989, 71, p. 178–187.
13. Flacke, J. W. Alpha2-adrenergic agonists in cardiovascular ane-sthesia. J. Cardiothor. and Vascular Anesth., 1992, 6, p. 344–359.
14. Ghignone, M., Quintin, L., Duke, P. C., Kehler, C. H., Calvillo, O.Effects of clonidine on narcotic requirements and hemodynamic responses during induction of fentanyl anesthesia and endotracheal intubation. Anesthesiology, 1986, 64, p. 36–42.
15. Orser, B. A. Depth-of-anesthesia monitor and the frequency of intraoperative awareness. N. E. J. Med., 2008, 358, p. 1189–1191.
16. Pandit, J. J., Cook, T. M., Jonker, W. R., O’Sullivan, E. A national survey of anaesthetists (NAP5 Baseline) to estimate an annual incidence of accidental awareness during general anaesthesia in the UK. Br. J. Anaesth., 2013, 110, p. 501–509.
17. Sandin, R. H., Enlund, G., Samuelsson, P., Lennmarken, C. Awareness during anaesthesia: a prospective case study. Lancet, 2000, 355, p. 707–711.
18. Sebel, P. S., Bowdle, T. A., Ghoneim, M. M. et al. The incidence of awareness during anesthesia: a multicenter United States study. Anesth. Analg., 2004, 99, p. 833–839.
19. Mashour, G. A., Shanks, A., Tremper, K. K. et al. Prevention of intraoperative awareness with explicit recall in an unselected surgical population: randomised comparative effectiveness trial. Anesthesiology, 2012, 117, p. 717–725.
20. Leslie, K., Chan, M. T., Myles, P. S., Forbes, A., McCul-loch, T. J. Posttraumatic stress disorder in aware patients from the B-aware trial. Anesth. Analg., 2010, 110, p. 823–828.
21. Avidan, M. S., Zhang, L., Burnside, B. A. et al. Anesthesia awareness and the bispectral index. N. E. J. Med., 2008, 358, p. 1097–1108.
22. Avidan, M. S., Jacobsohn, E., Glick, D. et al. Prevention of intraoperative awareness in a high-risk surgical population. N. E. J. Med., 2011, 365, p. 591–600.
23. Altermatt, F. R., Bugedo, D. A., Delfino, A. E. et al. Evaluation of the effect of intravenous lidocaine on propofol requirements during total intravenous anaesthesia as measured by bispectral index. Br. J. Anaesth., 2012, 108, p. 979–983.
24. Hüpfl, M., Schmatzer, I., Buzath, A. et al. The effects of aminophylline on bispectral index during inhalational and total intravenous anaesthesia. Anaesthesia, 2008, 63, p. 583–587.
25. Başar, H., Ozcan, S., Buyukkocak, U., Akpinar, S., Apan, A. Effect of bispectral index monitoring on sevoflurane consumption. Eur. Journal Anaesthesiol, 2003, 20, p. 396–400.
26. Ibrahim, T. H., Yousef, G. T., Hasan, A. L. A., Elseduky, H. I. Effect of bispectral index monitoring on desflurane consumption and recovery time in morbidly obese patients undergoing laparoscipic sleeve gastrectomy. Anaesthesia Essays and Researches, 2013, 7, p. 89–93.
27. Moppett, I. Inhalational anaesthetics. Anaesth Intens Care Med., 2012, 13, p. 348–353.
28. Singaravelu, P., Barclay, P. Automated control of end-tidal inhalation anaesthetic concentration using GE Aisys Carestation. Br. J. Anaesth., 2013, 110, p. 561–566.
29. Jin-Kyoung, K., Duk-Kyung, K., Myeong-Jin Lee Relationship of bispectral index to minimum alveolar concentration during isoflurane, sevoflurane or desflurane anaesthesia. Journal of International Medical Research [online]. 2013 [cit.2013-23-12]. Dostupné na www: http://imr.sagepub.com/content/early/2013/12/23/0300060513505525
30. Kaur, A., Jain. A. K., Seghal, R., Sood, J., Hemodynamics and early recovery characteristic of desflurane versus sevoflurane in bariatric surgery. J. Anaesthesiol. Clin. Pharmacol., 2013, 29, p. 36–40.
Štítky
Anesteziologie a resuscitace Intenzivní medicína
Článek Umělá plicní ventilaceČlánek ResuscitaceČlánek 22. Hoderův denČlánek Ceny ČSARIM za rok 2013Článek Konference a kongresyČlánek Pokyny pro autoryČlánek Rejstříky
Článek vyšel v časopiseAnesteziologie a intenzivní medicína
Nejčtenější tento týden
2014 Číslo 6- Jak souvisí postcovidový syndrom s poškozením mozku?
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
- Neodolpasse je bezpečný přípravek v krátkodobé léčbě bolesti
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Léčba akutní pooperační bolesti z pohledu ortopeda
-
Všechny články tohoto čísla
- Pohnuté loučení s peroperační beta-blokádou
- The effect of clonidine on desfluraneconsumption using bispectral index monitoring during general anaesthesia: Randomised, double--blind, placebo controlled study
- Perioperative myocardial ischaemia and myocardial infarction
- Echocardiographic evaluation of the right ventricular function
- Umělá plicní ventilace
- „Nejasná“ hyperglykémie u pacientů v intenzivní péči – nezapomínejme na farmaka
- Resuscitace
-
Praktická doporučení pro vyšetření kardiovaskulárních funkcí a perioperační péči u pacientů podstupujících nesrdeční operaci
(American College of Cardiology/American Heart Association 2014) - Stanovisko ČRR k používání metod mimotělní kardiopulmonální resuscitace u dospělých pacientů s náhlou zástavou oběhu
- Pravidla pro rozhodování pacientů o poskytování zdravotní péče
- 22. Hoderův den
- Re: Kandidová sepse jako komplikace u pacienta s polytraumatem
- Ceny ČSARIM za rok 2013
- Konference a kongresy
- Komise pro historii našeho oboru hledá nové členy či spolupracovníky
- Pokyny pro autory
- Rejstříky
- Anesteziologie a intenzivní medicína
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Echocardiographic evaluation of the right ventricular function
- Perioperative myocardial ischaemia and myocardial infarction
- Umělá plicní ventilace
- Pravidla pro rozhodování pacientů o poskytování zdravotní péče
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



