-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Diet and Physical Activity for the Prevention of Noncommunicable Diseases in Low- and Middle-Income Countries: A Systematic Policy Review
Background:
Diet-related noncommunicable diseases (NCDs) are increasing rapidly in low - and middle-income countries (LMICs) and constitute a leading cause of mortality. Although a call for global action has been resonating for years, the progress in national policy development in LMICs has not been assessed. This review of strategies to prevent NCDs in LMICs provides a benchmark against which policy response can be tracked over time.Methods and Findings:
We reviewed how government policies in LMICs outline actions that address salt consumption, fat consumption, fruit and vegetable intake, or physical activity. A structured content analysis of national nutrition, NCDs, and health policies published between 1 January 2004 and 1 January 2013 by 140 LMIC members of the World Health Organization (WHO) was carried out. We assessed availability of policies in 83% (116/140) of the countries. NCD strategies were found in 47% (54/116) of LMICs reviewed, but only a minority proposed actions to promote healthier diets and physical activity. The coverage of policies that specifically targeted at least one of the risk factors reviewed was lower in Africa, Europe, the Americas, and the Eastern Mediterranean compared to the other two World Health Organization regions, South-East Asia and Western Pacific. Of the countries reviewed, only 12% (14/116) proposed a policy that addressed all four risk factors, and 25% (29/116) addressed only one of the risk factors reviewed. Strategies targeting the private sector were less frequently encountered than strategies targeting the general public or policy makers.Conclusions:
This review indicates the disconnection between the burden of NCDs and national policy responses in LMICs. Policy makers urgently need to develop comprehensive and multi-stakeholder policies to improve dietary quality and physical activity.
Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 10(6): e32767. doi:10.1371/journal.pmed.1001465
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001465Summary
Background:
Diet-related noncommunicable diseases (NCDs) are increasing rapidly in low - and middle-income countries (LMICs) and constitute a leading cause of mortality. Although a call for global action has been resonating for years, the progress in national policy development in LMICs has not been assessed. This review of strategies to prevent NCDs in LMICs provides a benchmark against which policy response can be tracked over time.Methods and Findings:
We reviewed how government policies in LMICs outline actions that address salt consumption, fat consumption, fruit and vegetable intake, or physical activity. A structured content analysis of national nutrition, NCDs, and health policies published between 1 January 2004 and 1 January 2013 by 140 LMIC members of the World Health Organization (WHO) was carried out. We assessed availability of policies in 83% (116/140) of the countries. NCD strategies were found in 47% (54/116) of LMICs reviewed, but only a minority proposed actions to promote healthier diets and physical activity. The coverage of policies that specifically targeted at least one of the risk factors reviewed was lower in Africa, Europe, the Americas, and the Eastern Mediterranean compared to the other two World Health Organization regions, South-East Asia and Western Pacific. Of the countries reviewed, only 12% (14/116) proposed a policy that addressed all four risk factors, and 25% (29/116) addressed only one of the risk factors reviewed. Strategies targeting the private sector were less frequently encountered than strategies targeting the general public or policy makers.Conclusions:
This review indicates the disconnection between the burden of NCDs and national policy responses in LMICs. Policy makers urgently need to develop comprehensive and multi-stakeholder policies to improve dietary quality and physical activity.
Please see later in the article for the Editors' SummaryIntroduction
Noncommunicable diseases (NCDs) are the leading cause of death globally. Of the 57 million global deaths in 2008, 36 million (63%) were due to NCDs, principally cardiovascular diseases, diabetes, cancers, and chronic respiratory diseases [1]. Mortality and morbidity data reveal the growing and disproportional impact of the epidemic in low - and middle-income countries (LMICs). Nearly 80% of the yearly NCD deaths—equivalent to 29 million people—are estimated to occur in LMICs. Without effective prevention and control, an estimated 41 million people in LMICs will die from NCDs by 2015 [2]. NCDs will evolve into a staggering economic burden over the next two decades [3].
Poor dietary quality (in particular, high salt intake, high saturated and trans-fatty acid intake, and low fruit and vegetable consumption) and insufficient physical activity are key risk factors for NCD development [4] and mortality worldwide [5], and are considered priority areas for international action [6]. The mean salt intake in most LMICs exceeds the recommended maximum intake [7]. Reducing salt intake to about 6 g/d could prevent annually about 2.5 million deaths globally [8]–[11], and a 15% reduction of salt intake over a decade in LMICs could forestall 3.1 million deaths [11],[12]. Fruit and vegetable intake is inadequate [13], and this situation contributes to 2.7 million NCD-related deaths per year. Despite evidence indicating that proper levels of physical activity are associated with a 30% reduction in the risk of ischemic heart disease, a 27% reduction in the risk of diabetes, and a 21%–25% reduction in the risk of breast and colon cancer [14],[15], approximately 3.2 million deaths each year are attributable to insufficient physical activity [6]. Physical inactivity is increasingly becoming prevalent in LMICs and already constitutes one of the leading causes of mortality [16]. There is also concern about excess intake of saturated and transfatty acids in LMICs, although large regional differences are observed [17],[18].
Preventing NCDs is not impossible [19]. Cecchini and colleagues analyzed population-based strategies to prevent NCDs in a number of LMICs with a high burden of NCDs [4]. Health information and communication strategies, fiscal measures, and regulatory measures for marketing or provision of nutrition information to children that promotes healthy eating and physical activity were found to yield substantial and cost-effective health gains, in particular in LMICs [4]. In addition, these interventions were found to be particularly effective when delivered as a multi-intervention package. Hence, it is crucial to translate the available evidence into sustainable policies in LMICs [6].
In May 2004, all WHO member states endorsed the Global Strategy on Diet, Physical Activity and Health, aiming to address NCDs through diet and physical activity [20]. Recently, a United Nations high-level meeting convened to discuss measures to prevent and control the global NCD epidemic and stressed the need to accelerate the policy response to it [21]. Monitoring this international commitment is important and can be achieved by systematic policy reviews. Previous policy reviews [22],[23], however, provided only a partial view of efforts undertaken to address NCDs, as they relied on survey data and did not consider the actual content of the policies. As policy documents are the culmination of existing social processes, they reflect the views of various stakeholders and are considered to be a reliable account of prevailing policy paradigms in a country [24]. We carried out a stocktaking exercise on national policy actions for NCD prevention in LMICs, and assessed the extent to which these address critical risk factors for NCDs, i.e., salt, fat, and fruit and vegetable intake, and physical inactivity. We focused on the existence and content of policies for the prevention of NCDs, not on their actual implementation.
Methods
Collection of Policy Documents
We searched the Internet (key words [“Nutrition” OR “NCD”] AND [“Policy” OR “Strategies” OR “Actions”]) for all publicly available national policies related to diet, nutrition, NCDs, and health in the countries classified as LMICs by the World Bank in 2011 [25]. We also searched the websites of the national ministries involved in nutrition or NCD prevention (i.e., ministries of health, sports, welfare, social affairs, or agriculture) and government portals as well as national nutrition societies. For those countries for which no policy was retrieved through the web search, an e-mail request stating the purpose of the study was sent to the respective bodies. A similar e-mail request was also sent to the WHO Regional Offices and to personal contacts of the research team. When no reply was obtained after repeated contact attempts and no reference to the existence of relevant policy documents was found during our Internet search, we classified the country as one for which we were unable to assess availability of policies. In addition to our search, we used the policy database of the WHO Regional Office for Europe [26] to assess policy availability.
Screening and Selection of Documents
The following inclusion criteria were used to include the policies in the analysis: (i) the policy is from a country classified as LMIC according to 2011 World Bank classification [25], (ii) the policy is officially approved by the national government, (iii) the policy is a publicly available document, published between 1 January 2004 and 1 January 2013, and (iv) the policy relates directly or indirectly to prevention of NCDs (Text S1). We report our findings as a systematic policy review (Text S2). Because we present our results by WHO region, we also excluded countries that were not official member states of WHO in 2011. There was no language restriction. The definitions of “policy,” “action plan,” and “program” vary broadly among the national documents. For the purpose of the present review, a broad definition of policy was used, and all national documents that included the national objectives and guidelines for action in the domain of diet and/or physical activity and/or prevention of NCDs were included. No document was excluded based on its title (e.g., “plan” versus “policy” versus “strategy”).
Data Analysis
Structured content analysis was conducted by coding the documents in NVivo 8 (QSR International). The documents were coded independently by two researchers to minimize bias induced by subjective coding. The coded documents were compared, and if coding agreement was <99% (as assessed using Kappa test agreement in NVivo), the coded text was manually reviewed for inconsistencies.
We coded all text that explicitly referred to actions aiming to (i) limit salt, (ii) modify fat intake, (iii) increase fruit and vegetable intake, or (iv) promote physical activity. Although we acknowledge that it is particularly the shift of fat consumption from saturated fats to unsaturated fats and the elimination of dietary trans-fatty acids that are critical for the prevention of NCDs, we extracted all strategies relating to dietary fat intake, such as reduction of total fat intake. The key words for coding were structured as a coding tree (Figure 1). A query was constructed for each topic in NVivo to extract all relevant text electronically. We present the results by the principle target audience of the actions, grouped into three categories: (i) general public and consumers, (ii) government, and (iii) private sector.
Fig. 1. Coding tree for policy actions analyzed in the documents. 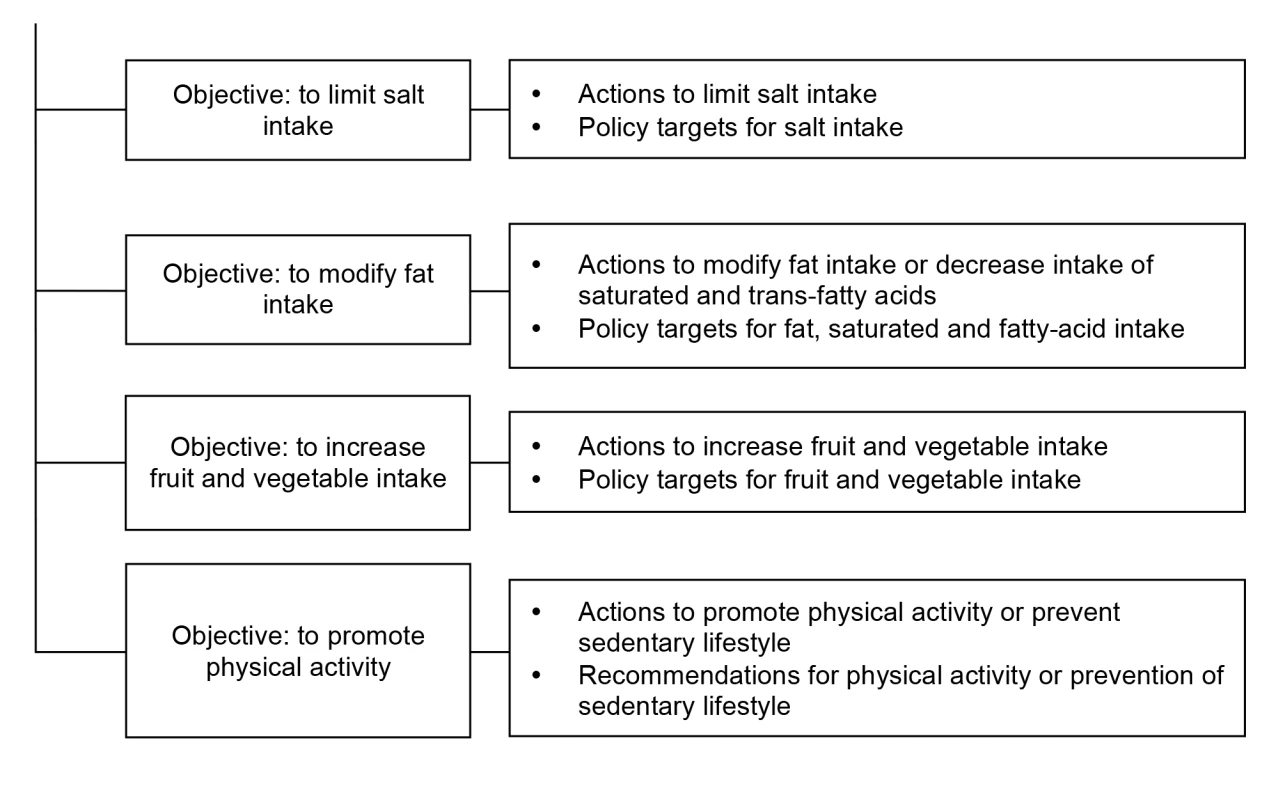
Results
Description of Policies
Out of the 144 countries classified by the World Bank as LMICs, four countries (Mayotte, West Bank and Gaza, the Republic of Kosovo, and American Samoa) were not official member states of WHO in 2011 and were excluded from the review. We note, however, the availability of a nutrition policy for West Bank and Gaza [27].
Of the 140 LMICs found in the six WHO regions (Africa, Europe, the Americas, South-East Asia, the Eastern Mediterranean, and the Western Pacific), we found information on the availability of policies for 83% (116/140) countries (Figure 2; Table S1). We were unable to assess the availability of policy documents for 24 countries, and in particular in the Eastern Mediterranean Region 40% (6 out of 15 countries in the region). In the European, African, Western Pacific, and South-East Asian Regions and the Region of the Americas, this proportion was 24% (5/21), 9% (4/45), 22% (4/18), 9% (1/11), and 13% (4/30), respectively. In total, 33 countries were excluded from review as they had no policy (n = 4), a policy published before 2004 (n = 19), or a policy document that was not officially endorsed (n = 3) or could not be circulated publicly (n = 3). In an additional four countries, a policy was reported to be available [26], but the full document could not be obtained.
Fig. 2. Selection process of nutrition, noncommunicable diseases, and health policies from low- and middle- income countries. 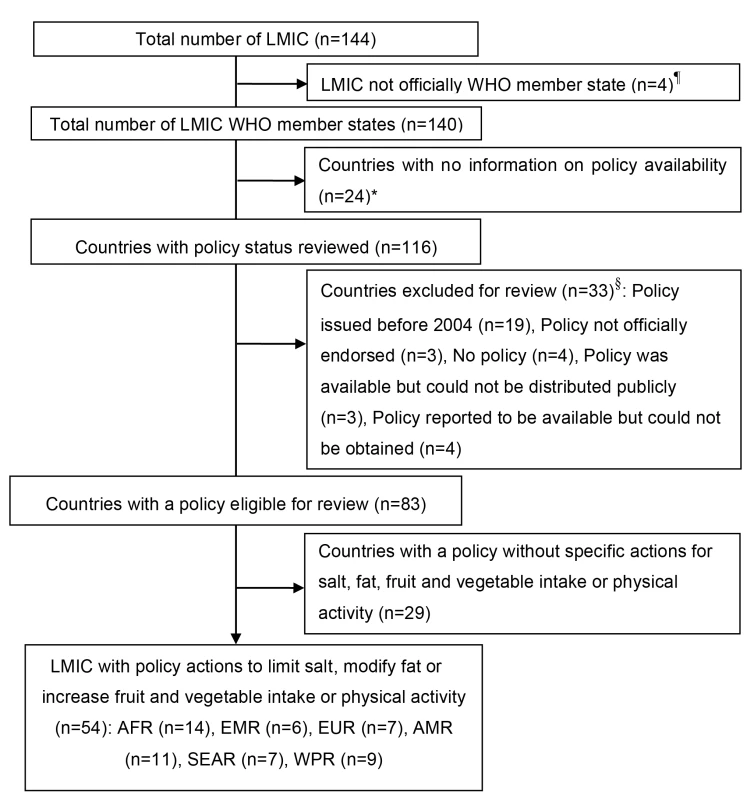
The WHO classification of regions and allocation of countries was used. AFR, African Region; AMR, Region of the Americas; EMR, Eastern Mediterranean Region; EUR, European Region; SEAR, South-East Asia Region; WPR, Western Pacific Region. ¶Mayotte, West Bank and Gaza, the Republic of Kosovo, and American Samoa. *Antigua and Barbuda, Egypt, Dominica, Democratic People's Republic of Korea, Sao Tome and Principe, Dominican Republic, Micronesia, Gabon, Tonga, Kyrgyzstan, Lebanon, Libya, Algeria, Iraq, Lithuania, Palau, Marshall Islands, Uzbekistan, Yemen, Romania, Saint Kitts and Nevis, Syrian Arab Republic, Turkmenistan, and Comoros. §Policy issued before 2004: Belize, Venezuela, Bosnia and Herzegovina, Eritrea, Lesotho, Papua New Guinea, Albania, Armenia, Burundi, Ecuador, El Salvador, Kiribati, Namibia, Sierra Leone, Gambia, Zimbabwe, Somalia, United Republic of Tanzania, and Vanuatu; policy not officially endorsed: Democratic Republic of the Congo, Senegal, and Tuvalu; no policy : Chad, Congo, South Africa, and Tajikistan; policy was available but could not be publically distributed: Central African Republic, Cameroon, and Tunisia; policy reported to be available [26] but could not be obtained: Azerbaijan, Belarus, Kazakhstan, and Ukraine. For 29 countries, the policy document reviewed did not contain any of the NCD prevention strategies reviewed [28]–[56]. In 30 countries, policy strategies to improve dietary quality did not specify actions for any of the dietary risk factors reviewed here [28],[29],[32]–[38],[40]–[52],[55]–[62]. In the countries reviewed, strategies that addressed intake of salt, fat, or fruits and vegetables or the promotion of physical activity were found in 47% (54/116) of policies. These policies had a main focus on food or nutrition (n = 34), general health (n = 11), and, to a lesser extent, the prevention of NCDs (n = 9). In total, 36 countries had explicit actions in their policies to increase fruit and vegetable intake, 20 specified actions aimed to address dietary fat consumption, 23 specified actions to limit salt intake, and 35 specified actions to promote physical activity. Although generally low, the proportion of countries with a policy that targeted at least one risk factor was higher in South-East Asia and the Western Pacific than in Africa, Europe, the Americas, and the Eastern Mediterranean. Only 12% (14/116) of the LMICs reviewed (Bhutan, Jamaica, Mauritius, the Republic of Moldova, Malaysia, Indonesia, the Philippines, Cambodia, the former Yugoslav Republic of Macedonia, Jordan, Montenegro, Brazil, Iran, and Mongolia) proposed a package that addressed all four risk factors, and approximately 23% (27/116) of countries addressed only one of the risk factors (Figure 3).
Fig. 3. Atlas of availability of national actions to limit salt or fat intake or increase fruit and vegetable intake or physical activity. 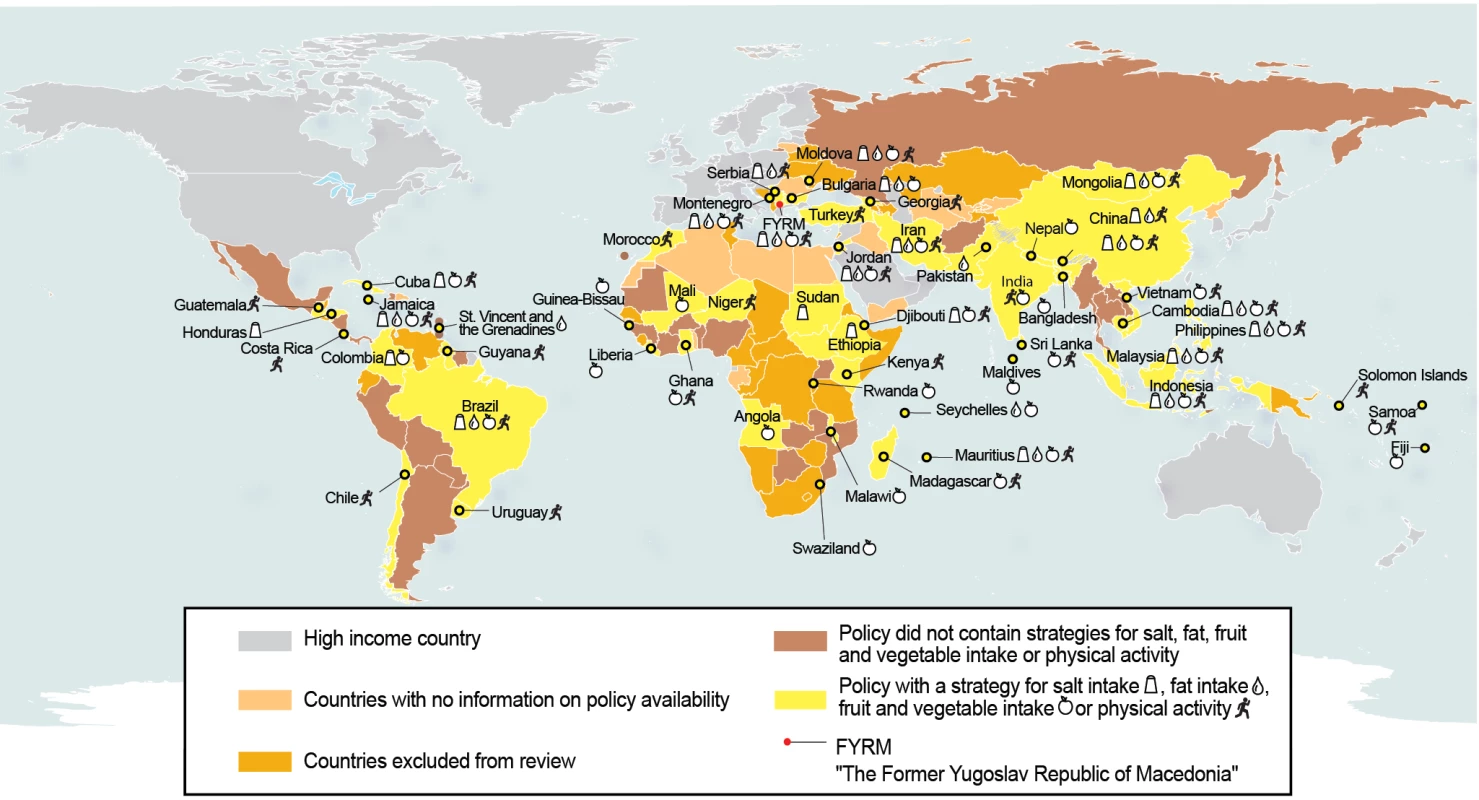
Geographic boundaries from the United Nations Cartographic Section were used [105]. Policy Actions to Limit Salt Intake
Only 20% (23/116) of the countries reviewed specified strategies to limit dietary salt intake, and eight policies detailed national targets to limit salt intake (Table 1). A large majority (83%; 19/23) of the countries with salt reduction strategies outlined measures of education and awareness creation in the general public and consumers, in particular focused on food labeling and promotion of foods, snacks, and packaged seasonings with reduced salt content. Strategies targeted towards the private sector were observed in 30% (7/23) of the policies and mainly related to product reformulation. The actions targeted at the governments were essentially the establishment of fiscal measures, labeling, and development of standards for salt in food and market regulations. Of the 83 countries with a policy eligible for review, 43 contained specific measures for salt iodization, but only ten of these also mentioned the need to reduce or manage dietary salt intake.
Tab. 1. National policy actions and targets to limit salt intake in LMICs by WHO region and target group. 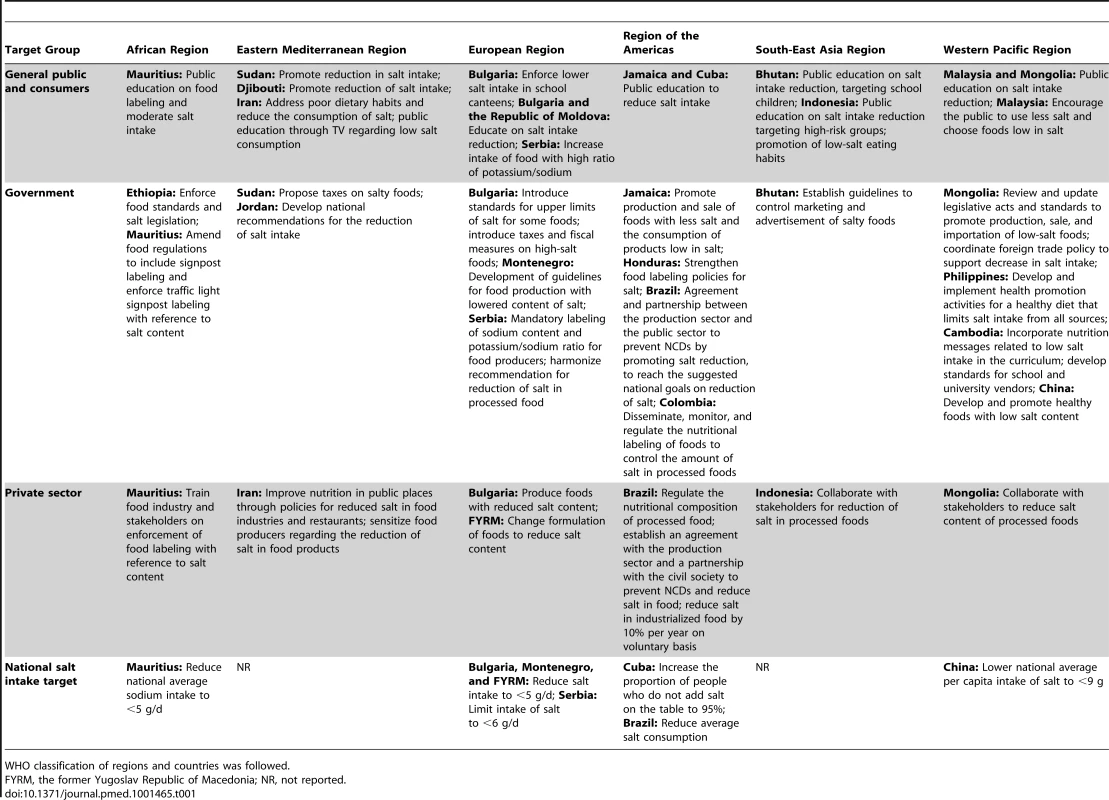
WHO classification of regions and countries was followed. Policy Actions to Modify Fat Intake
Of the countries with strategies to modify fat intake, 65% (13/20) proposed strategies targeting the general public and consumers via public education and awareness creation (Table 2). The use of dietary guidelines and food labeling were specifically mentioned as means of public education on dietary fat intake reduction in the Mauritius [63], Bulgaria [64], Jamaica [65], and Bhutan [66]. Imposition of fiscal measures, collaboration with the food industry for product reformulation, and the establishment and enforcement of food standards were mentioned as the main actions to be implemented by the government. Only Mauritius [63], Bulgaria [64], the former Yugoslav Republic of Macedonia [67], Iran [68], and Mongolia [69] outlined specific strategies targeted towards the private sector. Intake of specific fatty acids, and in particular saturated fat (Mongolia [69], the former Yugoslav Republic of Macedonia [67], Jordan [70], Bhutan [66], Cambodia [71], Bulgaria [64], Seychelles [72], the Philippines [73], Montenegro [74], and Iran [68]) and trans-fatty acids (the former Yugoslav Republic of Macedonia [67], Bhutan [66], Bulgaria [64], Seychelles [72], the Philippines [73], Montenegro [74], Mauritius [63], Brazil [75], and Iran [68]), was addressed in ten and nine countries, respectively. Whereas Mauritius [63] proposed research into the safety of reused oils, others focused on the type of fat (Iran [68] and Cambodia [71]) or the number of times oil should be used (Seychelles [72]). Six countries (Mauritius [63], Bulgaria [64], the former Yugoslav Republic of Macedonia [67], Montenegro [74], Malaysia [76], and Viet Nam [77]) mentioned specific national fat intake targets (Table 2).
Tab. 2. National policy actions and targets to limit fat intake by WHO region and target group. 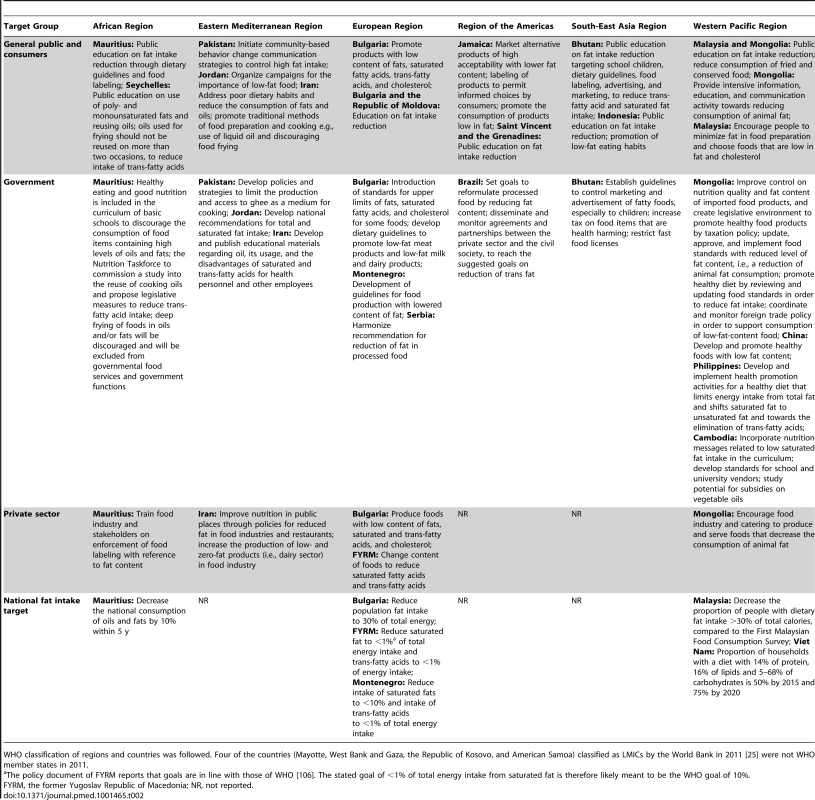
WHO classification of regions and countries was followed. Four of the countries (Mayotte, West Bank and Gaza, the Republic of Kosovo, and American Samoa) classified as LMICs by the World Bank in 2011 [25] were not WHO member states in 2011. Policy Actions to Increase Fruit and Vegetable Intake
Compared to the other dietary risk factors reviewed, the objective of increasing fruit and vegetable consumption had the highest coverage: 31% (36/116) of the policies reviewed (Table S1). Promotion of school gardening, home gardening, and urban agriculture were the main actions to ensure availability and accessibility of fruit and vegetables (Table 3). The majority (75%; 27/36) of the policy documents with strategies for fruit and vegetable intake focused on public education and demonstrations to promote increased fruit and vegetable intake. Malaysia proposed the development of special recipe books in this regard [76]. Other strategies, as found in Sri Lanka [78] and Mongolia [69] for instance, targeted the catering services in educational and government institutions to ensure strict inclusion of fruits and vegetables in the meals. In all of the WHO regions, policy documents that addressed increasing fruit and vegetable consumption included the need to produce, store, and process local fruits and vegetables, and to educate populations to consume them. Policy measures outlining responsibilities for the private sector were less frequently encountered (28%; 10/36) than those detailing actions to be implemented by the government (53%; 19/36) or targeting the general public (75%; 27/36).
Tab. 3. National policy actions and targets to increase fruit and vegetable intake by WHO region and target group. 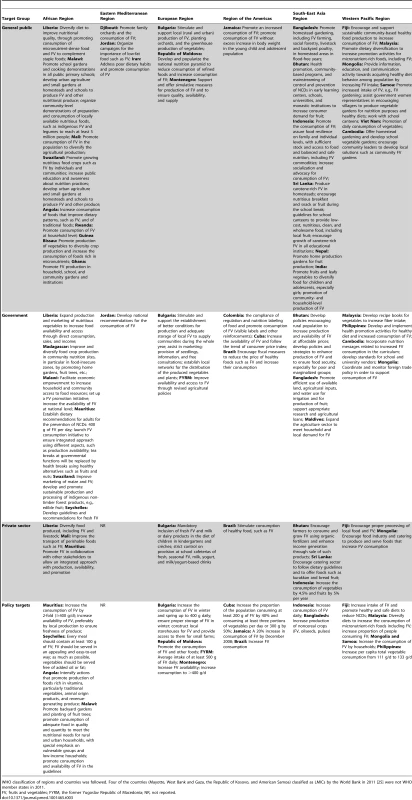
WHO classification of regions and countries was followed. Four of the countries (Mayotte, West Bank and Gaza, the Republic of Kosovo, and American Samoa) classified as LMICs by the World Bank in 2011 [25] were not WHO member states in 2011. Policy Actions to Increase Physical Activity and Address Sedentary Lifestyle
Public education and sensitization were the main strategies to promote physical activity in the policies (Table 4). Whereas countries such as Morocco [59], Mongolia [69], and Mauritius [63] targeted educational institutions, others, such as Bhutan [66], Guyana [79], and Malaysia [76], focused on workplaces. Samoa [80], the Niger [61], Indonesia [81], India [82], and Cambodia [71] targeted the community at large. Nine countries (Kenya [60], Morocco [59], Cuba [83], Uruguay [58], Jamaica [65], Brazil [75], Malaysia [76], the Philippines [73], and China [84]) proposed national policy targets for physical activity (Table 4).
Tab. 4. National policy actions and targets to promote physical activity by WHO region and target group. 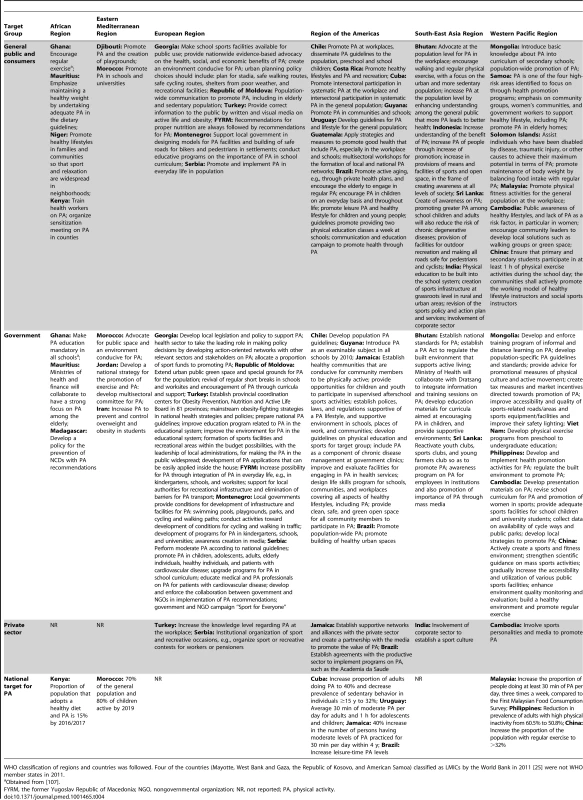
WHO classification of regions and countries was followed. Four of the countries (Mayotte, West Bank and Gaza, the Republic of Kosovo, and American Samoa) classified as LMICs by the World Bank in 2011 [25] were not WHO member states in 2011. Four countries' policy documents (Georgia [57], Mongolia [69], Mauritius [63], and Chile [85]) contained detailed actions and elaborated an implementation plan for stakeholders. The need to develop sports infrastructure and urban planning (e.g., bicycle lanes and recreational centers) featured in the policy documents of Georgia [57], the Republic of Moldova [86], Turkey [62], and Mongolia [69], for instance. Five countries (Mauritius [63], Brazil [75], Samoa [80], the Republic of Moldova [86], and Serbia [87]) mentioned the need to promote physical activity among the elderly. Only four countries (Bhutan [66], the Philippines [73], Cuba [83], and the Republic of Moldova [86]) outlined specific strategies to address sedentary lifestyles, and five (Turkey [62], Cambodia [71], Jamaica [65], Serbia [87], and India [82]) documented explicit actions to involve the private sector in the promotion of physical activity.
Discussion
Despite the global disease burden of NCDs in LMICs, policies that address at least one risk factor for NCDs were found in a minority of the LMICs reviewed, and only a handful of them comprehensively tackled NCDs through integrated action on various risk factors. Even if the 24 countries with unknown existence of a NCD prevention policy actually have such a policy, the proportion with countries tackling a risk factor would amount to 56% (78/140). This finding is discouraging, because in 2004, all countries expressed a strong commitment to action to address lifestyle, diet, and physical activity [20]. Our results show that, in spite of that official commitment, most LMICs are poorly prepared to tackle the NCD increase and that little progress has been made in recent years. This finding is consistent with the results of Alwan et al. [23], who reported the results of a survey in 2010 that was limited to countries with high NCD-related mortality.
Most of the policies in our review were poorly accessible and were only obtained after an extensive search or through personal contacts. Such a situation is certainly not favorable for benchmarking and communication of policies. In agreement with Sridhar et al. [88], we argue how better sharing of best practices and lessons learned with regard to policy development is needed to address the current NCD pandemic. Additional instruments and platforms to share lessons learned in policy development and implementation are needed. Policy databases with links to documents were created previously, but are restricted to nutrition action [89] or the European region [26]. An open-access, full-text global repository of initiatives and policies to address NCDs would be a great step forward. It could also contribute to global leadership and shared accountability in the global fight against NCDs, an issue that is long overdue [90]. Ideally, such a policy database would be connected to surveillance data on the main NCD risk factors, as suggested previously [23], and would facilitate tracking progress in the coming years. We are ready to organize such an open-access repository and invite interested policy makers to contact us for an update of the current database.
Priority setting and clear articulation of what needs to be done by stakeholders is a second key issue that emerged in this analysis. Countries seasoned in the fight against NCDs develop comprehensive strategies that focus on critical risk factors and what is expected of stakeholders [91]. In the present analysis, the level of detail and outlining of the organization of policy actions to undertake was generally discouraging. Only a minority of the policies reviewed surpassed description of policy actions and included a budget, implementation plan, time frame, and devolvement of responsibility for strategies to combat specific risk factors. Various policies describe strategies and actions for NCD prevention as “the need to develop and review dietary guidelines and recommendations for people suffering from nutrition-related NCDs” or use generic statements such as “create awareness of healthy eating lifestyle to control NCDs.” Such general statements are not informative, and clear actions need to be outlined in the policies to mobilize stakeholders for effective action [92].
Since its inception during the 1992 International Conference on Nutrition [93], the approach to streamline nutrition action in national policies has had limited success, partly because of the lack of strong leadership and commitment to lead concerted action involving various stakeholders [94]. The current scientific evidence and international experience in the fight against NCDs consistently indicates the need for comprehensive and integrated action on various risk factors [95]. Mobilization of the main actors—in particular, governments, international agencies, the private sector, civil society, health professionals, and individuals—is imperative [96]. An important limitation of most policies included in the analysis is the absence of plans, mechanisms, and incentives to foster multi-stakeholder and cross-sector collaboration. The food and nonalcoholic beverage industry, for instance, can play a role in the promotion of healthier lifestyles. However, before engaging with the private sector, government agencies should be aware of the need to manage potential conflicts of interest between the government and the private sector and should try to address these by defining clear roles, responsibilities, and targets to be achieved as a result of their collaboration [97]. Most strategies encountered in the policies were directed towards government agencies and consumers, and few were targeted at the business community, international agencies, or civil society. The United Nations Political Declaration on NCDs makes a strong call for multi-stakeholder partnerships to be leveraged for effective prevention of NCDs. Policy makers in LMICs may need additional support for the development of multi-stakeholder collaborations to address the burden imposed by NCDs as well as their root causes.
In our review of governmental policies relating to NCD prevention in LMICs, strategies to increase fruit and vegetable intake were the most frequent dietary action for NCD prevention. This is hardly surprising, as fruit and vegetable interventions were taken up early on in LMICs, primarily to address prevailing micronutrient deficiencies such as vitamin A deficiency [98]. Many of these experiences, however, are restricted to the development of food-based dietary guidelines or incentives targeted towards the agricultural sector. Policy measures to achieve better diet will require constructively engaging much more with a wider range of stakeholders, in particular the food industry, retail, and the catering sector [99]. The difficulty of developing a comprehensive policy response and integrated package of strategies is not restricted to NCDs alone, and has previously been observed in an in-depth analysis of high-burden countries for child malnutrition [100]. We also note that various countries have developed strategies to reduce total fat intake, despite convincing evidence that it is the reduction of saturated and trans-fatty acids in particular, and not total fat intake, that is effective to address NCDs [101].
Most strategies encountered in the policy documents focused on consumers and aimed to prevent NCDs through awareness creation, education (i.e., labeling), or changing individuals' behavior. The traditional approach to addressing lifestyle changes in individuals has met with very limited success. It is widely accepted that the environmental context drives individual diets and lifestyle [102] and that programs need to incorporate environmental determinants (i.e., the quantity, quality, or price of dietary choices, or the built environment for physical activity) in order to be effective. Such policy measures, in particular those addressing the private sector, were poorly elaborated in the policy documents [103].
A key issue is the actual implementation of policy measures in relation to what was articulated in the documents. The findings of this review indicate that few LMICs have made significant steps in the development of a comprehensive set of strategies to address NCDs. Although an in-depth evaluation of actual implementation, effects, and resources allocated has not been opportune to date, we hope that our findings provide baseline data and encourage countries to develop monitoring and evaluation mechanisms to assess policy response in due time. Documenting the effectiveness of population-based NCD prevention policies will be a critical factor of success to ensure effective action in LMICs [4].
For this review, we were able to assess documents in all languages received. Because of language constraints, however, two of the documents [74],[87] were coded by only one researcher. To assess the content of the policy of Iran, we relied on translations by experienced senior Iranian researchers. All other policy documents were obtained in Spanish, Portuguese, French, or English and were analyzed accordingly by the research team. For China and the Russian Federation, appropriate English versions of the policies were obtained from the Chinese Centers for Disease Control and the United States Department of Agriculture, respectively. Despite indications of availability of relevant policies in the European region [26], language limitations did not allow us to search the websites of a number of countries such as Azerbaijan, Belarus, and the Russian Federation.
The restriction of our review to only national policies presents a number of limitations. The mere presence or absence of policies or strategies for NCDs in a policy document does not necessarily reflect concrete action. Conversely, nutritional interventions have been implemented in some countries without a policy being developed and published [104]. In addition, this review assessed the contents of the policy documents as they were published and did not capture local or regional activities, or initiatives that emerged after the publication of the policies. The findings from a survey in countries with a high burden of NCDs, such as Thailand and South Africa, illustrate this discrepancy [23]. The contents might have been modified over time in response to new scientific findings, emerging nutritional challenges, or changes in the countries' priorities [91]. In addition, it is important to point out that we extracted only actions that explicitly referred to one of the risk factors analyzed. Generic statements such as “development of food-based dietary guidelines” or “establishment of fiscal measures for a healthy diet” were hence not coded.
The present review shows that the policy response to address current NCD challenges through diet and physical inactivity in LMICs is inadequate since endorsement of the Global Strategy on Diet, Physical Activity and Health [20]. LMICs urgently need to scale up interventions and develop integrated policies that address various risk factors for NCD prevention through multi-stakeholder collaboration and cross-sector involvement. Clear and prioritized actions are needed to harness the NCD epidemic. Such actions need to be documented in policy documents that are publicly available to share lessons learned, promote engagement with the stakeholders, and stimulate accountability and leadership in the fight against the burden of NCDs in LMICs. The establishment of an open-access and publicly accessible database of policy documents with regular systematic reviews of policy development might prove to be an incentive in this regard.
Supporting Information
Zdroje
1. World Health Organization (2011) Global status report on noncommunicable diseases. Geneva: World Health Organization.
2. AbegundeDO, MathersCD, AdamT, OrtegonM, StrongK (2007) Chronic diseases 1—the burden and costs of chronic diseases in low-income and middle-income countries. Lancet 370 : 1929–1938 ISI:000251517600031.
3. Bloom DE, Cafiero ET, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, et al.. (2011) The global economic burden of noncommunicable diseases. Geneva: World Economic Forum. 48 p.
4. CecchiniM, SassiF, LauerJA, LeeYY, Guajardo-BarronV, et al. (2010) Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. Lancet 376 : 1775–1784 ISI:000284984900033.
5. LimSS, VosT, FlaxmanAD, DanaeiG, ShibuyaK, et al. (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 : 2224–2260.
6. BeagleholeR, BonitaR, HortonR, AdamsC, AlleyneG, et al. (2011) Priority actions for the non-communicable disease crisis. Lancet 377 : 1438–1447 PM:21474174.
7. BrownIJ, TzoulakiI, CandeiasV, ElliottP (2009) Salt intakes around the world: implications for public health. Int J Epidemiol 38 : 791–813 ISI:000268810100028.
8. HeFJ, MacgregorGA (2004) Universal salt reduction. Hypertension 43: E12–E13 PM:14732726.
9. HeFJ, MacgregorGA (2005) Blood pressure—importance of salt intake. Am J Hypertens 18 : 1258–1259 PM:16182118.
10. HeFJ, MacgregorGA (2009) A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens 23 : 363–384 ISI:000266026600001.
11. HeFJ, JennerKH, MacgregorGA (2010) WASH—world action on salt and health. Kidney Int 78 : 745–753 PM:20720531.
12. AsariaP, ChisholmD, MathersC, EzzatiM, BeagleholeR (2007) Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet 370 : 2044–2053 PM:18063027.
13. HallJN, MooreS, HarperSB, LynchJW (2009) Global variability in fruit and vegetable consumption. Am J Prev Med 36 : 402–409 PM:19362694.
14. LeeIM, HsiehCC, PaffenbargerRSJr (1995) Exercise intensity and longevity in men. The Harvard Alumni Health Study. JAMA 273 : 1179–1184 PM:7707624.
15. PaffenbargerRSJr, KampertJB, LeeIM, HydeRT, LeungRW, et al. (1994) Changes in physical activity and other lifeway patterns influencing longevity. Med Sci Sports Exerc 26 : 857–865 PM:7934759.
16. World Health Organization (2009) Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization.
17. ElmadfaI, KornsteinerM (2009) Dietary fat intake—a global perspective. Ann Nutr Metab 54(Suppl 1): 8–14 PM:19641345.
18. PopkinBM (2006) Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr 84 : 289–298 PM:16895874.
19. GazianoTA, GaleaG, ReddyKS (2007) Scaling up interventions for chronic disease prevention: the evidence. Lancet 370 : 1939–1946 PM:18063028.
20. World Health Organization (2004) Global strategy on diet, physical activity and health, resolution of the fifty seventh World Health Assembly WHA57.17. Geneva: World Health Organization.
21. United Nations General Assembly (2011) Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. Available: http://www.un.org/ga/search/view_doc.asp?symbol=A/66/L.1. Accessed 6 May 2013.
22. World Health Organization (2010) A review of nutrition policies: draft report. Geneva: World Health Organization. Available: http://www.who.int/nutrition/EB128_18_Backgroundpaper1_A_review_of_nutritionpolicies.pdf. Accessed 6 May 2013.
23. Alwan A, Maclean DR, Riley LM, d'Espaignet ET, Mathers CD, et al.. (2010) Monitoring and surveillance of chronic non-communicable diseases: progress and capacity in high-burden countries. Lancet 376: : 1861–1868. PM:21074258
24. Miller FA, Alvarado K (2005) Incorporating documents into qualitative nursing research. J Nurs Scholarsh 37: : 348–353. ISI:000233170300016
25. World Bank (2011) Open Data Initiative: data catalog [database]. Available: http://data.worldbank.org/data-catalog#Tables. Accessed 6 May 2013.
26. World Health Organization (2011) WHO European database on nutrition, obesity and physical activity (NOPA). Copenhagen: WHO Regional Office for Europe. Available: http://data.euro.who.int/nopa/. Accessed 6 May 2013.
27. Palestinian National Authority Ministry of Health (2013) National nutrition policy, strategies & action plan (NNPSAP) 2011–2013. Available: http://www.moh.ps/attach/442.pdf. Accessed 6 May 2013.
28. Panama Ministerio de Salud (2010) Politicas y estrategias de salud 2005–2009.
29. Saint Lucia Ministry of Health (2000) Health sector reform proposals. 125 p.
30. Suriname Ministry of Public Health (2004) Health sector plan 2004–2008. Health care: a joint responsibility. 116 p. Available: http://www.healthresearchweb.org/files/National_Health_Policies-Suriname_2004-2008.pdf. Accessed 6 May 2013.
31. Argentina Ministerio de Salud de la Nación(2004) Bases del plan federal de salud 2004–2007. 55 p. Available: http://publicaciones.ops.org.ar/publicaciones/cdsMCS/05/pub_msan/PlaNFederaLdeSalud.pdf. Accessed 6 May 2013.
32. Nicaragua Ministerio de Salud (2004) Política nacional de salud 2004–2015. 75 p. Available: http://www.healthresearchweb.org/files/Politicas_Nacionales_Salud-Nicaragua_2004.pdf. Accessed 6 May 2013.
33. Timor-Leste Ministry of Health (2004) National nutrition strategy. Available: http://www.basics.org/documents/26-Timor-Leste-National-Nutrition-Strategy.pdf. Accessed 6 May 2013.
34. Uganda Ministry of Agriculture, Animal Industry & Fisheries, Uganda Ministry of Health (2004) The national food and nutrition strategy. 43 p. Available: http://www.drt-ug.org/book_files/National_Food_and_Nutrition_Strategy.pdf. Accessed 6 May 2013.
35. Nigeria Federal Ministry of Health (2004) Revised national health policy. 66 p. Available: http://osgf.dammy.net/payload?id=19d51d38-c75f-4461-91ce-f6a6d2298b87. Accessed 6 May 2013.
36. Paraguay Ministerio de Salud (2005) Política nacional de salud 2005–2008. 19 p. Available: http://new.paho.org/hq/dmdocuments/2010/Politicas_Nacionales_Salud-Paraguay_2005-2008.pdf%20. Accessed 6 May 2013.
37. Guinea Ministère de la Santé Publique (2005) Politique nationale d'alimentation—nutrition. 34 p. Available: http://www.pfnutrition.org/IMG/pdf/POLITIQUEDENUTRITION.pdf. Accessed 6 May 2013.
38. Boliva Ministra de Salud y Deportes (2006) Politicas nacionales salud Bolivia 2006–2010. 47 p.
39. Grenada Ministry of Health (2006) National strategic plan for health (2006–2010). 34 p.
40. Zambia Ministry of Health (2006) National health strategic plan 2006–2010 of Zambia. Available: http://www.who.int/nha/country/zmb/Zambia_NH_Strategic_plan,2006-2010%20.pdf. Accessed 6 May 2013.
41. Peru Ministerio de Salud (2007) Plan nacional concertado de salud. 38 p. Available: http://www2.paho.org/hq/dmdocuments/2010/Politicas_Nacionales_Salud-Peru_2007.pdf. Accessed 6 May 2013.
42. Burkina Faso Ministère de la Santé (2007) Politique nationale de nutrition. Ouagadougou: Burkina Faso Ministère de la Santé. 42 p.
43. Thailand Ministry of Public Health Bureau of Policy and Strategy (2007) Health policy in Thailand 2007. 64 p. Available: http://bps.ops.moph.go.th/HealthPolicy7.pdf. Accessed 6 May 2013.
44. Cape Verde Ministério da Saúde (2007) Politica nacional de saude. Available: http://www.governo.cv/documents/POLITINACIONALSAUDE_2020%20(2).pdf. Accessed 6 May 2013.
45. Mexico Secretaría de Salud (2007) Programma nacional de salud 2007–2012. Mexico City: Mexico Secretaría de Salud. 185 p.
46. Mozambique Secretariado Técnico de Segurança Alimentar e Nutricional (2007) Estratégia de segurança alimentar e nutricional. 51 p. Available: https://www.google.be/url?sa=t&rct=j&q=&esrc=s&source=web&cd=8&ved=0CGYQFjAH&url=http%3A%2F%2Fwww.omrmz.org%2Findex.php%2Frepositorio-bibliografico%2Fcategory%2F84-sector-agrario%3Fdownload%3D1328%3Asector-agrario&ei=pRx1UajGNqGW0AXj0oGACw&usg=AFQjCNG1PS8VYqn_e2dRbCh3tTHf-9cDfA. Accessed 6 May 2013.
47. Lao People's Democratic Republic Ministry of Health (2008) National nutrition policy. 17 p. Available: https://docs.google.com/file/d/10TAg_sT5reCM2U4Wp3OIyoVILwMIKY5n4z6vZbqkY3mFCJ0x9HdkRQOv2Iqb/edit?pli=1. Accessed 6 May 2013.
48. Afghanistan Ministry of Public Health and the Ministry of Agriculture, Irrigation and Livestock (2008) Health and nutrition sector strategy, Vol II.
49. Côte d'Ivoire Ministère de la Santé et de l'Hygiène Publique (2009) Politique nationale de nutrition. 32 p.
50. Global Agricultural Information Network (2010) Russian Federation: food security doctrine adopted. 12 p. Available: http://gain.fas.usda.gov/Recent%20GAIN%20Publications/Food%20Security%20Doctrine%20Adopted%20_Moscow_Russian%20Federation_2-11-2010.pdf. Accessed 6 May 2013.
51. Haiti Conseil Interministeriel pour la Securite Alimentaire, Haiti Coordination Nationale de la Securite Alimentaire (2010) Actualisation du plan nation de sécurité alimentaire et nutritionelle. 70 p. Available: http://infoagro.net/programas/seguridad/politicas/RegionCaribe/plan_Haiti.pdf. Accessed 6 May 2013.
52. Togo Ministère de la Sante (2010) Politique nationale d'alimentation et de nutrition.
53. Myanmar (2013) National health plan 2006–2011.
54. Benin Ministère de la Santé (2013) Plan national de développement sanitaire 2007–2016. 127 p.
55. Mauritania Ministere de la Sante et des Affaires Sociales (2015) Politique nationale de sante et d'action sociale 2006/2015. 31 p. Available: http://www.afro.who.int/index.php?option=com_docman&task=doc_download&gid=1208. Accessed 6 May 2013.
56. Botswana Ministry of Health (2005) National plan of action for nutrition 2005–2010. 57 p.
57. Georgia Ministry of Labour, Health and Social Affairs—Public Health Department (2006) Food security, healthy eating & physical activity national policy. 15 p.
58. Uruguay Ministerio de Salud Pública Direccion General de la Salud (2011) Programa nacional prioritario de nutricion 2005–2009. Available: http://www.msp.gub.uy/andocasociado.aspx?1973,14797. Accessed 6 May 2013.
59. Morocco Ministère de la Santé, United Nations Children's Fund (2013) La stratégie de la nutrition 2011–2019. 37 p. Available: http://www.unicef.org/morocco/french/Strategie_Nationale_de_Nutrition_.pdf. Accessed 6 May 2013.
60. Kenya Ministry of Public Health and Sanitation (2013) National nutrition action plan 2012–2017. 62 p.
61. Niger (2006) Politique nationale en matière d'alimentation et de nutrition. 32 p. Available: http://www.pfnutrition.org/IMG/pdf/Politique_Nationale_en_Alimentation_et_Nutrition.pdf. Accessed 6 May 2013.
62. Turkey Ministry of Health General Directorate of Primary Health Care (2010) Obesity prevention and control pogramme of Turkey (2010–2014). 112 p.
63. Mauritius Ministry of Health & Quality of Life—Nutrition Unit (2009) National plan of action for nutrition 2009–2010. 33 p. Available: http://www.gov.mu/portal/goc/moh/file/nutrition.pdf. Accessed 6 May 2013.
64. Bulgaria Council of Ministers (2005) National food and nutrition action plan 2005–2010. 89 p. Available: http://fnap.government.bg/UserFiles/File/ENGL%20sait/FNAP-Engl-revised-Superlast.doc. Accessed 6 May 2013.
65. Jamaica Ministry of Health (2004) National policy for the promotion of healthy lifestyles in Jamaica. 37 p. Available: http://db.natlaw.com/interam/jm/md/sp/spjmmd00001.pdf. Accessed 6 May 2013.
66. Bhutan Ministry of Health (2009) National policy and strategic frame-work on prevention and control of non communicable diseases. Available: http://www.health.gov.bt/downloads/NationalNCD.pdf. Accessed 6 May 2013.
67. The former Yugoslav Republic of Macedonia (2009) Second action plan on food and nutrition in the Republic of Macedonia for 2009–2014.
68. Iran Ministry of Health and Medical Education—Nutrition Department (2010) Operational plan to improve community nutrition. 34 p.
69. Mongolia Ministry of Health (2007) National programme on prevention and control of noncommunicable diseases. 36 p. Available: http://moh.mn/moh%20db/Healthreports.nsf/ecb18f03b32fae434825768500144b6e/776847c20ad6dc99c72572c1002eae42/FILE/XUTULBUR_ENG.pdf. Accessed 6 May 2013.
70. Jordan Ministry of Health, World Health Organization (2006) Nutrition in Jordan: update and plan of action. 101 p. Available: http://www.moh.gov.jo/MOH/Files/General_Info/aNutrition%20in%20Jordan-Policy.pdf. Accessed 6 May 2013.
71. Cambodia Ministry of Health—Department of Preventive Medicine (2006) National strategy for the prevention and control of noncommunicable disease: Cambodia (2007–2010). Available: ftp://ftp.wpro.who.int/scratch/HSD/Service_delivery_profiles/Cambodia/Documents%20from%20country/National%20Strategy%20for%20the%20prevention%20and%20contol%20of%20noncommunical%20disease.pdf. Accessed 6 May 2013.
72. Seychelles Ministry of Health and Social Development (2008) Ministerial nutrition policy of Seychelles. Victoria: Seychelles Ministry of Health and Social Development. 14 p.
73. Philippines Department of Health (2011) National policy on strengthening the prevention and control of chronic lifestyle related non communicable diseases. 14 p.
74. Montenegro Ministry of Health (2009) [Action plan for nutrition and food safety for Montenegro 2010–2014.] Podgorica: Montenegro Ministry of Health.
75. Brazil Ministry of Health (2011) Strategic action plan to tackle noncommunicable diseases (NCD) in Brazil: 2011–2022. 154 p. Available: http://portalsaude.saude.gov.br/portalsaude/arquivos/pdf/2012/Ago/29/cartilha_ingles_13102011.pdf. Accessed 6 May 2013.
76. Malaysia Ministry of Health—National Coordinating Committee on Food and Nutrition (2006) National plan of action for nutrition of Malaysia (2006–2015). Kuala Lumpur: Malaysia Ministry of Health. 55 p.
77. Viet Nam Prime Minister (2012) National nutrition strategy for 2011–2020, with a vision toward 2030. 48 p. Available: http://viendinhduong.vn/FileUpload/Documents/2.%20National%20Nutrition%20%20Strategy%202011-2020.pdf. Accessed 6 May 2013.
78. Sri Lanka Inter Ministerial Committee on Food Security (2004) Food and nutrition policy of Sri Lanka, 2004–2010. 9 p.
79. Guyana Ministry of Health (2008) National health sector strategy.
80. Samoa Ministry of Health (2008) Health sector plan 2008–2018. Available: http://www.wpro.who.int/health_services/samoa_nationalhealthplan.pdf. Accessed 6 May 2013.
81. Indonesia National Development Planning Board (2005) National action plan for food and nutrition 2006–2010. 83 p. Available: http://ntt-academia.org/Pangantt/RAN-Food-Nutrition-English.pdf. Accessed 6 May 2013.
82. India Planning Commission Government (2008) Eleventh five year plan: 2007–12. Volume II: social sector. New Delhi: Oxford University Press. 237 p. Available: http://planningcommission.nic.in/plans/planrel/fiveyr/11th/11_v2/11th_vol2.pdf. Accessed 6 May 2013.
83. Cuba Ministerio de Salud Pública (2006) Proyecciones de la salud pública en Cuba para el 2015 . 68 p. Havana: Cuba Ministerio de Salud Pública.
84. China Ministry of Health (2012) China national plan for NCD prevention and treatment (2012–2015). Available: http://www.chinacdc.cn/en/ne/201207/t20120725_64430.html. Accessed 6 May 2013.
85. Chile Ministerio de Salud (2002) Objetivos sanitarios para la década 2000–2010. 308 p. Available: http://epi.minsal.cl/epi/html/elvigia/vigia15.pdf. Accessed 6 May 2013.
86. Republic of Moldova (2007) National health policy: 2007–2021. Available: http://www.ms.gov.md/_files/1024-National%2520Health%2520Policy%2520Republicof%2520Moldova.pdf. Accessed 6 May 2013.
87. Serbia Ministry of Health (2010) National program for prevention, treatment and control of cardiovascular diseases in Republic of Serbia till 2020. Belgrade: Official Gazette of the Republic of Serbia. 20 p.
88. Sridhar D, Stephen Morrison J, Piot P (2011) Getting the politics right for the September 2011 UN High-Level Meeting on Noncommunicable Ddiseases. Available: http://csis.org/files/publication/110215_Sridhar_GettingPoliticsRight_Web.pdf. Accessed 6 May 2013.
89. World Health Organization (2013) Global Database on the Implementation of Nutrition Action (GINA) [database]. Available: https://extranet.who.int/nutrition/gina/. Accessed 23 April 2013.
90. BeagleholeR, BonitaR, AlleyneG, HortonR, LiL, et al. (2011) UN High-Level Meeting on Non-Communicable Diseases: addressing four questions. Lancet 378 : 449–455 PM:21665266.
91. LachatC, VanCJ, DeHS, MatthysC, LarondelleY, et al. (2005) A concise overview of national nutrition action plans in the European Union Member States. Public Health Nutr 8 : 266–274 PM:15918923.
92. GeneauR, StucklerD, StachenkoS, McKeeM, EbrahimS, et al. (2010) Raising the priority of preventing chronic diseases: a political process. Lancet 376 : 1689–1698 PM:21074260.
93. Food and Agriculture Organization, World Health Organization (1992) World declaration on nutrition. 50 p. Available: http://www.fao.org/docrep/U9920t/u9920t0a.htm. Accessed 6 May 2013.
94. JonssonU (2010) The rise and fall of paradigms in world food and nutrition policy. World Nutr 1 : 128–158.
95. Willett WC, Koplan JP, Nugent R, Dusenbury C, Puska P, et al.. (2006) Prevention of chronic disease by means of diet and lifestyle changes. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, et al.., editors. Disease control priorities in developing countries. Available: http://www.ncbi.nlm.nih.gov/books/NBK11795/pdf/ch44.pdf. Accessed 6 May 2013.
96. Gortmaker SL, Swinburn BA, Levy D, Carter R, Mabry PL, et al.. (2011) Changing the future of obesity: science, policy, and action. Lancet 378: : 838–847. PM:21872752
97. KraakVI, HarriganPB, LawrenceM, HarrisonPJ, JacksonMA, et al. (2012) Balancing the benefits and risks of public-private partnerships to address the global double burden of malnutrition. Public Health Nutr 15 : 503–517 PM:22014282.
98. PomerleauJ, LockK, KnaiC, McKeeM (2005) Interventions designed to increase adult fruit and vegetable intake can be effective: a systematic review of the literature. J Nutr 135 : 2486–2495 PM:16177217.
99. LachatC, RoberfroidD, HuybregtsL, Van CampJ, KolsterenP (2009) Incorporating the catering sector in nutrition policies of WHO European Region: is there a good recipe? Public Health Nutr 12 : 316–324 ISI:000263897400004.
100. United Nations Standing Committee on Nutrition (2009) Landscape analysis on countries' readiness to accelerate action in nutrition. Available: http://www.unscn.org/layout/modules/resources/files/scnnews37.pdf. Accessed 6 May 2013.
101. AstrupA, DyerbergJ, ElwoodP, HermansenK, HuFB, et al. (2011) The role of reducing intakes of saturated fat in the prevention of cardiovascular disease: where does the evidence stand in 2010? Am J Clin Nutr 93 : 684–688 PM:21270379.
102. SwinburnB, EggerG, RazaF (1999) Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med 29 : 563–570 ISI:000084397400017.
103. DaarAS, SingerPA, PersadDL, PrammingSK, MatthewsDR, et al. (2007) Grand challenges in chronic non-communicable diseases. Nature 450 : 494–496 PM:18033288.
104. BryceJ, CoitinhoD, Darnton-HillI, PelletierD, Pinstrup-AndersenP (2008) Maternal and child undernutrition: effective action at national level. Lancet 371 : 510–526 PM:18206224.
105. United Nations Cartographic Section (2012) World map: MAP No. 4170 Rev. 12, October 2011. Available: http://www.un.org/Depts/Cartographic/map/profile/world.pdf. Accessed 25 April 2012.
106. World Health Organization (2003) Diet, nutrition and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation. World Health Org Tech Rep 916 : 1–149.
107. Ghana Ministry of Health (2007) National health policy: creating wealth through health. Accra: Ghana Ministry of Health. 66 p.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 6- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Magnosolv a jeho využití v neurologii
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
-
Všechny články tohoto čísla
- Uncovering Treatment Burden as a Key Concept for Stroke Care: A Systematic Review of Qualitative Research
- Bigotry and Oppressive Laws in Africa Drive HIV in Men Who Have Sex with Men
- Household Air Pollution in Low- and Middle-Income Countries: Health Risks and Research Priorities
- The Health Effects of Motorization
- The Role of Adiposity in Cardiometabolic Traits: A Mendelian Randomization Analysis
- Patented Drug Extension Strategies on Healthcare Spending: A Cost-Evaluation Analysis
- The Effect of Intermittent Antenatal Iron Supplementation on Maternal and Infant Outcomes in Rural Viet Nam: A Cluster Randomised Trial
- Prevalence of Consensual Male–Male Sex and Sexual Violence, and Associations with HIV in South Africa: A Population-Based Cross-Sectional Study
- Associations between Active Travel to Work and Overweight, Hypertension, and Diabetes in India: A Cross-Sectional Study
- Addressing the Wicked Problem of Obesity through Planning and Policies
- Serum Iron Levels and the Risk of Parkinson Disease: A Mendelian Randomization Study
- Targeting Asymptomatic Malaria Infections: Active Surveillance in Control and Elimination
- Malignant Neglect: The Failure to Address the Need to Prevent Premature Non-communicable Disease Morbidity and Mortality
- Diet and Physical Activity for the Prevention of Noncommunicable Diseases in Low- and Middle-Income Countries: A Systematic Policy Review
- Modern Medicine Is Neglecting Road Traffic Crashes
- Integrating Health Care Delivery and Data Collection in Rural India Using a Rapidly Deployable eHealth Center
- Rising Health Care Costs and Life-Cycle Management in the Pharmaceutical Market
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Diet and Physical Activity for the Prevention of Noncommunicable Diseases in Low- and Middle-Income Countries: A Systematic Policy Review
- Addressing the Wicked Problem of Obesity through Planning and Policies
- Modern Medicine Is Neglecting Road Traffic Crashes
- Uncovering Treatment Burden as a Key Concept for Stroke Care: A Systematic Review of Qualitative Research
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



