-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Global services and support for children with developmental delays and disabilities: Bridging research and policy gaps
Pamela Collins and colleagues explain the research and policy approaches needed globally to ensure children with developmental delays and disabilities are fully included in health and education services.
Published in the journal: . PLoS Med 14(9): e32767. doi:10.1371/journal.pmed.1002393
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1002393Summary
Pamela Collins and colleagues explain the research and policy approaches needed globally to ensure children with developmental delays and disabilities are fully included in health and education services.
Summary points
The United Nations Sustainable Development Goals and the UN Convention on the Rights of the Child (CRC) envision an inclusive society in which health and education contribute to the well-being of all. To achieve this vision, children with developmental delays and behavioral, cognitive, mental, and neurological disabilities need greater access to health care, early childhood care and development services, and education.
Improved population-level detection, alongside screening, assessment, and linkage to evidence-based, intersectoral services in the first years of life, can help maximize capabilities and increase the chances of social inclusion for children with developmental delays and disabilities.
Educational programs for children with delays and disabilities whose service delivery structure supports the ability of parents to work should be encouraged so that parents can participate in achieving children’s educational goals while also meeting their financial needs.
Parents and caregivers who receive training in psychosocial interventions and ongoing support can help children with delays and disabilities thrive in family contexts.
Family mental health influences the developmental trajectory of children. Ensuring that parents and caregivers have access to affordable, quality mental health services helps to prevent poor outcomes for children.
Rigorous evaluation, continuous quality improvement, and regular monitoring of the programmatic outcomes of services and policy approaches targeting children and caregivers would inform their implementation and serve to disseminate lessons learned from successful policy and program implementation.
Background
The UN Sustainable Development Goals (SDGs) were formulated based on the principle that people everywhere deserve “equitable and universal access to quality education at all levels, to health care and social protection, where physical, mental and social well-being are assured” [1]. This vision for inclusive healthy societies includes children with developmental delays and cognitive, mental, and neurological disabilities (henceforth developmental delays and disabilities). The UN Convention on the Rights of the Child (CRC) further stipulates that children with disabilities cannot be excluded from free and compulsory primary and secondary education based on their disability [2]. Yet, children with disabilities are more likely to grow up in poverty and to receive less healthcare, early childhood care and development services, and education [3,4]. Caregivers and parents play a central role in facilitating children’s access to early childhood development interventions, including healthcare and education, but must be adequately supported.
Recent analyses highlight the importance of early child development and delineate the conditions that place children at risk for not achieving their developmental potential as well as the interventions and research needed to mitigate this [5–9]. With optimal implementation of existing prevention and care interventions, a subset of children will nevertheless be identified with developmental delays and disabilities of varying severity. Ideally, their caregivers, parents, community structures, and societies can be equipped to accommodate their needs to achieve maximum social inclusion and functioning. This paper identifies research and policy activities that, if implemented, could improve the identification of children with delays and disabilities and the ability of caregivers to help meet their developmental, health, and educational needs. We describe opportunities for research or policy shifts in 5 main areas: identifying children with delays and disabilities, ensuring access to early childhood programs and school programs for children, training and support of parents/caregivers to strengthen their ability to care for their children, supporting caregivers’ ability to work, and ensuring that the mental health needs of caregivers are met.
Identify children with delays and disabilities
The most recent Global Burden of Disease data estimate that in 2015, there were 3.6 million children aged 1–9 years living with autism and more than 15 million living with idiopathic developmental intellectual disability [10]. These are only 2 of many cognitive, emotional, mental, and neurological disabilities. Yet, neither incidence nor prevalence for the full range of childhood delays and disabilities is well established in global data. Rates of cognitive disabilities linked to infections (e.g., pneumonia, meningitis, encephalitis, and HIV), prematurity and stunting, neonatal encephalopathy, hyperbilirubinemia, prenatal iodine and other nutritional deficiencies, and neural tube defects linked to inadequate folic acid are likely higher in low - and middle-income countries (LMICs) than in high-income countries (HICs) given the numbers of children living in poverty and the distribution of these risk factors [11–14]. The accumulation of adversities, beginning before conception and continuing throughout prenatal and early life, can disrupt brain development, attachment, and early learning [5]. Developmental delays become evident in the first year, worsen during early childhood, and continue throughout life [6, 15].
Over the past decade, population-based studies have measured the prevalence of disabilities across several countries. Utilizing a disabilities module within the 2005–2007 Multiple Indicator Cluster Survey (MICS) [16], 1 study found that 20% of children across 16 LMICs screened positive for at least 1 impairment (range 3% to 45%), and 5%, 12.7%, 2.9%, and 6.2% of children screened positive for a cognitive, language, sensory, or motor impairment, respectively [17]. A more recent estimate derived from predictive modelling in 35 LMICs showed that 81 million 3-to-4-year-olds (33% prevalence) had low cognitive or socioemotional development in 2010 [18]. The proportion of under-5 children in LMICs at risk of not attaining their developmental potential because of extreme poverty and stunting remains high at 43% [5].
Accurate identification of a child’s impairment in the first years of life makes reversal or mitigation of adverse effects more likely [19]. Routine screening can be implemented in primary care with high fidelity, low cost, and acceptable levels of burden [20–23]. Provider training increases screening and identification of developmental delays [24, 25]. Proactive case finding using community informants is also a promising approach [26]. When linked with diagnostic assessment and evidence-based interventions, early detection helps to increase the proportion of children who achieve their developmental potential, fulfill their ability to work and contribute [27], are not raised in institutions, and do not need expensive services later in life [28–30]. Ethical care requires that screening be linked to intervention.
Increase access to early childhood programs, schooling, and after-school and out-of-school programs
The benefits of early intervention for children with developmental delays and disabilities, families, and communities have been well documented in HICs [28, 31, 32]. A recent review of studies from LMICs provides evidence of similar positive outcomes with early interventions for at-risk children, although research that examines outcomes for children with established disabilities is limited [33]. Scarce human resources for mental, neurological, or developmental pediatric care can limit access to services in LMICs. Task-sharing approaches that provide abbreviated training to less specialized providers for the delivery of evidence-based screening, care, and support interventions can help bridge the resource gap. Researchers in Pakistan screened a large rural community by distributing written descriptions of developmental disorders that included motivational messages and by administering the Ten Questions Screen for disability using an interactive voice response system [34]. Children who screened positive were eligible to work with a network of families equipped with “family champion volunteers” trained in evidence-based interventions outlined in the WHO Mental Health Gap Action Program’s (mhGAP) intervention guide. Significant results included reduced WHO Disability Assessment Schedule global disability scores, lower parent-reported socioemotional difficulties in children, and no diminution of caregiver well-being. Equally important, the family volunteers engaged in more advocacy for children’s education, healthcare, and community inclusion. In another study, nonspecialist health workers in India and Pakistan were trained to coach parents of children with autism to apply strategies for improving parent–child interactions, with an emphasis on communication [35]. Parents and children showed more synchronous communication, and children initiated more communication with the parent.
Access to education remains a critical intervention for children with delays and disabilities, but disparities in educational opportunity, quality, and outcomes persist [36]. Poorer outcomes are related in part to nonenrolment in school, exclusion from participation in classroom activities, and greater likelihood of school dropout [36]. Yet, children with developmental delays and disabilities and their peers without these conditions benefit when early childhood, school, and out-of-school programs are fully inclusive. Education helps break cycles of poverty, potentially for the child with the delay or disability and for siblings who begin a “caregiver career” rather than attending school [3, 37]. The availability of educational programs year-round during the workday plays a key role in ensuring that children and youth with delays and disabilities have the fullest developmental and educational opportunities in settings far better than institutional care can provide. Such programs increase the likelihood that their parents are able to work, support their families, and lead full lives [3]. Integrated education also serves to educate peers on the needs of children with disabilities and provide pathways for interaction and understanding. Table 1 outlines population - and community-level interventions alongside healthcare interventions that can benefit children with delays and disabilities [38].
Tab. 1. Platforms for interventions for children with developmental delays and disabilities. 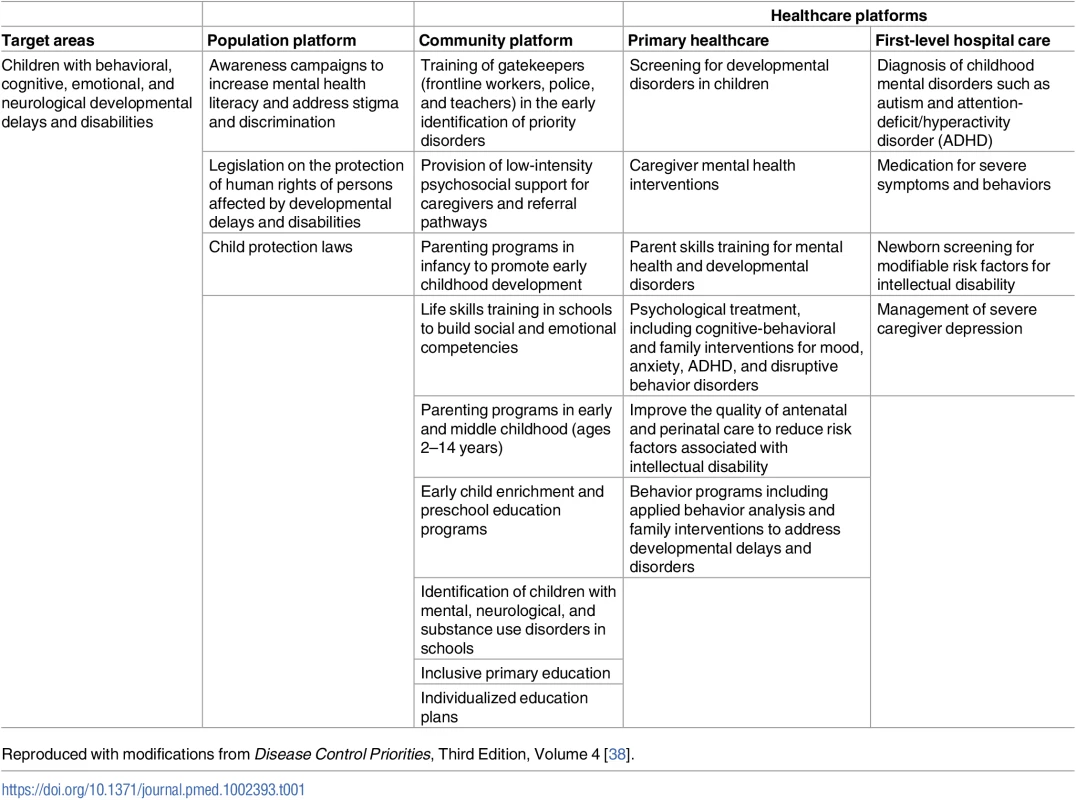
Reproduced with modifications from Disease Control Priorities, Third Edition, Volume 4 [38]. Train and support parents
Children with delays and disabilities can thrive in family contexts, particularly if parents and caregivers receive proper training and ongoing support. Directive parenting, combined with “sensitive, responsive, and reciprocal outcomes” and a stimulating home and community environment, led to favorable developmental outcomes for infants and children with Down syndrome in 1 study [39]. Conversely, a lack of knowledge about their child’s condition and needs, negative feelings, and lack of support adversely affected parent–child interactions, child behavior, and development. If provided with nurturing and supportive family care, children with delays and disabilities have a better chance of leading healthy and full lives, particularly when such care is provided from early in life. Nurturing care has recently been defined as a stable environment that is sensitive to children’s health and nutritional needs, with protection from threats, opportunities for early learning, and interactions that are responsive, emotionally supportive, and developmentally stimulating [40]. As an overarching concept, nurturing care is supported by an ecosystem of social contexts—from home to parental work, child care, schooling, the wider community, and policy influences [41].
Unfortunately, in many cases parents do not have access to specialized training and programs and/or flexibility in their work environment to care for their developmentally delayed or disabled child. In many countries, this results in high numbers of these children being institutionalized at an early age [42]. In Central and Eastern Europe and the Commonwealth of Independent States (CEE/CIS), a child with any type of disability is nearly 17 times more likely to be institutionalized than a child who does not have a disability [43]. When systemic measures to support children with disabilities and their families are encouraged and developed, institutionalization can often be prevented or reversed. With help from the civil sector, from 2009 to 2012, the Government of Moldova closed 18 institutions and reduced by 62% the number of children living in residential care [44]. Efforts like this http://www.openingdoors.eu/wp-content/uploads/2013/05/Facts-and-figures-Moldova-2015.pdf begin with and are sustained by empowering families and caregivers through making existing support programs more inclusive, developing specialized training programs on caring for atypically developing children, and ensuring that all parents of children with disabilities have access to this critical training. The need for services and support to parents to provide nurturing care and the need for training of health workers and nonspecialists have been identified as research priorities [7].
Support the ability of parents to work
Worldwide, families caring for children with disabilities have lower incomes because of constraints on employment [45]. The income needs of families with children with developmental delays and disabilities are on average higher than those of families whose children do not have these conditions because of the costs of services and care [46], which are rarely fully covered by public funds. Studies from LMICs and HICs demonstrate that parental attention to children’s health and involvement in education leads to better outcomes for children [45]. To do this while sustaining financial stability requires access to paid leave; yet, globally, marked disparities in access to paid leave for both parents persist [45]. Parents and caregivers employed in informal work sectors likely have even fewer protections. In the absence of adequate leave, wage loss can be significant [47].
Families benefit if there are quality, affordable developmental and educational programs that are accessible year-round while parents work. Moreover, from a societal perspective, the full inclusion of parents of children with special needs in the workforce contributes markedly to broad social inclusion just as fully integrated classrooms for students do. Monitoring these policies at a country level would provide important groundwork for achieving progress (see Table 2). Families may also need additional support, and the evolving data on cash transfers and psychosocial support are an encouraging pathway [40].
Tab. 2. Policies to support children with developmental delays and disabilities and their caregivers. 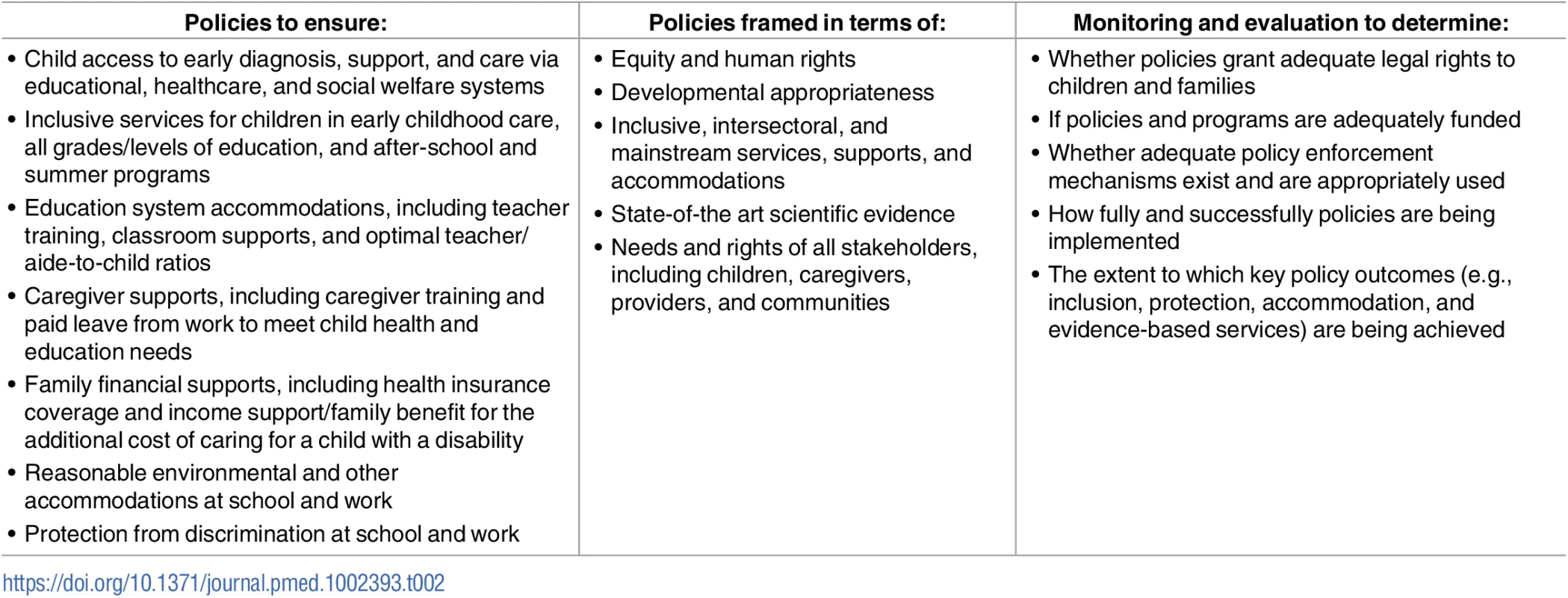
Child access to early diagnosis, support, and care via educational, healthcare, and social welfare systems Treat caregivers with mental health problems
In addition to psychosocial support, the mental health needs of caregivers must be met for them to nurture healthy developmental trajectories in their children. Disabling mental disorders like major depression are prevalent worldwide. The reported prevalence of maternal depression is higher in LMICs (15%–20%) compared to HICs (6%–13%), possibly because of the distribution of social risk factors for maternal depression and the limited healthcare infrastructure and resources for care [48, 49]. Depression limits a mother’s responsiveness to her infant and is associated with inconsistent behavior and less emotional sensitivity to the child [50]. Maternal depression may also lead to early cessation of breastfeeding and undernutrition in the first year of life, lower rates of immunization, higher rates of underweight and stunting [51], and higher rates of childhood illnesses like diarrhea [52]. As compared to children with healthy mothers, infants born to depressed mothers are at a higher risk of poorer long-term cognitive development and delayed motor development; have higher rates of antisocial behavior, hyperactivity, and attention difficulties; and have more frequent emotional problems [48].
There is a growing body of literature indicating that paternal mood also affects child development, and comprehensive provision needs to focus on both parents [53, 54]. Paternal depression is linked to an 8-fold increased likelihood of adverse child–child interactions, with the highest risk of problems with peers among children aged 4–6 years, possibly stemming from negative interactions of depressed fathers with their children [55]. Moreover, parenting children with developmental delays or disabilities can elevate caregivers’ stress, negatively impact quality of life [56, 57], and thus exacerbate the bidirectional adverse effects on both caregiver and child.
Several studies have shown the effectiveness of psychological therapies such as cognitive behavioral therapy and interpersonal therapy in successfully treating and decreasing the symptoms of depression in adults in HICs and LMICs. Where mental health providers are scarce, task shifting is a promising solution to this human resource problem. A meta-analysis of 13 studies that used task shifting to provide psychological therapies aimed at improving parental depression and child health outcomes showed associations between maternal mood and infant health and development as well as positive bidirectional effects of interventions [48, 58]. Across several studies, psychotherapy-based treatments for depressed mothers generally led to improved mother–child bonding, as well as improved language acquisition and fewer externalizing behavior problems in children, but data here are limited [48].
Conclusion
Managing the needs of children with developmental delays and disabilities and meeting their caregivers’ needs require collaboration across the health system as well as intersectoral cooperation (Table 1 [38]). Ideally, detection and screening would occur at all levels. Referrals for care typically involve educational and behavioral health specialists in HICs, but a small and growing evidence base from LMICs shows that families and nonspecialist providers can also be engaged. Crucially, medical providers must be sensitized to the needs of these children to ensure that they receive adequate preventive and curative healthcare alongside behavioral, social, and educational interventions. Care managers (employed in chronic care models) who can support families and facilitate communication among schools, social services, and healthcare personnel would prove valuable for coordinating care and support.
Whether researchers address questions related to the extent of need or the efficacy of programmatic and policy approaches, they must also keep their focus on equity to achieve the SDGs. This requires careful assessment of whether all groups of children and caregivers are being equally well served. When researchers examine policies, programs, and services, it will be essential to map the extent to which different approaches to promoting equal participation and opportunities for children with disabilities and their families are being implemented and are closing equity gaps (Table 3).
Tab. 3. Research gaps for the identification and care of children with developmental delays and disabilities. 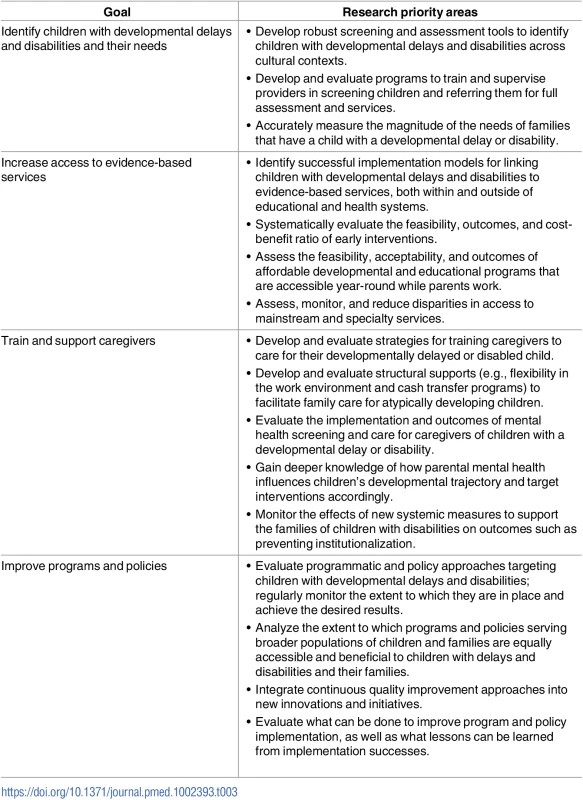
Develop robust screening and assessment tools to identify children with developmental delays and disabilities across cultural contexts. Progress will require regular monitoring and accountability to ensure that leaders who improve their approaches are rewarded, that countries and localities that lag are supported to improve, that toolkits growing out of the most effective solutions are readily available to all countries, and that approaches for accountability are widely disseminated to the public.
Zdroje
1. UN. Transforming our world: The 2030 Agenda for Sustainable Development. United Nations General Assembly, 2015.
2. UN. Convention on the Rights of the Child. New York: United Nations. 1989.
3. UNICEF. Children with Disabilities. New York: United Nations. 2013.
4. Heymann J, McNeill K. Children's Chances: How Countries Can Move from Surviving to Thriving. Boston, MA: Harvard University Press; 2013.
5. Black MM, Walker SP, Fernald LCH, Andersen CT, DiGirolamo AM, Lu C, et al. Early childhood development coming of age: science through the life course. Lancet. 2017; 389(10064):77–90. Epub 2016/10/09. doi: 10.1016/S0140-6736(16)31389-7 27717614
6. Britto PR, Lye SJ, Proulx K, Yousafzai AK, Matthews SG, Vaivada T, et al. Nurturing care: promoting early childhood development. Lancet. 2017;389(10064):91–102. Epub 2016/10/09. doi: 10.1016/S0140-6736(16)31390-3 27717615
7. Dua T, Tomlinson M, Tablante E, Britto P, Yousfzai A, Daelmans B, et al. Global research priorities to accelerate early child development in the sustainable development era. Lancet Global Health. 2016;4(12):e887–e9. Epub 2016/10/09. doi: 10.1016/S2214-109X(16)30218-2 27717631
8. Sharma R, Gaffy MF, Alderman H, Bassani DG, Bogard K, Darmstadt GL, et al. Prioritizing research for integrated implementation of early childhood development and maternal, newborn, child and adolescent health and nutrition platforms. J Glob Health. 2017;7(1): doi: 10.7189/jogh.07.011002 28685048
9. Richter LM, Daelmans B, Lombardi J, Heymann J, Boo FL, Behrman JR, et al. Investing in the foundation of sustainable development: pathways to scale up for early childhood development. Lancet. 2017; 389(10064): 103–18. doi: 10.1016/S0140-6736(16)31698-1 27717610
10. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388(10053): 1545–602. Epub 2016/10/14. doi: 10.1016/S0140-6736(16)31678-6 27733282
11. Bhutani VK, Zipursky A, Blencowe H, Khanna R, Sgro M, Ebbesen F, et al. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels. Pediatr Res. 2013; 74 Suppl 1 : 86–100. doi: 10.1038/pr.2013.208 24366465
12. Blencowe H, Lee AC, Cousens S, Bahalim A, Narwal R, Zhong N, et al. Preterm birth-associated neurodevelopmental impairment estimates at regional and global levels for 2010. Pediatr Res. 2013; 74 Suppl 1 : 17–34. doi: 10.1038/pr.2013.204 24366461
13. Lee AC, Kozuki N, Blencowe H, Vos T, Bahalim A, Darmstadt GL, et al. Intrapartum-related neonatal encephalopathy incidence and impairment at regional and global levels for 2010 with trends from 1990. Pediatr Res. 2013; 74 Suppl 1 : 50–72. doi: 10.1038/pr.2013.206 24366463
14. Seale AC, Blencowe H, Zaidi A, Ganatra H, Syed S, Engmann C, et al. Neonatal severe bacterial infection impairment estimates in South Asia, sub-Saharan Africa, and Latin America for 2010. Pediatr Res. 2013; 74 Suppl 1 : 73–85. doi: 10.1038/pr.2013.207 24366464
15. Walker SP, Wachs TD, Grantham-McGregor S, Black MM, Nelson CA, Huffman SL, et al. Inequality in early childhood: risk and protective factors for early child development. Lancet. 378(9799): 1325–38. doi: 10.1016/S0140-6736(11)60555-2 21944375
16. UNICEF. Multiple indicator cluster survey manual 2005: Monitoring the situation of children and women. New York: Division of Policy and Planning: UNICEF, 2006.
17. Bornstein MH, Hendricks C. Screening for developmental disabilities in developing countries. Soc Sci Med. 2013; 97 : 307–15. doi: 10.1016/j.socscimed.2012.09.049 23294875
18. McCoy DC, Peet ED, Ezzati M, Danaei G, Black MM, Sudfeld CR, et al. Correction: Early Childhood Developmental Status in Low - and Middle-Income Countries: National, Regional, and Global Prevalence Estimates Using Predictive Modelling. PLoS Med. 2017; 14(1):e1002233. Epub 2017/01/31. doi: 10.1371/journal.pmed.1002233 28135271
19. Fischer VJ, Morris J, Martines J. Developmental screening tools: feasibility of use at primary healthcare level in low - and middle-income settings. J Health Popul Nutr. 2014; 32(2): 314–26. Epub 2014/08/01. 25076668
20. Gura GF, Champagne MT, Blood-Siegfried JE. Autism spectrum disorder screening in primary care. J Dev Behav Pediatr. 2011; 32(1): 48–51. doi: 10.1097/DBP.0b013e3182040aea 21160437
21. Hix-Small H, Marks K, Squires J, Nickel R. Impact of implementing developmental screening at 12 and 24 months in a pediatric practice. Pediatrics. 2007; 120(2): 381–9. doi: 10.1542/peds.2006-3583 17671065
22. Miller JS, Gabrielsen T, Villalobos M, Alleman R, Wahmhoff N, Carbone PS, et al. The each child study: systematic screening for autism spectrum disorders in a pediatric setting. Pediatrics. 2011; 127(5): 866–71. doi: 10.1542/peds.2010-0136 21482605
23. Pierce K, Carter C, Weinfeld M, Desmond J, Hazin R, Bjork R, et al. Detecting, studying, and treating autism early: the one-year well-baby check-up approach. J Pediatr. 2011; 159(3): 458–65 e1–6. doi: 10.1016/j.jpeds.2011.02.036 21524759
24. Kobak KA, Stone WL, Ousley OY, Swanson A. Web-based training in early autism screening: results from a pilot study. Telemed J E Health. 2011; 17(8): 640–4. doi: 10.1089/tmj.2011.0029 21939382
25. Schonwald A, Huntington N, Chan E, Risko W, Bridgemohan C. Routine developmental screening implemented in urban primary care settings: more evidence of feasibility and effectiveness. Pediatrics. 2009; 123(2): 660–8. doi: 10.1542/peds.2007-2798 19171635
26. Jordans MJ, Kohrt BA, Luitel NP, Komproe IH, Lund C. Accuracy of proactive case finding for mental disorders by community informants in Nepal. Br J Psychiatry. 2015; 207(6): 501–6. Epub 2015/10/10. doi: 10.1192/bjp.bp.113.141077 26450582
27. Berens AE, Nelson CA. The science of early adversity: is there a role for large institutions in the care of vulnerable children? Lancet. 2015; 386(9991): 388–98. doi: 10.1016/S0140-6736(14)61131-4 25638660
28. Guralnick M. The developmental systems approach to early intervention. 1st ed. Baltimore: Brookes Publishing; 2005.
29. Phillips D, Shonkoff J. From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington, DC: National Academies Press; 2000.
30. Shonkoff J, Meisels S. Handbook of early childhood intervention. Cambridge: Cambridge University Press; 2000.
31. Brown S, Guralnick M. International human rights to early intervention for infants and young children with disabilities: Tools for global advocacy. Infants and Young Children. 2012; 25(4): 270. doi: 10.1097/IYC.0b013e318268fa49 26213446
32. Heymann J. Forgotten families: Ending the growing crisis confronting children and working parents in the global economy. New York: Oxford University Press; 2006.
33. Engle PL, Fernald LC, Alderman H, Behrman J, O'Gara C, Yousafzai A, et al. Strategies for reducing inequalities and improving developmental outcomes for young children in low-income and middle-income countries. Lancet. 2011;378(9799):1339–53. Epub 2011/09/29. doi: 10.1016/S0140-6736(11)60889-1 21944378
34. Hamdani SU, Minhas FA, Iqbal Z, Rahman A. Model for service delivery for developmental disorders in low-income countries. Pediatrics. 2015; 136(6): 1166–72. Epub 2015/11/26. doi: 10.1542/peds.2015-0861 26598452
35. Rahman A, Divan G, Hamdani SU, Vajaratkar V, Taylor C, Leadbitter K, et al. Effectiveness of the parent-mediated intervention for children with autism spectrum disorder in south Asia in India and Pakistan (PASS): a randomised controlled trial. Lancet Psychiatry. 2016; 3(2): 128–36. Epub 2015/12/26. doi: 10.1016/S2215-0366(15)00388-0 26704571
36. UNESCO. Education for All 2000–2015: Achievments and Challenges. Paris: United Nations Educational, Scientific and Cultural Organization; 2015.
37. Raina P, O'Donnell M, Schwellnus H, Rosenbaum P, King G, Brehaut J, et al. Caregiving process and caregiver burden: conceptual models to guide research and practice. BMC Pediatrics. 2004; 4(1): 1. doi: 10.1186/1471-2431-4-1 14723791
38. Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, et al. Global priorities for addressing the burden of mental, neurological, and substance use disorders. In: Patel V, Chisholm D, Dua T, Laxminarayan R, Medina-Mora ME, editors. Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, Third Edition (Volume 4). Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2016.
39. Hooste AV, Maes B. Family factors in the early development of children with Down syndrome. Journal of Early Intervention. 2003; 25(4): 296–309.
40. Britto PR, Lye SJ, Proulx K, Yousafzai AK, Matthews SG, Vaivada T, et al. Nurturing care: promoting early childhood development. Lancet. 2017;389(10064):91–102. Epub 2016/10/09. doi: 10.1016/S0140-6736(16)31390-3 27717615.
41. Shonkoff JP, Phillips DA. From neurons to neighborhoods: the science of early childhood development. Washington, DC: National Academies Press (US); 2000.
42. UNICEF. The right of children with disabilities to education: A rights-based approach to inclusive education. Geneva: UNICEF; 2011.
43. UNICEF. Progress for children: A report card on child protection. 2009.
44. Opening Doors. Opening Doors for Europe's Children: Moldova http://www.openingdoors.eu/wp-content/uploads/2016/12/country-fiche-Moldova-2014.pdf2013 [cited 2/25/2017].
45. Heymann J, McNeill K, Earle A. Filling a critical gap: measuring work policies that affect families globally. Community, Work & Family. 2013; 16(3): 239–60.
46. Robinson LR, Holbrook JR, Bitsko RH, Hartwig SA, Kaminski JW, Ghandour RM, et al. Differences in health care, family, and community factors associated with mental, behavioral, and developmental disorders among children aged 2–8 years in rural and urban areas—United States, 2011–2012. MMWR Surveillance Summaries. 2017;66(8):1–11. Epub 2017/03/17. doi: 10.15585/mmwr.ss6608a1 28301449
47. Earle A, Heymann J. The cost of caregiving: Wage loss among caregivers of elderly and disabled adults and children with special needs. Community, Work & Family. 2012; 15(3): 357–75.
48. Atif N, Lovell K, Rahman A. Maternal mental health: The missing "m" in the global maternal and child health agenda. Semin Perinatol. 2015; 39(5): 345–52. Epub 2015/07/15. doi: 10.1053/j.semperi.2015.06.007 26164538
49. Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. 2014; 384(9956): 1775–88. Epub 2014/12/03. doi: 10.1016/S0140-6736(14)61276-9 25455248
50. Meltzer-Brody S. New insights into perinatal depression: pathogenesis and treatment during pregnancy and postpartum. Dialogues Clin Neurosci. 2011; 13(1): 89–100. Epub 2011/04/14. 21485749
51. Surkan PJ, Kennedy CE, Hurley KM, Black MM. Maternal depression and early childhood growth in developing countries: systematic review and meta-analysis. Bulletin of the World Health Organization. 2011; 89(8): 608–15. Epub 2011/08/13. doi: 10.2471/BLT.11.088187 21836759
52. Rahman A, Surkan PJ, Cayetano CE, Rwagatare P, Dickson KE. Grand challenges: integrating maternal mental health into maternal and child health programmes. PLoS Med. 2013;10(5):e1001442. Epub 2013/05/15. doi: 10.1371/journal.pmed.1001442 23667345
53. Dave S, Petersen I, Sherr L, Nazareth I. Incidence of maternal and paternal depression in primary care: a cohort study using a primary care database. Arch Pediatr Adolesc Med. 2010; 164(11): 1038–44. Epub 2010/09/08. doi: 10.1001/archpediatrics.2010.184 20819960
54. Dave S, Sherr L, Senior R, Nazareth I. Major paternal depression and child consultation for developmental and behavioural problems. British J Gen Pract. 2009; 59(560): 180–5. Epub 2009/03/12. doi: 10.3399/bjgp09X407063 19275834
55. Dave S, Sherr L, Senior R, Nazareth I. Associations between paternal depression and behaviour problems in children of 4–6 years. Eur Child Adolesc Psychiatry. 2008; 17(5): 306–15. Epub 2008/03/28. doi: 10.1007/s00787-007-0672-6 18365134
56. Bhatia MS, Srivastava S, Gautam P, Saha R, Kaur J. Burden assessment, psychiatric morbidity, and their correlates in caregivers of patients with intellectual disability. East Asian Arch Psychiatry. 2015; 25(4): 159–63. Epub 2016/01/15. 26764290. 26764290
57. Estes A, Olson E, Sullivan K, Greenson J, Winter J, Dawson G, et al. Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain Dev. 2013; 35(2): 133–8. Epub 2012/11/14. doi: 10.1016/j.braindev.2012.10.004 23146332
58. Rahman A, Fisher J, Bower P, Luchters S, Tran T, Yasamy MT, et al. Interventions for common perinatal mental disorders in women in low - and middle income countries; a systematic review and meta-analysis. Bull World Health Organ. 2013; 91(8): 593–601. Epub 2013 Apr 18. doi: 10.2471/BLT.12.109819 23940407
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2017 Číslo 9- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
-
Všechny články tohoto čísla
- Self-monitoring of blood pressure in hypertension: A systematic review and individual patient data meta-analysis
- Preterm birth prevention—Time to PROGRESS beyond progesterone
- Women’s and men’s reports of past-year prevalence of intimate partner violence and rape and women’s risk factors for intimate partner violence: A multicountry cross-sectional study in Asia and the Pacific
- Global services and support for children with developmental delays and disabilities: Bridging research and policy gaps
- Risk, treatment duration, and recurrence risk of postpartum affective disorder in women with no prior psychiatric history: A population-based cohort study
- Chronic disease concordance within Indian households: A cross-sectional study
- Sustained effectiveness and cost-effectiveness of Counselling for Alcohol Problems, a brief psychological treatment for harmful drinking in men, delivered by lay counsellors in primary care: 12-month follow-up of a randomised controlled trial
- Effectiveness of food supplements in increasing fat-free tissue accretion in children with moderate acute malnutrition: A randomised 2 × 2 × 3 factorial trial in Burkina Faso
- Sustained effectiveness and cost-effectiveness of the Healthy Activity Programme, a brief psychological treatment for depression delivered by lay counsellors in primary care: 12-month follow-up of a randomised controlled trial
- Vaginal progesterone pessaries for pregnant women with a previous preterm birth to prevent neonatal respiratory distress syndrome (the PROGRESS Study): A multicentre, randomised, placebo-controlled trial
- Oral tetrahydrouridine and decitabine for non-cytotoxic epigenetic gene regulation in sickle cell disease: A randomized phase 1 study
- Cervical screening with primary HPV testing or cytology in a population of women in which those aged 33 years or younger had previously been offered HPV vaccination: Results of the Compass pilot randomised trial
- Keeping it real: A journal editor in clinic
- Impact of common genetic determinants of Hemoglobin A1c on type 2 diabetes risk and diagnosis in ancestrally diverse populations: A transethnic genome-wide meta-analysis
- HbA1c for type 2 diabetes diagnosis in Africans and African Americans: Personalized medicine NOW!
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Effectiveness of food supplements in increasing fat-free tissue accretion in children with moderate acute malnutrition: A randomised 2 × 2 × 3 factorial trial in Burkina Faso
- Oral tetrahydrouridine and decitabine for non-cytotoxic epigenetic gene regulation in sickle cell disease: A randomized phase 1 study
- Keeping it real: A journal editor in clinic
- Sustained effectiveness and cost-effectiveness of Counselling for Alcohol Problems, a brief psychological treatment for harmful drinking in men, delivered by lay counsellors in primary care: 12-month follow-up of a randomised controlled trial
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



