-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
Authors: A. Zobanová
Published in the journal: Čes. a slov. Oftal., 73, 2017, No. 5-6, p. 225-230
Category: Doporučené postupy
Summary
Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
INTRODUCTION
Vision or visual perception is a complex function of the visual analyser on all of its levels, i.e. the eye, ocular pathway and brain's visual processing centres, including the association areas. Visual acuity is only one of several parameters of vision. Others are e.g. the visual field, colour perception, contrast sensitivity, adaptation to light and darkness and spatial vision. Even for an experienced ophthalmologist it is very difficult to answer one of the most frequently asked questions of parents of a small child: “How does our child actually see?”
In the Czech Republic, the co-ordinators of healthcare for children are paediatricians and general practitioners for children and adolescents. These people are therefore the first line of contact for identifying various sensory disorders, and thus also of sight. In 1994 a very high-quality Health and Vaccination Licence for Children and Youth was compiled by the Czech Paediatric Society, the Czech Neonatology Society, the Czech Social Paediatrics Society, the Czech Society of Adolescent Medicine, the Association of General Practitioners for Children and Adolescents and the National Institute of Public Health and published with the consent of the Ministry of Health of the Czech Republic. The time plan for preventive checks of sight by a paediatrician was based upon the standardized protocol of the decree on preventive checks for children and adolescents in the Czech Republic, at the following ages: 3 months – 6 months – 12 months, 18 months – 3 years and then periodically every 2 years up to the age of 17 years. This recommendation is binding and copies practically all critical periods of development in a child's vision. It is better than the majority of systems for monitoring sight in other countries, not only in Europe.
A further measure is the prevention and identification of critical values of refractive errors with the aid of a Plusoptix test. This is a screening method for identifying critical refractive errors in children in the risk period, i.e. at the age of 6 months to 3 years. The target is timely determination of significant refractive (dioptric) errors in the population, which could cause developmental disorders of vision in children. The tool serves only as a preventive test, and therefore in no case does it replace a detailed examination by an ophthalmologist.
The time when an eye examination for children in pre-verbal age (or verbally non-communicating patients) provided at maximum a description of the primary position of the eyes, fundamental disorders of their motility, the finding on the anterior segment of the eye and ocular fundus, or identified severe disorders of vision, is considered insufficient from today's perspective! It is far more important to determine the quality of visual acuity, to determine objectively the size of refraction, and to assess the capacity and strength of accommodation. If possible, we attempt to map disorders in the visual field of the child and determine the quality of contrast sensitivity. On the basis of this data we have the possibility of proposing a therapeutic and visual rehabilitation plan for the development of visual functions, sometimes long before the definitive determination of the ocular diagnosis.
I. General section
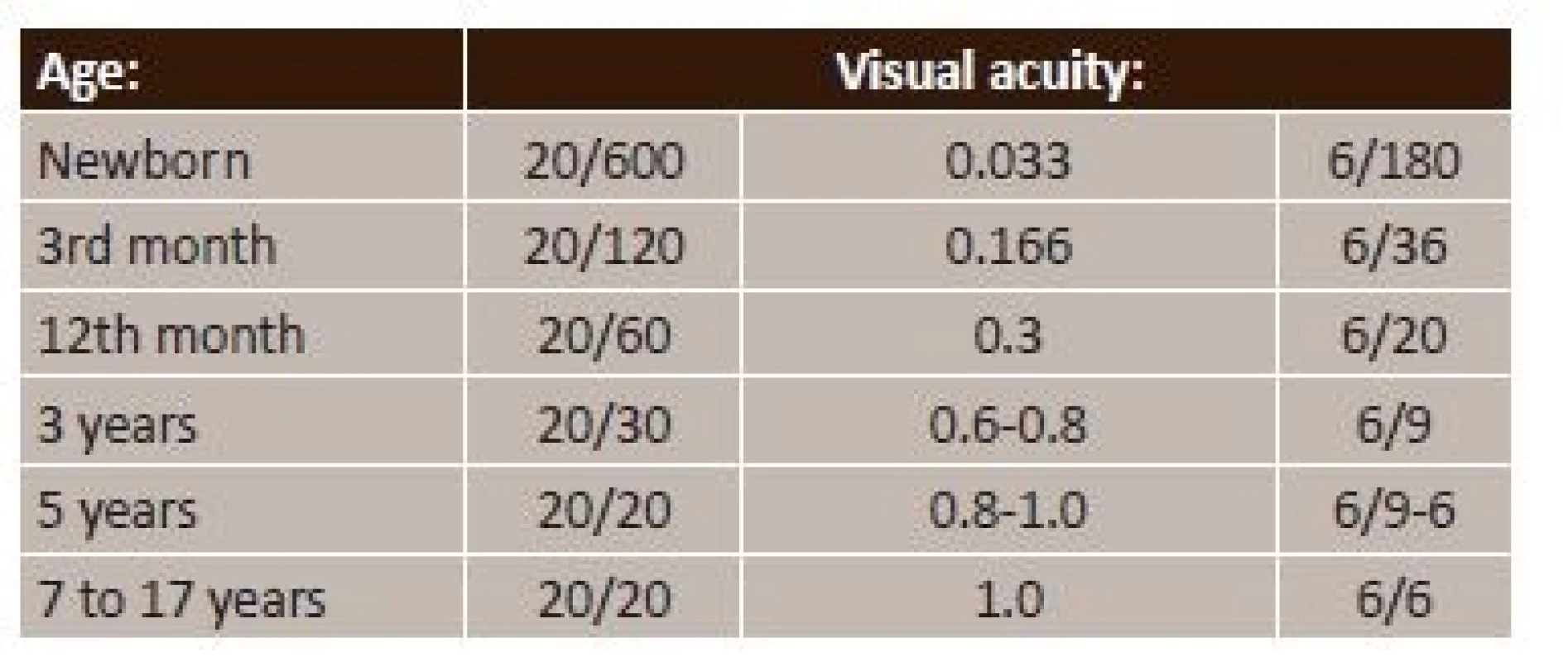
For the ophthalmologist to proceed correctly according to the above recommendation, it is necessary to know the physiological course of the development of vision (1, 2). Table 1 presents a brief summary of the essential periods.
Tab. 1. Physiological development of vision 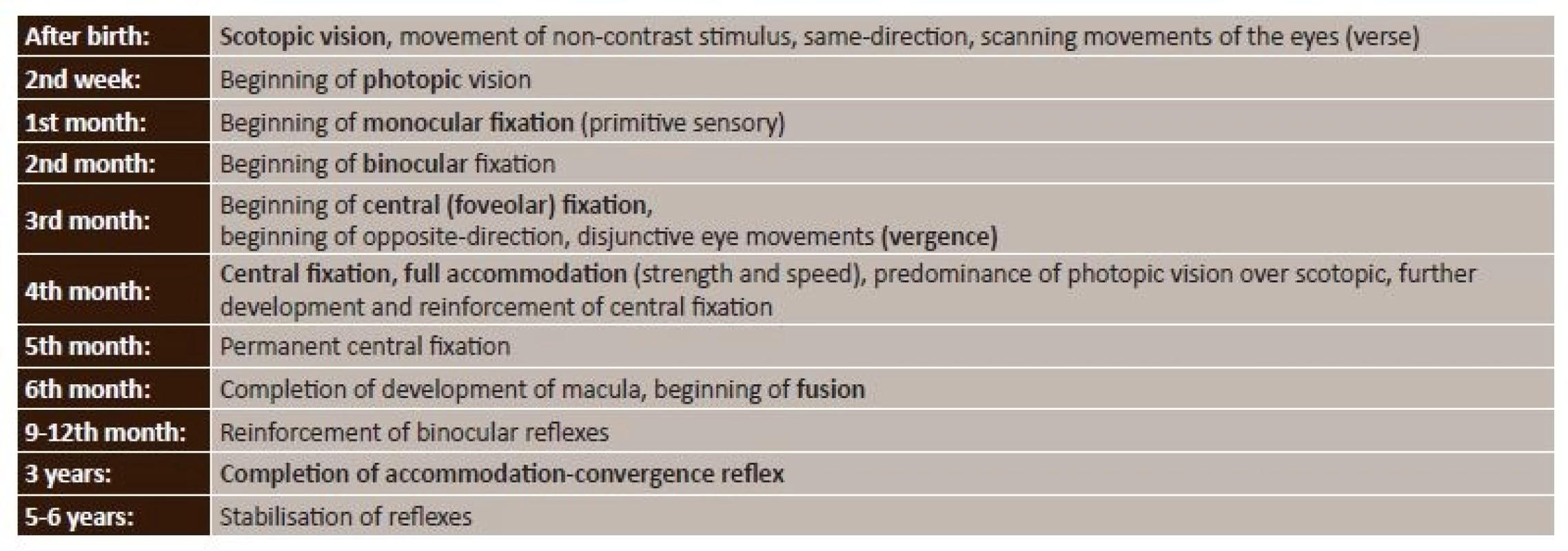
Newborn period (3, 4, 5)
A mature newborn has incomplete development of the eye as such. This relates primarily to the retina and accommodation muscle, also the newborn does not have a myelinated visual pathway, and the corresponding core visual centres are not appropriately differentiated.
On the retina the development of the area of most acute vision, i.e. the central macular landscape, is not complete. Although the macular landscape is differentiated, the cones that it contains exclusively in the future are not yet of the correct shape and arrangement. As a result, in the first days after birth peripheral vision predominates over central vision, i.e. scotopic over photopic. Scotopic vision is vision in twilight, it is mediated by rods and serves for the detection of moving, non-contrasting objects and changes in space. During this period the child cannot observe or fixate upon visual stimuli, not only due to the immaturity of the central landscape, but also because it lacks the association pathways between the ocular sensory and motor regions. The child responds to visual stimuli only by scanning space, i.e. by same-direction, conjugated, scanning movements of the eyes – verses. It further ensues from this that visual acuity in the first two weeks after birth cannot be better than the level of peripheral vision, thus 0.03, i.e. 2/60. Colour vision is also debatable in this period. We safely know that the child responds to black and white contrast, and also to red colour, about which it is known that it is the last colour that is distinguishable upon degenerative disorders of the retina.
Alignment of the function of the central and peripheral part of the retina takes place approximately within the 2nd week of life of the newborn. It is considered the beginning of photopic vision, i.e. vision in light of an immobile, highly contrasting object, and colour perception.
In the following two weeks, the central region begins to predominate functionally over the periphery, and as a result the beginning of the 1st month of life is considered the beginning of irregular, monocular fixation or primitive sensory fixation. The child uses each eye separately for fixation, fixates irregularly and convulsively, the gaze reflex is developed through stimulation of the central landscape.
Infant period (3, 4, 5)
From the 2nd month, sensory, passive, monocular fixation becomes active and short-term binocular fixation appears, i.e. the child uses both eyes simultaneously.
Between the 2nd and 3rd month of life, the connection of the primary visual centres with the cortical visual area mainly corresponding to the macular landscape is completed.
In the 3rd month, thanks to the full maturing of the most important part, i.e. the foveola, central fixation changes to irregular foveolar. At the same time, the child begins to set the angle of gaze of both eyes on the object, i.e. the beginning of opposite-direction, disjunctive movement of the eyes, i.e. vergence (close up convergence and divergent movement to distance).
In this period visual acuity changes very rapidly with the full maturing of the macula.
The fourth month is important for two reasons. A definitive predominance of the macular region over the periphery takes place, and furthermore the child is now capable of full accommodation. The basis of the accommodation convergence reflex originates, which is important not only for the development of binocular vision, but according to the latest observations also for the development of refraction, i.e. emmetropisation of the eye (meaning an eye without a fundamental dioptric defect).
In the 6th month the definitive development of the fovea and foveola is completed, and the fusion reflex begins to develop, i.e. the brain combines images of both eyes in one spatial perception.
In the following months the already formed binocular reflexes (fixation, accommodation convergence and fusion) are reinforced and perfected in connection with the child's touch reflexes and upright position.
Toddler period (3, 4, 5)
The interplay of accommodation and convergence is reinforced up to the age of 2 years. The development of all the reflexes is completed at the age of 3 years.
Pre-school period (3, 4, 5)
Up to the 6th year of age, the vision developed hitherto is stabilised, and acquires strength corresponding to unconditional reflexes.
School period (3, 4, 5)
During this period vision develops only little, and it is very difficult to maintain the existing level of vision of the afflicted eye through the rectification of neglected defects.
Visual acuity
Table 2 summarises the course of development of visual acuity as it changes in connection with the already described development of the individual parts of the eye, visual pathway and brain's visual processing centres (4, 5).
How to examine visual acuity in children
During the examination we have limited time, so as not to lose the child's attention. For this reason we always choose a test for the given age and the correct distance (pre-school age for 3 m max.). The other eye is always covered, on principle by a plaster eye patch (the child must have the possibility of movement during the examination).
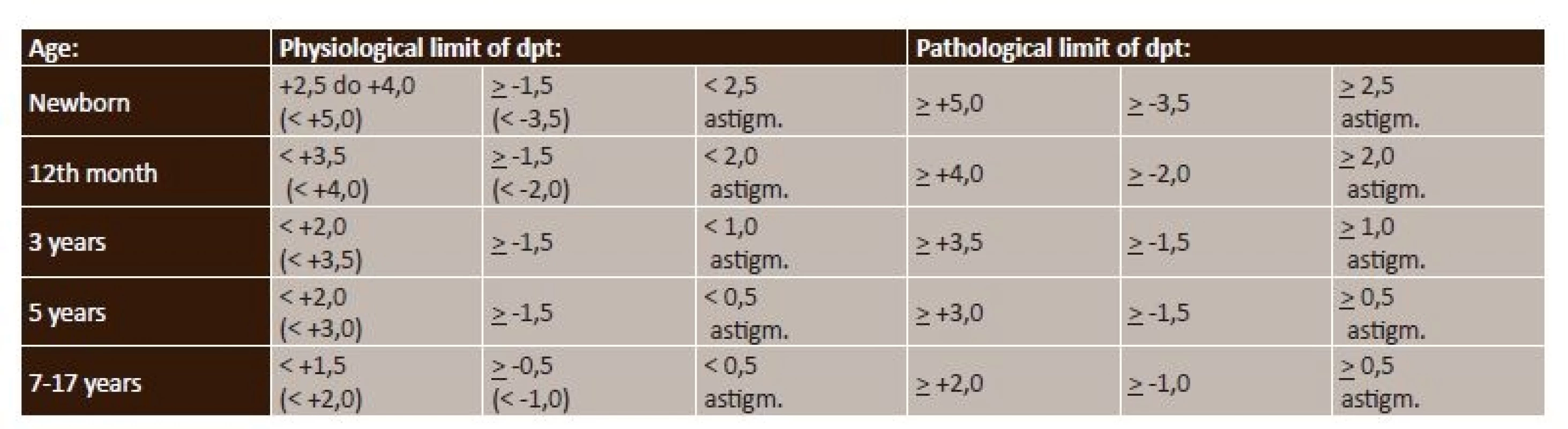
Refraction
The size of refraction, including the values considered critical for the occurrence of amblyopia, is presented in table 3.
II. Special section
When examining children it is important to ensure the preparedness of the environment (a small adjustment is sufficient, but must be planned in advance, i.e. to have some toys and above all a motivation box full of “children's goodies” in the surgery), staff (children notice body language and the tone we speak in) and knowledge (examination and procedure upon prescription of correction for children). Communication with parents leads to gaining the child's trust regardless of the parents' reaction, sets down the rules of the game, and a non-commercial approach is also important.
Anamnesis
Parents are the best observers of their child. If parents are of the opinion that something is not right with regard to sight and the eyes, listen to them and then ask: Who has the impression that your child is squinting? When did they notice squinting, nystagmus, inclination of the head...? Does the child make eye contact? Does he/she smile at visual stimuli? Does he/she behave differently from your expectations? Does he/she have nystagmus? Does he/she follow the light in a dark room? How does he/she react to strong light? Do the pupils react to illumination and also to objects offered close up?
There then follows our own observation upon the introductory meeting with the child: Can I induce optokinetic nystagmus? How easily does the child allow one eye to be covered? How quick and good is fixation after uncovering or after blinking? From what distance does the child focus on an offered object? How is the child's movement in space, how precisely does he/she reach for objects?
Examination schema (5, 10)
This has exact principles for children, similarly as with adult patients, but we attempt a contact-free approach from an appropriate distance and observe:
- Head position
- Face
- Position and configuration of eyes
- Cover test (CT) and alternate cover test (ACT)
- Convergent movement (CM)
- Motility
- Visual acuity
- Refraction naturally with the aid of autorefractometer (AR)
- Pupil reaction
- Examination of anterior segment of eye on slit lamp
- Examination of posterior segment of eye by indirect ophthalmoscopy
- Refraction in cycloplegia with the aid of autorefractometer (AR)
- Prescription of correction
- Instruction of parents
- * Examination of child by ophthalmologist in newborn age takes place according to the following schema:
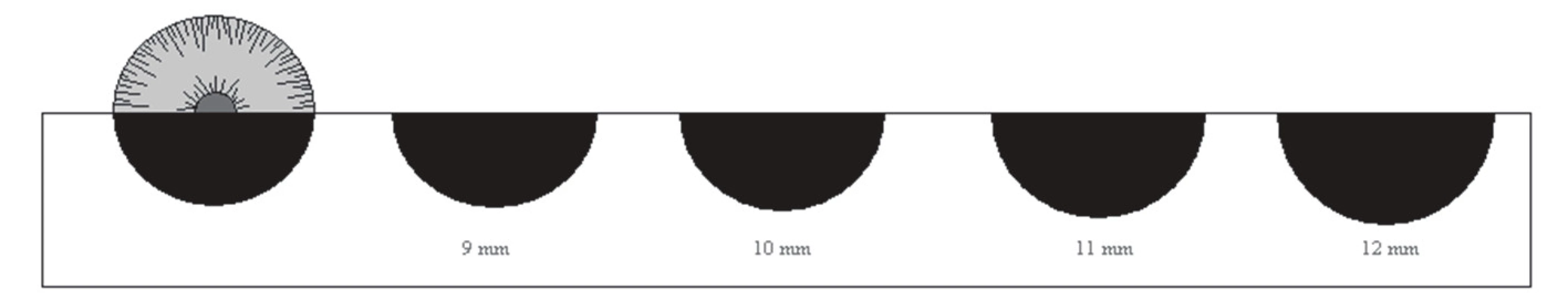
- Recommended examination aids – paper measure on which we draw black circles with a diameter of 8 mm, 9 mm, 10 mm, 11 mm, 12 mm..., and then cut them in half lengthwise and compare the halves with the size of the corneas (see fig. 1).
- Point pocket torch or direct ophthalmoscope, black and white chessboard with square size of 2 and 1.5 cm.
- We examine:
- Fundamental malformations of the eye – presence of both eyes, their size (cornea 10 mm), position (with regard to eye socket), configuration, i.e. basic convergence or divergence of one or both eyes according to reflexes on corneas and Bruckner test, in case of positive result whether the deviation is stable, nystagmus. Reaction to black and white chessboard – scanning (eyes identify stimulus, continue to search further and return again to place of original stimulus), macroscopically visible deviations of anterior segment of eye, reflex from ocular fundus (re-screening for congenital cataract), IOP, examination of ocular fundus best by indirect binocular ophthalmoscope.
- * Examination of child by ophthalmologist at age of 3 and 6 months takes place according to the following schema:
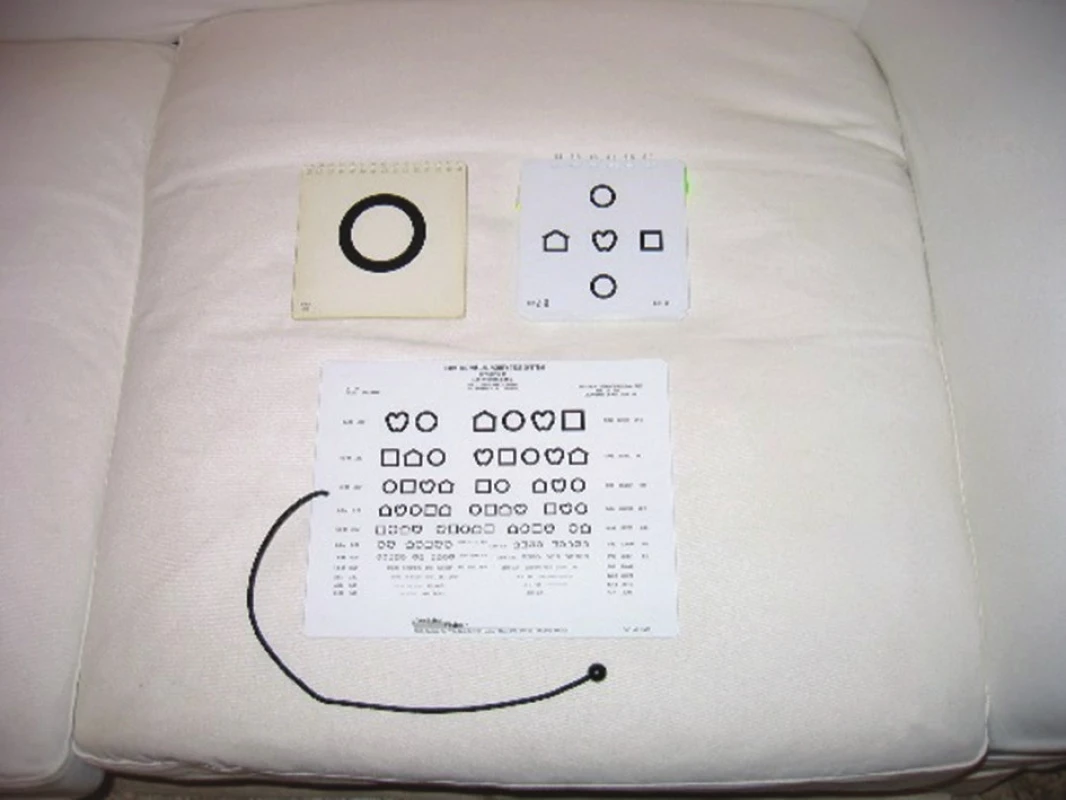
- Recommended examination aids see above and schematic face with a diameter of minimum 5 cm from a distance of 38 cm from the child's face.
- (see fig. 2)
- We examine:
- Position and movement of both eyes – convergence or divergence, nystagmus yes or no!!! or, if applicable, other abnormal eye movements.
- Monocular fixation and following of movement of chessboard pattern or schematic face. Examination of anterior segment of eye, reflex from ocular fundus (re-screening for congenital cataract), examination of ocular fundus best by indirect binocular ophthalmoscope.
- * Examination of child by ophthalmologist at age of 12 and 18 months takes place according to the following schema:
- Recommended examination aids – see above and black and white chessboard with a size of squares of 0.8 cm from a distance of 55 cm from the child's face (size of squares based on width of strips used in examination of visual acuity with the aid of preferential looking), plaster occlusor, schematic face (see fig. 2).
- We examine:
- Light fixation, following of immobile object with high contrast (black and white chessboard) monocularly and binocularly, following of mobile non-contrasting object = visual field. Symmetry of verses and vergences of both eyes (face), macroscopic examination of face and eyelids. Examination of anterior segment of eye, reflex from ocular fundus, examination of ocular fundus best by indirect binocular ophthalmoscope, add examination of refraction!!!
- * Examination of child by ophthalmologist at age of 3 and 5 years takes place according to the following schema:
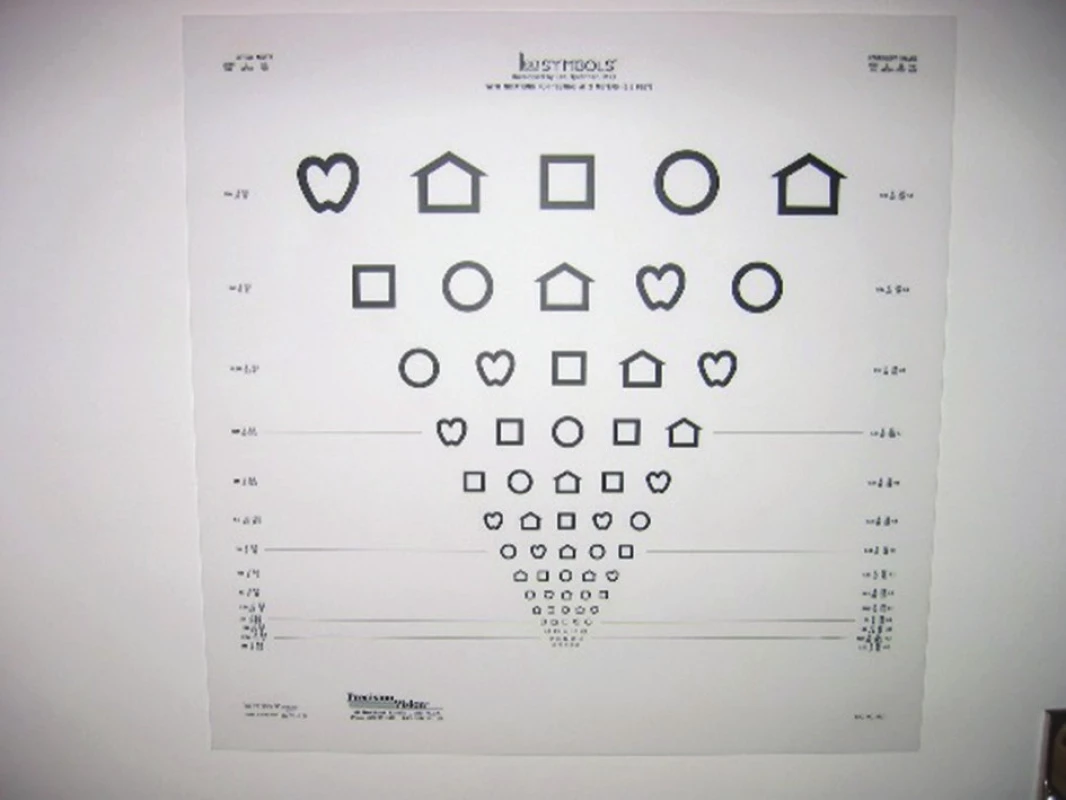
- Recommended examination aids see above and plaster occlusor!!!, optotypes (individual and row optotypes of images and E at 3 m see fig. 3). Upon child's refusal to co-operate educational interview with parents is required, concerning the need for occlusion of the eye upon determining visual acuity and training of copied images or E symbols used in your practice, and making a further additional appointment for examination of visual acuity.
- We examine:
- Symmetry of verses and vergences of both eyes, stereopsis with the aid of Lang test, visual acuity in verbally co-operating children – distinguishing visual acuity (row optotypes of images and E to 3m). Colour perception. Macroscopic examination of face and eyelids. Examination of anterior segment of eye, reflex from ocular fundus, examination of ocular fundus best by indirect binocular ophthalmoscope. Examination of vision and refraction, setting of correction.
- * Examination of child by ophthalmologist at age of 7 to 17 years takes place according to the following schema:
- Recommended examination aids see above, plaster occlusor, optotypes (row optotypes letters or numbers and E at 5 or 6 m), colour perception tables, otherwise as for adult patient.
- We examine:
- Symmetry of verses and vergences of both eyes, stereopsis with the aid of Lang test, visual acuity in verbally co-operating children – distinguishing visual acuity (row optotypes of images and E to 3m). Colour perception. Macroscopic examination of face and eyelids. Biomicroscopic examination of anterior segment of eye, examination of ocular fundus on slit lamp or indirect binocular ophthalmoscope.
What correction we prescribe
The setting of accurate correction is the condition for a precise assessment of other disorders, e.g. configuration, binocularity etc. The difference between a prescription of glasses by a doctor and an optometrist consists in the fact that an ophthalmologist prescribes glasses on the basis of an evaluation of all the available examination methods, and at the same time has the possibility of taking into account any further determined health problems. We measure children, as we do adult individuals, naturally and then in cycloplegia (the comparison of values also provides us with information about accommodation). Do not confuse mydriasis – tropicamide, phenylephrine and cycloplegia – cyclopentolate, atropine, homatropine, scopolamine. We measure refraction skiascopically or by autorefractor, on principle it is not possible to prescribe glasses according to Plusoptix.
Upon prescribing correction we begin with the logical consideration of the reason why we are prescribing correction, what kind of refractive error we are faced with (myopia, hypermetropia, astigmatism), and take into account the patient's age. A question remains as to whether to test the child subjectively for correction or not. We attempt this once the child reaches school age and for adult patients, if we wish to make a large change as against the original correction, or if we are fundamentally altering the axes of cylinders. We then determine the dominant eye (if possible), have the patient read naturally, we test with what the patient reads best with using the dominant eye and after cycloplegia, we respect the patient's choice in the dominant eye (myopia lowest, hypermetropia highest, astigmatism full – we respect the axis chosen by the patient). We prescribe full correction always including the full value of astigmatism in myopia, strabismus, amblyopia.
Upon prescribing correction for children we take into consideration:
A – improvement of visual acuity (child has no other complaints)
B – prevention of occurrence of strabismus and amblyopia
C – for therapeutic reasons (in the case of strabismus, amblyopia and disorders of accommodation)
We then continue as follows:
- In the case of hypermetropia ½ or 2/3 of measured value in cycloplegia for correction of visual acuity and the child has no other complaints, if we are in the critical band of refraction.
- In the case of hypermetropia ½ or 2/3 of measured value in cycloplegia even if we are not in the critical band, if the patient is from a group of risk children.
- Compare lateral difference. Always full value of cylinder.
Glasses for distance or near vision for persons younger than 42 years do not exist. Only constant, all-day wearing of glasses for all distances, as well as in the case of contact lenses or if we performed a refractive surgical procedure.
Accommodation (9)
Accommodation for distance is a state of relaxation of the accommodation muscle, and for near this is an active process. Normal accommodation, i.e. the ability to focus from distance to near, is connected to a change in pupil width. Assessment of pupil reactions is part of a complete neurological and also ophthalmological examination. Through a comparison of the quality of the pupil response with objective measurement of accommodation obtained with the aid of dynamic retinoscopy, a direct dependency between both examinations was determined. Patients with a delayed, reduced or lacking pupil response have a significantly worse level of accommodation. Brain damage generally has a significant impact on the capacity for accommodation, both on its speed and its strength. A child with an inability to accommodate cannot make eye to eye contact, cannot fixate upon the face of the mother, and the gaze bypasses offered toys. The child often gives an impression of autism or central blindness.
We compensate for insufficient or lacking accommodation with a prescription for addition (at least +2.5 or +3.0 D) for full correction of refraction, measured in cycloplegia, i.e. in the form of bifocal or multifocal glasses or hypercorrection, i.e. only by prescription of glasses with a value of D for near vision. The setting of correction brings about a passive sharpening of the impression reaching the macula. Intensive passive sensory stimulation of the macula may then lead to a renewal of the development of the accommodation convergence reflex.
III. Interpretation of abnormal findings
Methods of examining sight by an ophthalmologist are constantly being developed, and are usable always from a certain month of age.
- A newborn must be examined by an ophthalmologist in the case of any congenital deficiency or severe deviation of the eye and its surrounding areas, including the eyelids and lachrymal ducts. Upon a larger as well as smaller diameter of corneas, accompanied by photophobia and lachrymation we suspect increased intraocular pressure.
- We look for nystagmus at the latest within the 2nd-3rd month of life. Its presence after the 2nd month of age attests rather to a neurological problem than to rare congenital nystagmus. Nystagmus which appears in or after the 2nd month of age generally has its basis in a severe ocular defect. Every nystagmus which does not have typical characteristics of congenital nystagmus (horizontal, symmetrical) requires further multi-disciplinary examination.
- We test fixation using a black and white contrast pattern, and from the 4th month, if possible, separately in each eye. In the case of a child who repeatedly resists coverage of one eye we must determine the cause of reduced vision.
- It is also necessary to monitor disorders of motility and symmetry of configuration of the eyes practically from the 4th month of age of the child, at the latest at the age of 6 months.
- Practically from the 6th month it makes sense to measure refraction, but this is possible from the moment of birth. A positive family anamnesis of blunt vision or large refractive error is the reason for measuring refraction at the latest within the 8th to 12th month of life, at least for a screening test with the aid of a Plusoptix instrument.
- We test visual acuity after prior training of co-operation. We always use a plaster occlusor to cover the other eye.
- We insist on all-day wearing of glasses.
CONCLUSION
It is evident that the most critical period for the development of vision is the first year of the child's life, especially the first half thereof. During this period the child is entirely in the hands of the paediatrician, upon whom it solely depends to consult an ophthalmologist in time in the case of any unclear disorder of visual functions. The ophthalmologist must assess the current clinical finding and decide upon a further examination and/or therapeutic procedure, or to send the child to a specialised centre. The time we lose in the 1st year of the child's life due to late or inaccurate determination of the diagnosis and non-functional therapeutic plan is critical and irreplaceable for the development of vision!!! It is not possible to satisfy ourselves with the answer that the child cannot be examined due to his/her age or inability to communicate.
It is necessary to know that by determining the size of the refractive error and the level of visual acuity we can commence therapy e.g. of blunt sightedness or squinting in a timely manner, which essentially means glasses and if applicable correct occlusion therapy and orthoptics (8). This conservative therapy as a preparation before any applicable surgical solution or for training is unsubstitutable, and this applies also to the youngest children, non-communicating children or weak sighted children with vision on the boundary of severe weak sightedness (7, 9).
MUDr. Anna Zobanová
Soukromá oční ordinace
Krškova 807
152 00 Praha 5, Barrandov
e mail: zobanova.anna@volny.cz
Zdroje
1. Divišová, G.: Strabismus, Avicenum Praha, 1979; 44–67.
2. Hyvarinen, L.: Vision in children normal and abnormal, Meaford, Ontario, 1988; 1–9, 11–16, 21–22.
3. Buckley, E. G.: Pediatric neuro-ophthalmology examination, Pediatric Ophthalmology and Strabismus, Wright K.W. and Spiegel P.H., Springer-Verlag New York, Inc., 2003; 865–875.
4. Stout, U.: Pediatric eye examination, Pediatric Ophtalmology and Strabismus, Wright K.W. and Spiegel, P.H., Springer-Verlag New York, Inc., 2003; 57–67.
5. Zobanova, A.: Respektování fysiologického vývoje zraku v preventivních prohlídkách dětí a dorostu, Vox pediatrie 2004; 9, 20–21.
6. Repka, M. X.: Refraction in infants and children, Pediatric Ophthalmology, Nelson L. B., Calhou J. H,. Harley R.d., Eds. W,B, Sauneders Company, 1991; 94–106.
7. Jacobson, L., Ek, U., Fernell, E. et al.: Visual impairment in preterm children with periventricular leukomalac – visual, cognitive and neuropaediatric characteristics related to cerebral imaging, Developmental Medicine and Child Neurology, 199; 38, 724–735.
8. Modlingerova, E., Zobanova, A.: Základní ortoptické vyšetření prováděné ortoptistou, Oftalmologie pro praxi, 2017; 15–17.
9. Zobanova, A.: Dětská mozková obrna z pohledu oftalmologa, Neurologie pro praxi, 2011; 12(4), 234–238.
Štítky
Oftalmologie
Článek Autorský rejstřík
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2017 Číslo 5-6- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Léčba chronické blefaritidy vyžaduje dlouhodobou péči
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Konjunktivitida a původce Corynebacterium macginleyi – kazuistika
-
Všechny články tohoto čísla
- OCT nálezy a dlouhodobé výsledky vitrektomie u jamky terče s makulopatií
- Perzistující arteria hyaloidea – indikovat k operaci či nikoli?
- Kombinovaná intravitreálna aplikácia kortikosteroidov a anti-vegf u pacientov s edémom makuly po uzávere žily sietnice
- Jubileum doc. MUDr. Šárky Pitrové, CSc., FEBO
- Sarkoidóza a její oční manifestace (rozbor šesti kazuistik)
- Výsledky léčby diabetické retinopatie laserovým systémem pascal
- Liečba melanómu corpus ciliare stereotaktickou rádiochirurgiou
- Výsledky liečby pacientov s lymfómovým ochorením v oblasti očnice
- Rozdíl mezi „Ganglion cells complex“ a vrstvou nervových vláken ve stejné altitudinální polovině sítnice u hypertenzních a normotenzních glaukomů
- Xeróza u pacientky s deficiencí vitaminu A
- Doporučený postup očního vyšetření u nejmenších dětí a dětí předškolního věku v běžné ambulantní praxi
- Autorský rejstřík
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Sarkoidóza a její oční manifestace (rozbor šesti kazuistik)
- Doporučený postup očního vyšetření u nejmenších dětí a dětí předškolního věku v běžné ambulantní praxi
- Perzistující arteria hyaloidea – indikovat k operaci či nikoli?
- Výsledky liečby pacientov s lymfómovým ochorením v oblasti očnice
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání