-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaEvaluation of medium-term outcomes of surgical treatment of talus neck fractures at the Department of Trauma Surgery, University Hospital Brno
Authors: Radim Ulman; Milan Krtička; Daniel Ira
Authors place of work: Klinika úrazové chirurgie, Fakultní nemocnice Brno
Published in the journal: Úraz chir. 25., 2017, č.4
Summary
Purpose of the study:
Retrospective evaluation of medium-term outcomes of surgical treatment in patients witha fracture of the talus neck treated at the Department of Trauma Surgery, University Hospital Brno between 2008 and 2014.
Material and methods:
The observed group consisted of 15 patients, 10 men (66.7 %), and 5 women (33.3 %). The average age of patients was 38 years (19–66 years). All dislocated talus neck fractures were indicated for surgical treatment, together with most undislocated fractures. The selected treatment of choice was osteosynthesis, with two cannulated screws inserted in parallel to each other, either with assisted arthroscopy, mini-invasively, or by open reduction. Regular clinical controls were performed in all patients after surgery, after 1, 3, and 6 months, and furthermore 24 months from the surgery. In order to assess the outcomes, the AOFAS score (American Orthopaedic Foot and Ankle score) was used.
Results:
The average period of hospitalization among the observed patient population was 9 days. The period from the injury to definite surgical management varied between one and ten days, with 4.7 days on average.
A total of 33.3 % of patients sustained type-I fracture classified according to Hawkins, 53.3 % of patients sustained type-II fracture, and 13.3 % of patients were treated with type-III fractures. The most frequently used surgical approach was anteromedial approach (33.3 %). According to the American Orthopaedic Foot and Ankle score, excellent outcome was observed in 20 % of our patients, good outcome in 26.7%, satisfactory outcome in 20 %, and poor outcome in 33.3 % of patients.
The average total AOFAS score was 72.5, and varied between 38 and 97 points. No difference was observed in the average AOFAS score between the group of patients treated within two days from the injury and the patients who underwent a delayed definite treatment. Signs of I-II degree arthritis were observed after 24-month follow-up period in 26.7 % of patients, avascular necrosis was diagnosed in 6.7 % of patients.
Discussion:
The most common mechanism of injury in talus neck fractures is indirect and high-energy. It affects mostly the young and active part of population. When diagnosing talus fractures, we began with anamnestic data, and continued with physical examination, X-ray and CT examination. The surgical procedure may be performed at the acute stage, as a definite treatment, or in stages, as a delayed procedure. Both dislocated and undislocated talus neck fractures are indicated for surgical management, due to earlier postoperative mobilization and prevention of complications associated with long-term fixation of fractures. Osteonecrosis represents a very serious complication, closely related to the anatomical structure of talus vascular supply. Another less serious, however rather frequent complication, is the development of post-injury arthritis.
Conclusions:
alus fractures belong among very serious fractures, considering the frequent occurrence of postoperative complications, which are closely associated with the anatomical structure of the talus, vulnerable vascular supply, and high-energy requirements imposed upon the talus. The most effective means of elimination of these complications is an emergency reduction in every dislocated, luxation or open fracture. From the outcomes obtained among our patient population it becomes apparent that talus neck fractures may be treated primarily at one time, or in stages, as a delayed procedure. However, even the best possible timing and planning of surgical management of these fractures does not completely eliminate complications associated with this type of injury.
Keywords:
Talus neck fracture, osteosynthesis, treatment results.
INTRODUCTION
The talus, given its structure, is adapted for significant mechanical load – with the talus neck being the least resistant. No muscle is attached to the talus, 3/5 of the talus surface are covered with cartilage, which forms a total of five articulation surfaces, which significantly reduce the possibility of vessels to enter into the bone, which makes the vascular supply of the talus more vulnerable [1, 5, 15].
Talus fractures are relatively rare. They account for approximately 0.85 or 1.0 % of all fractures, for approximately 2 % of all injuries of lower extremities, and for about 5–7 % of foot injuries. The mechanism of injury is most frequently indirect [3,19]. Talus neck fractures are responsible for about 50 % of all talus fractures [12, 17]. They are often associated with high-energy mechanisms of injury – falls from heights, car and motorcycle accidents, predominantly in the young, active and mobile part of population [3, 16, 19]. The fact that high-energy mechanism of injury is directly related to talus fractures is also reflected in the fact that already in the course of WWI, this type of injury was described by Anderson as “aviator’s astragalus”, when the pedal of the rudder pushed the pilot’s foot into dorsiflexion [3, 6, 12, 15]. Low-energy mechanism of injury may be applied namely in fractures of talus processes and protuberances – e.g. on snowboard. Approximately 15–20 % of talus fractures are open fractures, related to a compound injury. These fractures are characterized by trauma of surrounding soft tissues, including the vascular supply of the talus, dislocation, and often comminuted character of the fractures [3]. The fractures are mostly caused by flexion-extension mechanism of injury. Forcible supination and adduction movements result in luxation. The weakest part of this extremely solid bone is the neck [19]. Fractures with a more serious dislocation or luxation are associated with a greater risk of avascular necrosis. That is why emergency reduction of luxation talus fractures is required [12, 19].
MATERIAL AND METHODS
Patient file
A total of 54 patients with talus fractures were treated at the Department of Trauma Surgery, University Hospital Brno, between 1st September 2008 and 31st December 2014. Patients with undislocated peripheral talus fractures treated conservatively (n=19), furthermore patients undergoing surgery due to peripheral talus fractures (n=5), and patients with open luxation talus neck fractures treated with Kirschner wires and external fixation (n=4) were excluded. Retrospective analysis was performed in 15 patients with talus neck fractures, treated with osteosynthesis using the lag screw technique.
Assessed parameters
In our patient population, the following parameters were evaluated retrospectively: age, sex, cause of injury, classified type of fracture, associated injuries, length of hospital stay, time from injury to definite surgical treatment, type of surgery and surgical approach, and the AOFAS Ankle-Hindfood score (American Orthopaedic Foot and Ankle score) [8]; for more details please see below. Furthermore, radiographs were assessed, together with signs of arthritis and the range of ankle movement in dorsal and plantar flexion, inversion and eversion, and the quality of achieved reduction. The presence of AVN was assessed 6 months from the injury, based upon radiographic examination (AP and lateral projection of the ankle). In cases when AVN was suspected, a native MRI scan was obtained.
Assessment according to AOFAS (American Orthopaedic Foot and Ankle score)
The AOFAS score represents a questionnaire consisting of nine questions, providing results in the range of 0–100 points, where three areas are being assessed: pain (40 points), function (50 points), and position of the foot (10 points). The sum of all points between 90–100 points is considered to be an excellent outcome, 80–90 points means good, 70–80 points mean satisfactory, and a result below 70 points means poor outcome [8].
Imaging techniques
All patients were initially examined with ankle radiographs in anteroposterior, lateral and Drašnar’s projections (Fig. 1 a, b, c), and radiographs of the foot in anteroposterior, oblique and lateral projections (Fig. 2 a, b, c). During the postoperative period, X-ray control examinations were performed in order to monitor the treatment results, in the following intervals: 5th–7th postoperative day, and subsequently 1, 3, 6, 12 and 24 months from the surgery. In all patients with talus fractures confirmed on radiography, a native CT examination of the injured site was performed (Fig. 3 a, b). In most cases, also 3D CT reconstruction was used (Fig. 4).
Fig. 1. a, b, c: Ankle radiograph – AP, Drašnar’s and lateral projection 
Fig. 2. a, b, c: Foot radiograph – AP, oblique and lateral projection 
Fig. 3. a, b: CT examination of talus neck fracture – sagittal and coronary slices 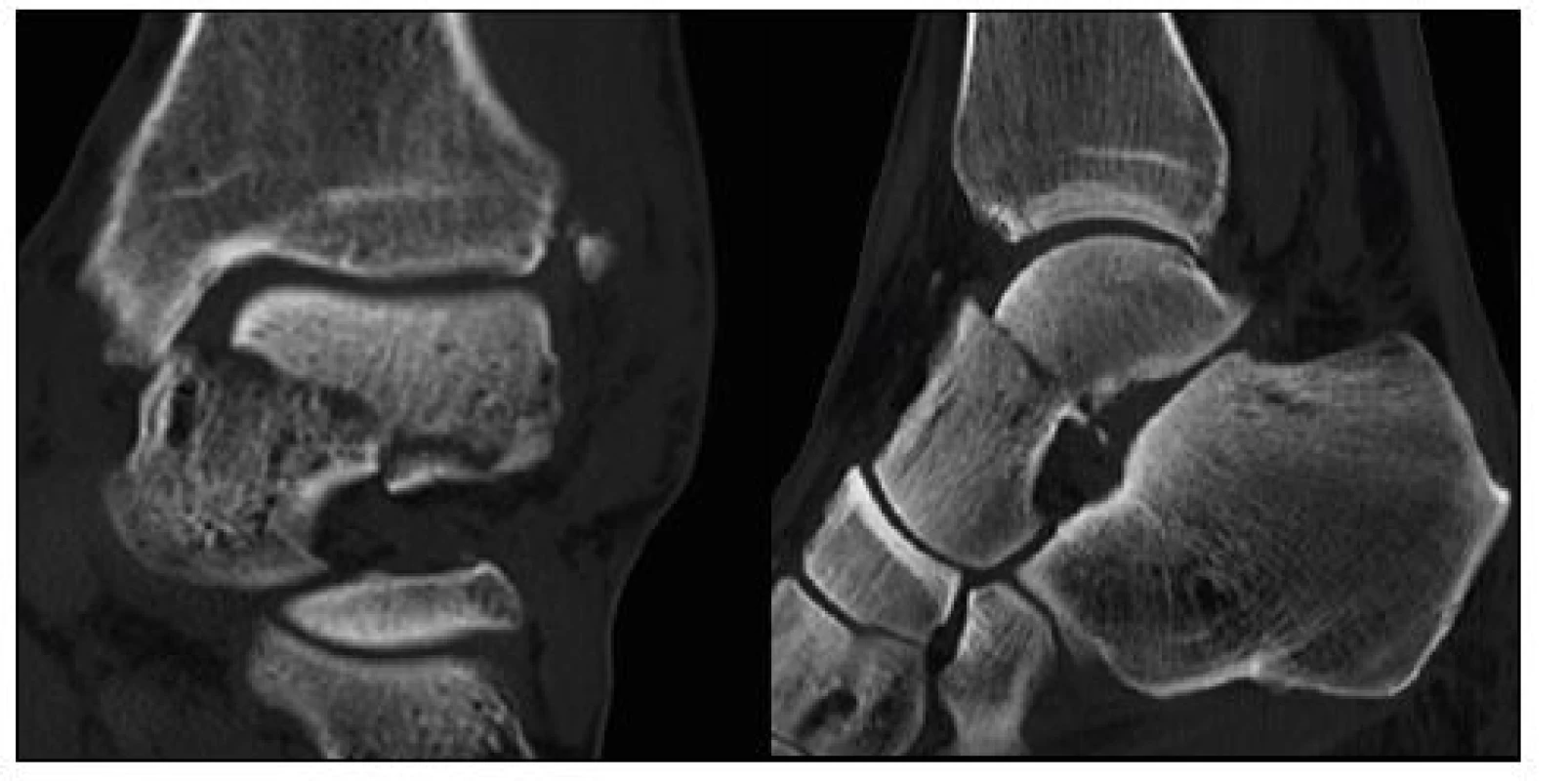
Fracture classification
In order to classify the talus neck fractures, Hawkins-Canale classification was used; this classification was first introduced in 1970 by Hawkins with regard to vascular supply of the talus and subsequent risks of posttraumatic avascular necrosis [7].Canale and Kely extended the classification already in 1978, by adding Type IV talus neck fractures [4].
Indication, timing, surgical approach and techniques
Luxation and dislocated talus neck fractures were reduced upon admission, at the outpatient clinic or at the emergency room, and were fixed with a plaster splint. In cases when achieving reduction at the outpatient clinic was not possible, it was performed at the operating theatre, with application of an external fixator, in order to minimize the damage of the vascular supply to the talus, and to decrease the associated degree and seriousness of subsequent talus osteonecrosis.
Fig. 4. Three-dimensional CT reconstruction of the ankle 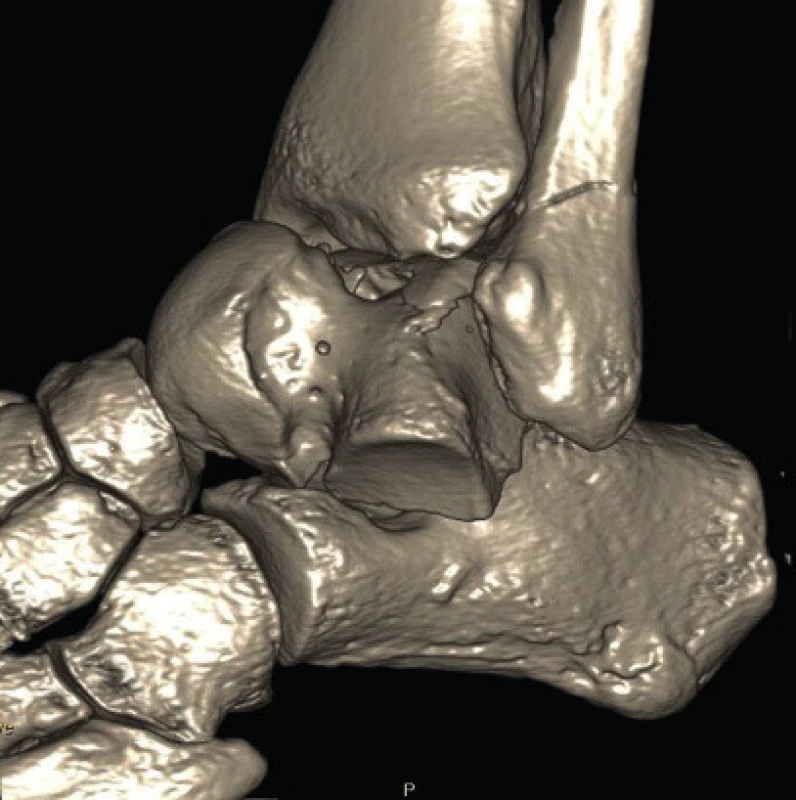
Arthroscopy-assisted osteosynthesis was indicated in cases of undislocated or minimally dislocated talus neck fractures. Anterior and posterolateral approach to the ankle was used during arthroscopy procedures; visualisation of cartilages and ligaments was achieved after washing out coagula and minor bone fragments. Anatomic reduction was performed under X-ray control from anterolateral incision, with subsequent temporary fixation of fragments using Kirschner wires; two cannulated screws with the diameter of 4.0 mm (B-Braun Konigsee) were inserted under skiascopic and arthroscopic control from the dorsal part of the talus, perpendicularly to the fracture line.
Minimally invasive osteosynthesis was indicated also in undislocated or minimally dislocated fractures, in which closed reduction under skiascopic control was achieved. Reduction under X-ray control was performed from small incisions located anteromedially and anterolaterally. After anatomical reduction, two 1.8 mm Kirschner wires were inserted first, followed by insertion of two cannulated screws with the diameter of 4.0 mm (B-Braun Konigsee) – Fig. 5 a, b.
In patients with dislocated fractures, in whom closed reduction was not possible, it was necessary to perform an open reduction from anteromedial or combined approach (anteromedial and anterolateral). Debridement was performed first, followed by washing out coagula and small bone fragments. Anatomical reduction was achieved under X-ray control. Subsequently, a temporary transfixation with 1.8 mm Kirschner wires under X-ray control was performed, followed by insertion of two cannulated screws, perpendicularly to the fracture line. In fractures with a comminuted zone, plaster fixation was applied for the period of 2–3 weeks. The aim of surgical treatment of talus fractures (also undislocated) is to perform an absolutely stable osteosynthesis using lag screws, in order to achieve primary bone healing, even with the poor vascular supply to the talus.
Fig. 5. a, b: Postoperative radiographs of the ankle following osteosynthesis with cannulated screws (4.0 mm) 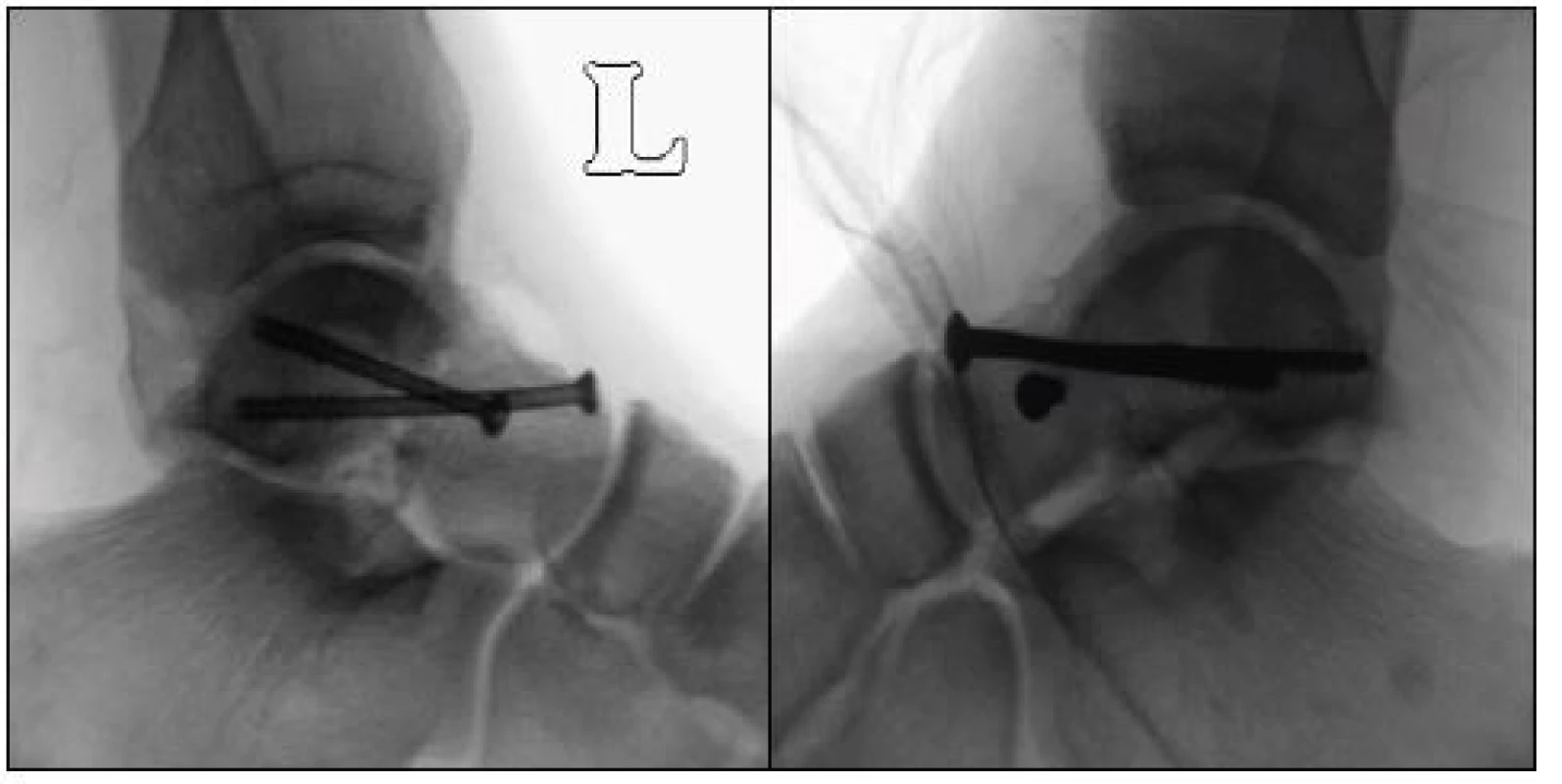
Postoperative care
Cefazolin was used as a standard antibiotic prophylaxis (Ciprofloxacin was used in patients with known penicillin allergy), in a standard dosing according to the patient’s body weight. In patients with a prolonged surgery procedure lasting more than two hours, administration of antibiotics was extended to three doses after eight hours. In patients with contusion of soft tissues, antibiotic therapy was maintained for the period of one week. Prevention of thromboembolic disease was realized with low-molecular weight heparins (LMWH). Postoperative physiotherapy was initiated early after the acute pains have diminished, with subsequent parallel analgetization, primarily using passive dorsal and plantar flexion. A great emphasis was put on early verticalization of the patient, using crutches or a walker, with an accompanying person and without any loading of the extremity, according to the patient’s abilities. Gradual loading was allowed after 6 weeks, full weight bearing was achieved after 3–4 months in most cases, based upon continuous X-ray controls, which were performed on the 5th–7th postoperative day, after 4 weeks, and 3, 6, 12 and 24 months. In uncooperative patients, plaster fixation is recommended for the period of three months.
RESULTS
The observed patient file consisted of 15 patients, 10 men (66.7 %) and 5 women (33.3 %).
The average age was 38 years (19–66 years).
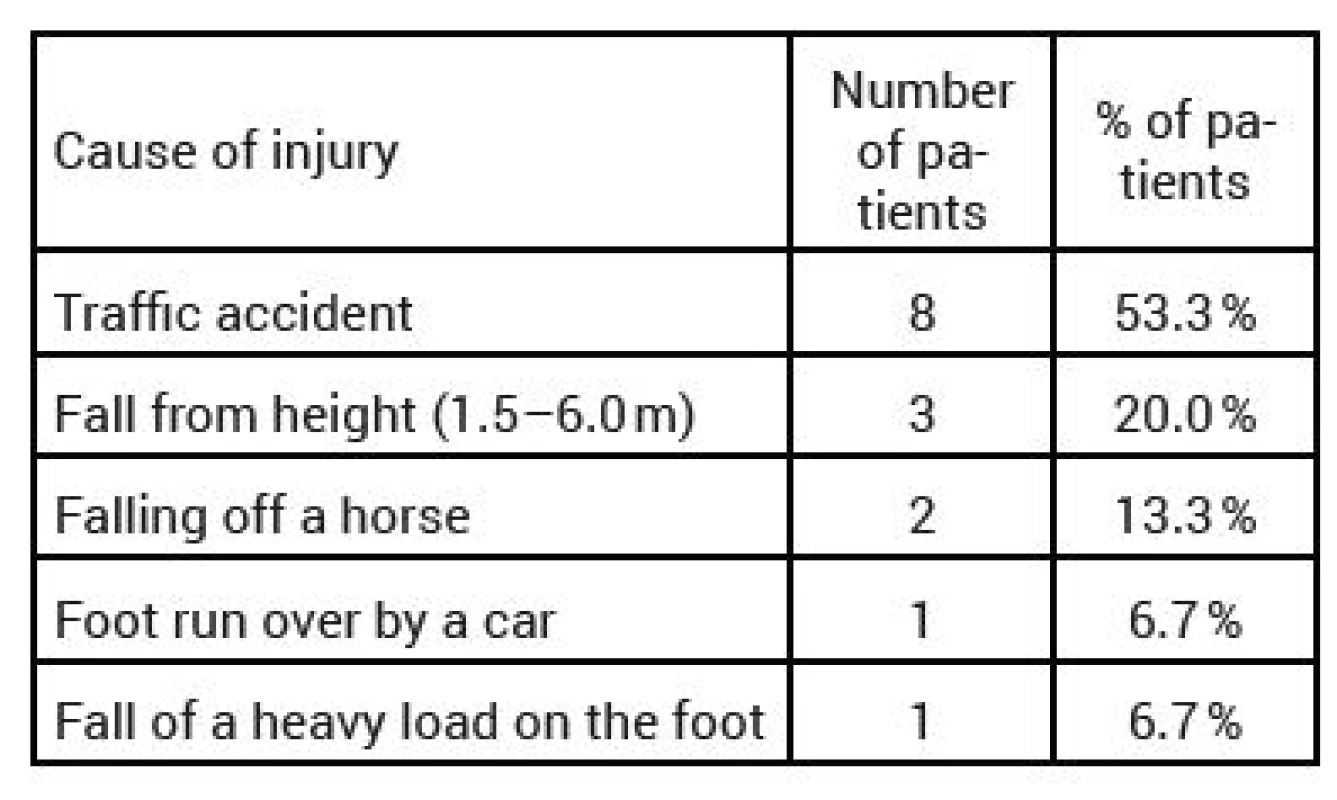
Talus fracture in monotrauma was observed in 7 patients (46.7 %), three patients (20 %) sustained a compound injury. In five cases (33.3 %), the talus fracture was associated with ipsilateral injury of the fibular ankle, tibia or calcaneus. The fractures types, assessed according to the Hawkins classification, were the following: Type I fracture was observed in 5 patients (33.3 %), Type II fracture in 8 patients (53.3 %), and Type III fracture in 2 patients (13.3 %). High-energy mechanism of injury was recorded in most patients; the injury mechanisms are presented in detail in Table 1.
The average length of stay among the observed patients was 9 days (4–21 days). The patients were treated with a definite osteosynthesis on the 5th day post injury on average (1–10 days). The reasons for postponing the surgical management included ankle and foot swelling, and also superficial injury of the soft-tissue cover at the surgical site.
Types of surgical approaches and techniques
Surgical approaches were selected according to the type and character of the fracture, and also the extent of fragment dislocation or the possibility to achieve a closed reduction under skiascopic control, and also according to the condition of soft tissues. Open reduction and stabilization with cannulated screws was performed in five patients from the anteromedial approach (33.3 %). In three patients, stabilization using cannulated screws was performed from anteromedial percutaneous incisions (20 %). Arthroscopy-assisted osteosynthesis with cannulated screws from puncture incisions located anteriorly and posterolaterally was performed in three patients (20 %). Antero-medial approach for open reduction was used in two patients, with Chevron osteotomy technique at the medial ankle (13.3 %). In the remaining two patients (13.3 %), a combined anterolateral – anteromedial approach was used. See Table 2. Arthroscopy-assisted osteosynthesis was performed in three patients (20 %) with undislocated or minimally dislocated talus neck fractures. Mini-invasive osteosynthesis was indicated in three patients (20 %) with undislocated or minimally dislocated fractures, in which closed reduction under skiascopic control was achieved. In nine patients (60 %), it was necessary to perform an open reduction from the anteromedial or combined approach (anteromedial and anterolateral).
Tab. 2. Types of surgical procedures and surgical approaches 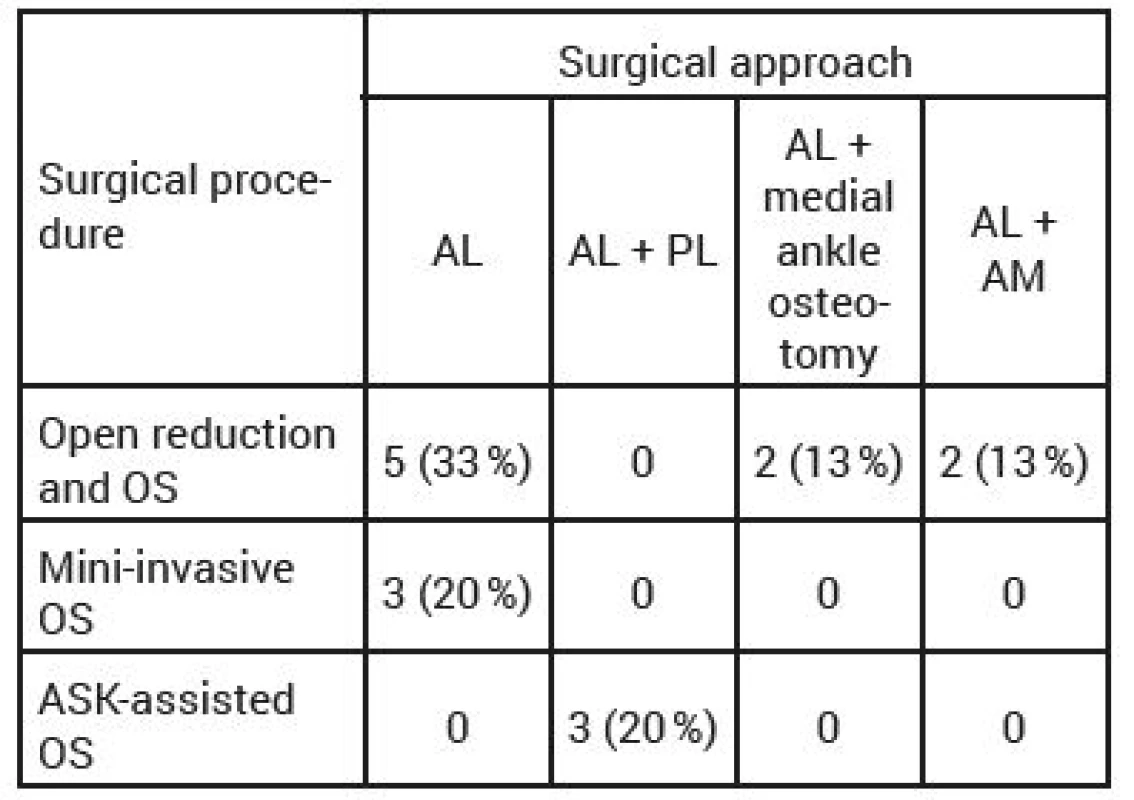
OS-osteosynthesis, ASK-arthroscopically, AL-anterolateral, PL-posterolateral, AM-anteromedial Radiographic results
Signs of I-II degree arthritis on radiography were observed in four patients (26.7 %) after 24-month follow-up. See Fig. 7. In one patient (6.7 %), who is still being followed, avascular necrosis was suspected, based upon MRI (magnetic resonance) findings.
Fig. 6. Ankle arthritis according to X-ray examination (AP and lateral projection of the ankle) 
Fig. 7. Ankle arthritis according to X-ray examination (AP and lateral projection of the ankle 
Functional outcomes of the range of movement of the ankle and the foot – dorsal flexion and plantar flexion in the upper ankle joint and inversion and eversion of the foot
The ranges of movement of the ankle and the foot were always compared with the contralateral healthy extremity.
In order to assess the dorsal and plantar flexion, we divided the patients into three groups. In nine patients (60 %), normal or minimally limited range of movement (30°and more) was observed; furthermore, we noted six patients (40 %) with medium limitation of movement (15–30°). The last was a group of patients with a significant limitation (less than 15°), which was however not observed in any of the patients in our group.
Also for evaluation of inversion and eversion of the foot, the patients were divided into three groups. Six patients (40 %) were included in the first group with normal findings or a minimal limitation (75–100 % of normal findings), seven patients (46.7 %) belonged to the second group with a medium limitation (25–75 % of the normal range of movement), and two patients (13.3 %) fell within the third group with a significant limitation of movement (less than 25 % of the normal range of movement). (See Tables 3 and 4).
Tab. 3. Range of movement – flexion/extension 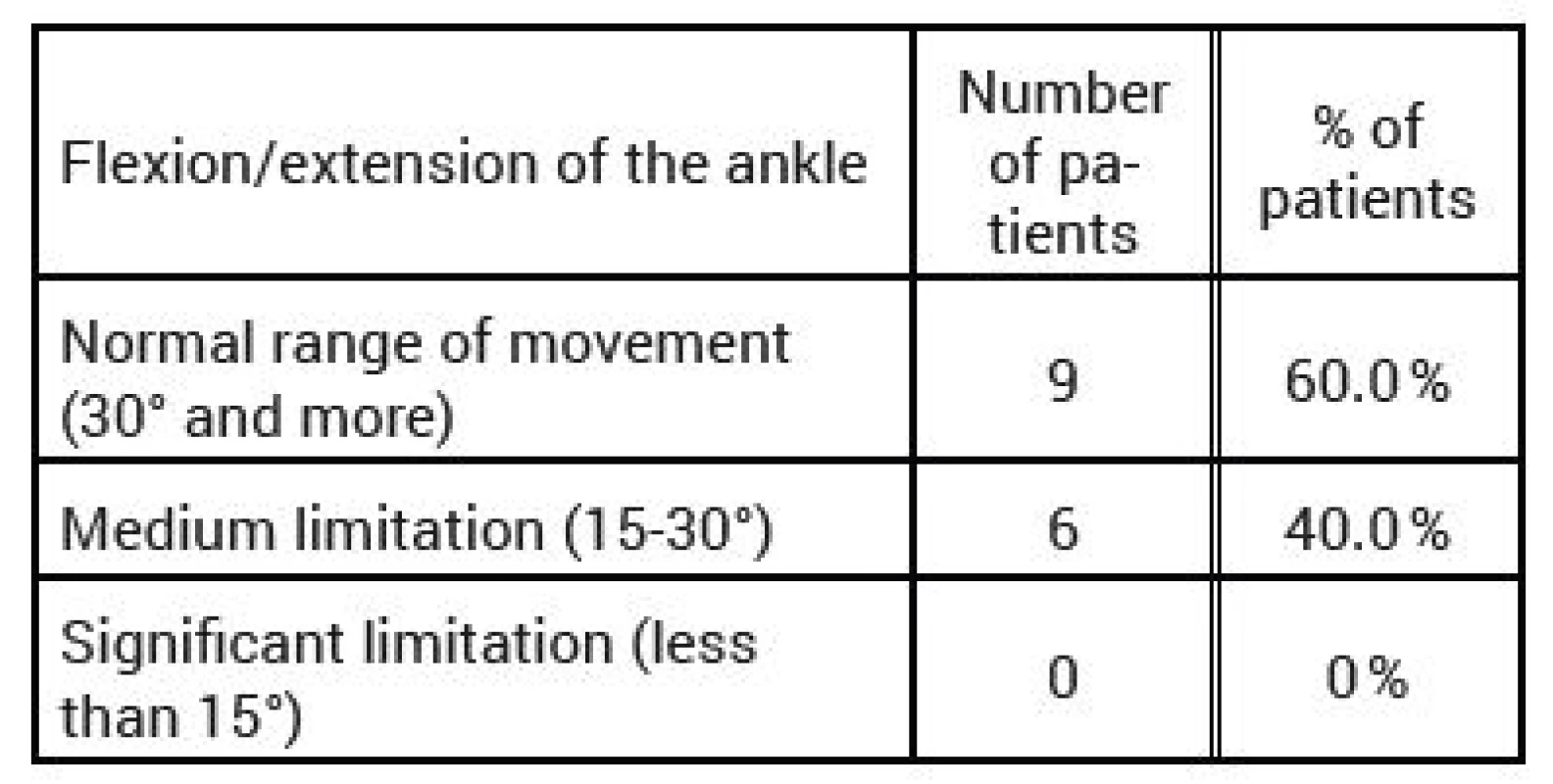
Tab. 4. Range of movement – inversion/eversion 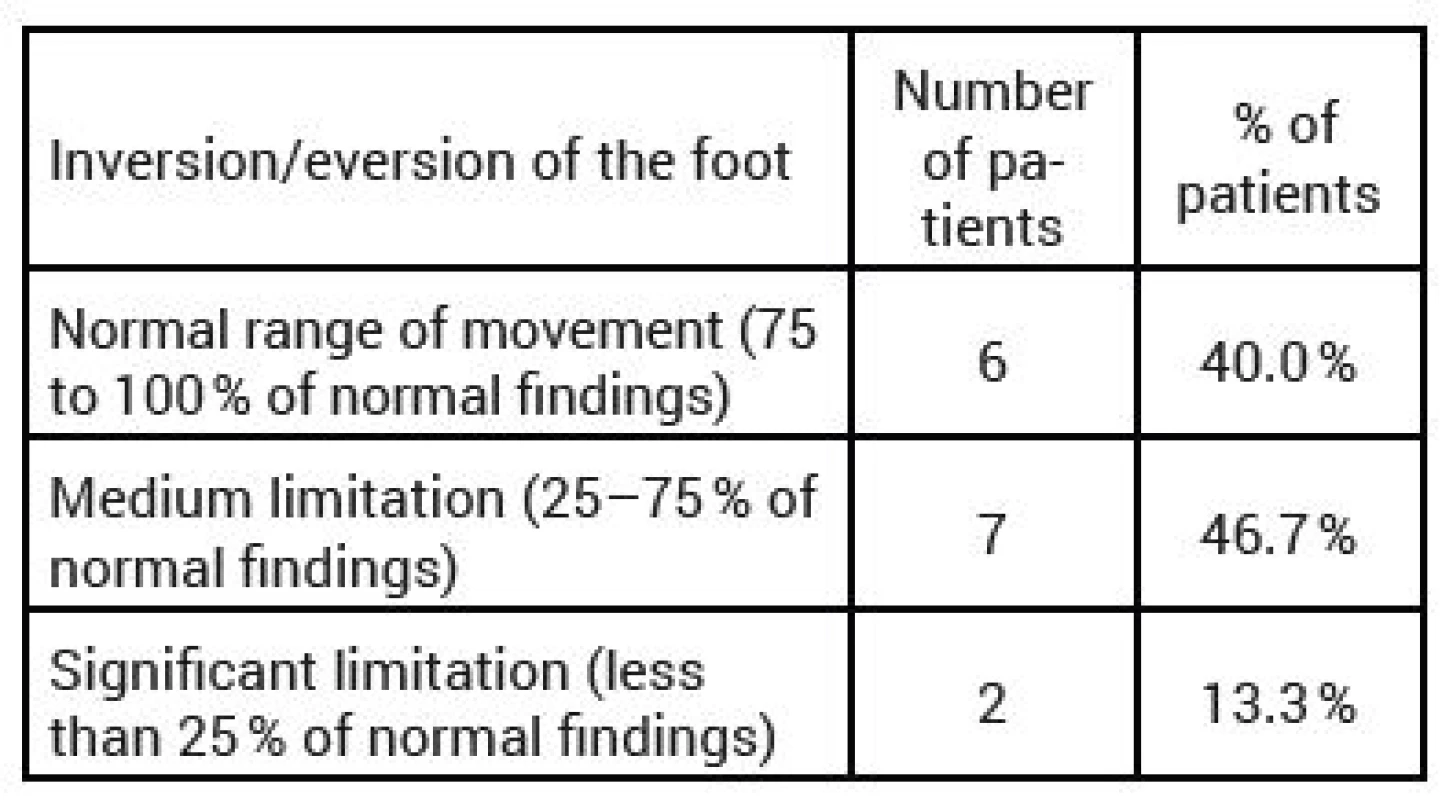
The average total AOFAS score among the observed patient population was 72.5 points (38–97 points); excellent outcome was achieved in three patients (20 %), good outcome in four patients (26.7 %), satisfactory outcome in three patients (20 %), and poor outcome in five patients (33.3 %). (See Chart 1). A total of six patients (40 %) with the average AOFAS score of 73 were treated within 1–2 days after injury. Nine patients (60 %) with the average AOFAS score of 72 points were treated between 4th and 10th day after injury.
The quality of achieved reduction in talus neck fractures was evaluated according to perioperative radiographs of the ankle in anteroposterior and lateral projections, as recommended by Lindvall et al. [22]. The fractures were considered anatomically reduced when no dislocation or angulation of fragments was observed in the frontal plane. Approximately or almost anatomically reduced fractures showed a dislocation of max. 1–3 mm and angulation in the frontal plane less than or equal to 5 degrees. Fractures with dislocation exceeding 3 mm and angulation over 5 degrees were assessed as insufficiently reduced. See Table 5.
Tab. 5. Demographic data, types of fractures, quality of reduction, complications 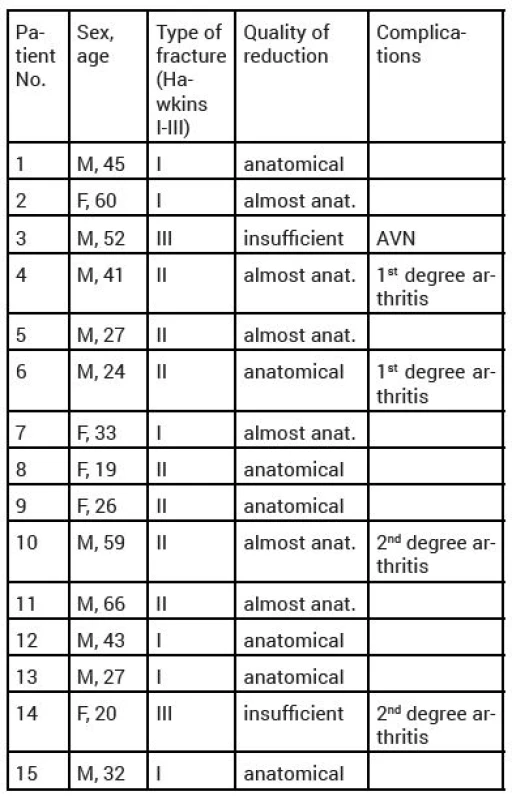
M-male, F-female, AVN-avascular necrosis DISCUSSION
According to literature, the mechanism of injury in talus neck fractures is usually indirect [3, 19]. Also in our patient population, indirect mechanism of injury was noted in most of the cases. These fractures are very often associated with high-energy mechanisms of injury – falls from heights, car and motorcycle accidents, and occur predominantly in the young, active, and mobile part of population [3, 16, 19]. The patient population that we analysed included a higher proportion of men, and increased share of patients younger than forty years of age. Traffic accidents were responsible for the injury in more than half of the patients. A high-energy mechanism of injury was reported in 86.7 % of cases. Domestic authors report a high-energy mechanism of injury in 95 % [9]. It is therefore possible to say that our results correlate with the expert literature. Isolated talus fractures were observed in 46.7 % of cases (n=7). Lorentzen, whose patient file included 123 cases of talus neck fractures, described an associated injury in 49 % of cases in total, and 10 % representation of associated injuries of the calcaneus [17]. Kopp et al. reported the incidence of associated injuries between 5.7 and 20.5 % [9, 20]. When diagnosing talus fractures, we proceeded from anamnestic data (mechanism of injury – high-energy vs. low-energy), over to physical examination (pain, swelling, haematoma, deformity). Subsequently, radiograph of the ankle and the foot was obtained in standard projections. In cases when a fracture was diagnosed on the radiographs, CT examination of the ankle followed, which provided us with necessary information for correct classification of the talus fracture. This imaging modality is irreplaceable for correct assessment of mutual position of the fragments, especially in more fragmented fractures, congruence of joint surfaces, and imaging of possible subluxations, namely in the subtalar junction, and thus associated preoperative planning [15, 16]. Also other domestic authors describe identical diagnostic procedure [9, 20]. In indicated cases, 3D CT reconstruction was also performed.
Magnetic resonance imaging (MRI) plays an important role in assessing the injuries of cartilage, associated soft-tissue injuries, and particularly the degree of post-injury necrosis, which applies to the conservative as well as surgical treatment. MRI may be also used for postoperative assessment of the fracture following implantation of osteosynthetic material [3, 15], or possible diagnostics of non-unions.
We performed an MRI examination without the use of a contrast agent in one case, at the interval of eight months from surgery, based upon a suspicion of avascular necrosis on a control radiograph in AP and lateral projections of the ankle, with apparent changes of bone structures of the talus, and its partial collapse.
As far as timing of the surgery is concerned, expert literature recommends rather delayed performance of the surgical procedure – definite management following after emergency reduction [11, 12, 16, 18]. The patients observed in our group were treated on the first or second postoperative day in 40 % of cases, delayed surgery, within 4 and 10 days, was performed in 60 % of patients, with almost identical outcome AOFAS score, see above. The results of our observations show that there exist no significant differences between patients undergoing definite management immediately after injury, and patients with a delayed definite treatment, after a primary emergency reduction, and temporary stabilization using external or plaster fixation.
Our decision-making whether to perform immediate or delayed surgical procedure was influenced mainly by the following factors: monotrauma or compound injury, open or closed fracture, condition of soft tissues, and last but not least, also the availability of an erudite and experienced trauma surgeon dealing with the given topic.
At our centre, also undislocated or minimally dislocated talus neck fractures are indicated for surgical treatment, mainly due to the earlier postoperative mobilization and prevention of complications associated with a long-term fixation of extremities – muscle dystrophy, osteoporosis, arthritis, joint stiffness, longer and more demanding postoperative physiotherapy. This procedure is recommended for example by Kopp et al. [9]. The most frequently used surgical approach among our patients was the anteromedial approach. Some authors recommend the medial approach, which may be supplemented with anterolateral approach, in order to perform a precise anatomical reduction [2, 16]. Our results show that in cases of undislocated or minimally dislocated fractures, especially Hawkins type I–II, it is more suitable to indicate a mini-invasive type of osteosynthesis or the arthroscopy-assisted approach. These mini-invasive types of fracture osteosyntheses eliminate the disadvantages of open reduction and osteosynthesis, especially as far as faster physiotherapy and healing of soft tissues are concerned. Another undisputable advantage is the ability to achieve a visual control of the fragment reduction and congruence of the joint surface in arthroscopy-assisted types of osteosyntheses. Nevertheless, this procedure is closely associated with the experience of the operating surgeon dealing with ankle arthroscopy [9].
Plate osteosynthesis, recommended by some authors as a treatment of choice [9, 10], was not used in our patients.
Another serious complication, closely related to the anatomical layout of the talus vascular supply, is avascular osteonecrosis (AVN). The severity rate of AVN is directly related to the primary dislocation of fragments caused by the injury mechanism [16, 18]. The reported risk for Hawkins type I fractures is 0–14 %, for type II fractures 20–50 %, and for type III and IV, the reported risk is between 75 and 100 % [4, 7]. Hawkins published a study in 1970, in which he evaluated a total of 57 talus neck fractures, with a 53 % - incidence of avascular necrosis [7]. Canale and Kely, in a group of 71 patients, reported an incidence of 52 % [3, 4]. Sanders et al. (2004) reported an 11 % incidence of AVN in 70 observed patients [11]. Vallier observed AVN in 25 % of cases [18].
Among our patients, we observed avascular necrosis in one female patient only (6.7 %). Kopp et al. and Zeman et al. report the incidence of avascular necrosis between 14 and 17 % [9, 20].
The observed significant difference, when compared with foreign literary sources, is most probably caused by the size of our group and the length of their follow-up.
The incidence of post-injury arthritis is very common, together with arthrofibrosis and stiffening of the ankle [19]. Among our patients, we observed post-injury arthritis on X-ray in four patients (26.7 %). Domestic literary sources report the incidence of post-injury arthritis in the range of 23.8–40 % of cases [9, 20]. Lamothe observed post-injury arthritis in almost 100 % of patients with extended follow-up [11]. Vallier divided post-injury arthritis according to impairment of individual talar joints, and reported the arthritis incidence of 38 % in the subtalar, 29 % in the tibiotalar, and 4.6 % in the talonavicular joint [18]. The observed difference is caused, according to our opinion, by the various length of patient follow-up from the injury, and by different interpretation of X-ray findings. Deep infection is often associated with a serious invalidity of the patient, and results in impaired function of the foot [15]. We did not observe any case of deep talar infection among our patient population. In cases of open talus fractures of a higher degree, it is advantageous to use vacuum therapy for primary treatment of the skin cover [10].
Domestic literature reports a superficial infection of soft tissues in 7 % of cases [13]; Kopp et al. mention deep infection, which required a removal of the osteosynthetic material and administration of antibiotic therapy in two of his patients, i.e. 4.8 % of cases [9]. Vallier observed deep infection in 1.3 % of patients [18].
Non-unions are relatively rare in talus fractures, however they present a serious complication. They tend to develop into secondary degenerative changes, which often require performance of arthrodesis of the lower or upper ankle joint, with subsequent significant functional limitation of the ankle [19]. We did not observe any non-unions among our patient population.
CONCLUSION
Talus fractures belong among serious fractures, due to the frequent occurrence of post-injury complications, which may significantly limit the movement of the patient, and thus threaten the patient’s social participation. This applies to both conservatively and surgically treated fractures of the talus neck. These complications are given by the anatomical structure of the talus, vulnerable vascular supply, and also by the high mechanical requirements imposed upon the talus. They are closely related to the primary dislocation or luxation of fragments caused by the injury, character and type of fracture, and ultimately also to the fact whether the fracture is closed or open. In order to eliminate the mentioned complications in the most effective way, a timely reduction is required in every dislocated, luxation or open fracture. Our results show that in undislocated or minimally dislocated talus neck fractures, with a favourable condition of the soft tissues, and availability of an experienced surgeon, it is possible to perform definite treatment the fracture at one time, using mini-invasive or arthroscopy-assisted osteosynthesis. Also undislocated fractures should be indicated for surgical stabilization. Nevertheless, in cases of fractures with initial severe displacement, luxation or open fractures, on if not permitted by the condition of soft tissues, it is more beneficial to perform a primary emergency reduction and apply external fixator or plaster fixation, and to perform a delayed definite treatment, with a careful preoperative consideration, after the condition of the patient and soft tissues has been stabilized. The results from our patients show that the primary definite management of the fracture, as well as a staged delayed procedure of talus fracture treatment are possible. However, even the best timing and planning of surgical management of these fractures does not completely eliminate early complications, associated with this type of fractures.
Zdroje
-
Bartoníček, J. Základy klinické anatomie pohybového aparátu. Praha : Maxdorf, 2004. 256 s.
-
Berlet, GC., Lee, Th, Massa, EG. Talar neck fractures. The Orthopedic Clinics of North America. 2001, 32, 53–64.
-
Browner, Jupiter, Levine, Trafton, Krettek, Skeletal trauma: Basic Science, Management, and Reconstruction, Volume two. Philadelphia, USA: Saunders Elsevier, 2008, 2585–2618 s .
-
Canale, ST, Kelly, FB Jr. Fractures of the neck of the talus. J Bone Joint Surg Am. 1978, 60, 143–156.
-
Čihák, R. Anatomie. Praha : Avicenum. 1987, 456 s.
-
Coltart, WD. Aviators astralagus. J Bone Jt Surg. 1952, 34, 545–566.
-
Hawkins, LG. Fractures of the neck of the talus. J Bone Jt Surg. 1970, 52-A, 991–1002.
-
Kitaoka, HB., Alexander, IJ., Adelaar, RS. et al. Clinical rating system for the ankle-hindfood, midfoot, hallux and lesser toes. Foot Ankle int. 1994, 15, 349–353s.
-
Kopp, L., Obruba, P., Riegl, J. et al. Chirurgická léčba zlomenin talu – střednědobé funkční a rentgenové výsledky. Acta Chirurgiae Orthopaedicae et Traumatologiae Čechosl. 2013, 80, 165–170.
-
Krtička, M., Ira, D., Nekuda, V. et al. Primární aplikace podtlakové terapie u otevřených zlomenin III. stupně a její vliv na vznik infekčních komplikací. Acta Chirurgiae Orthopaedicae et Traumatologiae Čechosl. 2016, 83,117–122.
-
Lamothe, JM., Buckley, RE. Zlomeniny talu. Současný pohled z hlediska diagnostiky, léčby a výsledků. Acta chirurgiae orthopaedicae et traumatologiae Čechosl. 2012, 79, 97–106.
-
Paul, JJ., Dabbah, M., Harris, TG. Talar neck fractures. Foot Ankle Clin. 2004, 9, 723–736.
-
Peml, M., Kácal, P., Kopačka, P. et al. Periferní zlomeniny talu – střednědobé výsledky operační léčby. Acta Chir Orthop Traumatol Čech. 2016, 83, 399–404.
-
Pokorný, V. a kol. Traumatologie. Praha : Triton, 2002, 220–223.
-
Rockwood and Greens. Fractures in adults – seventh edition. Philadelphia, USA, 2010, 2022-2061s.
-
Rammelt, S., Zwipp, Z. Talar neck and body fractures. 2009, 2, 120–135.
-
Lorentzen, JE, Bach, SC., Krogsøe, S.. Fractures of the neck of the talus. Acta Orthopaedica Scandinavica. 1977, 115–120.
-
Vallier, HA. et al. A New Look at the Hawkins Classification for Talar Neck Fractures: Which Features of Injury and Treatment Are Predictive of Osteonecrosis? J Bone Jt Surg. 2014, 3, 192–197s.
-
Wendsche, P., Veselý, R. et al. Traumatologie. Praha : Galén, 2015, 278–282.
-
Zeman, J., Matějka, J., Pavelka, T. Chirurgické léčení zlomenin krčku a těla talu. Acta Chirurgiae Orthopaedicae etTraumatologiae Čechosl. 2012, 79, 119–123.
-
Žvák, I., Brožík, J., Kočí, J. et al. Traumatologie ve schématech a RTG obrazech. Praha : Grada Publishing, a.s. 2006, 165–168.
-
Lindvall, E., Haidukewych, B., DiPasquale, T., et al. Open reduction and stable fixation of isolated, displaced talar neck and body fractures. J Bone Jt Surgery. 2004, 86, 2229–2234.
Štítky
Chirurgie všeobecná Traumatologie Urgentní medicína
Článek vyšel v časopiseÚrazová chirurgie
Nejčtenější tento týden
2017 Číslo 4- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Stillova choroba: vzácné a závažné systémové onemocnění
- Hojení análních fisur urychlí čípky a gel
- Jak souvisí postcovidový syndrom s poškozením mozku?
- Cinitaprid – v Česku nová účinná látka nejen pro léčbu dysmotilitní dyspepsie
-
Všechny články tohoto čísla
- Surgical stabilization of chest wall –development of the method and contemporary trends
- Abdominal compartment syndrome in polytrauma
- Blunt liver and splenic trauma due to distal rib fracture
- Evaluation of medium-term outcomes of surgical treatment of talus neck fractures at the Department of Trauma Surgery, University Hospital Brno
- Přečetli jsme za Vás
- Úrazová chirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Abdominal compartment syndrome in polytrauma
- Blunt liver and splenic trauma due to distal rib fracture
- Surgical stabilization of chest wall –development of the method and contemporary trends
- Evaluation of medium-term outcomes of surgical treatment of talus neck fractures at the Department of Trauma Surgery, University Hospital Brno
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání