-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Surgical stabilization of chest wall –development of the method and contemporary trends
Authors: Maria Štěpánková 1; František Vyhnánek 2; Robert Gürlich 2; Dana Škrabalová 3
Published in the journal: Úraz chir. 25., 2017, č.4
Summary
Introduction:
Surgical stabilization of flail chest and other unstable injuries of the thoracic wall is a relatively new treatment procedure. The indications for rib osteosynthesis include, apart from flail chest fractures of at least three ribs, also a defect or chest wall deformities, dislocated rib fractures with injury of the lungs, open rib fractures, impaired fracture healing and stabilization of fractures in patients with emergency thoracotomy performed due to blunt and penetrating chest injuries. The aim of this article is to present an overview of development of plate stabilization of the chest wall, and to inform the reader about the current trends in indications and timing of this procedure.
Material and results:
The historical summary of chest wall stabilization using plate fixation also mentions important milestones in the development of this technique. The subsequent overview summarizes advantages of the technique, together with new knowledge in the management of blunt chest trauma.
Conclusion:
The area of chest wall stabilization remains a topical issue. Although this technique is not considered a standard procedure in the management of blunt chest trauma, it becomes of great interest for trauma surgeons and manufacturers of implants. New guidelines define a broader use of surgical chest stabilization, and advocate an early intervention in indicated cases.
Keywords:
Surgical chest wall stabilization, flail chest.
Introduction
Blunt chest injuries with multiple rib fractures often occur as a part of polytrauma and compound injuries. They most frequently originate as a consequence of traffic accidents or falls, and represent 25% of all trauma-related deaths. The number of complications, morbidity and mortality associated with chest wall injuries increases in parallel with age [29], the number of fractured ribs, and the presence of flail chest [6]. Rib fractures are observed in up to 39 % of patients with blunt chest trauma. [9].
A flail chest is characterized by the presence of at least two fracture lines of at least three neighbouring ribs, in between of which a segment is broken off (Fig. 1, 2). In flail chest injuries, mechanical cohesion between the broken off segment and the chest wall is lost, which results in paradoxical movement [7]. The prevalence of flail chest trauma reaches about 10 % in patients with blunt chest trauma, and is associated with a relatively high degree of mortality (9–16 %) even today [10]. The presence of flail chest is often associated with pulmonary contusion, hemothorax and pneumothorax [7]. These injuries often lead to acute pain and mutually contribute to disruption of respiratory mechanics. The body reacts to the acute pain by decreasing the respiratory volume, which is a predisposition for the onset of atelectasis, hypoxemia, respiratory insufficiency [15], and ultimately a higher incidence of pneumonia, ARDS, and which often requires prolonged artificial ventilation, with all its associated risks and complications [9]. In patients treated without a surgical intervention, a high level of long-term complications persists, such as chronic pain, chest wall deformity, long-term sickness leave and decreased quality of life [19].
Fig. 1. MDCT image of flail chest on the right 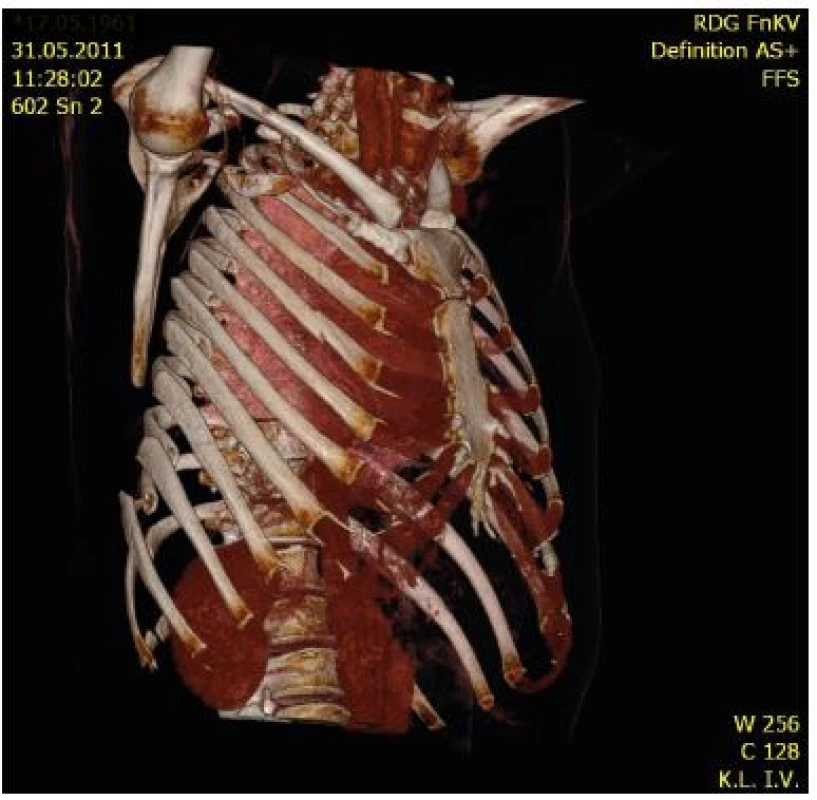
Two basic principles are applied in the therapy of flail chest. Artificial ventilation, supplemented with appropriate analgesia and bronchoalveolar lavage represents a standard conservative treatment. However, this technique cannot compensate for the chest wall deformities, which may lead to chronic respiratory insufficiency and prolonged pain [17]. On contrary, surgical treatment, when compared with conservative therapy, including implantation of modern instruments, provides various benefits for patients in indicated cases; these result from better stabilization of the chest wall. Despite the already proven advantages, surgical stabilization of the chest wall remains a relatively infrequently used technique. From the results of the retrospective analysis, using the data from National Trauma Data Bank in Canada including 3 467 patients with flail chest trauma treated between 2007 and 2009 it becomes apparent that only 0.7 % of patients underwent surgical stabilization of the chest wall [10].
Fig. 2. MDCT image of flail chest fracture of 7 ribs on the right, with a deformity of the chest wall 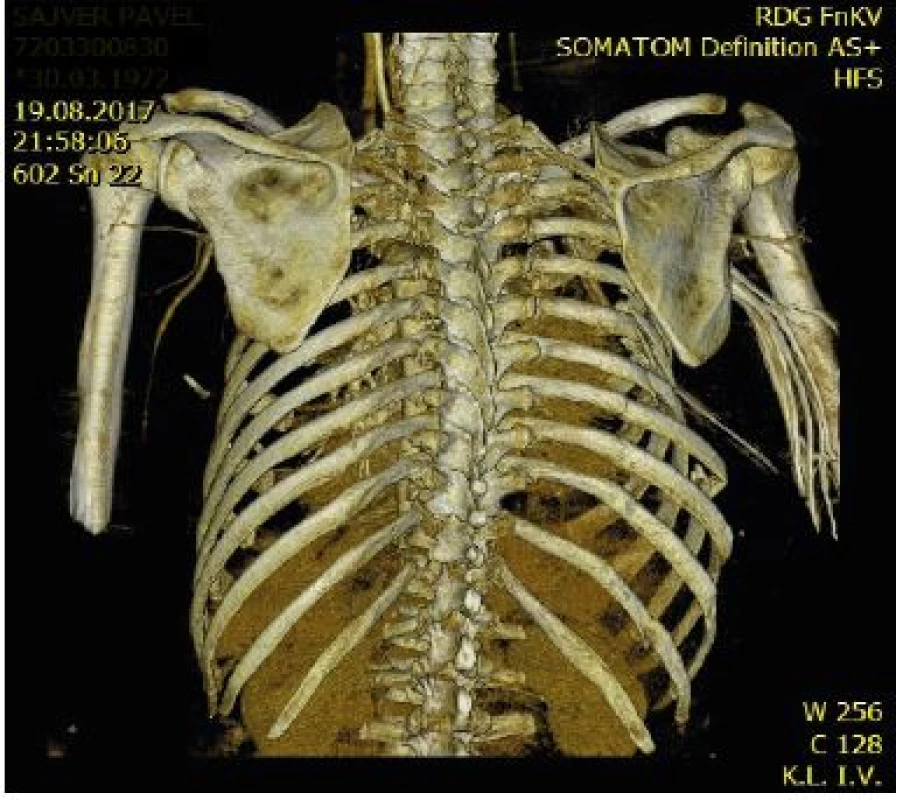
Previously reported reasons of persisting tendencies towards conservative therapy included a lack of clinical studies with long-term outcomes comparing both treatment methods [11], general risks of surgical treatment, early infections, and a lack of experienced surgeons [22]. The randomized clinical trials, which have been published so far, enrolled only low numbers of probands, and the control groups lack a comparison of outcome measures of conservative treatment in modern units of intensive care [11].
These present drawbacks have been compensated with a meta-analysis of data obtained from results of controlled clinical trials of conservative therapy of flail chest injuries, and with comparing them to clinical outcomes of all surgically treated patients in randomized clinical trials. The results of the meta-analysis show significantly more favourable clinical outcomes in patients undergoing surgical treatment [27].
What is more, new guidelines were published last year; these are based upon a consensus of experts, and broaden the already existing indications for surgical stabilization of the chest wall [26].
These findings create favourable conditions for the increasing interest of trauma surgeons and manufacturers of implants in gaining more experience with surgical chest wall stabilization.
Development of surgical plate stabilization of the chest wall
The history of plate osteosynthesis of the chest wall dates back to the 1960s, when this type of fixation was first described in the work of Sillar; these plates were intended predominantly for stabilization of sternal fractures, as rib fractures were being fixed with K-wires at that time [30]. In 1973, Judet introduced his plate with lateral hooks intended for fixation of the plate to the rib using pliers [14]. Two years later, Paris published a report concerning the use of various types of plates for rib fixation with suture or wire cerclage, including one of the first techniques of minimally invasive plate osteosynthesis, when the plates were implanted through small incisions, and also long plates which could be used for treatment of the broken off segment of the chest wall [23]. In 1979, Véscei [34] introduced a short plate intended for treatment of simple rib fractures; the plate was fixed with cerclage. Another milestone was the introduction of Labitzke’s clamp plates in 1980 [18], where the individual clamps were joined asymmetrically, which made bending at the plate level possible. By introduction of these plates, a period of further development of chest wall osteosynthesis using clamp plates began; these plates were equipped, contrary to the previously used types, with lateral hooks, which were fixed to the rib using pliers. This means of fixation is generally considered to be a safer technique than fixing the plates with wire cerclage or suture. Although it was possible to lay the Labitzke’s plates over both fracture lines of the chest segment, this type of implant was not suitable for treatment of flail chest injuries, due to its already mentioned flexibility. In 1982, Sánchez-Lloret presented a clamp plate enabling a rigid osteosynthesis of flail chest injuries [28].
At present, anatomically shaped plates MatrixRIB® of the DePuy Synthes company are widely used. Their main advantage is elimination of the need to bend the plate prior to implantation. The plates are fixed using locking screws, which provide a rigid stabilization, and are thus suitable for fixation of flail chest injuries [1]. Among the current modern implants it is not possible to omit the STRATOS™ system for chest osteosynthesis, made by the MedXpert company, developed at the University Hospital in Strasbourg in 2007 [40].
Development of plate osteosynthesis for the chest wall manufactured by the Czech company Medin a.s. from Nové Město na Moravě, was realized in cooperation with colleagues from the Research Centre of Special Surgery and Traumatology, Trauma Hospital in Brno. These are clamp plates, similar to the Judet’s clamps, with lateral hooks intended for fixation of the plate. The team of this Centre published their first clinical experiences in 1996 [21]. In 2007, Vodička et al. published results of a retrospective study [35], which included 40 patients treated with Medin plates in the course of 10 years. Development of innovated rib LCP plates Medin was accomplished in the following years, in cooperation between the Traumatology Centre and Department of Surgery, University Hospital Královské Vinohrady and 3rd Faculty of Medicine, Charles University in Prague and the Development Department of the Medin company. Last year, the team of Vyhnánek et al. published their first clinical experience with these plates in patients with unstable chest injuries [36, 37] (Fig. 3, 4).
Fig. 3. Perioperative image of rib osteosynthesis performed using the innovated Judet-type plates prior to closure of thoracotomy 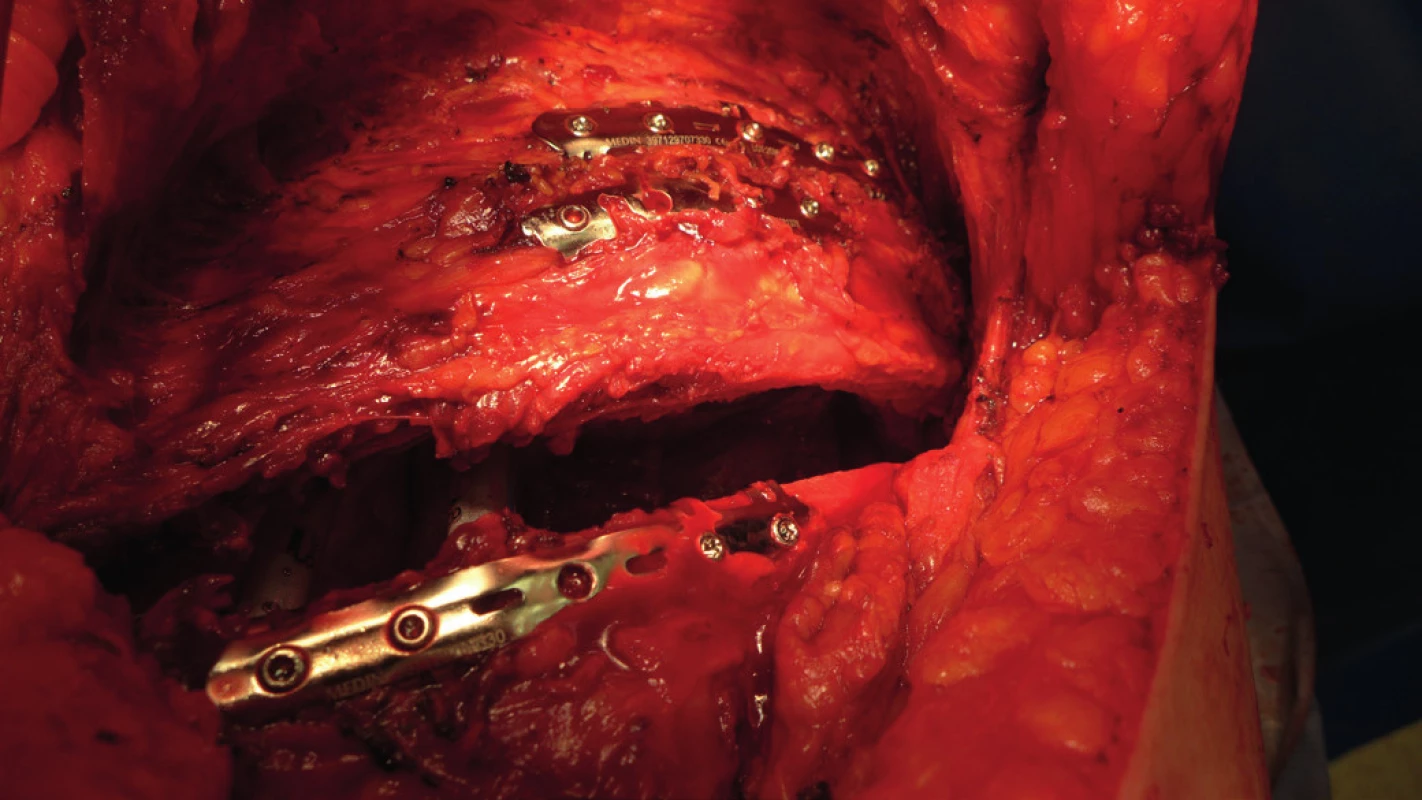
Fig. 4. MDCT image of osteosynthesis of 4 ribs on the right side, using the innovated Judet-type plates 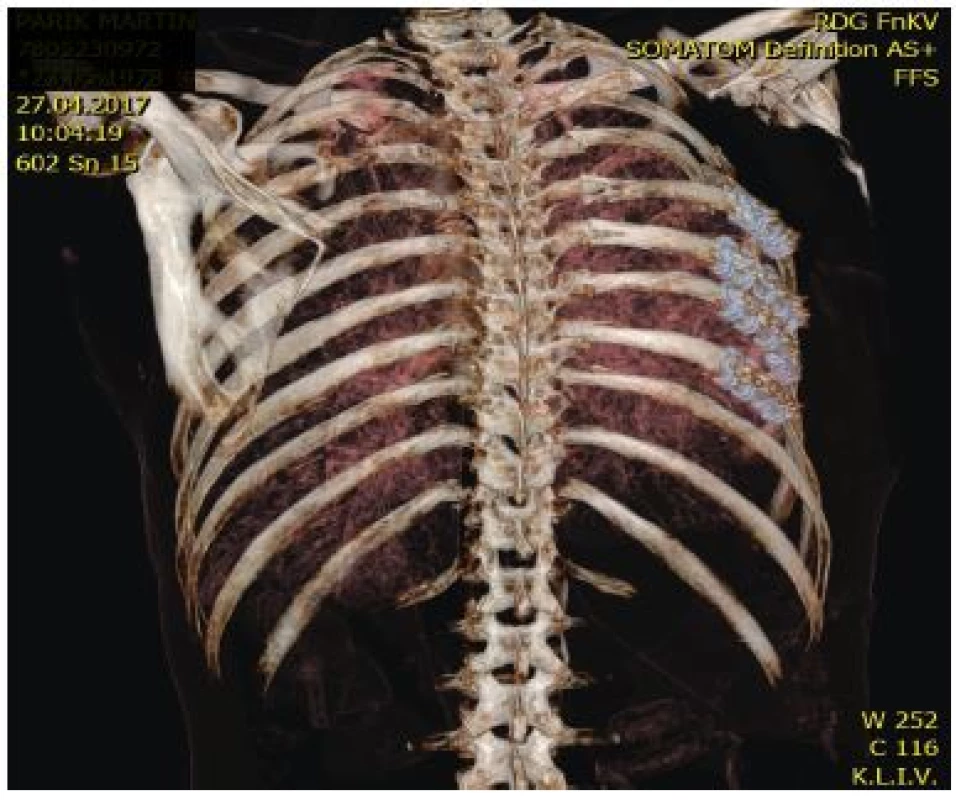
In the Czech Republic, various plates from Czech and foreign manufacturers are currently used. The instruments from foreign producers are represented namely with the already mentioned MatrixRIB® Synthes and STRATOS™ MedXpert systems. Domestic manufacturers are represented with the innovated Medin clamp plates.
Advantages of surgical chest wall stabilization
A number of clinical, mostly retrospective studies have proven the benefit of surgical chest wall stabilization in patients with flail chest, in the sense of shortening the period of mechanical ventilation and the ICU stay, lower incidence of pneumonia and lower mortality [3, 4, 13, 16, 25, 38, 39, 41, 42, 43]. These studies have analysed non-homogeneous groups of patients of various ages, with various comorbidities and mechanisms of injury.
In international expert literature, three randomized studies have been published so far, proving the beneficial effect of surgical stabilization in patients with flail chest. A total of 37 patients with flail chest injuries were enrolled into the study published by Tanaka et al. [32]; the patients required mechanical ventilation support, and were initially treated conservatively at intensive care unit, according to identical protocol. The patients were divided into two groups, a surgical group (18 patients), and a group of patients treated conservatively (19 patients). In all patients, the parameters such as age, representation of males and females, trauma score (ISS + AIS), localization of the flail segment (anterolateral/posterolateral), number of fractured ribs and ventilation parameters (PaO2/FIO2 index) upon admission to the hospital were comparable. The patients in the first group underwent surgical stabilization with Judet’s clamps five days after trauma, and the second group of patients were left on ventilation support. Among the group of patients undergoing the surgical procedure, the following was confirmed, when compared with the conservatively treated patients: shorter period of ventilation support (10 versus 18 days), shorter ICU stay (16 versus 26 days), and a lower incidence of pneumonia (24 % versus 77 %). In the study published by Granetzny et al. [12], Kirchner wires or steel wires were used to stabilize the chest wall in patients undergoing surgical treatment, in the course of 24–36 hours after trauma. Among the patients with surgical stabilization of the chest wall, a significantly shorter period of artificial ventilation (2 versus 12 days), shorter ICU stay (9 versus 14 days), and a lower incidence of pneumonia (10 % versus 50 %) were observed, when compared with the group of patients on conservative therapy. By analogy, better ventilation parameters were recorded in patients with surgical treatment when compared to patients treated conservatively 2 months after trauma. The third randomized study was published by Marasco et al. [20], who used a biodegradable plate for treatment of flail chest; parameters such as artificial ventilation and ICU stay were in favour of the surgical treatment, however no significant difference in parameters on spirometry in both groups was observed 3 months after trauma.
Coughlin et al. published a meta-analysis in 2016 studying the results of treatment in patients with flail chest. The clinical outcomes of the three above-presented clinical trials, with the total number of 123 patients treated surgically were compared with the outcomes of conservative treatment of flail chest presented in published control trials. Surgical treatment of flail chest was associated with generally more favourable clinical parameters. The incidence of pneumonia was lower by two thirds, the period of mechanical ventilation and ICU stay were 6 days shorter, and the total period of hospitalization was 11 days shorter [8].
Another advantage brought about by the surgical chest stabilization is a demonstrable decrease of financial costs when compared to conservative treatment. The reason for this observation is a lower need of follow-on care, such as treatment of pneumonia, respiratory failure, and ICU costs [31].
Current indications of surgical stabilization and timing
Flail chest is traditionally considered to be an indication for surgical stabilization of the chest wall. The benefits of surgical intervention for patients were described in the three above-mentioned randomized clinical trials [12, 20, 32], and were also repeatedly proven in many retrospective studies.
Recent studies have proven better outcome parameters also in surgical patients with a more common type of chest trauma, which is a serial fracture of the ribs with dislocation. Uchida et al. have shown a shorter period of artificial ventilation, lower incidence of pneumonia, and a shorter ICU stay in surgical patients with multiple dislocated rib fractures, without the presence of flail chest [33]. In 2016, Pieracci described in his prospective study the positive impact of surgical stabilization upon the course and length of treatment, together with the incidence of complications in patients with other indications than flail chest, which included multiple dislocated rib fractures and serious chest deformity [25]. These indications are frequently based upon the poor perspective of conservative treatment in this group of patients, and include respiratory insufficiency and/or acute pain, persisting despite appropriate conservative therapy, and chronic pain or impaired respiratory mechanics [24].
Another clinically significant indication is a chronic non-union, which must be considered in cases of pains in the chest wall persisting 3–6 months after trauma, and also in cases when the initial radiography findings were negative [2]. Kaplan et al. reported on a therapy of multiple non-unions of the ribs using plate osteosynthesis, supplemented with autologous bone grafts [15].
When considering the prediction of complications associated with rib fractures, the use of CT scoring systems has become a new trend at trauma centres. Chapmann published his RibScore in 2016, which distinguishes among six categories, according to CT findings, and lists associated predictions of risks of pneumonia, respiratory failure and indication for tracheostomy [5].
New guidelines were published in 2017, based upon the consensus of participants of the Rib Fracture Colloquium Park City Utah 2016. Among the newly recommended indications belong multiple bicortical rib fractures, regardless of the fact whether mechanical ventilation is required, and furthermore also failure of optimal conservative therapy administered at an early stage, regardless of the radiography findings. All patients with flail chest are indicated for surgical stabilization. On the other hand, the earlier valid contraindications of surgical chest wall stabilization, such as pulmonary contusion and concomitant intracranial injury, were relativized, and the indication of surgical therapy should be considered individually in these patients [26].
Pieracci et al. analysed databases of patients from four trauma centres. These patients, who underwent a surgical stabilization of the chest wall between 2006 and 2016 (551 in total), were divided into three groups, according to the interval between the admission to the hospital and performance of surgical stabilization of the chest (I. Day 0; II. Day 1–2; III. Day 3–10). The reported indications for surgery included flail chest, at least three bicortical and dislocated rib fractures, chest deformity with more than 30 % reduction of the hemithorax volume, and failure of conservative therapy. The differences between the groups regarding the severity of the injury were not significant. The duration of surgery, incidence of pneumonia, number of days at artificial ventilation, length of hospital stay, length of ICU stay, and the number of patients with tracheostomy increased in parallel with the order of the group. Based upon these results, the authors recommend an early indication of surgical stabilization, ideally within 24 hours from admission [27].
Conclusion
Surgical plate stabilization of the chest wall has been developing since the 1950s, and presently offers various kinds of modern sets for providing rigid and safe stabilization of flail chest.
The advantages of surgical stabilization of the chest, when compared to conservative treatment, represented by artificial ventilation, are well known; they are reserved for an indicated group of patients with blunt chest trauma.
The most important indications for the procedure are flail chest, multiple bicortical rib fractures, and posttraumatic deformities of the chest wall.
New recommendations based upon the results of analyses of data from databases of trauma centres advocate even earlier stabilization.
Zdroje
-
BOTTLANG, M., HELZEL, I., LONG, WB. Anatomically contoured plates for fixation of rib fractures. J Trauma. 2010, 68, 611–615.
-
CACCHIONE, RN., RICHARDSON, JD. et al. Painful nonunion of multiple rib fractures managed by operative stabilization. J Trauma. 2000, 48, 319–321.
-
CARAGOUNIS, EC., FAGEVIC, OM., PAZOOKI, D. Surgical treatment of multiple rib fractures and flail chest in trauma: a one-year follow-up study. World J Emerg Surg. 2016, 11, 27.
-
CATANEO, AJ., CATANEO, DC., DE OLIVEIRA, FH. Surgical versus nonsurgical interventions for flail chest. Cochrane Database Syst Rev. 2015, 29, 7.
-
CHAPMAN, BC., HERBERT, B., RODIL, M. et al. RibScore: A novel radiographic score based on fracture pattern that predicts pneumonia, respiratory failure, and tracheostomy. J Trauma Acute Care Surg. 2016, 80, 95–101.
-
CHIEN, CY., CHEN, YH., HAN, ST. et al. The number of displaced rib fractures is more predictive for complications in chest trauma patients. Scand J Trauma Resusc Emerg Med. 2017, 28, 19.
-
CIRAULO, DL., ELLIOTT, D., MITCHEL, KA. et al. Flail chest as a marker for significant injuries J Am Cool Surg. 1994, 178, 466–470.
-
COUGHLIN, TA., NG, JW., ROLLINS, KE. et al. Management of rib fractures in traumatic flail chest: a meta-analysis of randomised controlled trials. Bone Joint J. 2016, 98-B,1119–1125.
-
DAVIGNON, K., KWO, J., BIGATELLO, LM. Pathophysiology and management of the flail chest. Minerva Anestesiol. 2004, 70, 193–199.
-
DEHGHAN, N., DE MESTRAL, C. MCKEE, MD. et al. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014, 76, 462–468.
-
FITZPATRICK, DC., DENARD, PJ., PHELAN, D. et al. Operative stabilization of flail chest injuries: Review of literature and fixation options. Eur J Trauma Emerg Surg. 2010, 36, 427–433.
-
GRANETZNY, A., ABD EL-AAL, M., EMAM, E. et al. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005, 4, 583–587.
-
JAYLE, CP., ALLAIN, G., INGRAND, P. Flail chest in polytraumatized patients: surgical fixation using Stracos reduces ventilator time and hospital stay. Biomed Res Int. 2015, 2015, 624–723.
-
JUDET, R. Costal osteosynthesis. Rev Chir Orthop Reparatrice Appar Mot. 1973, 59, 1, 334–335.
-
KAPLAN, DJ., BEGLY, J., TEJWANI, N. Multiple Rib Nonunion: Open Reduction and Internal Fixation and Iliac Crest Bone Graft Aspirate. J Orthop Trauma. 2017, 31, S34–S35.
-
KOCHER, JG., SHARAFI, S., AZENHA, LF. et al. Chest wall stabilization in ventilator-dependent traumatic flail chest patients: who benefits? Eur J Cardio-Thorac Surg. 2017, 51, 696–697.
-
KHANDELWAL, G., MATHUR, RK., SHUKLA, S. et al. Prospective single center study to assess the impact of surgical stabilization in patients with rib fracture. Int J Surg. 2011, 9, 478–481.
-
LABITZKE, R., SCHMIT-NEURBURG, KP., SSCHRAMM, G. Indications for thoracotomy and rib stabilization in thoracic trauma in the aged. Chirurg. 1980, 51, 576–580.
-
MARASCO, S., LEE, G., SUMMERHAYES, R. Quality of life after major trauma with multiple rib fractures. Inj. 2015, 46, 61–65.
-
MARASCO, SF., DAVIES, AR., COOPER, J. et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013, 216, 924–932.
-
MICHEK, J., ZELNÍČEK, P., KUBAČÁK, J. et al. Včasné ošetření instabilního hrudníku u polytraumatizovaných. Rozhl Chir. 1996, 75, 202−205.
-
NIRULA, R., MAYBERRY, JC. Rib fracture fixation: controversies and technical challenges. Am Surg. 2010, 76, 793–802.
-
PARÍS, F., TARAZONA, V., BLASCO, E. et al. Surgical stabilization of traumatic flail chest. Thorax. 1975, 30, 521–527.
-
PIERACCI, FM., RODIL, M., STOVALL, RT. Surgical stabilization of severe rib fractures. J Trauma Acute Care Surg. 2015, 78, 883–887.
-
PIERACCI, FM., LIN, Y., RODIL, M. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg. 2016, 80, 187–194.
-
PIERACCI, FM., MAJERCIK, S., ALI-OSMAN, F. Consensus statement: Surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Inj. 2017, 48, 307–321.
-
PIERACCI, FM., COLEMAN, J., ALI-OSMAN, F. A multicenter evaluation of the optimal timing of surgical stabilization of rib fractures. J Trauma Acute Care Surg. 2018, 84, 1–10.
-
SÁNCHEZ-LLORET, J., LETANG, E., MATEU, M. Indications and surgical treatment of the traumatic flail chest syndrome. An original technique. Thorac Cardiovasc Surg. 1982, 30, 294–297.
-
SHORR, RM., RODRIGUES, A., INDECK, MC. Blunt chest trauma in the elderly. J Trauma. 1989, 29, 234–237.
-
SILLAR, R. The crushed chest. Management of the flail anterior segment. J Bone Joint Surg Br. 1961, 43-B, 738–7345.
-
SWART, E., LARATTA, J., SLOBOGEAN, G. et al. Operative Treatment of Rib Fractures in Flail Chest Injuries: A Meta-analysis and Cost-Effectiveness Analysis. J Orthop Trauma. 2017, 31, 64–70.
-
TANAKA, H., YUKIOKA, T., YAMAGUTI, Y. et al. Surgical stabilization or internal pneumatic stabilization? A prospected randomized study of management of severe flail chest patients. J Trauma. 2002, 52, 727–732.
-
UCHIDA, K., NISHIMURA, T., TAKESADA, H. Evaluation of efficacy and indications of surgical fixation for multiple rib fractures: a propensity-score matched analysis. Eur J Trauma Emerg Surg. 2017, 43, 541–547.
-
VÉCSEI, V., FRENZEL, I., PLENK, H. JR. A new rib plate for the stabilization of multiple rib fractures and thoracic wall fracture with paradoxical respiration. Hefte Unfallheilkd. 1979, 138, 279–282.
-
VODICKA, J., SPIDLEN, V., SAFRANEK, J. et al. Severe injury to the chest wall-experience with surgical therapy. Zentralbl Chir. 2007, 132, 542–546.
-
VYHNÁNEK, F., OČADLIK,M., ŠÁBER, M. et al. Inovovaná žeberní dlaha Judetova typu u nestabilního poranění hrudní stěny (první klinické zkušenosti). Úraz chir. 2017, 25, 23–27.
-
VYHNANEK, F., JIRAVA, D., OCADLIK, M. Inovované žeberní dlahy Judetova typu - preklinická studie, první klinické zkušenosti. Acta Chir et Orthop Czechoslov. 2018, 85, 226–230 .
-
WADA,T., YASUNAGA, H., INOKUCHI, R. Effectiveness of surgical rib fixation on prolonged mechanical ventilation in patients with traumatic rib fractures: A propensity score-matched analysis. J Crit Care. 2015, 30, 1227–1231.
-
WIESE, MN., KAWEL-BOEHM, N., MORENO DE LA SANTA, P. et al. Functional results after chest wall stabilization with a new screwless fixation device. Eur J Cardiothorac Surg. 2015, 47, 868–875.
-
WIHLM, JM., GROSDIDIER, G., CHAPELIER, A. Thoracic osteosyntheses for chest wall malformations, traumas and tumors using the STRATOS titanium system: initial experience. Interact CardioVasc Thorac Surg. 2007, 6, 273.
-
WU, WM., YANG, Y., GAO, ZL. Which is better to multiple rib fractures, surgical treatment or conservative treatment? Int J Clin Exp Med. 2015, 8, 7930–7936.
-
XU JQ., QIU, PL., YU, RG. Better short-term efficacy of treating severe flail chest with internal fixation surgery compared with conservative treatments. Eur J Med Res. 2015, 20, 55.
-
ZHANG, X., GUO, Z., ZHAO, C. Management of patients with flail chest by surgical fixation using claw-type titanium plate. J Cardiothorac Surg. 2015, 10, 145.
Štítky
Chirurgie všeobecná Traumatologie Urgentní medicína
Článek vyšel v časopiseÚrazová chirurgie
Nejčtenější tento týden
2017 Číslo 4- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Stillova choroba: vzácné a závažné systémové onemocnění
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Cinitaprid – v Česku nová účinná látka nejen pro léčbu dysmotilitní dyspepsie
-
Všechny články tohoto čísla
- Chirurgická stabilizace hrudní stěny – vývoj metody a současné trendy
- Abdominální kompartment syndrom u polytraumat
- Tupé poranění jater a sleziny v důsledku fraktury distálních žeber
- Zhodnocení střednědobých výsledků operačního řešení zlomenin krčku talu na Klinice úrazové chirurgie Fakultní nemocnice Brno
- Přečetli jsme za Vás
- Úrazová chirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Abdominální kompartment syndrom u polytraumat
- Tupé poranění jater a sleziny v důsledku fraktury distálních žeber
- Chirurgická stabilizace hrudní stěny – vývoj metody a současné trendy
- Zhodnocení střednědobých výsledků operačního řešení zlomenin krčku talu na Klinice úrazové chirurgie Fakultní nemocnice Brno
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



