-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Developmental morphology of the elbow joint in relation to injuries of the paediatric skeleton
Authors: Martin Čepelík; Tomáš Pešl; Petr Havránek
Authors place of work: Klinika dětské chirurgie a traumatologie 3. LF UK, Thomayerova nemocnice, Praha – Krč
Published in the journal: Úraz chir. 26., 2018, č.1
Summary
Introduction:
The elbow joint is considered the most complicated region regarding fracture diagnostics in paediatric skeletal traumatology. It comprises of 6-10 secondary ossification centres, which appear at different ages. This article summarizes the knowledge regarding the development of ossification around the elbow joint and its relationship to diagnostics of paediatric skeletal trauma, with a focus on the most frequent pitfalls of the evaluation of radiographs of the elbow joint in paediatric patients.
Methods:
Review of literature with addition of the authors’ own experience.
Conclusion:
Plain X-rays are often sufficient in the diagnostics of paediatric elbow trauma; however, precise and correct evaluation requires a perfect knowledge of the ossification process of epi - and apophyses, as well as broad experience with paediatric elbow X-rays at individual age categories.
Keywords:
Elbow joint – growth plate – growing skeleton – secondary ossification centre – epiphysis
Introduction
The elbow joint belongs among the most complex diagnostic areas within paediatric skeletal traumatology. This is mostly due to the number of secondary ossification centres, their variability and means of ossification. At the same time, it is the third most frequently injured area of the paediatric skeleton (following fractures of fingers and the distal forearm) [4]. A perfect knowledge of the developmental morphology of the elbow joint and experiences with analysis of radiographic images of the growing skeleton are the basic precondition for a correct assessment of elbow joint injuries in children, and determination of a correct therapeutic procedure. The aim of this article is to summarize the knowledge concerning ossification of the elbow joint in relation to the diagnostics in paediatric traumatology, with a special emphasis on the most frequent problems encountered by physicians assessing the radiographic images of the elbow joint in children.
Ossification of the elbow joint
Articular bone ends forming the elbow joint consist of the total of six secondary ossification centres, or ossification nidi – capitilum of the humerus (capitulum humeri), trochlea, ulnar and radial epicondyle, head of the radius and the olecranon (Fig. 1a-b).
Fig. 1. a-b: Overview of ossification nidi of the elbow joint, boy, 13 years of age. C – capitulum humeri, R – caput radii, I – epicondylus medialis, T – trochlea humeri, O – olecranon, E – epicondylus lateralis 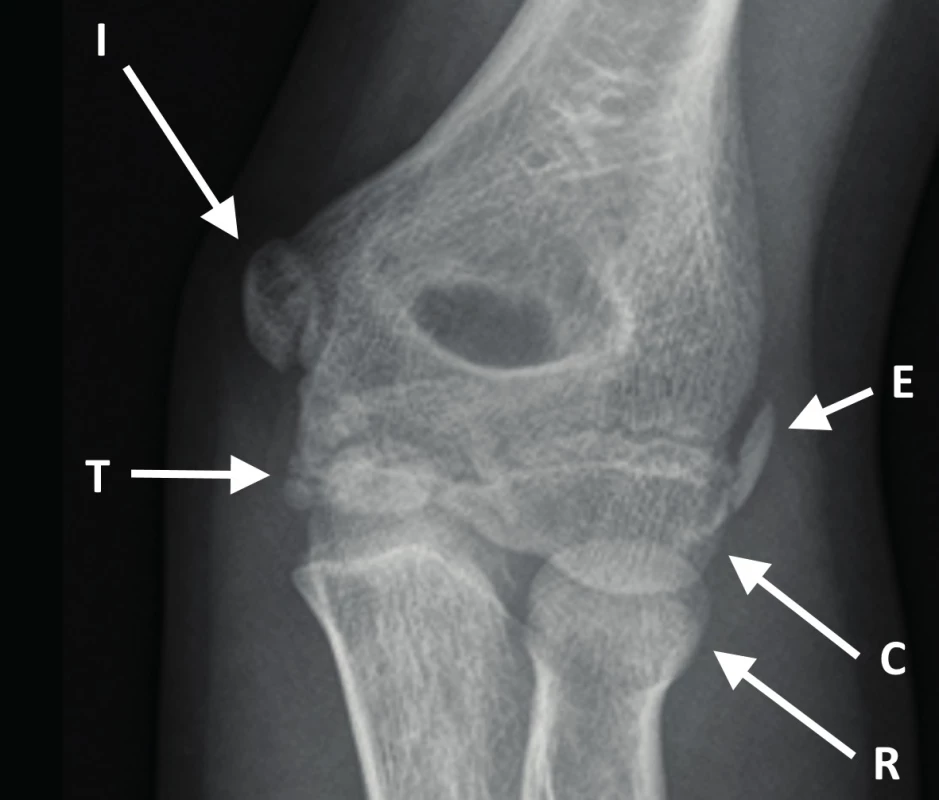
The individual centres are frequently divided into several parts, that is why it is also possible to find a description of 6-10 ossification nidi of the elbow joint, which need to be differentiated from a traumatic lesion (Fig. 2).
Fig. 2. Divided nidus of the olecranon, boy, 13 years of age 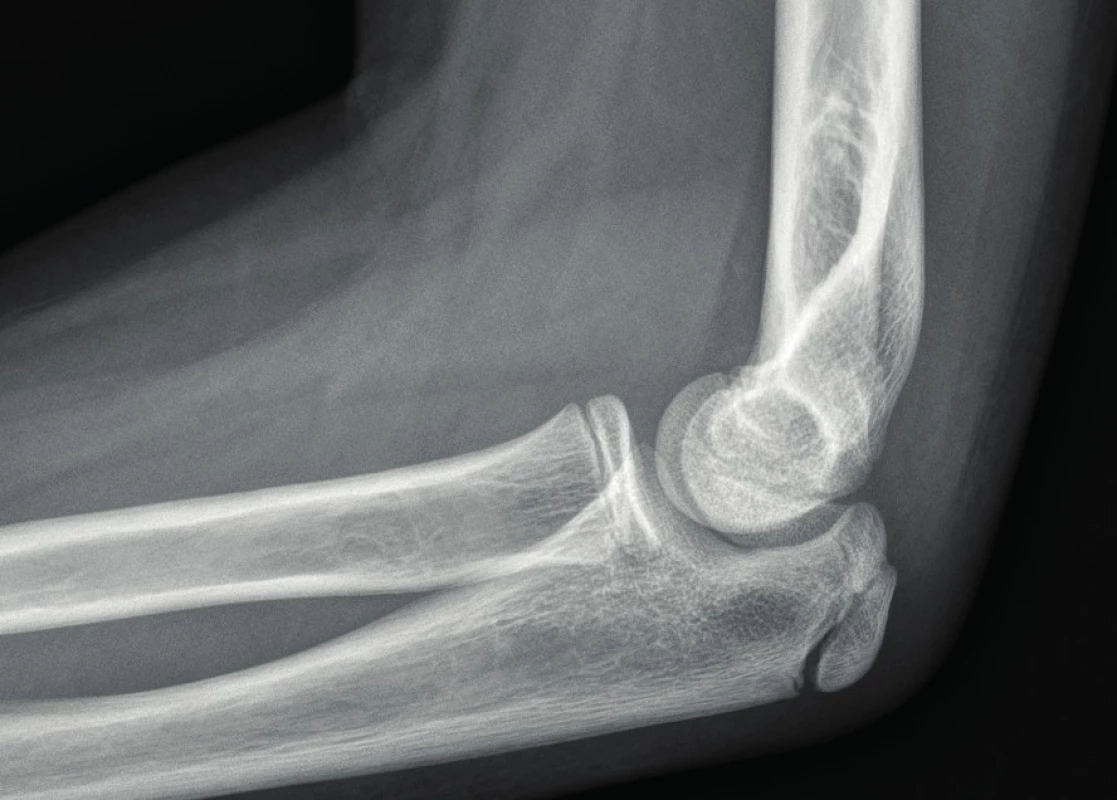
The process of ossification of individual nidi begins already in the first year of life, when the nidus of capitulum humeri becomes manifested, and the process further continues in the following sequence: radial head “ ulnar epicondyle “ trochlea “ olecranon “ radial epicondyle. Fusion of secondary ossification centres with the metaphysis and closure of growth cartilages occurs between the 13th and 18th year of age. In girls, the manifestation and fusion of nidi occur approximately 1-2 years earlier (with the exception of capitulum humeri) [5, 7, 8, 9, 10, 11] (Tab. 1 and Fig. 3a-e).
Tab. 1. Overview of manifestation and fusion times of ossification nidi at the elbow joint (according to Ogden) 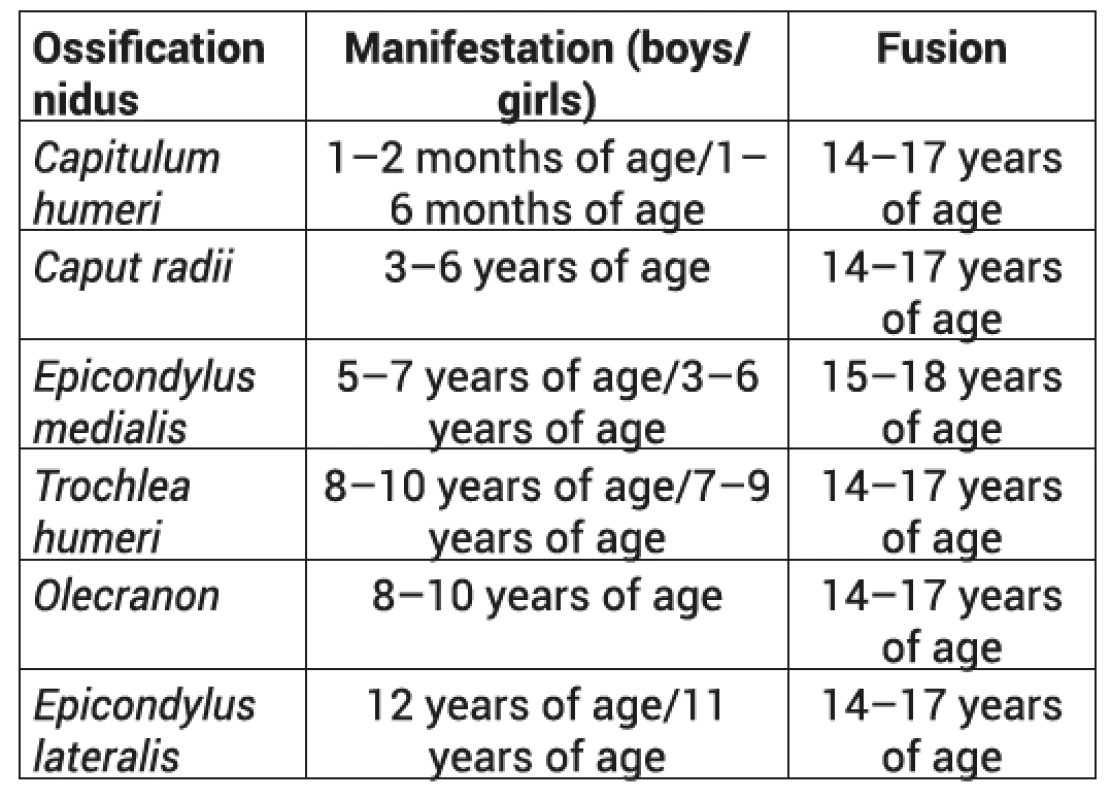
Fig. 3. a-e: Gradual development of ossification of the elbow joint. a - 3 years of age, b - 6 years of age, c - 8 years of age, d - 11 years of age, e - 14 years of age 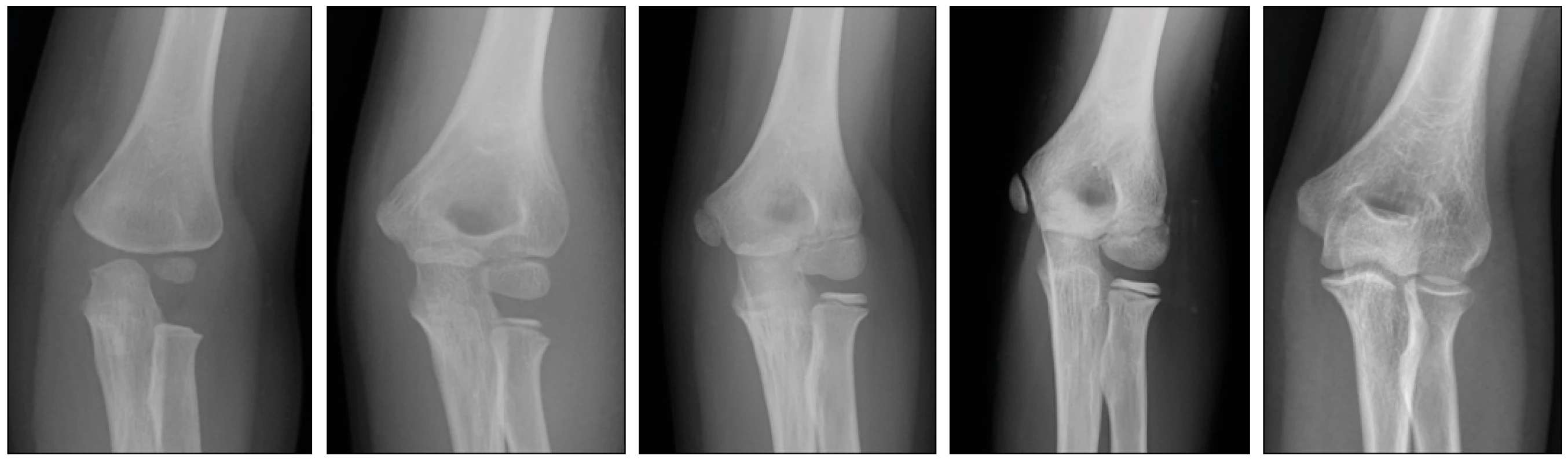
When assessing an injury of the elbow joint in children, it is also necessary to consider the fact that a large part of the epi - and apophysis is still cartilaginous, and their image on radiography presents only a part of their true size. Also, the ossification occurs eccentrically, especially at the capitulum humeri, when the nidus becomes manifested proximally, ventrally and medially from the middle of the cartilaginous part [2], which may make the diagnostics more difficult, particularly in assessing the humeroradial joint [3, 13, 16]. The problems of of the ossification of capitulum humeri and its influence upon inaccurate assessment of radiographic images of the growing elbow is most significant in children younger than five years of age.
Diagnostic possibilities
A plain radiograph taken in two planes – anteroposterior and lateral – remains the basic diagnostic modality for assessment of injuries of the paediatric skeleton. For a correct assessment of the radiograph, it is crucial to perform the imaging precisely in these projections; taking the image in incorrectly set projections may result in false positive and false negative findings, or an incorrect assessment of the degree of displacement in a diagnosed fracture [15]. For obtaining a radiograph of the elbow joint in the lateral projection, it is most suitable to perform the lateral projection using a horizontal ray, without a rotation of the extremity. In cases of confusing findings or inability to achieve images of the required quality (e.g. due to pain associated with manipulation with the extremity in cases of displaced fractures), it is possible to perform the desired manipulation under X-ray (in sedation or general anaesthesia of the patient), while obtaining static or dynamic images. Another possibility is to obtain a comparative image of the contralateral healthy extremity, which will reveal the state of ossification of individual nidi in cases of uncertainty, whether the finding is a traumatic lesion or physiological condition of not yet fully ossified skeleton.
The popularity of CT in the diagnostics of injuries of the adult skeleton increases, and this trend is projected to paediatric traumatology as well. However, for the assessment of injuries of the elbow joint in children (and the paediatric skeleton in general), CT examination will only seldom offer a better lead within the basic diagnostic-therapeutic process when compared with a plain radiograph. What is more, CT examination cannot display cartilaginous parts of the growing skeleton, and cannot offer a solution when in doubts regarding the correct diagnosis. Despite the relatively low radiation load of CT examination of the elbow joint (0.14 mSv, which corresponds to approximately two weeks of irradiation from natural sources), it still presents a hundred times higher dose when compared with a plain radiograph (0.001 mSv, corresponding to approx. 3 hours of irradiation from natural sources) [1, 12], and as such should be reserved for clear indications of certain intra-articular fractures and specific cases only (namely post-traumatic conditions and very specific acute injuries, e.g. free radioopaque body inside the joint).
When compared with CT, magnetic resonance imaging (MRI) is not ideal for assessment of a skeletal injury, however, it may provide a detailed overview of cartilaginous parts of the not yet fully ossified skeleton and soft tissues. At the same time, MRI is considered to be a safe and radiation-free technique. The persisting problem lies in the lack of availability of this examination and its length, requiring the patient to remain perfectly still. That is why MRI examinations in children younger than 6 years of age are routinely performed under general anaesthesia, and even in case of older patients, the examination is sometimes impossible without sedation. Considering the fact that the age of about 5 years is the most critical for assessment of the growing elbow joint, MRI remains an imaging modality, which is only rarely used in the clinical practice for assessment of elbow injuries in children.
Ultrasonography examination (USG) gains popularity in cases of diagnostic uncertainty in paediatric traumatology. This examination offers a rapid, available and radiation-free technique for the patient, and enables us to assess the condition of the cartilaginous parts of ossification nidi, which are not visible on radiography; very frequently, it is also possible to distinguish between a fresh and an older lesion. The main limitation of this technique is the relatively low experience of physicians with using USG for the purpose of skeletal traumatology.
Supracondylar fractures of the distal humerus
In order to be able to determine a correct therapeutic procedure in patients with supracondylar fractures of the distal humerus, assessment of antecurvature of the capitulum humeri (distal epiphysis – diaphyseal-condylar angle) is crucial; this angle should reach 25-40° [4]. The assessment is performed in the sagittal plane, when the line leading through the frontal edge of the humerus (anterior humeral line) should pass through the middle of the capitulum humeri. The basic precondition for this assessment is a precise lateral projection of the elbow joint. Incorrectly projected image may lead to false positive or false negative findings [15].
Ossification of the capitulum humeri occurs already during the first six months of life. Due to the gradual and eccentric ossification of the capitulum humeri [3], the anterior humeral line may become shifted towards the middle of the ossified nidus of the capitulum humeri, ventrally and dorsally [6, 14]; nevertheless, the anterior humeral line should at least touch the capitulum humeri at all times. This problem is most prominent in patients younger than five years of age, and may be responsible for an incorrect assessment of antecurvature of the capitulum humeri, and thus the degree of its displacement in cases of supracondylar fractures.
Injury of the ulnar epicondyle of the distal humerus
Ossification of the ulnar epicondyle begins between the fifth and seventh year of life (in girls, this may be up to two years earlier), and its fusion with the distal metaphysis occurs between 15 and 18 years of age (as the last of the ossification nidi in the elbow joint). In both these time periods, the ossifying ulnar epicondyle presents a risk of false positive assessment of the radiographic image, when the ossification nidus may seem too distant from the metaphysis at first, and the disappearing cartilage may imitate a fracture line in the period of beginning fusion, which is often potentiated by the fact that the patient has reached an age when the radiograph is being assessed by an adult trauma surgeon. In cases of possible doubts, a comparative image of the contralateral healthy elbow joint may be advantageous, as it very often confirms or rejects the suspicion of epicondyle avulsion.
Another diagnostic problem may be an avulsion of the ulnar epicondyle of the 3rd degree, when an epicondylar fragment is wedged into the joint, and is projected into the area of humeral trochlea, and may thus create the impression of a false negative findings, which results in overlooking the serious injury. For the assessment of this type of injury it is important to realize that the ulnar epicondyle always ossifies earlier than the humeral trochlea, and its fusion occurs later than in the fusion of the trochlea [7, 9]. That is why the physician, not seeing an absence of the ossification nidus of the ulnar epicondyle on the radiograph, and seeing the ossification nidus of the trochlea, should always consider a possible avulsion of the ulnar epicondyle, an its possible summation inside the elbow joint. Similarly, in cases when the physician suspects already accomplished epicondylar fusion but still does see the growth cartilage of the trochlea, he should actively search for a possible avulsion with wedging of the epicondyle into the joint, where it aligns with the image of the trochlea.
Injury of the radial part of the condyle of the distal humerus and avulsion of the radial epicondyle
The ossification of the radial epicondyle of the humerus begins as the last one from the nidi of the elbow joint, most frequently around the eleventh year of life (up to two years earlier in girls), and its fusion usually begins within two years from its manifestation [7, 9, 11]. Thus, it is individually apparent for a very limited period of life only, and a physician, who does not perform routine assessment of radiographs of the paediatric skeleton, encounters the image of its manifestation only exceptionally, which may often lead to false positive findings regarding the fractures of the radial part of the humeral condyle or the rare avulsion of the radial epicondyle. Fusion of the radial epicondyle occurs from the distal end proximally, which often strengthens the impression of a fracture line in this area (Fig. 4). Also in these cases of ambiguous findings, a comparative radiograph of the healthy contralateral extremity may be beneficial.
Fig. 4. Beginning fusion of the ossified radial epicondyle taking place from the distal end proximally, boy, 13 years of age 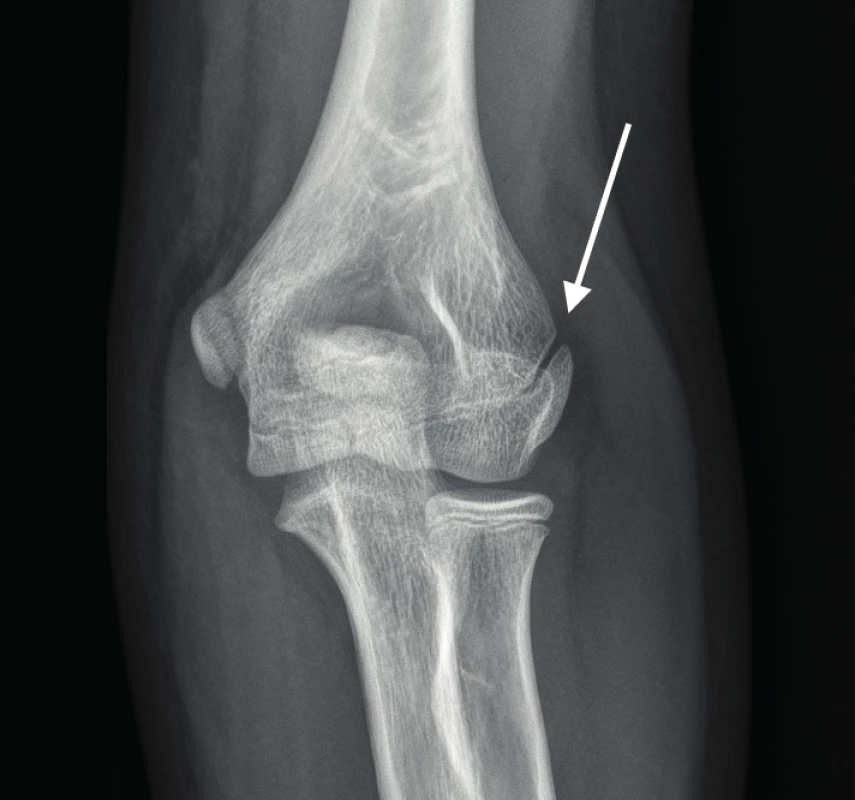
Monteggia lesion of the growing skeleton
Monteggia lesion is a relatively rare injury, which is defined as an ulnar fracture at any level, associated with a lesion (dislocation) of the humeroradial joint. Seriousness of this injury lies predominantly in its difficult diagnostics, when the physician, upon finding an ulnar fracture, does not search further for a possible injury of the humeroradial joint. That is why an individual image of the elbow joint should be obtained in patients with a finding of a solitary ulnar fracture, and the physicians should actively look for a Monteggia lesion [4].
A rule applies with the assessment of humeroradial articulation that the radial axis (line running through the neck, or diaphysis of the radius) should be positioned in the centre of the capitulum humeri in healthy elbow joints in all projections. Due to the eccentric ventro-medio-proximal ossification of the capitulum humeri, and the eccentric (radial) ossification of the radial head, the radiograph obtained in younger children (critical period below five years of age) very often makes it seem that this line crosses the capitulum humeri eccentrically, or completely misses it, especially in the anteroposterior projection (Fig. 5) [2, 13].
Fig. 5. Healthy elbow joint with a false positive image of humeroradial dislocation, boy, 3 years of age 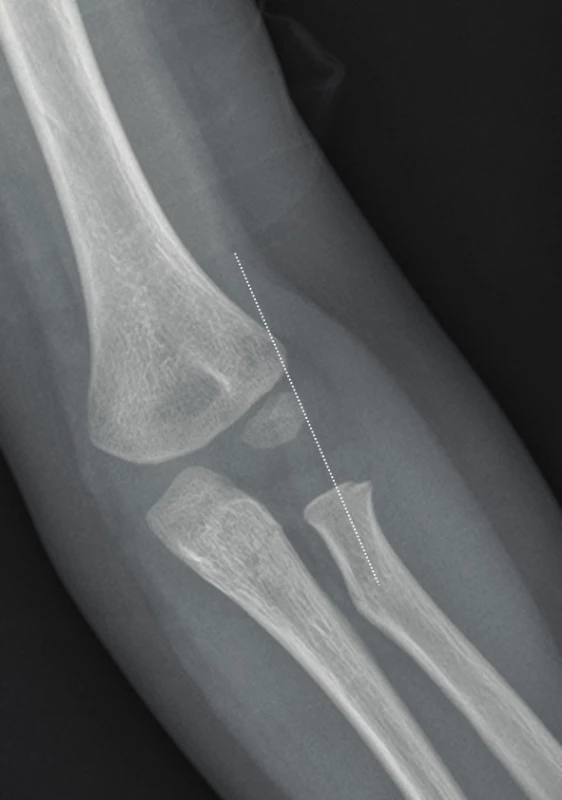
A lateral humeral line has been proposed in order to make the diagnostics more precise, crossing the most lateral point of the visible skeleton in a precise anteroposterior projection, parallel to the axis of the humerus. This line should, in cases of healthy elbow joints, pass around the radial neck area from the lateral side (Fig. 6) [16]. In cases of persisting doubts, it is necessary to obtain a radiograph under general anaesthesia, and safely assess the congruence and stability of the humeroradial joint.
Fig. 6. Healthy elbow joint, lateral humeral line miss the radial neck from the lateral side, boy, 3 years of age 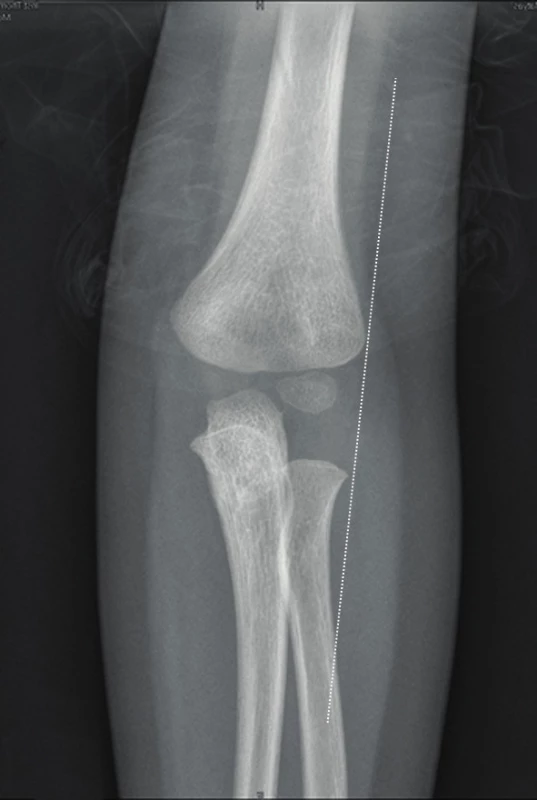
Conclusion
Injuries of the elbow joint in children belong among frequently observed injuries, and present a diverse group of possible skeletal lesions. Their assessment belongs among the most difficult diagnostic tasks for a paediatric traumatology surgeon. For the basic diagnostics of elbow injuries, plain radiographs are usually sufficient, however, in order to be able to assess them correctly, the physicians must have a detailed knowledge of ossification of individual nidi of epi - and apophyses, its sequence and course, use of auxiliary evaluation criteria and especially experience with assessing radiographic images of the growing elbow in individual age categories.
MUDr. Martin Čepelík
Zdroje
- BISWAS, D., BIBLE, JE., BOHAN, M. et al. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009, 91, 1882–1889. ISSN 0021-9355
- FADER, LM., LAOR, T., EISMANN, EA. et al. J. Eccentric Capitellar Ossification Limits the Utility of the Radiocapitellar Line in Young Children. J Pediatr Orthop. 2016 36, 161–166. ISSN 0271-6798
- FADER, LM., LAOR, T., EISMANN, EA. et al. MR imaging of capitellar ossification: a study in children of different ages. Pediatr Radiol. 2014, 44, 963–970. ISSN 0301-0449
- HAVRÁNEK, P. et al. Dětské zlomeniny. 2. vyd. Praha : Galén, 2013. 389 s. ISBN 978-80-7262-983-1
- HAVRÁNEK, P., PEŠL, T., ČEPELÍK, M. Klasifikace dětských zlomenin. Praha : Galén, 2014. 63 s. ISBN 978-80-7492-143-8
- HERMAN, MJ., BOARDMAN, MJ., HOOVER, JR. et al. Relationship of the anterior humeral line to the capitellar ossific nucleus: variability with age. J Bone Joint Surg Am. 2009, 91, 2188–2193. ISSN 0021-9355
- CHENG, JC., WING-MAN, K., SHEN, WY. et al. A new look at the sequential development of elbow-ossification centers in children. J Pediatr Orthop. 1998, 18, 161–167. ISSN 0271-6798
- KIM, HH., GAUGUET, JM. Pediatric Elbow Injuries. Semin Ultrasound CT MR. 2018, 39, 384–396. ISSN 0887-2171
- MIYAZAKI, CS., MARANHO, DA., AGNOLLITTO, PM. et al. Study of Secondary Ossification Centers of the Elbow in the Brazilian Population. Acta Ortop Bras. 2017, 25, 279–282. ISSN 1413-7852
- OGDEN, JA. Skeletal Injury in the Child. New York : Springer, 2000. 1198 s. ISBN 0-387-98510-7
- PATEL, B., REED, M., PATEL, S. Gender-specific pattern differences of the ossification centers in the pediatric elbow. Pediatr Radiol. 2009, 39, 226–231. ISSN 0301-0449
- Radiation Dose in X-Ray and CT Exams. Radiology.org [online]. Oak Brook (Illinois): RSNA, 2018, 20 Apr 2018 [cit. 2018-09-08]. Dostupné z: https://www.radiologyinfo.org/en/pdf/safety-xray.pdf
- RAMIREZ, RN., RYAN, DD., WILLIAMS, J. et al. A line drawn along the radial shaft misses the capitellum in 16% of radiographs of normal elbows. J Pediatr Orthop. 2014, 34, 763–767. ISSN 0271-6798
- RYAN, DD., LIGHTDALE-MIRIC, NR., JOINER, ER. et al. Variability of the Anterior Humeral Line in Normal Pediatric Elbows. J Pediatr Orthop. 2016, 36, 14–16. ISSN 0271-6798
- SKIBO, L., REED, MH. A criterion for a true lateral radiograph of the elbow in children. Can Assoc Radiol J. 1994, 45, 287–291. ISSN 0846-5371
- SOUDER, CD., ROOCROFT, JH., EDMONDS, EW. Significance of the Lateral Humeral Line for Evaluating Radiocapitellar Alignment in Children. J Pediatr Orthop. 2017, 37, 150–155. ISSN 0271-6798
Štítky
Chirurgie všeobecná Traumatologie Urgentní medicína
Článek vyšel v časopiseÚrazová chirurgie
Nejčtenější tento týden
2018 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Stillova choroba: vzácné a závažné systémové onemocnění
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Cinitaprid – v Česku nová účinná látka nejen pro léčbu dysmotilitní dyspepsie
Nejčtenější v tomto čísle- Operační léčba zlomenin diafýzy pažní kosti
- Vývojová morfologie loketního kloubu ve vztahu k poranění dětského skeletu
- Poúrazová peritonitida
- Artroskopicky asistovaná osteosyntéza triplane zlomeniny - kazuistika
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




