-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaMonitoring and Evaluating Progress towards Universal Health Coverage in Ghana
article has not abstract
Published in the journal: . PLoS Med 11(9): e32767. doi:10.1371/journal.pmed.1001691
Category: Collection Review
doi: https://doi.org/10.1371/journal.pmed.1001691Summary
article has not abstract
This paper is part of the PLOS Universal Health Coverage Collection. This is the summary of the Ghana country case study. The full paper is available as Supporting Information file Text S1.
Background
Since independence in 1957, Ghana has explored sustainable ways of attaining the WHO-defined goal of Health for All. Following transition from a completely government-funded system post-independence, to a full cost recovery, out-of-pocket payment system, the government continues to pursue strategies to increase accessibility to health services.
Universal Health Coverage: The Policy Context
Since 2003, the Government of Ghana has been implementing the National Health Insurance Scheme (NHIS) as the main strategy to progressively bridge financial access barriers and provide a social risk protection system [1]. The scheme complements the Community-based Health Planning and Services program—the national strategy to progressively reduce geographical access barriers to health services [2]. The concurrent strengthening of the District Health Systems will contribute to improving health outcomes.
Monitoring and Evaluation for Universal Health Coverage
Ghana uses an elaborate system of periodic health sector reviews at district, regional, and national levels to assess progress on its sector-wide indicators outlined in its National Health Strategy, in concordance with the objectives of the four-year Health Sector Medium-Term Development Plan. This annual process, led by the ministry of health, organizes a comprehensive review system using a variety of tools such as the Holistic Assessment Tool, feeding into the Interagency Performance Review, and culminating in the National Health Summit.
Routine administrative health service data are enhanced by periodic population-based surveys; Demographic and Health Surveys (DHSs) (conducted every five years beginning in 1988) and Multiple-Indictor Cluster Surveys (MICS) (2006 and 2011) are used to evaluate health service performance emphasizing key health interventions and equity, and progress within wealth quintiles and other stratifiers. National Health Accounts (NHAs) exercises were conducted in 2005 and 2010.
Progress towards Universal Health Coverage in Ghana
While child mortality trends alone are not a good indicator of universal health coverage (UHC) as many factors contribute to intervention coverage, mortality trends nonetheless offer a general measure to assess progress in reducing the gaps. Overall, under-five mortality rates have declined by about one-third since 1990 (MICS 2011 reports 82 deaths per 1,000 live births for 2007–2011, in comparison, Ghana DHS 1988 reports 155 per 1,000). Neonatal mortality rates declined much more slowly, with only a 5% reduction since 2003, while the gaps between the wealthiest and poorest households have widened in recent years.
Coverage has been consistently high for United Nations Millennium Development Goal (MDG)-related interventions although increases have not been significant (Figure 1). Survey data indicate wide disparities in skilled attendant coverage by household wealth status. Only limited data are available on coverage for non-communicable disease interventions.
Fig. 1. Trends in selected coverage indicators 2010–2012 (health facility data). 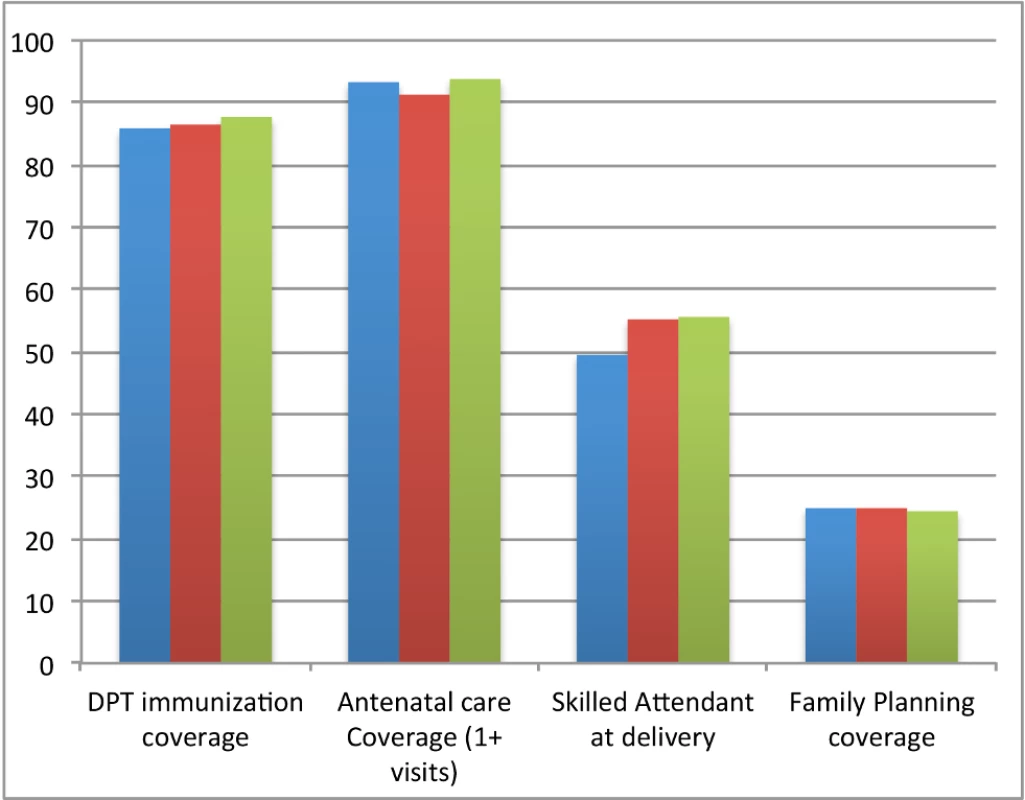
Immunization rates are high, but skilled birth attendance and family planning coverage are still low and do not appear to be increasing. All coverages are in percentages (%). Blue, 2010; red, 2011; green, year 2012. Inequalities in health worker distribution are significant, with little improvement in doctor-to-population ratio. There are 11-times fewer doctors per population in the Upper West Region in comparison to the Greater Accra Region, the latter representing approximately 50% of all Ghana's doctors [3].
Current national per capita expenditure on health is about 10% of the total national budget. Increments in health expenditure have not matched growth in the size of national income. Total health expenditure as a percentage of GDP fell from 6.4 to 3.3 from 2005 to 2010 [4],[5].
NHIS coverage in 2012 was 34% of the population compared to the target of 70%. Designed to be pro-poor, membership on NHIS favors the middle-wealth quintiles [6]. Out-of-pocket health expenditure remained the same at just under 30% of total health expenditure [4].
Conclusions and Recommendations
To achieve UHC, increases in health sector resources should correspond to targeted investments in preventative, curative services and community-based care. The impediment to achieving UHC are two-fold: First, the poorly understood concept of cost containment in UHC and second, no mechanism for determining the basic package of services and how these reflect population needs over time.
In-country monitoring mechanisms and relevant evaluation tools are inadequate. There are significant gaps in quantifying equity and financial risk protection among different wealth quintiles, and in addressing the spread and control of non-communicable diseases and other chronic conditions.
Institutionalizing the National Health Accounts will provide a useful means for comparisons between investments and health outcomes.
With expected progress on expansion of pro-poor strategies, there is an urgent need to synergize both national strategies to achieve UHC and its desired impact. Expanding health insurance coverage to enhance quality care is key to the goal of UHC, and implementation within the current primary health care system will ensure that the lowest quintiles are not excluded.
National monitoring and evaluation frameworks should incorporate relevant global-level indicators that define and track country effective coverage for meaningful comparisons among countries of similar socio-economic and demographic characteristics.
Supporting Information
Zdroje
1. MillsA, AtagubaJE, AkaziliJ, BorghiJ, GarshongB, et al. (2012) Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage. Lancet 380 : 126–133.
2. NyonatorFK, Awoonor-WilliamsJK, PhillipsJF, JonesTC, MillerRA (2005) The Ghana community-based health planning and services initiative for scaling up service delivery innovation. Health Policy Plann 20 : 25–34.
3. Ministry of Health (2012) Holistic assessment of the health sector programme of work. Available: http://www.mohghana.org/UploadFiles/Publications/2012%20Holistic%20Assessment%20Report%20ofoe130715062103.pdf. Accessed 17 October 2013.
4. (2010) Report on the National Health Accounts 2005.
5. (2012) National Health Insurance Authority 2012 Annual Report.
6. Jehu-AppiahC, AryeeteyG, SpaanaE, de HoopT, AgyepongI, et al. (2011) Equity aspects of the National Health Insurance Scheme in Ghana: who is enrolling, who is not and why? Soc Sci Med 72 : 157e–165e.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2014 Číslo 9- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
-
Všechny články tohoto čísla
- Monitoring and Evaluating Progress towards Universal Health Coverage in Ghana
- Sorting Reality from What We Think We Know About Breast Cancer in Africa
- The PLOS “Monitoring Universal Health Coverage” Collection: Managing Expectations
- Monitoring and Evaluating Progress towards Universal Health Coverage in India
- Monitoring and Evaluating Progress towards Universal Health Coverage in Tanzania
- Monitoring and Evaluating Progress towards Universal Health Coverage in Brazil
- Monitoring and Evaluating Progress towards Universal Health Coverage in Thailand
- Monitoring and Evaluating Progress towards Universal Health Coverage in Estonia
- Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
- Prioritizing Pregnant Women for Long-Lasting Insecticide Treated Nets through Antenatal Care Clinics
- Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges
- Convergence of Mortality Rates among Patients on Antiretroviral Therapy in South Africa and North America
- Malaria Prevention during Pregnancy—Is There a Next Step Forward?
- Beyond UHC: Monitoring Health and Social Protection Coverage in the Context of Tuberculosis Care and Prevention
- Intimate Partner Violence and Reproductive Coercion: Global Barriers to Women's Reproductive Control
- Genetic Predisposition to Increased Blood Cholesterol and Triglyceride Lipid Levels and Risk of Alzheimer Disease: A Mendelian Randomization Analysis
- Readmissions after Hospitalization for Heart Failure, Acute Myocardial Infarction, or Pneumonia among Young and Middle-Aged Adults: A Retrospective Observational Cohort Study
- Intermittent Preventive Treatment of Malaria in Pregnancy with Mefloquine in HIV-Infected Women Receiving Cotrimoxazole Prophylaxis: A Multicenter Randomized Placebo-Controlled Trial
- Equity-Oriented Monitoring in the Context of Universal Health Coverage
- The Clinical and Economic Impact of Point-of-Care CD4 Testing in Mozambique and Other Resource-Limited Settings: A Cost-Effectiveness Analysis
- Effective Coverage: A Metric for Monitoring Universal Health Coverage
- Mortality in Patients with HIV-1 Infection Starting Antiretroviral Therapy in South Africa, Europe, or North America: A Collaborative Analysis of Prospective Studies
- Global Financing and Long-Term Technical Assistance for Multidrug-Resistant Tuberculosis: Scaling Up Access to Treatment
- Oral Cholera Vaccine Development and Use in Vietnam
- Monitoring and Evaluating Progress towards Universal Health Coverage in Bangladesh
- Monitoring and Evaluating Progress towards Universal Health Coverage in South Africa
- Monitoring and Evaluating Progress towards Universal Health Coverage in Ethiopia
- Preventing Acute Malnutrition in Young Children: Improving the Evidence for Current and Future Practice
- Monitoring and Evaluating Progress towards Universal Health Coverage in Singapore
- Monitoring and Evaluating Progress towards Universal Health Coverage in China
- Monitoring and Evaluating Progress towards Universal Health Coverage in Tunisia
- Receptor-Defined Subtypes of Breast Cancer in Indigenous Populations in Africa: A Systematic Review and Meta-Analysis
- WHO Essential Medicines Policies and Use in Developing and Transitional Countries: An Analysis of Reported Policy Implementation and Medicines Use Surveys
- Intermittent Preventive Treatment of Malaria in Pregnancy with Mefloquine in HIV-Negative Women: A Multicentre Randomized Controlled Trial
- Preventing Acute Malnutrition among Young Children in Crises: A Prospective Intervention Study in Niger
- Monitoring Progress towards Universal Health Coverage at Country and Global Levels
- Monitoring Intervention Coverage in the Context of Universal Health Coverage
- Regular Breakfast Consumption and Type 2 Diabetes Risk Markers in 9- to 10-Year-Old Children in the Child Heart and Health Study in England (CHASE): A Cross-Sectional Analysis
- Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study
- Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
- Malaria Prevention during Pregnancy—Is There a Next Step Forward?
- Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



