-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Household Air Pollution in Low- and Middle-Income Countries: Health Risks and Research Priorities
article has not abstract
Published in the journal: . PLoS Med 10(6): e32767. doi:10.1371/journal.pmed.1001455
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001455Summary
article has not abstract
Summary Points
-
Household air pollution (HAP) from solid fuel (biomass or coal) combustion is the leading environmental cause of death and disability in the world.
-
Many governments, multinational companies and nongovernmental organizations are developing programs to promote access to improved stoves and clean fuels, but there is little demonstrated evidence of health benefits from most of these programs or technologies.
-
A stakeholder meeting hosted by U.S. government sponsors identified research gaps and priorities related to the health effects of HAP and unsafe stoves in seven areas (cancer; infections; cardiovascular disease; maternal, neonatal, and child health; respiratory disease; burns; and ocular disorders) and gaps in four cross-cutting areas that are relevant to research on HAP (exposure and biomarker assessment, women's empowerment, behavioral approaches, and program evaluation).
-
It is vital that researchers partner with implementing organizations and governments to evaluate the impacts of improved stove and fuel programs to identify and share evidence regarding the outcomes of the many implementation programs underway, including the socio-behavioral aspects of household energy use.
Introduction
Household air pollution (HAP), which results from incomplete combustion of the solid fuels traditionally used for cooking and heating, affects the homes of nearly 3 billion people. It is the leading environmental cause of death and disability worldwide, with highest risks for women and children due to their domestic roles [1]. The high levels of pollutants found in HAP cause a range of diseases [1], in addition to burns and scalds [2] and injuries or violence experienced during fuel collection [3]. Additionally, household solid fuel use can pose substantive environmental risks, including degradation from fuel gathering as well as climate change from release of both CO2 and short-lived climate forcers, such as black carbon, during combustion [4]. Despite the broad support to find solutions, only a few solid fuel interventions have shown that they might improve health over the long term [5]–[7], especially when implemented at the scale required (Box 1).
Box 1. Finding Household Energy Solutions—The Context
To be successful, efforts to introduce improved stoves and fuels must take into account the scale of the problem as well as the complex social, environmental, and economic context of HAP:
-
Scale of the problem: Nearly 3 billion people use unsafe and inefficient traditional stoves and fuels for cooking and heating.
-
Gender - and age-specific risks: Women and children have the greatest exposures to HAP and unsafe stoves but may be constrained by cultural and gender-related factors to change their household exposures and risks with fuel-gathering.
-
Cultural contexts: Traditional methods of cooking and heating have been used for many generations and are adapted to local dietary, environmental, and cultural needs.
-
Environmental risks: Household fuel combustion contributes to outdoor air pollution and climate change and, in some regions, fuel-gathering for inefficient stoves contributes to environmental degradation, including deforestation and desertification.
-
Poverty: Solid fuel use is closely linked to poverty both within and between countries, and clean cooking technologies must be affordable and desirable to families with limited and often insecure incomes to provide sustainable solutions.
Using data from 2004, the World Health Organization (WHO) estimated that nearly 2 million premature HAP-related deaths occurred from acute lower respiratory infections (ALRI) in young children, chronic obstructive pulmonary disease (COPD), and lung cancer [8]. The recent Global Burden of Disease 2010 update by the Institute for Health Metrics and Evaluation nearly doubles the estimated mortality to 3.5 million (4 million including HAP's contribution to 16% of outdoor air pollution deaths), due to the inclusion of HAP deaths from cardiovascular disease and lung cancer from biomass smoke [1]. Prenatal exposure to HAP is linked to the increased risk of stillbirth, low birth weight [9], and impaired cognitive development [10], and direct HAP exposure is linked to cataracts [11] and possibly trachoma [12],[13].
In line with the United Nations (UN)-led initiative, Sustainable Energy for All (SEFA)—an ambitious campaign to bring modern energy to every home by 2030 [14] — governments, multinational companies and nongovernmental organizations (NGO) are increasing investments in programs to promote access to improved stoves and clean fuels that could mitigate these harmful effects. Much of this effort is facilitated by the United Nations Foundation's Global Alliance for Clean Cookstoves (Alliance) [15], which has the goal that 100 million homes adopt clean stoves and fuels by 2020. Furthermore, agreement on a set of voluntary, tiered standards for stove performance [16] and new WHO indoor air pollution guidelines for household fuel combustion expected to be published in 2013 [17] will allow consumers and those implementing these efforts to know, for the first time, the emissions and potential health impacts of a given stove. Because momentum to improve stoves and household air quality is growing rapidly, evaluation of the impact of household energy interventions on health is both urgent and essential [18].
Programs to introduce clean cookstoves cannot simply assume that these so-called improved stoves will be accepted by the household or that they will benefit health. Forgoing a thorough evaluation during the initial stages of implementation and scale-up, particularly of the stove's acceptability and performance in everyday use, carries the risk that implementation will not improve health [19]. In addition, preliminary exposure–response results from the recent RESPIRE trial suggest that stoves must significantly reduce exposures (by at least 50%) to substantially improve health [20]. If this finding is replicated in future studies, the daunting task ahead is to facilitate access to cleaner-burning stoves and fuels that are affordable, acceptable to families, and scalable to hundreds of millions of households.
This report results from an international meeting of experts in research, technology, and development, hosted by the National Institutes of Health (NIH) and other U.S. government partners, that led to a proposed research agenda to address the gaps in the current evidence on the health effects of HAP and unsafe stoves and the identification of critical considerations for effective implementation (Box 2). The imminent scale-up of stove and fuel improvement programs offers a great opportunity for health researchers to work with program implementers. Failure to do so risks introducing new cooking technologies to millions of homes without understanding whether the intended health benefits are realized—or worse, whether there are unintended adverse consequences.
Box 2. Process for Developing HAP Health Research Recommendations
Participants
The recommendations presented in this report result from a workshop involving 139 participants (See Supplement S1 for agenda and participant list):
-
Participants were from 15 nations
-
Participants included 8 members of the expert group on HAP for the new Global Burden of Disease project comparative risk assessment 2010 update [1],[48]
Topics
Working groups examined:
-
A set of health outcomes
-
Cancer
-
Infections
-
Cardiovascular disease
-
Maternal, neonatal, and child health
-
Respiratory disease
-
Burns
-
Ocular disorders
-
-
A set of cross-cutting considerations for health research on improved stoves and fuels
-
Exposure and biomarker assessment
-
Women's empowerment
-
Behavioral approaches
-
Program evaluation
-
-
Health research strategies needed to fill knowledge gaps
Process
For each of the above topics, working groups identified health research gaps and crafted recommendations through group consensus via the following process:
-
Pre-workshop: Drafted 10 white papers. Drafts drew on:
-
Published systematic reviews (where available)
-
Additional recent primary publications identified through PubMed and ISI Web of Knowledge, references from identified papers, and working group members' knowledge of other published and unpublished studies
-
-
During workshop: Further developed white papers.
-
Ten topic-specific working groups further developed the white papers
-
Working groups presented white papers in plenary sessions for further input
-
-
Post-workshop: Drafted current paper as a result of a writing workshop with authors in October 2011. The organizing committee and working groups selected the authors by consensus to provide this summary report.
Findings
We identified gaps in research relating to the health effects of unsafe stoves and fuels in seven disease areas (Table 1) and several cross-cutting considerations for all research on improved stoves and fuels (Table 2).
Tab. 1. Summary of major research gaps and needs for evidence on health outcomes. 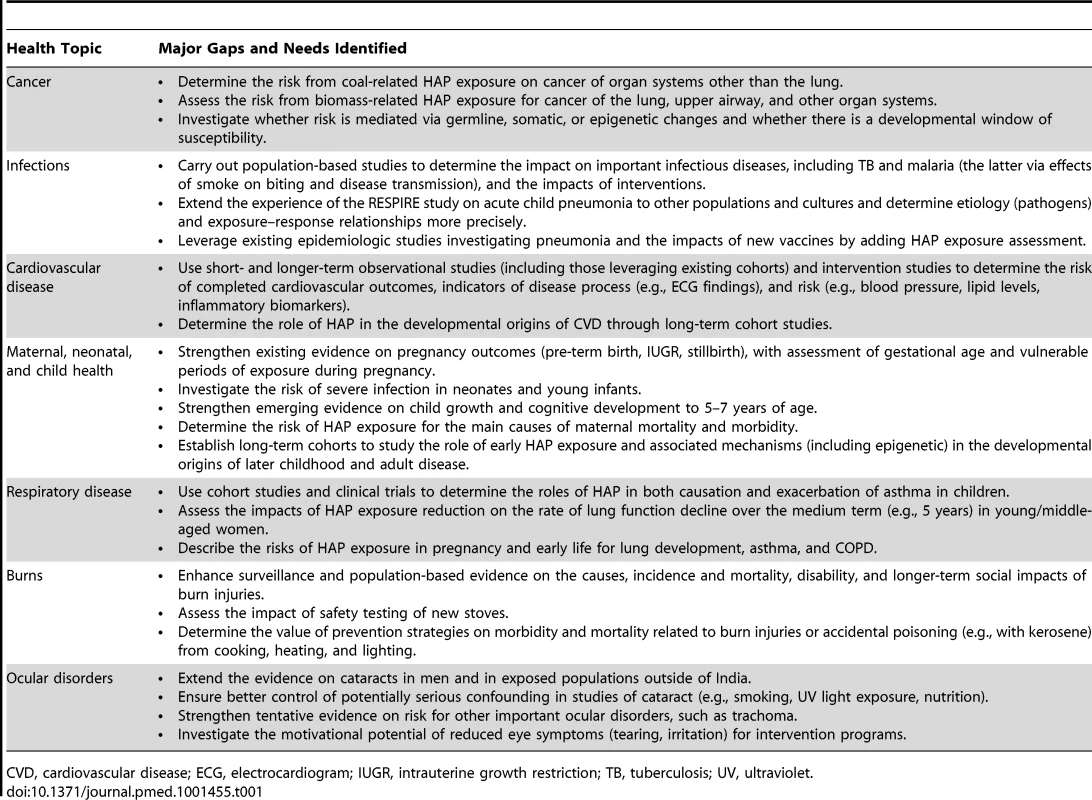
CVD, cardiovascular disease; ECG, electrocardiogram; IUGR, intrauterine growth restriction; TB, tuberculosis; UV, ultraviolet. Tab. 2. Summary of major gaps and research needs for cross-cutting issues. 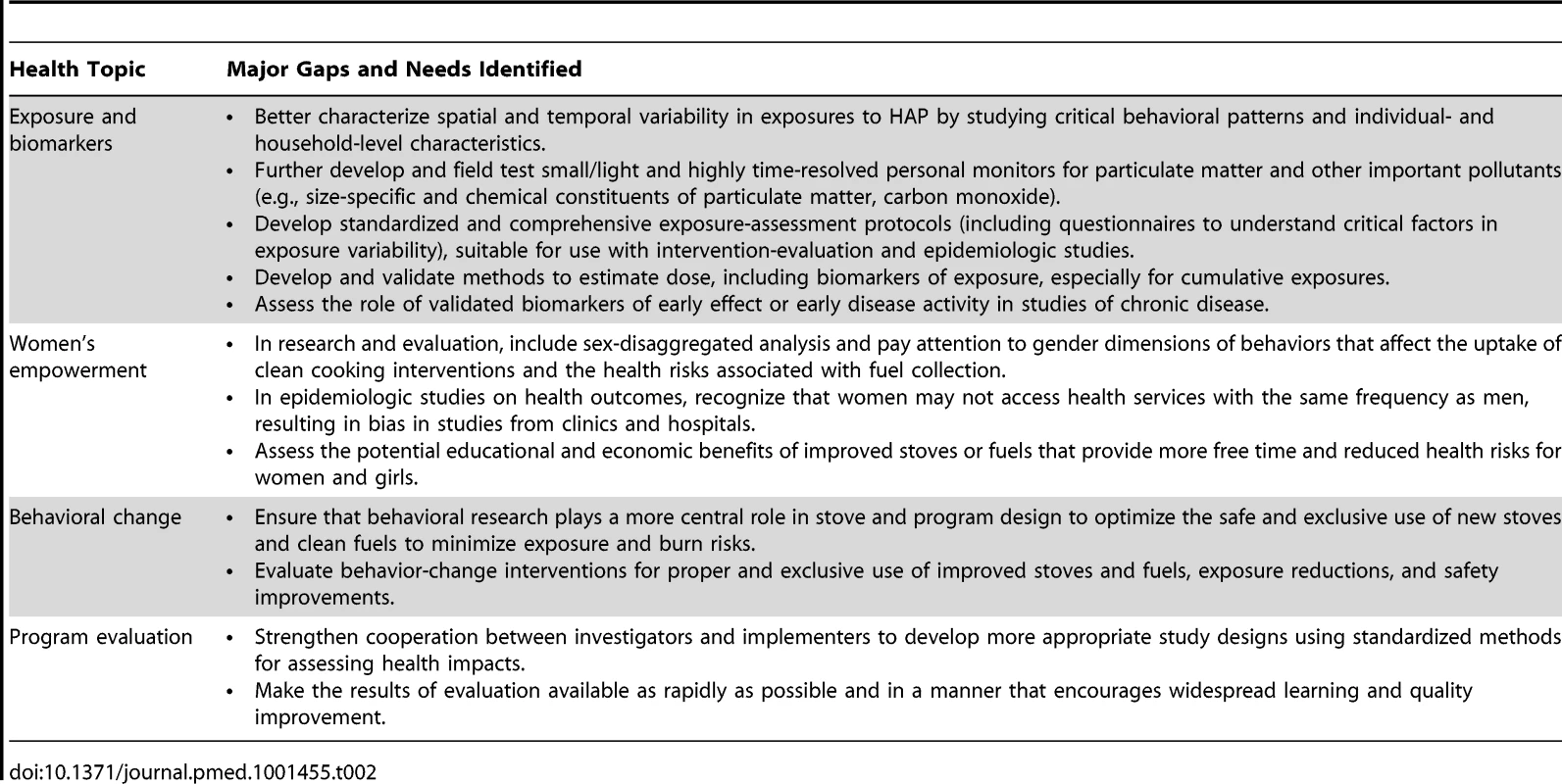
Key Gaps in Health Research
Among the research gaps presented in Table 1, those relating to the highest burden (e.g., cardiovascular disease, child pneumonia) and outcomes linked to child survival and development are likely to have the most impact on generating awareness of the problem and in mobilizing international mitigation efforts and funding. The impact of HAP exposure during pregnancy and early infancy on the development of disease in later life is another emerging, high-priority topic, as is the prevention of burns, scalds, and poisoning, which has received far too little attention in the past. Nevertheless, securing strong and consistent evidence of the impact of HAP on other conditions, such as tuberculosis and eye diseases, e.g., cataracts, would not only extend the overall evidence and attributable disease burden linked to HAP exposure, but also have important implications for strategic priorities in the respective control programs. (The priorities outlined in Table 1 are further developed and available for review as part of the Roadmap Recommendations of the Alliance's Health Working Group [21].)
Cross-cutting Considerations for Research
Exposure and Biomarker Assessment
Exposure assessment must account for a complex set of factors (Figure 1) that result in large variations in actual exposure and dose through time, between individuals, and among settings. Exposure assessments used in cookstove studies have tended to use simple, often categorical or qualitative measures [22]–[25]. Because these measures cannot account for the high degree of uncertainty and variability in HAP exposures [26],[27], studies using these measures are limited in their ability to elucidate dose–response curves and to detect changes in health outcomes associated with differences in exposure with sufficient statistical power. Greater investment is needed to enhance the sophistication of exposure assessments, including more frequent and numerous samples and more rigorous characterization of the factors that influence exposure variability. Because the factors driving spatial and temporal variability are not identical across different locations, studies need to include the collection of relevant data for exposure variability and uncertainty for their study context, using consistent and compatible protocols, survey tools, and instrumentation.
Fig. 1. HAP in urban and rural settings with examples of other confounding sources of pollutants. 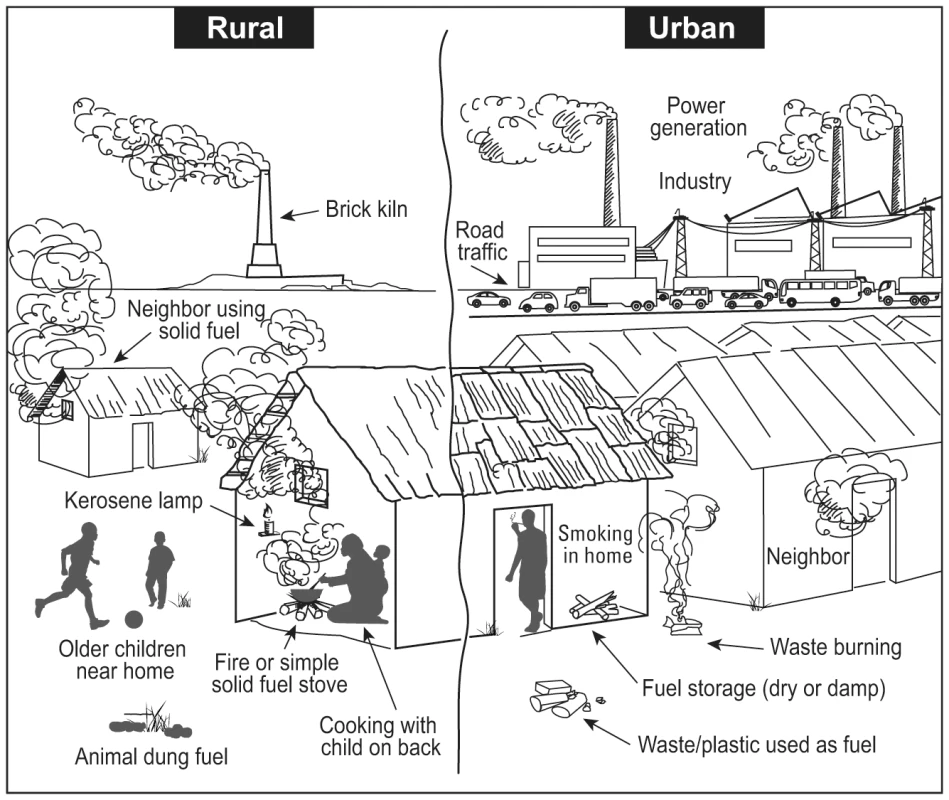
Multiple factors influencing household air pollution and personal exposure levels need to be considered for effective measurement of exposure in health research and evaluation studies, which will differ in urban vs. rural settings and may vary based on cultural practices, geography, and elevation. Each site of HAP must be carefully assessed for other potential sources of products of incomplete combustion that may confound household or personal monitoring of exposure. Biomarkers (e.g., carboxyhemoglobin, polycyclic aromatic hydrocarbon urine metabolites, isoprostane [28], and lung macrophage carbon loading [29],[30]) have been employed to assess human doses, especially for short-term exposures. Affordable biomarkers that are validated to accurately reflect medium - to longer term exposure and are scalable for applications in both health research and program evaluation are a priority research need. Research may seek to extend knowledge on the potential application and usefulness of currently recognized biomarkers or develop and test new biomarkers. Biomarkers of effect and early stages of disease can also play a role in cookstove health studies, especially for chronic, latent health effects, for which these biomarkers may prove especially useful.
Women's Empowerment
Women and girls in developing countries are usually responsible for cooking and fuel-gathering and thus experience the greatest exposures and HAP-related elevations of risk. Due to poverty and the perception of low opportunity costs for time spent fuel-gathering and cooking with inefficient stoves, women may be constrained in their ability to change this situation [31],[32]. In addition to the health risks from HAP exposure and burns, women and girls face hazards during fuel-gathering, including violence and injuries [3], and spend long hours at this task that may reduce engagement in educational or economic activities [33]. Future research must assess both the gender-specific risks of traditional stoves and fuels and the putative benefits of their improvement.
Behavioral Approaches
Human behavior is critical to adopting clean, safe stoves and fuels, using them properly, and improving health outcomes. Behavioral research can determine the best ways to influence the attitudes and beliefs relevant to adopting and maintaining new stoves and fuels, identify the positive features of improved stoves—such as fuel savings—that promote adoption and sustained use, assist in the design of interventions, help ensure proper use of new technology, and improve the home environment [34]. Although research in this area is limited, behavioral changes have been proposed to reduce risks to children [35]. Additionally, evidence-based strategies to change behavior relating to water and sanitation [36] may be adaptable to reduce HAP exposure [33].
Program Evaluation
Household energy interventions are “complex”, involving new technologies and fuels, promotion of behavioral changes, and institutional factors, including product supply and financing, all of which might be implemented through combinations of markets, governments, and NGOs. Not surprisingly, evaluation of intervention programs is far from straightforward. Various evaluation methods should be used to inform program design; examine whether stoves are adopted, used, and maintained; determine whether anticipated exposure reduction and consequent health benefits are realized; examine costs relative to benefits; and determine the reasons for a program's results.
Program evaluation that includes the measurement of impacts on health outcomes is needed to demonstrate the effectiveness of interventions at scale, but it will be resource-intensive. Consequently, such evaluation must be carefully planned to provide evidence on a relatively small but representative number of intervention types and settings. As measurement of exposure and biomarkers improves and exposure–response evidence is strengthened, these tools should provide a simpler, cheaper means of estimating health impacts on a large scale, as a complement but not a substitute for the direct measurement of health outcomes in some studies.
Because randomized controlled trials are difficult to implement in programmatic situations (especially where market-driven), program-appropriate evaluation designs capable of providing robust evidence are needed. Evaluators must overcome practical challenges, such as building political support for evaluation, balancing competing pressures, and managing the expectations of multiple stakeholders [37].
Research Strategies
Three interrelated approaches are needed to address these research and evaluation priorities. The first approach is to focus research over 5 to 10 years on (i) establishing and quantifying risk where this is unknown or still uncertain and elucidating the mechanisms by which HAP results in disease; and (ii) strengthening and extending the description of exposure–response functions for some of the high-burden outcomes. Intervention-based research over this timeframe will be restricted to diseases with relatively short time intervals between exposure and effect, exacerbation of chronic disease, or markers of longer term disease development. Retrospective observational designs (e.g., case-control studies) can be used to investigate risk for established chronic disease over a short time frame, but not as a result of an intervention (examples in Table 3).
Tab. 3. Approaches and key study designs required to address research and evaluation priorities. 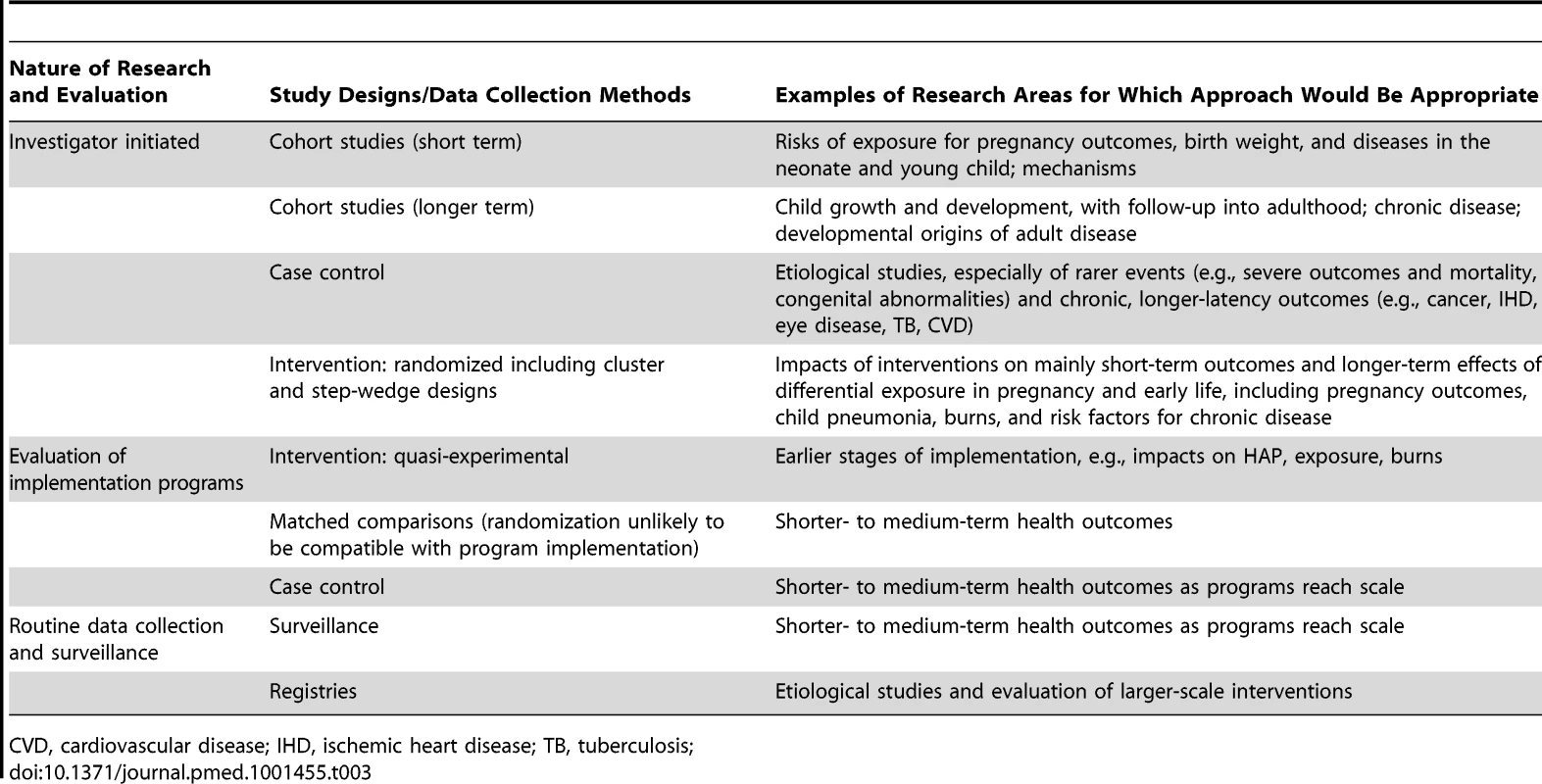
CVD, cardiovascular disease; IHD, ischemic heart disease; TB, tuberculosis; The second approach is to monitor longitudinal cohorts over longer periods and to assess the risks of HAP exposure on the development of chronic diseases. A range of study designs will be required over varying time scales (Table 3), and existing investments such as birth cohort studies [38] and large-scale intervention programs can be leveraged to support these long-term analyses.
The third strategy involves evaluating health impacts from large-scale introductions of improved stoves or fuels in real-world settings, using either randomized or non-randomized designs (Table 3). Because the rapid evolution of clean cookstove technology may result in replacement of an outdated stove in the middle of a long-term study, the success of such research will depend on stable, pre-defined standards for measuring pollution in the household environment and biomarkers in household members. This third approach is the most challenging as it requires commitment of partners that may have very different agendas. Evaluation will be greatly facilitated by cooperation with the programs concerned, but must be independent and avoid any conflicts of interest.
Discussion
Now is a unique opportunity in time to determine key factors that can sustainably reduce exposure to HAP and improve health in low - and middle-income countries. To achieve synergy with the converging commitments of governments, funders, NGOs, and stove manufacturers to implement clean cooking solutions, research and evaluation must focus on priority areas (Tables 1 and 2), which include: (1) strengthening evidence across a range of health outcomes; (2) scalable applications of exposure monitoring and use of biomarkers; and (3) determinants of successful implementation programs, including socio-behavioral aspects of household energy use. Also included must be an awareness of and additional focus on those with the highest exposures: women and young children. The goal is the coordinated and timely use of research and evaluation to inform and, when needed, modify implementation programs to provide the best chance to help the most people in the shortest time possible.
Lessons from the Past
The field of public health is littered with examples of failed interventions designed to improve human health [39]. Primary among these are those interventions that require substantial changes in human behavior to be successful [36]. Unless households adopt and use cleaner stoves and fuels that are capable of delivering sufficient exposure reductions, their health benefits will not be realized. Many factors influence adoption of clean energy solutions, which, at the household and community levels, include whether: (1) they are affordable and desirable to families, (2) women have decision-making influence, and (3) there is community involvement and support at the beginning of the intervention [33].
Despite the best intentions, interventions to improve health may not only be unsuccessful, but may have unintended, catastrophic consequences. An example is the wells installed in south Asia to provide access to clean groundwater and prevent the spread of cholera; they did not prevent cholera but did lead to widespread arsenic poisoning [40]. Improving indoor air quality is not likely to have such striking adverse impacts, as compliance with air quality standards has provided tremendous public health benefits [41]. It is commonly believed in malaria-endemic areas that indoor smoke wards off mosquitoes and could therefore reduce malaria transmission. Biran et al. notes, however, that while smoke may reduce bites, there is no evidence that cleaner indoor air promotes malaria [42]. Nonetheless, the message is clear: Independent evaluation of implementation programs not only provides the opportunity to confirm whether the primary program goals are realized; it also permits assessment of unexpected co-benefits or adverse outcomes.
The challenge is to develop a forum for implementers and investigators to share their perspectives and goals in a way that permits independent evaluation of the programs' health impacts and allows evaluators to propose modifications to improve outcomes.
Design Challenges for New Research
Three unique challenges will be inherent to HAP studies. First, the proposed improved stove or fuel intervention must achieve a large and sustainable reduction in HAP [20]. Second, each household must be willing to (more or less) exclusively use the new improved stove or fuel, as shared use of the new and traditional stoves, or “fuel stacking”, is common [31] and is unlikely to result in sufficient reduction in exposure [43]. Studies must objectively assess stove use in practice, by using electronic devices such as “stove use monitors” (SUMs) [44], and conducting qualitative research to understand preferences and choices. Third, study budgets must adequately support thorough exposure measurement to ensure sustained reductions occur and to quantify exposure–response relationships.
Building Capacity for New Investigators
Training and sharing of experience will help to effectively overcome these challenges. Furthermore, considering the range of research priorities and the pressing requirement for thorough program evaluation, new, multidisciplinary investigator teams will be essential. A small number of training sites already exist in host countries [45], while others are managed by NGOs [46]. In 2012, the Alliance announced its first RFA for health research related to HAP and child survival [47], which emphasizes strengthening of local capacity. Also in 2012, the NIH funded 14 competitive awards to supplement NIH grantees and hosted its first HAP training workshop for investigators. Despite these encouraging developments, substantial new investment will be necessary to build the capacity to carry out this research and evaluation agenda.
Conclusions
Although nearly 3 billion of the world's poorest people still rely on household fuels and stoves that have changed little from prehistoric times, the international community is at last showing signs of a meaningful response. Major implementation programs are already underway to meet the Alliance's 100 million 2020 goal and the UN SEFA target of universal access by 2030. However, research and evaluation must be part of this global effort. It cannot simply be assumed that current efforts to encourage adoption of cleaner and more fuel-efficient stoves and fuels will deliver large health benefits. To secure these gains, programs require evidence-based technology and delivery mechanisms and robust, well-resourced, transparent, and timely evaluation. This report identifies research priorities for global efforts to implement effective clean cooking solutions, with important implications for disease control programs, exposure measurement and biomarker validation, behavioral considerations for effective adoption, and program evaluation. Well-planned investment, complemented by cooperation between the research and implementation communities on research, evaluation, and training, can fill these gaps and make an important contribution to improving health. The recent developments in energy access, described in the Introduction, provide the field with its first opportunity to mobilize and coordinate existing efforts by integrating research and training with practical solutions across various sectors to improve health and quality of life for millions, especially women and children living in poverty. Quickly demonstrating the beneficial health impacts of clean stoves in multiple settings could ensure the successful scale-up and funding of this critical health program.
Supporting Information
Zdroje
1. LimSS, VosT, FlaxmanAD, DanaeiG, ShibuyaK, et al. (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 : 2224–2260.
2. PeckMD, KrugerGE, van der MerweAE, GodakumburaW, AhujaRB (2008) Burns and fires from non-electric domestic appliances in low and middle income countries Part I. The scope of the problem. Burns 34 : 303–311.
3. Women's Commission for Refugee Women and Children (2006) Beyond firewood: Fuel alternatives and protection strategies for displaced women and girls. 122 East 42nd Street, New York, NY 10168-1289: Women's Commission for Refugee Women and Children.
4. UNEP (2011) Near-term climate protection and clean air benefits: actions for controlling short-lived climate forcers. A UNEP synthesis report. Nairobi: UNEP.
5. ChapmanRS, HeX, BlairAE, LamQ (2005) Improvement in household stoves and risk of chronic obstructive pulmonary disease in Xuanwei, China: retrospective cohort study. BMJ 331 : 1050.
6. LanQ, ChapmanRS, SchreinemachersDM, TianL, HeX (2002) Household stove improvement and risk of lung cancer in Xuanwei, China. JNCI J Natl Cancer Inst 94 : 826–835.
7. ShenM, ChapmanRS, VermeulenR, TianL, ZhengT, et al. (2009) Coal use, stove improvement, and adult pneumonia mortality in Xuanwei, China: a retrospective cohort study. Environ Health Perspect 117 : 261–266.
8. World Health Organization (2009) Global health risks. Mortality and burden of disease attributable to selected major risks. Geneva, WHO.
9. PopeDP, MishraVK, ThompsonL, SiddiquiAR, RehfuessE, et al. (2010) Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol Rev
10. Dix-CooperL, EskenaziB, RomeroC, BalmesJ, SmithKR (2012) Neurodevelopmental performance among school age children in rural Guatemala is associated with prenatal and postnatal exposure to carbon monoxide, a marker for exposure to woodsmoke. Neurotoxicology 33 : 246–254.
11. PokhrelAK, SmithKR, KhalakdinaA, DeujaA, BatesMN (2005) Case-control study of indoor cooking smoke exposure and cataract in Nepal and India. Int J Epidemiol 34 : 702–708.
12. MesfinMM, de la CameraJ, TarekeIG, AmanualG, ArayaT, et al. (2006) A community-based trachoma survey: prevalence and risk factors in the Tigray region of northern Ethiopia. Ophthalmic Epidemiol 13 : 173–181.
13. TurnerVM, WestSK, MunozB, KatalaSJ, TaylorHR, et al. (1993) Risk factors for trichiasis in women in Kongwa, Tanzania: A case-control study. Int J Epidemiol 22 : 341–347.
14. United Nations Foundation (2011) Sustainable Energy for All. Available: http://www.sustainableenergyforall.org/. Accessed February 14, 2012.
15. United Nations Foundation (2012) Global Alliance for Clean Cookstoves. Available: http://cleancookstoves.org/. Accessed May 21, 2012.
16. International Organization for Standardization (2012) Guidelines for evaluating cookstove performance. IWA 11 : 2012: ISO.
17. World Health Organization (2011) Indoor air pollution and health. WHO. Available: http://www.who.int/mediacentre/factsheets/fs292/en/. Accessed May 25, 2012.
18. MartinWJII, GlassRI, BalbusJM, CollinsFS (2011) A major environmental cause of death. Science 334 : 180.
19. Hanna R, Duflo E.,Greenstone M., (2012) Up in Smoke: The Influence of Household Behavior on the Long-Run Impact of Improved Cooking Stoves. Working Paper 12-10. Massachusetts Institute of Technology Department of Economics Working Paper Series. Social Science Research Network Paper Collection
20. SmithKR, McCrackenJP, WeberMW, HubbardA, JennyA, et al. (2011) Effect of reduction in household air pollution on childhood pneumonia in Guatemala (RESPIRE): a randomised controlled trial. Lancet 378 : 1717–1726.
21. Global Alliance For Clean Cookstoves Health Working Group (2011) Roadmap Recommendations: Health. Available: http://www.cleancookstoves.org/assets/rfps-and-rfas/working-group-recommendations.pdf Accessed May 25, 2012.
22. BruceN, NeufeldL, BoyE, WestC (1998) Indoor biofuel air pollution and respiratory health: The role of confounding factors among women in highland Guatemala. Int J Epidemiol 27 : 454–458.
23. McCrackenJP, SchwartzJ, BruceN, MittlemanM, RyanLM, et al. (2009) Combining individual - and group-level exposure information: child carbon monoxide in the Guatemala woodstove randomized control trial. Epidemiology 20 : 127–136.
24. SmithKR, SametJM, RomieuI, BruceN (2000) Indoor air pollution in developing countries and acute lower respiratory infections in children. Thorax 55 : 518–532.
25. ZhangJ, SmithKR (2007) Household air pollution from coal and biomass fuels in China: Measurements, health impacts, and interventions. Environ Health Perspect 115 : 848–855.
26. EzzatiM, SalehH, KammenDM (2000) The contributions of emissions and spatial microenvironments to exposure to indoor air pollution from biomass combustion in Kenya. Environ Health Perspect 108 : 833–839.
27. World Health Organization (2010) WHO Guidelines for Indoor Air Quality: Selected Pollutants. Available: http://www.euro.who.int/__data/assets/pdf_file/0009/128169/e94535.pdf. Accessed May 25, 2012.
28. RobertsLJ, MorrowJD (2000) Measurement of F(2)-isoprostanes as an index of oxidative stress in vivo. Free Radic Biol Med 28 : 505–513.
29. KulkarniNS, PrudonB, PanditiSL, AbebeY, GriggJ (2005) Carbon loading of alveolar macrophages in adults and children exposed to biomass smoke particles. Sci Total Environ 345 : 23–30.
30. ZhouH, KobzikL (2007) Effect of concentrated ambient particles on macrophage phagocytosis and killing of Streptococcus pneumoniae. Am J Respir Cell Mol Biol 36 : 460–465.
31. HeltbergR (2005) Factors determining household fuel choice in Guatemala. Environ Dev Econ 10 : 337–361.
32. WickramasingheA (2011) Energy access and transition to cleaner cooking fuels and technologies in Sri Lanka: Issues and policy limitations. Energy Policy 39 : 7567–7574.
33. World Bank (2011) Household Cookstoves, Environment, Health and Climate Change: A New Look at an Old Problem (63217, World Bank Washington, DC, 2011).
34. Ballard-Tremeer G, Mathee A (2000) Review of interventions to reduce the exposure of women and young children to indoor air pollution in developing countries. WHO/USAID consultation on Indoor Air Pollution and Health May 3–4, 2000. Washington, DC.
35. BarnesBR, MatheeA, KriegerL, ShafritzL, FavinM, et al. (2004) Testing selected behaviors to reduce indoor air pollution exposure in young children. Health Educ Res 19 : 543–550.
36. Environmental Health Project, UNICEF Water Environment and Sanitation Program, USAID, World Bank Water and Sanitation Program, Water Supply & Sanitation Collaborative Council (2004) The hygiene improvement framework: A comprehensive approach for preventing childhood diarrhea. Office of Health, Infections Diseases and Nutrition, Bureau for Global Health, USAID.
37. The Evaluation Gap Working Group (2006) When will we ever learn? Improving lives through impact evaluation. Washington, D.C.: Center for Global Development.
38. McClureEM, PashaO, GoudarSS, ChombaE, GarcesA, et al. (2011) Epidemiology of stillbirth in low-middle income countries: A Global Network Study. Acta Obstet Gynecol Scand 90 : 1379–1385.
39. RacioppiF, BertolliniR, Taylor GeeV (2004) Catastrophic failures of public health. Lancet 363 : 1552–1553.
40. SmithAH, LingasEO, RahmanM (2000) Contamination of drinking-water by arsenic in Bangledesh: A public health emergency. Bull World Health Organ 78 : 1093–1103.
41. PopeCA3rd, EzzatiM, DockeryDW (2009) Fine-particulate air pollution and life expectancy in the United States. N Engl J Med 360 : 376–386.
42. BiranA, SmithL, LinesJ, EnsinkJ, CameronM (2007) Smoke and malaria: Are interventions to reduce exposure to indoor air pollution likely to increase exposure to mosquitos? Trans R Soc Trop Med Hyg 101 : 1065–1071.
43. Ruiz-MercadoI, MaseraO, ZamoraH, SmithKR (2011) Adoption and sustained use of improved cookstoves. Energy Policy 39 : 7557–7566.
44. Ruiz-MercadoI, LamN, CanuzE, DavilaG, SmithKR (2008) Low-cost temperature data loggers as Stove Use Monitors (SUMs). Boiling Point 55 : 16–18.
45. University of California, KR S (2012) Household Energy, Climate, and Health Project. University of California, Berkeley. Available: http://ehs.sph.berkeley.edu/krsmith/?page_id=1000. Accessed May 25, 2012.
46. Aprovecho Research Center (2012) Stove Camp - A Hands-On Seminar on Stove Design and Testing. Available: http://www.aprovecho.org/lab/work/conferences/stove-camp. Accessed May 24, 2012.
47. Global Alliance For Clean Cookstoves (2012) Request for Applications: Cookstoves and Child Survival (RFA 12-1). Available: http://www.cleancookstoves.org/funding-opportunities/rfa-4-5_final.pdf Accessed May 24, 2012.
48. HortonR (2012) GBD 2010: understanding disease, injury, and risk. Lancet 380 : 2053–2054.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 6- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Antikoagulační léčba u pacientů před operačními výkony
-
Všechny články tohoto čísla
- Uncovering Treatment Burden as a Key Concept for Stroke Care: A Systematic Review of Qualitative Research
- Bigotry and Oppressive Laws in Africa Drive HIV in Men Who Have Sex with Men
- Household Air Pollution in Low- and Middle-Income Countries: Health Risks and Research Priorities
- The Health Effects of Motorization
- The Role of Adiposity in Cardiometabolic Traits: A Mendelian Randomization Analysis
- Patented Drug Extension Strategies on Healthcare Spending: A Cost-Evaluation Analysis
- The Effect of Intermittent Antenatal Iron Supplementation on Maternal and Infant Outcomes in Rural Viet Nam: A Cluster Randomised Trial
- Prevalence of Consensual Male–Male Sex and Sexual Violence, and Associations with HIV in South Africa: A Population-Based Cross-Sectional Study
- Associations between Active Travel to Work and Overweight, Hypertension, and Diabetes in India: A Cross-Sectional Study
- Addressing the Wicked Problem of Obesity through Planning and Policies
- Serum Iron Levels and the Risk of Parkinson Disease: A Mendelian Randomization Study
- Targeting Asymptomatic Malaria Infections: Active Surveillance in Control and Elimination
- Malignant Neglect: The Failure to Address the Need to Prevent Premature Non-communicable Disease Morbidity and Mortality
- Diet and Physical Activity for the Prevention of Noncommunicable Diseases in Low- and Middle-Income Countries: A Systematic Policy Review
- Modern Medicine Is Neglecting Road Traffic Crashes
- Integrating Health Care Delivery and Data Collection in Rural India Using a Rapidly Deployable eHealth Center
- Rising Health Care Costs and Life-Cycle Management in the Pharmaceutical Market
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Diet and Physical Activity for the Prevention of Noncommunicable Diseases in Low- and Middle-Income Countries: A Systematic Policy Review
- Addressing the Wicked Problem of Obesity through Planning and Policies
- Modern Medicine Is Neglecting Road Traffic Crashes
- Uncovering Treatment Burden as a Key Concept for Stroke Care: A Systematic Review of Qualitative Research
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



