Effect of Pneumococcal Conjugate Vaccination on Serotype-Specific Carriage and Invasive Disease in England: A Cross-Sectional Study
Background:
We investigated the effect of the 7-valent pneumococcal conjugate vaccine
(PCV7) programme in England on serotype-specific carriage and invasive
disease to help understand its role in serotype replacement and predict the
impact of higher valency vaccines.
Methods and Findings:
Nasopharyngeal swabs were taken from children <5 y old and family members
(n = 400) 2 y after introduction
of PCV7 into routine immunization programs. Proportions carrying
Streptococcus pneumoniae and serotype distribution
among carried isolates were compared with a similar population prior to PCV7
introduction. Serotype-specific case∶carrier ratios (CCRs) were
estimated using national data on invasive disease. In vaccinated children
and their contacts vaccine-type (VT) carriage decreased, but was offset by
an increase in non-VT carriage, with no significant overall change in
carriage prevalence, odds ratio 1.06 (95% confidence interval
0.76–1.49). The lower CCRs of the replacing serotypes resulted in a
net reduction in invasive disease in children. The additional serotypes
covered by higher valency vaccines had low carriage but high disease
prevalence. Serotype 11C emerged as predominant in carriage but caused no
invasive disease whereas 8, 12F, and 22F emerged in disease but had very low
carriage prevalence.
Conclusion:
Because the additional serotypes included in PCV10/13 have high CCRs but low
carriage prevalence, vaccinating against them is likely to significantly
reduce invasive disease with less risk of serotype replacement. However, a
few serotypes with high CCRs could mitigate the benefits of higher valency
vaccines. Assessment of the effect of PCV on carriage as well as invasive
disease should be part of enhanced surveillance activities for PCVs.
:
Please see later in the article for the Editors' Summary
Published in the journal:
. PLoS Med 8(4): e32767. doi:10.1371/journal.pmed.1001017
Category:
Research Article
doi:
https://doi.org/10.1371/journal.pmed.1001017
Summary
Background:
We investigated the effect of the 7-valent pneumococcal conjugate vaccine
(PCV7) programme in England on serotype-specific carriage and invasive
disease to help understand its role in serotype replacement and predict the
impact of higher valency vaccines.
Methods and Findings:
Nasopharyngeal swabs were taken from children <5 y old and family members
(n = 400) 2 y after introduction
of PCV7 into routine immunization programs. Proportions carrying
Streptococcus pneumoniae and serotype distribution
among carried isolates were compared with a similar population prior to PCV7
introduction. Serotype-specific case∶carrier ratios (CCRs) were
estimated using national data on invasive disease. In vaccinated children
and their contacts vaccine-type (VT) carriage decreased, but was offset by
an increase in non-VT carriage, with no significant overall change in
carriage prevalence, odds ratio 1.06 (95% confidence interval
0.76–1.49). The lower CCRs of the replacing serotypes resulted in a
net reduction in invasive disease in children. The additional serotypes
covered by higher valency vaccines had low carriage but high disease
prevalence. Serotype 11C emerged as predominant in carriage but caused no
invasive disease whereas 8, 12F, and 22F emerged in disease but had very low
carriage prevalence.
Conclusion:
Because the additional serotypes included in PCV10/13 have high CCRs but low
carriage prevalence, vaccinating against them is likely to significantly
reduce invasive disease with less risk of serotype replacement. However, a
few serotypes with high CCRs could mitigate the benefits of higher valency
vaccines. Assessment of the effect of PCV on carriage as well as invasive
disease should be part of enhanced surveillance activities for PCVs.
:
Please see later in the article for the Editors' Summary
Introduction
Streptococcus pneumoniae is a bacterium that frequently colonises the human nasopharynx. Apart from disease outcomes such as sinusitis, otitis media, and community-acquired pneumonia, which result from direct spread from the nasopharynx, the pneumococcus can invade the bloodstream and cause septicaemia, meningitis, and invasive pneumonia. Most carriage episodes, however, do not result in either local or systemic disease. It is believed that the propensity to cause invasive disease in healthy individuals—termed invasiveness—is largely determined by the characteristics of the pneumococcus' polysaccharide capsule, although the explicit underlying mechanisms are yet to be identified [1],[2]. On the basis of the immune response to differences in capsular polysaccharide structure, more than 90 serotypes causing invasive disease have been described [3].
A pneumococcal conjugate vaccine (PCV7) that induces anticapsular antibodies against the seven serotypes, which at that time were responsible for most of the pneumococcal invasive disease in the United States (US), was introduced into the US childhood immunisation schedule in 2000 and the majority of the developed world subsequently. Since PCV7 is protective against invasive pneumococcal disease (IPD) [4] and carriage [5],[6], the assumption of protection of the unvaccinated against vaccine type (VT) IPD through herd immunity played a major role in evaluating the likely impact and cost-effectiveness of vaccination [7]. Prevention of VT carriage, however, creates a potential ecological niche in the nasopharynx for previously less prevalent serotypes to emerge (replacement).
The extent to which the benefits of herd immunity will be offset by serotype replacement is hard to predict [8] and may vary by country depending on local factors such as differences in serotype distribution before vaccination and the population demography. Hence, there is a need for enhanced surveillance to evaluate the effect of vaccination in different epidemiological settings. Most surveillance systems focus on IPD and have shown large reductions in the numbers of VT cases in the targeted age groups, irrespective of vaccine schedule [9]–[11]. However, differences were observed in the indirect effect (i.e., the degree of induced herd immunity and the level of non–vaccine-type [NVT] replacement), the reasons for which remain unclear but may include vaccine coverage, time since introduction of PCV, and sensitivity of the reporting system [12].
Monitoring disease outcomes provides little insight into the underlying mechanisms that determine herd immunity and serotype replacement. For this, carriage data are essential. Carriage studies in children from Massachusetts and Norway suggest full replacement of pneumococcus in carriage after PCV7 introduction [13],[14]. The implications of changes in serotype-specific carriage prevalence for expression as IPD will, however, depend on the invasiveness of individual serotypes, which is reflected by the case∶carrier ratio (CCR). Invasiveness has only been studied in one of these settings and was restricted to children [15],[16]. Improving our understanding of this relationship, largely determined by the invasiveness potential of the replacing NVT organisms, is essential to understanding the effect of PCV7 in different epidemiological settings.
In September 2006, PCV7 was introduced into the immunisation schedule in the United Kingdom as a 2/4/13-month routine schedule with a catch-up for children up to 2 y of age. Information on carriage in England prior to PCV7 introduction is available from a longitudinal study conducted in 2001/2002 in index children and their household members. We report here the results of a cross-sectional carriage study conducted in a demographically similar population in 2008/2009. We compare our post-PCV7 findings with the pre-PCV7 baseline both for carriage and IPD to help understand the serotype-specific effects of PCV7 on both carriage and IPD and use this analysis to predict the potential impact of higher valency conjugate vaccines on herd immunity and replacement disease.
Methods
Study Population
Children born since 4 September 2004 and thus eligible for routine or catch-up PCV were recruited along with family members from general practices in Hertfordshire and Gloucestershire. Exclusion criteria were: moderate to severe disability, cerebral palsy, neurological disorders affecting swallowing, ear, nose, and throat disorders affecting the anatomy of the ear, or immunosuppression. The NHS National Research Ethics Service approved the study protocol. Written informed consent was obtained from adult study participants and from a parent/guardian of study children prior to enrolment. Information was collected on participants' age, gender, household size, number of smokers in household, recent antibiotic treatment, hours in day-care and PCV7 vaccination history.
To compare to prevaccination carriage in England, we used the results from a longitudinal study carried out in 2001/2002 in families attending the same general practices in Hertfordshire in which swabs were taken each month over a 10-mo period [17]. At that time, serotype 6C could not be distinguished from 6A, but in 2009, 19 of the 122 serotype 6As from the earlier study were randomly retested, six of which were found to be 6C. We have assumed that this proportion (32%) holds for the rest of the 6A carriage isolates from the 2001/2002 study.
Specimen Collection and Testing
Nasopharyngeal swabs (calcium-alginate) were taken between April 2008 and November 2009 by trained nurses and placed directly in STGG broth. Samples collected at Hertfordshire were sent by same day courier to the Respiratory and Systemic Infection Laboratory at the Centre for Infections (RSIL). They were stored overnight in at 2–8°C and frozen the next morning at −80°C. Samples collected at Gloucestershire were stored locally at the Gloucester Vaccine Evaluation Unit at −80°C and transferred to RSIL in batches on dry ice. On receipt the batches were stored at −80°C. The sample then was thawed, vortexed, and 50 µl STGG broth was placed onto each of Columbia blood agar plate (HPA media services) with optochin disc (MAST) and Streptococcus-selective Columbia blood agar plate (HPA media services) and streaked out. The plates were incubated overnight at 35°C with 5% CO2. Any colonies resembling pneumococcus were subjected to normal identification methods and serotyped using the standard laboratory protocol [18].
Statistical Analysis
Descriptive data analysis was performed in R 2.11.0 and Generalized Estimating Equations (GEEs) models were analysed with STATA 10.1. Exact binomial 95% confidence intervals (CIs) were obtained for carriage rates in 2008/2009 by age group (<5, 5–20,>20 y). To account for longitudinal design in the 2001/2002 study, we computed these carriage rates using a GEE model with exchangeable correlation structure. To determine the significance of changes in carriage for individual serotypes between 2001/2002 and 2008/2009, a Fisher exact test was used because of small numbers. When comparing overall carriage as well as vaccine and NVT carriage between periods, this comparison took account of the longitudinal design of the 2001/2002 along with other covariates by using a GEE model with exchangeable correlation structure and factors for study period, age in years, gender, whether the household has a smoker, and the number of children and adults in the household. For comparability with previously reported changes in carriage, the data were stratified into two age groups (<5 and ≥5 y).
For calculating the CCR the numbers of each serotype were extracted from the national surveillance database for England and Wales [19] for the epidemiological years 2001/2002 and 2008/2009 and related to data from the carriage studies conducted in the same years (Table S1). CCRs were calculated using serotype-specific carriage prevalence as denominator. Ages younger than 60 y were combined in both the IPD and carriage datasets. 95% CIs were calculated on the basis of the 95% CIs of the serotype-specific carriage prevalence assuming the national incidence data on IPD to be complete and not based on a population sample [19]. For serotypes with estimates in both datasets, Spearman's rank test was used to estimate the correlation of our estimates and those obtained by Sleeman and colleagues from a paediatric pre-PCV7 carriage dataset in one region of England corrected for duration of carriage [20].
Simpson's index for diversity was calculated to assess the change in diversity in the bacterial population following vaccination [21]. Ranked serotype distribution was compared to the prevaccination distribution and CIs were obtained using the methods described by Hanage and colleagues [22]. To ensure that only a single isolate per carriage episode was included we excluded consecutive swabs with the same serotype (this included swabs of more than one sample interval apart if the individual was not sampled in between) in the 2001/2002 study on the assumption that it was carriage persisting from the previous month.
Results
400 individuals were enrolled between 24 April 2008 and 9 November 2009. One participant withdrew before being swabbed and in 17 individuals swabbing had to be aborted early; these 18 participants were excluded from further analyses. The demographic features of the remaining 382 participants were similar to the participants in the 2001/2002 study, apart from the proportion of households with at least one smoker, which was lower in the more recent study (Table 1). Of 180 children eligible for catch-up or infant vaccination only four were unvaccinated.
A pneumococcus was grown from 127 of the 382 (33.2%) swabs and a serotype determined in 123 (97%). The most prevalent serotypes were 19A (10), 23B (9), 11C (8), 15B (8), 21 (8), and 6C (8). Compared to prevaccination levels, we found a significant reduction in carriage of VTs 6B, 14, 19F, 23F, and 6A. For the remaining PCV7 types no carriage episodes of serotypes 4 and 9V were found postvaccination, but prevaccination levels were too low to detect any significant change. VT 18C was identified in three out of 382 (0.79%) swabs in 2008/2009 and in 25 out of 3,868 (0.64%) in the 2001/2002 study. NVTs 33F, 7F, 10A, 34, 15B, 31, 21, 3, 19A, 15C, and 23A significantly increased (p<0.05) in carriage with odds of 40.9, 30.8, 20.4, 20.3, 16.5, 10.2, 8.2, 6.2, 4.5, 3.6, and 3.6, respectively. A significant increase was also found in serotypes 23B, 11C, 11B, 24F, and 33A, which were only detected in the postvaccination study.
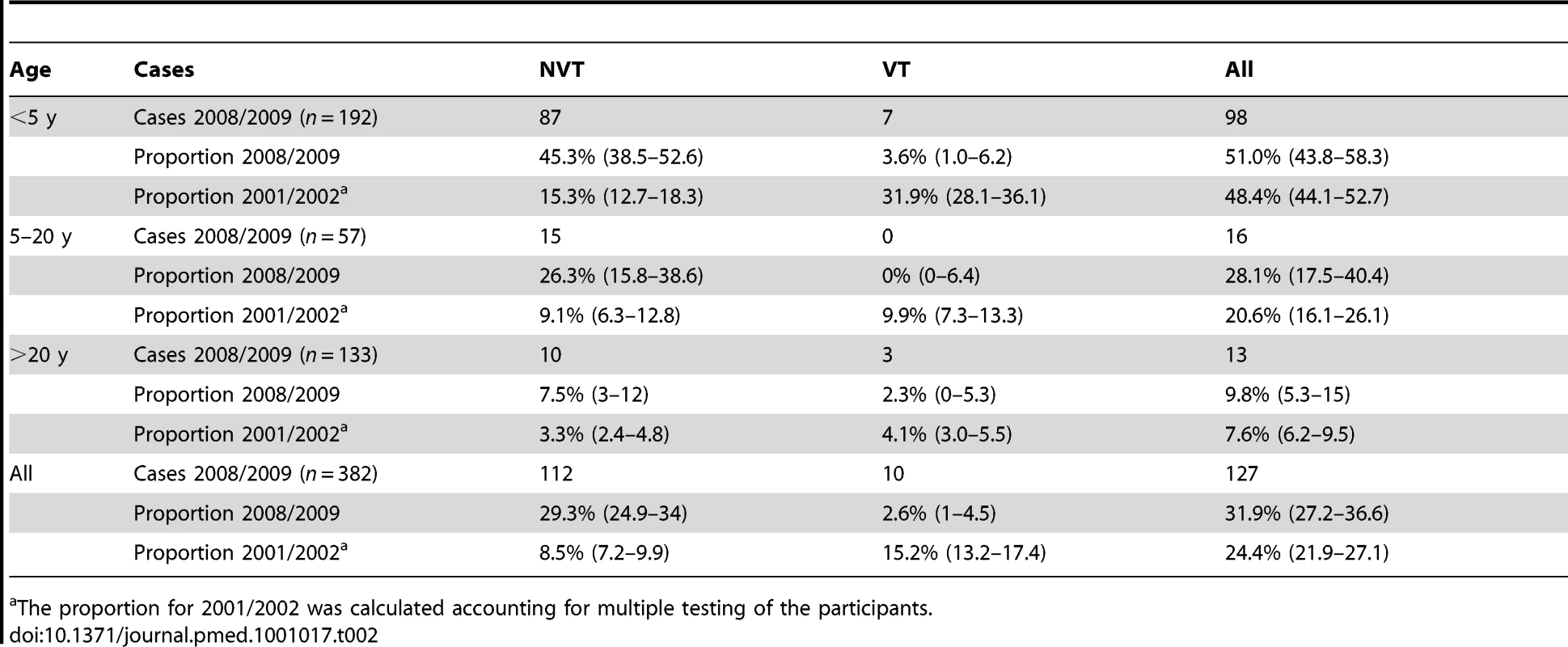
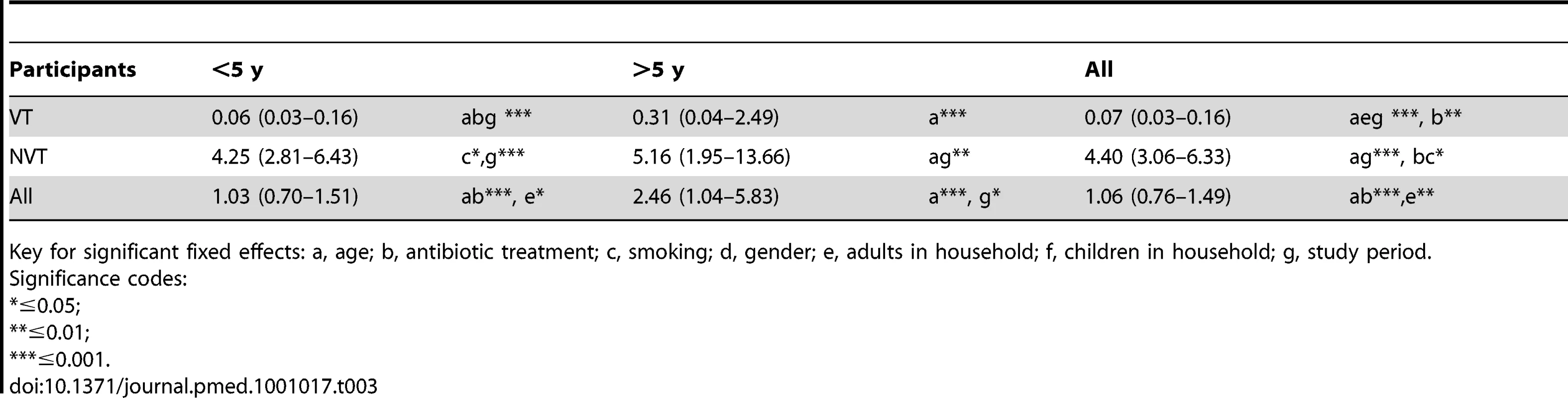
The proportion of swabs with VT and NVT serotypes according to age group in both studies is shown in Table 2. The odds ratio of VT and NVT carriage postvaccination compared to prevaccination using the GEE with binary outcome was estimated to be 0.07 95% CI (0.03–0.16) and 4.40 95% CI (3.06–6.33), respectively, with, no significant effect on overall carriage: 1.06 95% CI (0.76–1.49) (Table 3). When applying the same models to individuals younger than 5 y only, we found similar patterns. In individuals aged 5 y or older, we detected evidence for herd immunity and full serotype replacement as well (odds ratio [OR] 0.31 95% CI (0.04–2.49), 5.16 95% CI (1.95–13.66), respectively), although the reduction in VT carriage was not significant.
Simpson's index of diversity for the 2001/2002 samples was 0.908 95% CI (0.899–0.917); children: 0.891 95% CI (0.878–0.904) and adults: 0.936 95% CI (0.926–0.947). It increased significantly in the 2008/2009 samples to: 0.961 95% CI (0.953–0.969); children: 0.960 95% CI (0.949–0.971) and adults: 0.955 95% CI (0.928–0.982). Furthermore, the ranked frequency distribution of the serotypes, while similar in the prevaccination era in both children and adults in our study compared to children in Massachusetts, changed to become more distinct after vaccination (Figure 1).
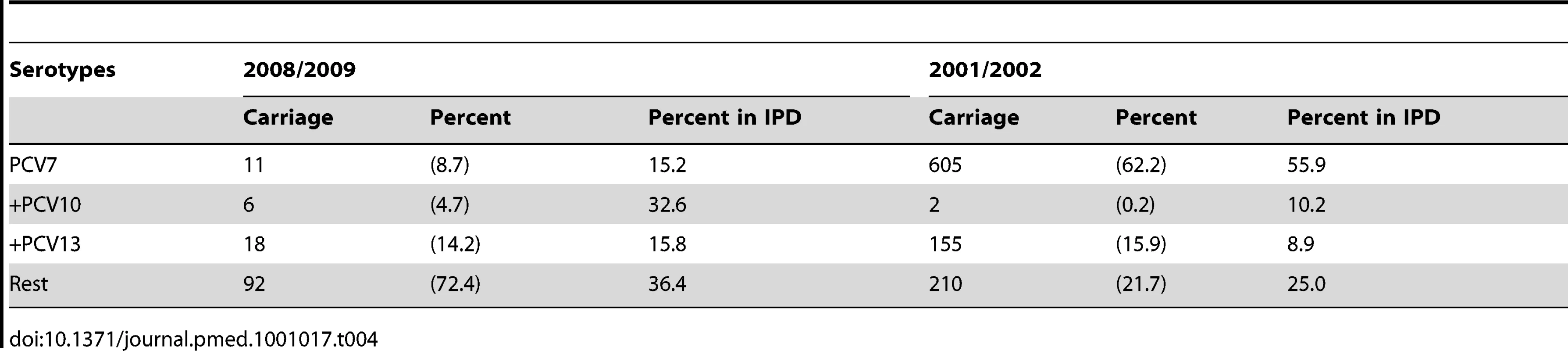
Prior to its introduction, PCV7 included types responsible for similar proportions of carriage episodes (62.2%) and disease (55.9%). In 2008/2009 the additional types covered by higher valency vaccines were more prevalent in IPD than carriage, particularly the additional three in PCV10, which comprised 32.6% of IPD but only 4.7% of carried isolates (Table 4).
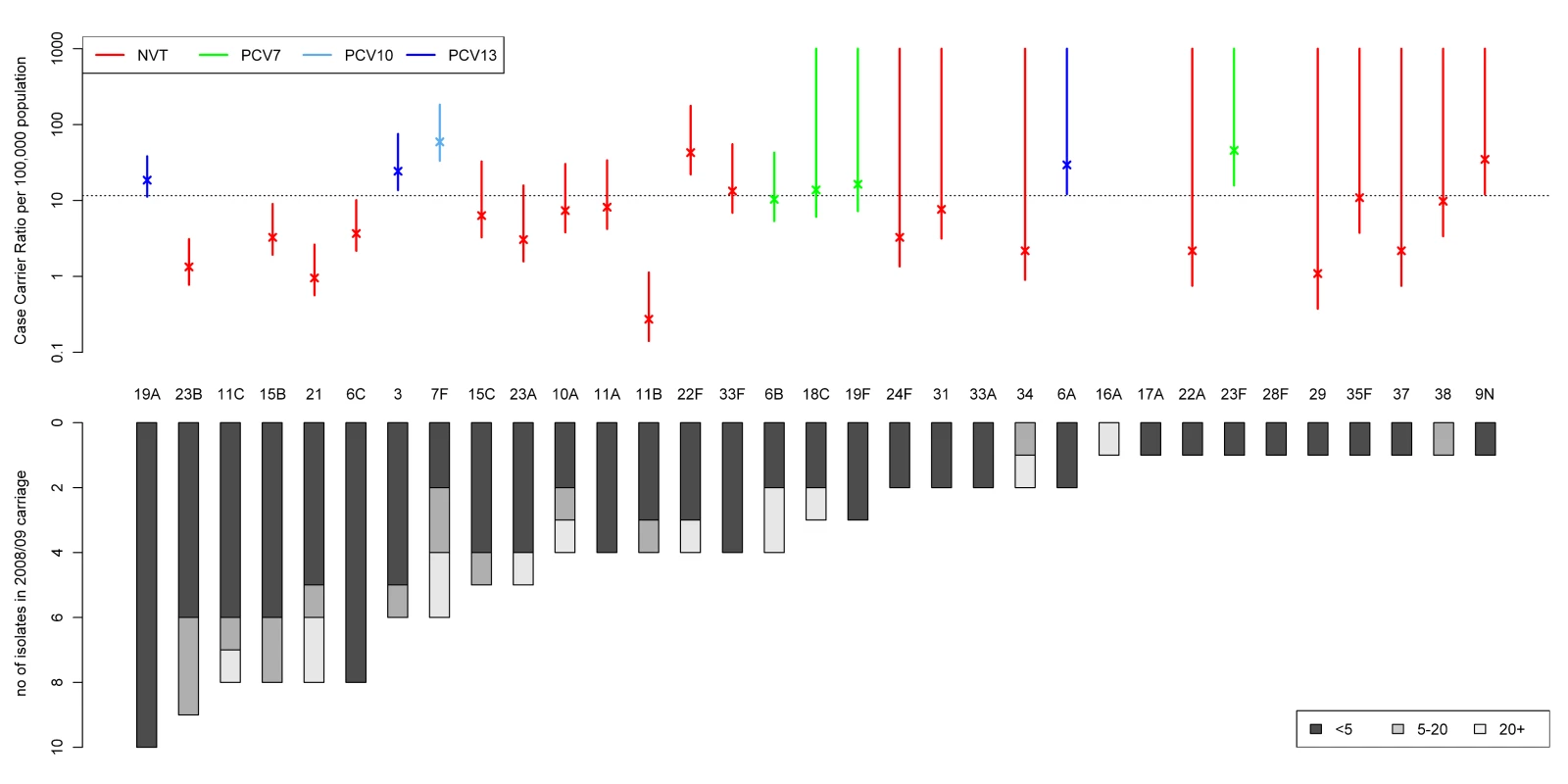
The ranking of carried serotypes by frequency of detection in the post-PCV7 dataset and their associated CCRs as estimated from our 2008/2009 carriage prevalence data are shown in Figure 2. CCR estimates were highly correlated (p<0.001, ρ = 0.72) to those from Sleeman and colleagues estimated from carriage incidence [20] and allow to distinguish the more from the less invasive serotypes. From the 15 most prevalent serotypes in carriage in 2008/2009 19A, 3, 7F, and 22F stand out with a generally higher CCR. Despite their high incidence in invasive disease serotypes 1, 8, 12F, 4, and 14 (1.14, 0.58, 0.25, 0.22, 0.14 cases per 100,000 population, respectively, in under 60 y olds in 2008/2009) were not detected in carriage. On the other hand, despite being found in 2008/2009 carriage serotypes, 11C, 16A, 17A, 28F, and 33A were not found in 2008/2009 IPD at all and only caused 0, 1, 0, 1, and 0 cases, respectively, of invasive disease out of over 13,000 isolates serotyped between July 2006 and June 2009.
Discussion
Our study documents the changes in carried pneumococci following the introduction of PCV7 in England and relates these to concomitant changes in disease in order to assess the invasiveness potential of the serotypes now predominating carriage. This knowledge is essential for understanding replacement pneumococcal disease and provides insight into the likely population impact of higher valency vaccines. As reported elsewhere [13],[14], we found a major reduction in VT carriage in vaccinated children under 5 y, but no overall change in carriage prevalence due to replacement with NVTs. In contrast, there was an overall reduction in IPD in this age group, illustrating that the outcome of the PCV programme as expressed in IPD is determined by the invasiveness potential of the individual NVTs emerging in carriage. Overall carriage prevalence in older unvaccinated siblings and parents was somewhat higher post-PCV7 as found in parents of 2 y olds in a vaccine trial with a 2-dose or a 2+1-dose schedule in the Netherlands [23]. This finding was due to a large increase in NVT and a smaller nonsignificant reduction in VT carriage. However, IPD in these older age groups has not shown an overall increase in the UK [24], indicative of the lower overall invasiveness of the replacing NVTs.
Our study shows that PCV7 provided protection against serotypes that were highly prevalent in both disease and carriage in the UK. The additional serotypes covered by PCV10 and PCV13 are now responsible for a large proportion of invasive disease but were found relatively rarely in carriage (Table 4). While further replacement in pneumococcal carriage is likely to occur after introduction of these higher valency vaccines, our findings suggest that since most of the potential replacement types identified have lower CCRs they will cause less invasive disease. However, serotypes like 22F and especially the ones not found in carriage but present in IPD (e.g., serotype 8 and 12F) could reduce the overall benefits of higher valency vaccines. Interestingly, the three additional serotypes covered by PCV10 had a very low carriage prevalence accounting for <5% of the carried serotypes in 2008/2009 but >30% of IPD cases, whereas the further three serotypes in PCV13 are more similar to the PCV7 serotypes, being similarly prevalent in carriage and disease. While changing to PCV10 has therefore less potential to prevent IPD than PCV13, it may cause fewer perturbations in the nasopharyngeal pneumococcal population. Comparative carriage studies in countries using PCV10 with those using PCV13, or with different PCV coverage of prevalent serotypes before introduction, would be informative to help understand the carriage dynamics underlying serotype replacement. These studies would ideally be repeated cross-sectional studies to monitor alterations in carriage prevalence, which could be linked to changes in serotype-specific IPD in the same population. The latter requires the continued microbiological investigation of suspected cases of invasive disease, including those in fully vaccinated children, in order to document the serotype-specific changes in IPD associated with vaccine-induced changes in carriage.
The diversity of the pneumococcal carriage population in the absence of any external pressure is thought to be relatively stable [22]. If this population is challenged by vaccination with a reduction in the dominance of a few highly prevalent types, the diversity increases and the population takes time to return to the previous level of diversity. Hanage and colleagues suggested methods of assessing these changes: Simpson's index of diversity and the concept of a typical distribution for the ranked frequency of the serotypes [22]. Applying these to our prevaccination carriage data, we see similar diversity in children and slightly higher diversity in adults, although the significance of this difference was not consistent between both methods. However, we found an increase in overall diversity in 2008/2009 as well as in children and in adults (although not significant in adults), consistent with the PCV7-induced changes in the bacterial population still evolving at that time. Evidence for this can also be found in the ongoing changes in non-PCV7 IPD in 2009/2010, prior to introduction of PCV13. These show a continuing increase in the six additional serotypes covered by PCV13 but a decrease in non-PCV13 serotypes in children under 2 y compared with 2008/209 [25]. With the introduction of PCV13 in the UK in March 2010 [26], it will not be possible to evaluate further the longer term impact of PCV7 on carriage and IPD, but it is important to note that PCV7 may continue to have an effect and therefore not all future changes will necessarily be attributable to PCV13.
Recently developed molecular serotyping methods found up to nine times higher proportions of multiple carriage than detectable with standard WHO culturing methods [27]. Using the WHO method we identified one (0.26%) multiple carriage episode in 2008/2009 and four (0.10%) in 2001/2002. Undetected episodes of multiple carriage would result in over estimation of CCRs. However, direct comparison of molecular and conventional serotyping methods have so far only been performed on specimens from developing countries where carriage prevalence is very high [28],[29]. In such settings, molecular methods might reveal more multiple carriage episodes than in countries such as England where carriage prevalence is lower. Furthermore, there is some evidence that detecting multiple serotype carriage is likely to primarily uncover carriage episodes of serotypes previously found to be less prevalent [30]. Therefore we believe that the potential bias introduced by the WHO standard culturing methods would have little impact on our inferences from the CCR, because we focus on the serotypes more common in carriage.
Our study has some limitations. First, the earlier study had a longitudinal design while the recent study was cross-sectional. However, we accounted for multiple testing of individuals in the earlier study as well as differences in age distribution within the age groups, gender, exposure to smoke, and household size by using a GEE, which is designed to fit the parameters of a generalised linear model in the presence of unknown correlation. Second, owing to the lack of power of serotype-specific carriage data in adults, we pooled data of children and adults to derive the CCR, despite different age distributions in the samples for IPD and carriage. Previously reported CCR estimates for children and adults in England and Wales [19] using the carriage data from the earlier study are highly correlated (Figure S1), supporting our use of pooled carriage data from children and adults in the later study. Third, secular changes in serotype distribution in IPD can occur in the absence of vaccination [31], which may be due to alterations in carriage prevalence. With the cross-sectional design of the 2008/2009 study, we were not able to account for these. However, in England the only major secular change in the serotypes causing IPD observed over the last decade has been in serotype 1, which was not detected in either our pre- or post-PCV7 carriage studies. Fourth, invasion is thought to follow shortly after acquisition of carriage rather than being a constant risk throughout the duration of carriage [32]. Thus, a further potential limitation of our study is that we estimate CCRs using carriage prevalence rather than the incidence of new carriage episodes, the latter being derived using prevalence and carriage duration. Few data on serotype-specific duration of carriage are published, and for the serotypes newly emerging after introduction of PCV7, no information is available. Therefore, we used carriage prevalence to get an estimate of the CCRs. Where information on CCRs estimated using carriage incidence was available [20], we found a high correlation with our estimates. Furthermore, our estimates for the CCRs were consistent with those derived from 2001/2002 carriage and IPD (unpublished data), showing that this measure is stable over time. Hence we are confident that our estimates of the CCR can distinguish serotypes with lower invasiveness from those with higher invasiveness.
In conclusion, our study illustrates the value of generating carriage data in parallel with IPD surveillance data to help understand the serotype-specific changes in IPD observed in different epidemiological settings and predict the effect of higher valency vaccines. We provide evidence that the incremental benefit on IPD of the recent switch from PCV7 to PCV13 in the UK, while likely to be substantial, may be somewhat offset by increases in serotypes 8, 12F, and 22F. Such emerging serotypes with high CCRs are potential candidates for inclusion in future conjugate vaccines. More research to elucidate the serotype-specific capsular properties [2],[33] or other factors associated with carriage and invasiveness is needed in order to understand better the likely impact of future conjugate vaccines.
Supporting Information
Zdroje
1. BrueggemannABGriffithsDTMeatsEPetoTCrookDW
2003
Clonal relationships between invasive and carriage Streptococcus
pneumoniae and serotype- and clone-specific differences in invasive disease
potential.
J Infect Dis
187
1424
1432
2. WeinbergerDMTrzcinskiKLuY-JBogaertDBrandesA
2009
Pneumococcal capsular polysaccharide structure predicts serotype
prevalence.
PLoS Pathog
5
e1000476
doi:10.1371/journal.ppat.1000476
3. CalixJJNahmMH
2010
A new pneumococcal serotype, 11E, has a variably inactivated wcjE
gene.
J Infect Dis
202
29
38
4. BlackSShinefieldHFiremanBLewisERayP
2000
Efficacy, safety and immunogenicity of heptavalent pneumococcal
conjugate vaccine in children. Northern California Kaiser Permanente Vaccine
Study Center Group.
Pediatr Infect Dis J
19
187
195
5. DaganRMelamedRMuallemMPiglanskyLGreenbergD
1996
Reduction of nasopharyngeal carriage of pneumococci during the
second year of life by a heptavalent conjugate pneumococcal
vaccine.
J Infect Dis
174
1271
1278
6. DaganRGivon-LaviNZamirOSikuler-CohenMGuyL
2002
Reduction of nasopharyngeal carriage of Streptococcus pneumoniae
after administration of a 9-valent pneumococcal conjugate vaccine to
toddlers attending day care centers.
J Infect Dis
185
927
936
7. BeutelsPThiryNDammePV
2007
Convincing or confusing? Economic evaluations of childhood
pneumococcal conjugate vaccination–a review
(2002–2006).
Vaccine
25
1355
1367
8. MelegaroAChoiYHGeorgeREdmundsWJMillerE
2010
Dynamic models of pneumococcal carriage and the impact of the
Heptavalent Pneumococcal Conjugate Vaccine on invasive pneumococcal
disease.
BMC Infect Dis
10
90
9. PilishviliTLexauCFarleyMMHadlerJHarrisonLH
2010
Sustained reductions in invasive pneumococcal disease in the era
of conjugate vaccine.
J Infect Dis
201
32
41
10. WalsPDRobinEFortinEThibeaultROuakkiM
2008
Pneumonia after implementation of the pneumococcal conjugate
vaccine program in the province of Quebec, Canada.
Pediatr Infect Dis J
27
963
968
11. RodenburgGDGreeffSC deJansenAGCSMelkerHE deSchoulsLM
2010
Effects of pneumococcal conjugate vaccine 2 years after its
introduction, the Netherlands.
Emerg Infect Dis
16
816
823
12. WHO
2010
Changing epidemiology of pneumococcal serotypes after
introduction of conjugate vaccine: July 2010 report.
Weekly Epidemiological Record
85
434
436
13. HuangSSHinrichsenVLStevensonAERifas-ShimanSLKleinmanK
2009
Continued impact of pneumococcal conjugate vaccine on carriage in
young children.
Pediatrics
124
e1
11
14. VestrheimDFHøibyEAAabergeISCaugantDA
2010
Impact of a pneumococcal conjugate vaccination program on
carriage among children in Norway.
Clin Vaccine Immunol
17
325
334
15. PeltonSIHuotHFinkelsteinJABishopCJHsuKK
2007
Emergence of 19A as virulent and multidrug resistant Pneumococcus
in Massachusetts following universal immunization of infants with
pneumococcal conjugate vaccine.
Pediatr Infect Dis J
26
468
472
16. YildirimIHanageWPLipsitchMSheaKMStevensonA
2010
Serotype specific invasive capacity and persistent reduction in
invasive pneumococcal disease.
Vaccine
29
283
288
17. HussainMMelegaroAPebodyRGGeorgeREdmundsWJ
2005
A longitudinal household study of Streptococcus pneumoniae
nasopharyngeal carriage in a UK setting.
Epidemiol Infect
133
891
898
18. LundEHendrichsenJ
1978
Laboratory diagnosis, serology and epidemiology of Streptococcus
pneumoniae. Methods in microbiology
London
Academic Press
241
262
19. TrotterCLWaightPAndrewsNJSlackMEfstratiouA
2009
Epidemiology of invasive pneumococcal disease in the
pre-conjugate vaccine era: England and Wales,
1996–2006.
J Infect
60
200
208
20. SleemanKLGriffithsDShackleyFDiggleLGuptaS
2006
Capsular serotype-specific attack rates and duration of carriage
of Streptococcus pneumoniae in a population of children.
J Infect Dis
194
682
688
21. SimpsonEH
1949
Measurement of diversity.
Nature
163
688
22. HanageWPFinkelsteinJAHuangSSPeltonSIStevensonAE
2010
Evidence that pneumococcal serotype replacement in Massachusetts
following conjugate vaccination is now complete.
Epidemics
2
80
84
23. GilsEJM vanVeenhovenRHHakERodenburgGDBogaertD
2009
Effect of reduced-dose schedules with 7-valent pneumococcal
conjugate vaccine on nasopharyngeal pneumococcal carriage in children: a
randomized controlled trial.
JAMA
302
159
67
24. MillerEAndrewsNJWaightPASlackMPEGeorgeRC
2011
Herd immunity and serotype replacement four years after
pneumococcal conjugate vaccination in England and Wales: An observational
cohort study.
Lancet Infect Dis
In press
25. HPA
2010
Pneumococcal disease.
Available: http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Pneumococcal/.
Accessed 29 July 2010
26. SalisburyD
2010
Introduction of Prevenar 13 ® into the Childhood Immunisation
Programme.
Available: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_112192.pdf.
Accessed 4 June 2010
27. TurnerPHindsJTurnerCJankhotAGouldK
2011
Improved detection of nasopharyngeal co-colonization by multiple
pneumococcal serotypes using latex agglutination or molecular serotyping by
microarray.
J Clin Microbiol
doi:10.1128/JCM.00157-11
28. AbdullahiONyiroJLewaPSlackMScottJAG
2008
The descriptive epidemiology of Streptococcus pneumoniae and
Haemophilus influenzae nasopharyngeal carriage in children and adults in
Kilifi district, Kenya.
Pediatr Infect Dis J
27
59
64
29. HillPCTownendJAntonioMAkisanyaBEbrukeC
2010
Transmission of Streptococcus pneumoniae in rural Gambian
villages: a longitudinal study.
Clin Infect Dis
50
1468
1476
30. BruggerSDFreyPAebiSHindsJMuehlemannK
2010
Multiple colonization with S. pneumoniae before and after
introduction of the seven-valent conjugated pneumococcal polysaccharide
vaccine.
PLoS One
5
e11638
doi:10.1371/journal.pone.0011638
31. HarboeZBBenfieldTLValentiner-BranthPHjulerTLambertsenL
2010
Temporal trends in invasive pneumococcal disease and pneumococcal
serotypes over 7 decades.
Clin Infect Dis
50
329
337
32. GrayBMConverseGMDillonHC
1980
Epidemiologic studies of Streptococcus pneumoniae in infants:
acquisition, carriage, and infection during the first 24 months of
life.
J Infect Dis
142
923
933
33. WeinbergerDMHarboeZBSandersEAMNdirituMKlugmanKP
2010
Association of serotype with risk of death due to pneumococcal
pneumonia: a meta-analysis.
Clin Infect Dis
51
692
699
Štítky
Interní lékařstvíČlánek vyšel v časopise
PLOS Medicine
2011 Číslo 4
- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- MINISERIÁL: Když ženám stoupá tlak...
- Specifika v komunikaci s pacienty s ránou – laická doporučení
- Antikoagulační léčba u pacientů před operačními výkony
- Definice a klasifikace chronického onemocnění ledvin dle KDIGO
Nejčtenější v tomto čísle
- Global Health Philanthropy and Institutional Relationships: How Should Conflicts of Interest Be Addressed?
- A Call for Action: The Application of the International Health Regulations to the Global Threat of Antimicrobial Resistance
- Claims about the Misuse of Insecticide-Treated Mosquito Nets: Are These Evidence-Based?
- Medical Complicity in Torture at Guantánamo Bay: Evidence Is the First Step Toward Justice