-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Hospital Performance, the Local Economy, and the Local Workforce: Findings from a US National Longitudinal Study
Background:
Pay-for-performance is an increasingly popular approach to improving health care quality, and the US government will soon implement pay-for-performance in hospitals nationwide. Yet hospital capacity to perform (and improve performance) likely depends on local resources. In this study, we quantify the association between hospital performance and local economic and human resources, and describe possible implications of pay-for-performance for socioeconomic equity.Methods and Findings:
We applied county-level measures of local economic and workforce resources to a national sample of US hospitals (n = 2,705), during the period 2004–2007. We analyzed performance for two common cardiac conditions (acute myocardial infarction [AMI] and heart failure [HF]), using process-of-care measures from the Hospital Quality Alliance [HQA], and isolated temporal trends and the contributions of individual resource dimensions on performance, using multivariable mixed models. Performance scores were translated into net scores for hospitals using the Performance Assessment Model, which has been suggested as a basis for reimbursement under Medicare's “Value-Based Purchasing” program. Our analyses showed that hospital performance is substantially associated with local economic and workforce resources. For example, for HF in 2004, hospitals located in counties with longstanding poverty had mean HQA composite scores of 73.0, compared with a mean of 84.1 for hospitals in counties without longstanding poverty (p<0.001). Hospitals located in counties in the lowest quartile with respect to college graduates in the workforce had mean HQA composite scores of 76.7, compared with a mean of 86.2 for hospitals in the highest quartile (p<0.001). Performance on AMI measures showed similar patterns. Performance improved generally over the study period. Nevertheless, by 2007—4 years after public reporting began—hospitals in locationally disadvantaged areas still lagged behind their locationally advantaged counterparts. This lag translated into substantially lower net scores under the Performance Assessment Model for hospital reimbursement.Conclusions:
Hospital performance on clinical process measures is associated with the quantity and quality of local economic and human resources. Medicare's hospital pay-for-performance program may exacerbate inequalities across regions, if implemented as currently proposed. Policymakers in the US and beyond may need to take into consideration the balance between greater efficiency through pay-for-performance and socioeconomic equity.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 7(6): e32767. doi:10.1371/journal.pmed.1000297
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1000297Summary
Background:
Pay-for-performance is an increasingly popular approach to improving health care quality, and the US government will soon implement pay-for-performance in hospitals nationwide. Yet hospital capacity to perform (and improve performance) likely depends on local resources. In this study, we quantify the association between hospital performance and local economic and human resources, and describe possible implications of pay-for-performance for socioeconomic equity.Methods and Findings:
We applied county-level measures of local economic and workforce resources to a national sample of US hospitals (n = 2,705), during the period 2004–2007. We analyzed performance for two common cardiac conditions (acute myocardial infarction [AMI] and heart failure [HF]), using process-of-care measures from the Hospital Quality Alliance [HQA], and isolated temporal trends and the contributions of individual resource dimensions on performance, using multivariable mixed models. Performance scores were translated into net scores for hospitals using the Performance Assessment Model, which has been suggested as a basis for reimbursement under Medicare's “Value-Based Purchasing” program. Our analyses showed that hospital performance is substantially associated with local economic and workforce resources. For example, for HF in 2004, hospitals located in counties with longstanding poverty had mean HQA composite scores of 73.0, compared with a mean of 84.1 for hospitals in counties without longstanding poverty (p<0.001). Hospitals located in counties in the lowest quartile with respect to college graduates in the workforce had mean HQA composite scores of 76.7, compared with a mean of 86.2 for hospitals in the highest quartile (p<0.001). Performance on AMI measures showed similar patterns. Performance improved generally over the study period. Nevertheless, by 2007—4 years after public reporting began—hospitals in locationally disadvantaged areas still lagged behind their locationally advantaged counterparts. This lag translated into substantially lower net scores under the Performance Assessment Model for hospital reimbursement.Conclusions:
Hospital performance on clinical process measures is associated with the quantity and quality of local economic and human resources. Medicare's hospital pay-for-performance program may exacerbate inequalities across regions, if implemented as currently proposed. Policymakers in the US and beyond may need to take into consideration the balance between greater efficiency through pay-for-performance and socioeconomic equity.
: Please see later in the article for the Editors' SummaryIntroduction
Pay-for-performance is an important market-based approach to improving health care quality. During the past decade, the approach has been adopted widely, by health systems in the UK [1], Australia [2], and Taiwan [3], among others. Pay-for-performance has also been used in the US, but in a piecemeal fashion, in some states, by some insurance firms, for some health care providers [4]. Now a unified effort is underway, with the US government poised to implement pay-for-performance nationwide within its Medicare health insurance program [5],[6]. As the provider of near-universal health insurance to Americans age 65 y and older, Medicare is a powerful driver of US health care policy. For example, Medicare was the innovator in the introduction of hospital prospective payment under the Diagnosis Related Groups [DRGs] program [7]. That payment reform was in turn adopted in the private health insurance sector, and is the standard throughout the US today. Medicare reforms also resonate internationally, as evidenced by the widespread implementation of the DRG case mix approach in 25 nations worldwide [8].
Pay-for-performance assumes that providers have adequate economic and human resources to perform, or improve their performance, within a short time frame. Yet the prevailing distribution of resources in the US health care system makes it difficult for some providers to operate effectively as it is [9]. Payment based on performance may worsen inequalities, as hospitals in underresourced areas lose funds to their better-off counterparts, with the government acting as a sort of “reverse Robin Hood.”
This scenario is not entirely far-fetched. In the US, hospital revenues are largely derived from a mix of private and public health insurance payments, which vary with local socioeconomic conditions [9]. Strong finances give hospitals the opportunity to invest in quality improvement [10]. Hospitals also draw on local human resources. Arguably the most important of these is clinical staff. But not all facilities have access to a high quality talent pool. To date, much research and policy attention has been directed toward attracting physicians, nurses, pharmacists, and other clinicians to areas that would be otherwise underserved, because of local poverty, limited spousal employment opportunities, and sub-par schools [11]–[13].
Moreover, the US—and the world at large—is increasingly segregated, both economically and in terms of educational level [14]–[16]. Demographers in the US have noted a growing concentration of college-educated people in a relatively small subset of geographical areas [16]. This “regional concentration of human capital” has translated into higher productivity in places with more educated workforces, and a decline of economies in areas where this advantage is lacking [17],[18]. Although there is evidence that clinical outcomes vary by geographical area [19], little research has explored the impact of the regional concentration of wealth and human capital on health care.
In this study, we examine the association between local resources and hospital performance, seeking to understand the potential redistribution of funds under an important pending change in hospital reimbursement. We also explore the implications of our findings for health systems beyond the US, as pay-for-performance expands worldwide.
Methods
Setting
The US Medicare program is administered through the Centers for Medicare and Medicaid Services (CMS), a federal governmental agency. Over the past decade, the CMS has piloted pay-for-performance in a variety of settings [6]. Under the agency's ambitious “Value-Based Purchasing (VBP) Initiative,” the first wave of national implementation is slated to take place in hospitals, which will have a portion of their revenues withheld and then returned, conditional on their ability to meet quality targets [6]. Later, the approach will be extended to payment for other types of providers, including physicians, nursing homes, and home health agencies [6].
Groundwork for hospital pay-for-performance was laid when, in 2004, the agency called for hospitals to voluntarily report their performance on process-of-care measures for three clinical conditions (acute myocardial infarction [AMI], heart failure [HF], and pneumonia). Shortly thereafter, the agency began providing financial incentives for reporting, under so called “pay-for-reporting” [20]. The transition was to have been made to hospital pay-for-performance in 2009, but with the change in administration and focus on health care reform, that effort was temporarily suspended. Nonetheless, pay-for-performance enjoys a high degree of support in the agency, the Congress, the hospital industry, and the Obama administration, and is widely expected to be implemented, with the recent passage of health care reform [21].
Data Sources and Sample
The performance data used in this study were derived during Medicare's voluntary reporting period from 2004–2007. Hospitals were eligible for inclusion in the study if they were located in the 50 United States, and voluntarily reported to the Medicare program under the Hospital Quality Alliance [HQA] program during the period. We merged the HQA process-of-care data (which are publicly posted on the program's Hospital Compare website [22]) with data on hospital characteristics and finances from the Medicare Cost Reports [23]. These data were merged with county-level information from the Health Resources and Services Administration's Area Resource File [24].
We used a dataset of institutions reporting at least some HQA data for at least 1 y during the study period. Because a goal of the study was to assess change in all measures over time, we limited the study sample to those hospitals reporting on all seven measures in both 2004 and 2007 (n = 2,705; see below).
Measures
Composite HQA performance score
We used clinical process-of-care measures for AMI and HF, two of the three conditions for which process measures were collected under the HQA throughout the study period. We do not present findings on the third condition (pneumonia), because the initial measures for that condition were controversial and were modified during the study period [25]. However, findings for the pneumonia measures were qualitatively similar to those reported here for AMI and HF, albeit with somewhat attenuated impacts.
Detailed standards for these measures are published elsewhere [26]. Consistent with previous research [27],[28], we selected the following individual measures in developing composite scores: AMI (aspirin on admission, aspirin at discharge, angiotensin converting enzyme [ACE] inhibitor for left ventricular dysfunction, beta-blocker on admission, beta-blocker at discharge); HF (assessment of left ventricular function, ACE inhibitor for left ventricular dysfunction). These are process measures that can be successfully met by physician order or chart notation, including documentation of a contraindication. We excluded measures of the delivery of cognitive services such as smoking cessation counseling that may be sensitive to patient characteristics [29]. For each year, for each of the two conditions, we computed a single weighted average “composite” score, following a standard methodology [30], which assigned each hospital a score ranging from 0 to 100, reflecting the mean hospital performance on a patient receiving the processes of care for which s/he was eligible, for that condition.
Locational resources
We characterized hospital locational resources at the county level across a set of dimensions. Local economic conditions were measured in two ways. First, chronicity of local poverty was assessed using a modified version of a metric developed by the US Department of Agriculture's Economic Research Service [ERS], which identifies counties with respect to their population poverty levels over the past four decennial census periods (1970–2000). “Persistently poor” counties had >20% of their population living in poverty in all four of those census years; “intermittently poor” counties met the >20% criterion during at least one census year; and “never poor” counties never met the >20% poverty level during any of the census years. The current health of the local economy was summarized by the local unemployment rate according to the 2000 census, using the ERS cut point for “high” unemployment (<65% of residents 21–64 y old employed).
Three measures reflected the availability and characteristics of the local workforce. Availability of health professionals was measured using the federal government's Health Professional Shortage Area (Primary Care) (HPSA) designation [31]. The HPSA designation applied to the whole county, a portion of the county, or to no portion of the county. The education level of the local workforce was measured in two ways. The ERS's “low education” designation identifies counties for which >25% of those aged 25–64 y do not have a high school diploma or equivalent, based on the 2000 census [32]. Because the local prevalence of college graduates is the standard measure of workforce human capital used by economic geographers, we also used the proportion of people aged 25 y and over who had completed 4 y of college. For bivariate and multivariable analyses, we divided the sample of hospitals into quartiles on the basis of the prevalence of college graduates in the local county.
For each of the dimensions of locational resources, one resource level was designated “locationally disadvantaged” (persistently poor, high unemployment, entire county designated as HPSA, high prevalence of non-high school graduates in workforce, lowest quartile college educated). Dimensions of advantage/disadvantage were moderately intercorrelated between counties, with unweighted values of Cramer's V ranging from 0.21 (HPSA designation and prevalence of college graduates in the local county) to 0.56 (chronicity of local poverty and high unemployment).
Individual hospital characteristics
Measures of hospital size and ownership were derived from the 2003 Medicare Cost Reports. From the same source, the ratio of interns and residents to beds was used to compute a 3-valued measure of teaching status, with a cut point of 0.10 separating “major” and “minor” teaching institutions, and hospitals with a value of zero designated as “non-teaching” [33]. Location was classified using the Office of Management and Budget's 2003 urban/rural continuum codes, collapsed into three standard categories: “metropolitan,” “micropolitan” (town or small city), and “non-core” (roughly, rural). From the Cost Reports we computed the percent of bed days attributable to Medicaid revenue, and total margin in 2003. Cost Report data were unavailable for 175 (6.4%) of the hospitals. Those institutions were excluded in multivariable analysis.
Attainment, improvement, and net performance score (Performance Assessment Model)
To assess potential redistribution under VBP, we used the Performance Assessment Model that is detailed in Appendix B of CMS's November 2007 Report to Congress [5]. This model is “the methodology that could be used for scoring hospital performance on specific measures” in hospital VBP, according to CMS's January 2009 Roadmap for Implementing Value Driven Healthcare in the Traditional Medicare Fee-for-Service Program [6]. Under the model, hospitals are assigned scaled two scores for each condition annually, one based on attainment (absolute performance) and the other based on improvement (increase in performance from the prior reporting year). A net performance score is then assigned for each condition equal to the attainment or improvement score, whichever is greater.
We assigned these scores to hospitals using the model's “standard” method, as illustrated in Figure 1. To determine the attainment score, for each condition, for each year, there is an attainment range with an upper limit benchmark (the mean of the top decile of performance for all hospitals, for the previous year) and a lower limit attainment threshold (the 50th percentile of performance for all hospitals, for that the previous year). Hospitals at or below the attainment threshold receive 0 attainment points. Those at or above the benchmark receive 10 attainment points. Hospitals performing within the attainment range receive a scaled score between 1 and 9 attainment points. A similar scale methodology generates the improvement score, with the upper benchmark fixed at the same level as for that measure's attainment score. However, the lower threshold is defined differently for every hospital, and is set at the hospital's performance score in the previous period. Thus, the improvement scoring range varies across hospitals, and requires a greater increase in the number of points on the part of previous low-performers than previous high-performers in order to obtain the same scaled score. We also assigned scores using the model's alternative method for “topped-out” measures [5]. Results of our analyses were not significantly changed.
Fig. 1. Performance Assessment Model scoring example (standard method). 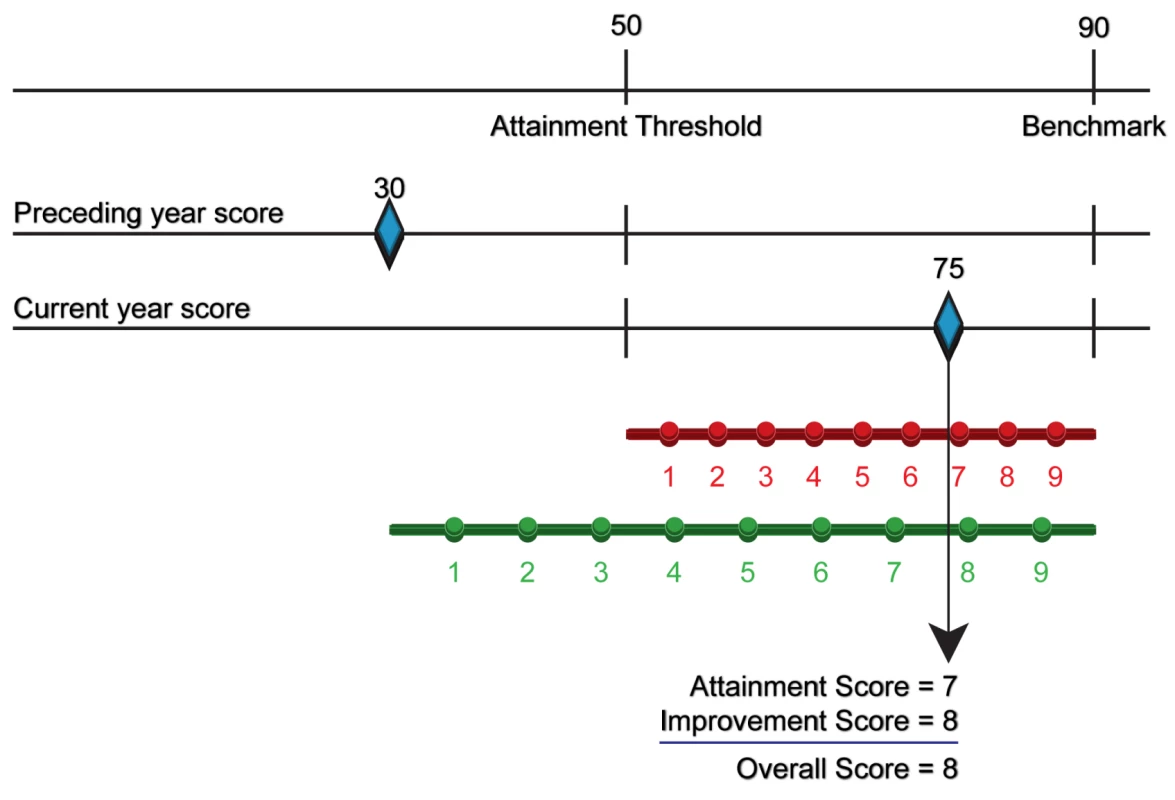
For this example, the attainment threshold is 50 points, and the benchmark is 90 points, based upon hospital performance nationwide during the previous year (see text). This hypothetical hospital received a composite score of 30 during the preceding year, and a score of 75 during the current year. This is converted to attainment and improvement scores, as follows: For the attainment score, the current year score falls in the attainment range, and the hospital is assigned a scaled attainment score of 7. For the improvement score, the current year score falls in the improvement range, and the hospital is assigned a scaled score of 8. The overall score is the larger of the two scores (a value of 8). Figure adapted from the Centers for Medicare and Medicaid Services Report to Congress (2007) [5]. Statistical Analysis
We began by describing the distribution of the sample of hospitals with respect to the individual characteristics and locational resources described above. Then, with hospitals as the units of analysis, we computed mean annual composite HQA performance scores, for each dimension of location, by resource level, and developed 95% confidence intervals (CIs) around each mean. To formally test trends in performance over time, for each condition and dimension, we developed mixed models that included resource level, time, and their interactions as fixed effects, along with random effects of hospital and county, to reflect repeated measures for hospitals and clustering of hospitals within counties. For each condition and dimension, we also assessed differences in mean composite scores, comparing hospitals at the most and the least disadvantaged resource level for that dimension, for the year 2004. These bivariate analyses incorporated robust standard errors to account for the clustering of hospitals within counties. The same set of analyses were conducted for the year 2007.
To assess the independent contributions of the dimensions of location, we developed mixed multivariable models of composite HQA performance score for each condition in 2004 and 2007, entering the locational and hospital characteristics simultaneously as fixed effects, with county as a random effect. We performed regression diagnostics using the approach described by Belsley, Kuh, and Welch [34], and the models performed favorably. Finally, we examined bivariate differences in mean Performance Assessment Model attainment, improvement, and net scores for 2007, for each condition, comparing hospitals at the most and least disadvantaged resource level, within each locational dimension. For these tests, robust standard errors were used to correct for the clustering of hospitals within counties.
We also performed analyses that were weighted for hospital size. Again, the results were quantitatively similar; we present unweighted statistics here.
Results
Although 4,786 different institutions reported HQA data for at least 1 y during the study period, some did not report certain measures during some years. Of the 3,698 hospitals that reported at least one measure of AMI and HF performance in 2004, 3,147 (85.1%) reported on all seven of the measures used in this study in that year, and of those, 2,705 (85.9%) were “complete reporters,” providing data on all seven measures again in 2007. These 2,705 hospitals formed the cohort for the present study. Compared to all hospitals, complete reporters were disproportionately large, had a teaching mission, and were comparatively advantaged in terms of local economy and workforce. Analysis revealed that hospitals that were complete reporters performed at a higher level than noncomplete reporters, within every stratum of the five dimensions of advantage/disadvantage. We performed sensitivity analyses to assess the extent to which the inclusion criteria may have impacted our findings, as reported below.
For most dimensions of locational resources, relatively few of the sample hospitals are in counties with the lowest resource levels (Table 1). For example, only 130 (4.8%) of hospitals are in counties that have been persistently poor in the years 1970–2000, and 231 (8.5%) are in counties with high unemployment. Nevertheless, for some dimensions, a substantial proportion of hospitals are in relatively disadvantaged locations. For instance, 12.5% of hospitals are in areas with a low prevalence of high school graduates, and nearly 25% of hospitals are in areas where fewer than 16.2% of local adults are college graduates. In all, 873 (32.7%) of the hospitals in the sample are in a county that is locationally disadvantaged on at least one dimension.
Tab. 1. US hospitals reporting on all seven HQA measures from 2004 through 2007, according to individual characteristics and locational resource levels. 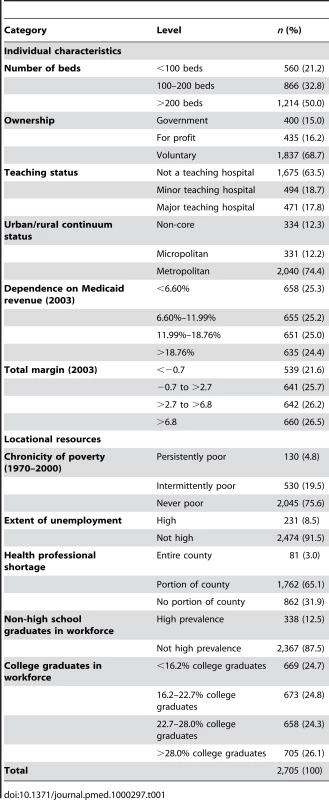
Trends in Performance
There was general improvement in mean composite score over time (for all hospitals, for AMI, 1.62 points/year, 95% CI = 1.55–1.70; for HF, 3.33 points/year, 95% CI = 3.24–3.40).Details of the yearly trends in composite scores for the two conditions are depicted in Figures 2 and 3. The top panels in Figure 2 (Figure 2A and 2B) shows trends defined by baseline (2004) performance quartile. For both conditions, hospitals starting in the lowest quartile showed the most improvement over time (p<0.001 for a comparison of the linear time trend between the first and fourth quartiles, for both conditions), but even by the fourth year of reporting, those in the initial lowest quartile had not reached parity with the other groups (p<0.001 for the difference of means for the first and fourth quartile in 2007, for both conditions). The remaining panels in Figures 2 and 3 display performance trends over time for the five dimensions of locational resources, stratified by resource level. For all five dimensions, hospitals at the most disadvantaged level of resources fared relatively poorly at the outset (p<0.001 for the difference between hospitals at the most and least disadvantaged resource levels for all dimensions, for both conditions), and that significant disadvantage continued, but was attenuated over time (p<0.05 for the difference in linear trend between hospitals at the most and least disadvantaged resource levels, for all dimensions, for both conditions, with the exception of health professional shortage for AMI). By the fourth year of performance reporting, hospitals in disadvantaged areas continued to lag significantly behind their advantaged counterparts (p<0.001 for the difference in means between hospitals at the least and most disadvantaged resource levels for all dimensions, for both conditions) (Table S1).
Fig. 2. Mean composite HQA performance scores (AMI and HF) for US hospitals, 2004–2007, stratified by various characteristics. 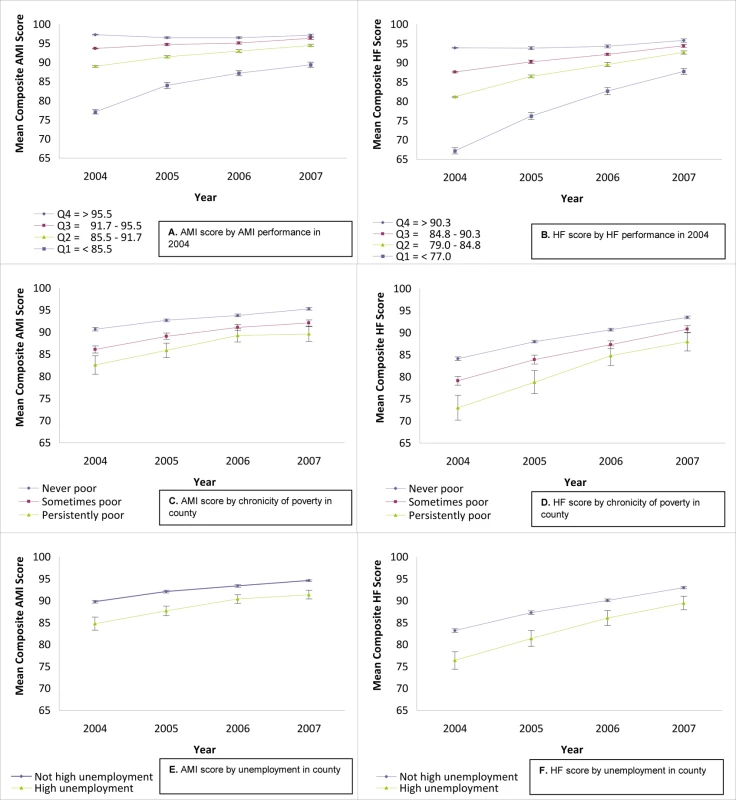
Graphics on the left-hand side (A,C,E) reflect temporal trends in composite performance scores for AMI, and those on the right hand side (B,D,F) reflect temporal trends in composite performance scores for HF. (A and B) show mean composite performance score, stratified by performance quartile in 2004. (C and D) show mean composite performance score, stratified by chronicity of poverty in county. (E and F) show mean composite performance score, stratified by unemployment in county. In (A–F), mean composite scores are presented with 95% CIs. Fig. 3. Mean composite HQA performance scores (AMI and HF) for US hospitals, 2004–2007, stratified by various characteristics. 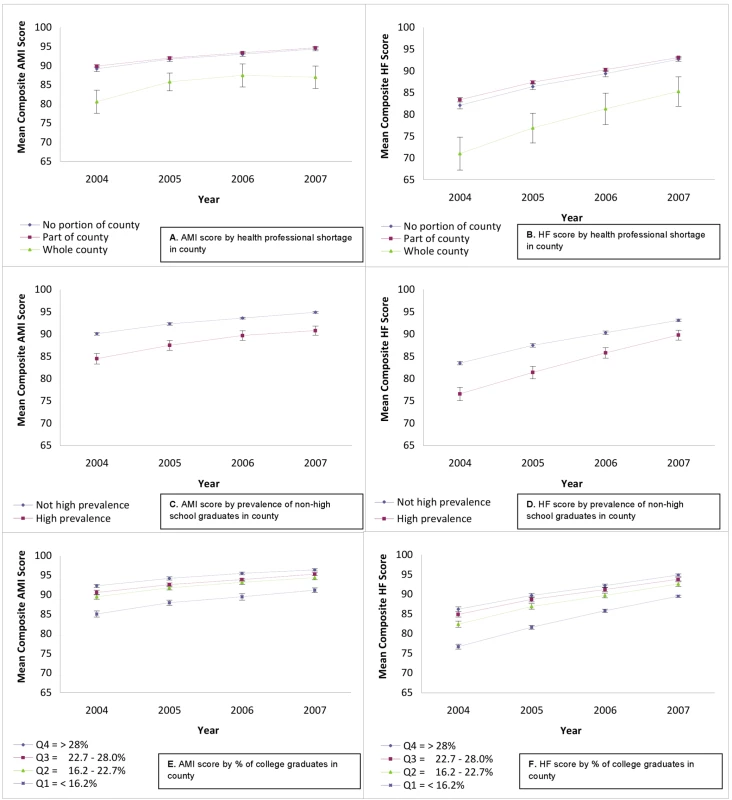
Figure 3 continues the series begun in Figure 2. Again, graphics on the left-hand side (A,C,E) reflect temporal trends in composite performance scores for AMI, and those on the right-hand side (B,D,F) reflect temporal trends in composite performance scores for HF. (A and B) show mean composite performance score, stratified by health professional shortage in county. (C and D) show mean composite performance score, stratified by prevalence of non-high school graduates in county. (E and F) show mean composite performance score, stratified by percent of college graduates in county. In (A–F), mean composite scores are presented with 95% CIs. Multivariable Analysis of Dimensions of Location
The five dimensions of location are conceptually interrelated, and may be correlated with individual hospital characteristics. Table 2 shows the change in composite performance score independently attributable to individual hospital characteristics, and then independently attributable to each locational dimension, expressed as a difference in score between each level and the most locationally advantaged level, within each dimension. The data show consistent independent effects for chronicity of poverty, entire county health professional shortages, and percent college graduates, with levels of chronicity of poverty and percent college graduates in the workforce showing dose-response relationships to performance.
Tab. 2. Independent effects of individual characteristics and locational resource levels on hospital composite performance scores for AMI and HF, 2004 and 2007. 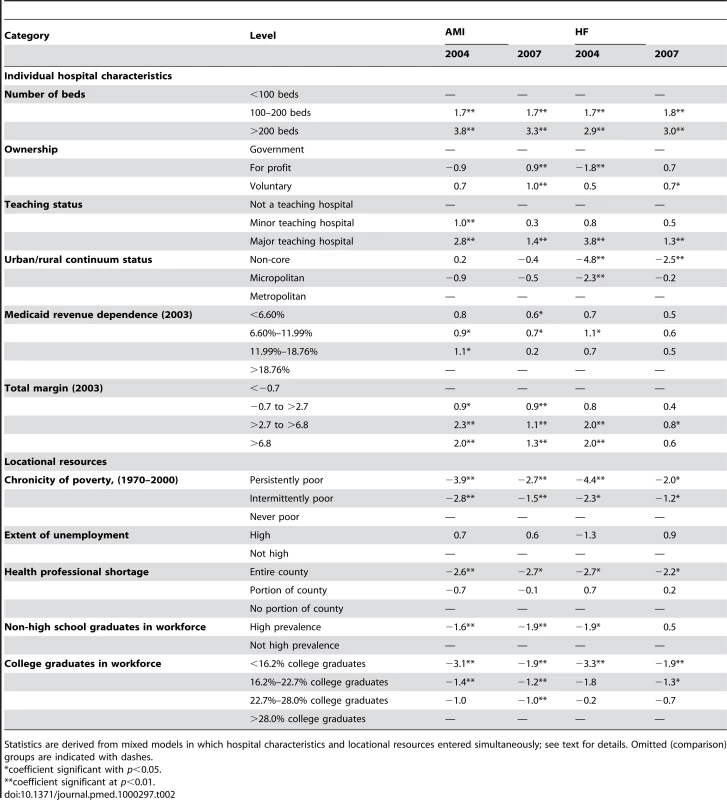
Statistics are derived from mixed models in which hospital characteristics and locational resources entered simultaneously; see text for details. Omitted (comparison) groups are indicated with dashes. Location and Performance Assessment Model Score
Applying the Performance Assessment Model to the 2007 data allowed calculation of attainment, improvement, and net Performance Assessment Model scores (Table 3). Hospitals in more advantaged locations had substantially higher attainment scores (p<0.01 for all five dimensions in both AMI and HF). Hospitals in advantaged locations also had higher improvement scores than their disadvantaged counterparts, though differences in improvement scores were narrower and not all statistically significant (p<0.05 for all dimensions for AMI, but only for chronicity of poverty and college graduates in the workforce for HF). For locationally advantaged hospitals, attainment generally exceeded improvement; the converse was true for disadvantaged hospitals. The net result was that the Performance Assessment Model score–the suggested basis for reimbursement under VBP–was consistently higher for hospitals in the most advantaged locations than those in the least advantaged locations, for both conditions and for all five locational characteristics (p<0.02 for both conditions, all five characteristics).
Tab. 3. Mean Performance Assessment Model scores (attainment, improvement, and net score), by hospital locational resource levels, US Hospitals, 2007. 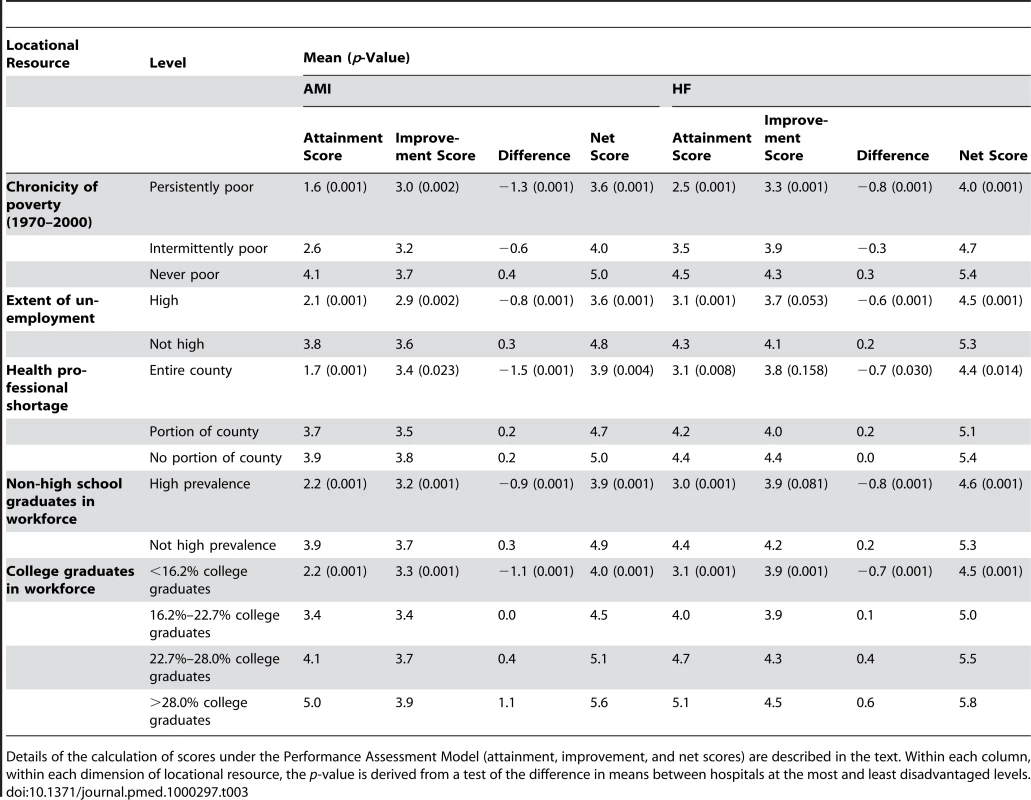
Details of the calculation of scores under the Performance Assessment Model (attainment, improvement, and net scores) are described in the text. Within each column, within each dimension of locational resource, the p-value is derived from a test of the difference in means between hospitals at the most and least disadvantaged levels. Sensitivity of Findings to Inclusion Criteria
To assess the sensitivity of our core findings to our “complete reporters throughout” inclusion criteria, we conducted longitudinal (2004–2007) analyses with the larger sample of hospitals that reported completely in 2004 (n = 3,147), as well as cross-sectional (2007) analyses with complete reporters for AMI in that year (n = 3,074) and HF (n = 3,908). In each case the results were substantially equivalent to those reported here.
Discussion
We found that US hospitals operating in locations with richer economic and human resources attained significantly higher clinical process scores than those located in less advantaged areas during the period 2004–2007. This pattern was evident along several dimensions of the local economy and workforce. Over the study period, hospital performance improved generally, with initially low-performing hospitals showing the greatest increases. Since locationally disadvantaged hospitals were disproportionately low performers initially, they showed more improvement over the 4-y period, and by the end of the study period, disparities by degree of locational advantage had decreased appreciably. Still, by the fourth year of public reporting, locationally disadvantaged hospitals had not achieved scores comparable to their advantaged counterparts.
Our finding of an association between location and performance does not establish causality or specify a mechanism by which the local economy or workforce affect quality. However, it bears emphasis that the association is consistent with research in health management that suggests that effective human and material resources are essential to hospital performance and performance improvement, and that reported performance is only as strong as the weakest link [35]–[40]. Moreover, regardless of the causal history, the fact that better-endowed providers are significantly better performers suggests that pay-for-performance may transfer funds from providers in disadvantaged locations to their better-endowed counterparts. This possibility has international resonance, as is discussed below.
Limitations
We selected our process measures carefully to ensure that variations in hospital performance are unlikely to reflect differences in the characteristics of patients served by hospitals. As noted previously, performance on the measures is satisfied by a physician's order, as documented by a medical records abstractor. For example, in order for a hospital to have succeeded in satisfying the process measure for “administration of an aspirin upon admission,” there need only be an order in a patient record (or documentation of a contraindication) that is reported to CMS. Successfully meeting these criteria does not depend upon a patient action or compliance, and is plausibly independent of patient characteristics. Indeed, the Medicare Payment Advisory Commission (MedPAC) has discussed this matter, and has concluded that risk adjustment for patient characteristics “is not necessary” for these measures [41]. This recommendation is consistent with a recent study that found that performance on the measures used in our study was not consistently associated with patient race/ethnicity, within hospitals [29].
We would not suggest that location is the sole determinant of performance. On the contrary, we found substantial within-county variation in performance, some of which was correlated with hospital characteristics including size, ownership, teaching status, and financial strength. Accounting for within-location variation is beyond the scope of this paper, although it is the focus of some of our ongoing work. On a note related to locational determinism, we would not suggest that hospitals necessarily hire and promote the best of local talent. However, having a strong talent pool from which to draw upon is likely to contribute to organizational strength, all else being equal.
Our estimates of effect should be interpreted with some caution. In measuring and assigning “location,” we used county as the geographic unit for analysis, because it is the unit for which information about the characteristics of interest is readily available. However, locational characteristics of hospitals are not necessarily fully defined at the county level. For example cross-county commuting is common in some areas, with over 25% of US workers nationwide crossing county boundaries to reach their workplace [42]. To the extent that more educated workers are drawn across county lines in order to work at high-performing hospitals, the associations reported here understate the relationship between workforce characteristics and hospital performance. A related caveat pertains to variations in county size and population. Across the US, counties range in size from 67 to 227,556 square km [43]. Some counties are small rural areas; others are entire metropolitan regions. Within large counties, there is likely to be substantial heterogeneity of workforce and economic characteristics. The assignment of average characteristics in such counties is especially imprecise, and as a result our estimates of the impact of location are again likely to be biased downward. To explore this effect, we replicated our analyses, omitting hospitals in counties with populations greater than 1 million, and then again omitting hospitals in counties with populations greater than 500,000. As the sample was restricted to smaller counties, estimates of locational impacts generally increased (analyses not shown).
Other caveats have to do with representativeness and generalizability. As we noted at the outset, locationally disadvantaged institutions were relatively underrepresented in our sample because they were less likely to report consistently to CMS than their better-resourced counterparts. For example, in our sample 4.8% of hospitals were in “persistently poor” counties, but in the nation at-large that figure is 7.5%. Therefore, while our sensitivity analysis did not suggest bias in our estimates of the impact of locational disadvantage, disadvantage is more prevalent than our sample would suggest. In addition, we used process measures of performance for only two clinical conditions. It remains to be seen whether similar trends and patterns will be found, when data are available for other conditions, or for measures of the outcomes of care.
Finally, while our analyses suggest that Medicare's pay-for-performance will transfer funds from poorly resourced to better off areas, we cannot assign dollar values to the transfers that are likely to occur, for several reasons. First, our data derive from a period of public reporting, and the addition of payment incentives may influence provider behavior beyond those changes induced by public reporting. Second, the specifics of payment remain to be determined by the Congress and the CMS. Critical issues include the percent of revenue to be withheld under the scheme, the extent to which that revenue will be returned to providers (rather than retained by the Medicare program [5],[6]) and the translation of performance scores to dollar amounts (the so-called “exchange function” [5]).
Policy Implications
With respect to Medicare, CMS has acknowledged that pay-for-performance may inadvertently worsen the lot of hospitals that “consistently face challenges in improving or maintaining their performance” ([5], p. 85). In its Report to Congress, the agency has outlined plans to monitor the distribution of funds as pay-for-performance is implemented. If some subsets of hospitals are disadvantaged under the payment reform, then those hospitals could be offered training, site visits, and other forms of technical assistance, the agency has suggested. Our work argues for a more proactive approach. Rethinking the way that performance is assessed could help avoid some of the “reverse Robin Hood” consequences that are foreshadowed by our analysis. As we have noted, in its current published form, the Performance Assessment Model credits improvement conditional on starting point. This means that baseline low-attainers must have a greater absolute score increase in order to “improve” as much as baseline high-attainers. Since locationally disadvantaged hospitals are typically baseline low-attainers, they are perforce less likely to be identified as high performers under the model. Changing the model so that it credits improvement regardless of starting point, or assesses improvement over a longer time frame, could help make the program more equitable. It is important to note that the Performance Assessment Model, while referenced in multiple CMS documents as a likely basis for Medicare reform, is still preliminary. Thus, opportunities exist to modify and improve upon the current version. Alternatively, rather than altering the model, CMS may wish to consider comparing hospitals to their similarly located peers, thereby enhancing equity through an “apples-to-apples” comparison. However this strategy carries the risk of institutionalizing inequalities, and finding the right balance may be difficult [44],[45].
Do our findings apply beyond the US? While our specific measures of locational disadvantage may not apply everywhere, there are likely analogs in other settings. For instance, significant health workforce inequalities can be found within and across nations, around the world [46],[47]. These are likely to translate into regional differences in capacities to perform. A recent study in the UK found that general practitioner practices in deprived areas are disproportionately staffed by older physicians, and those who received their medical training outside of the UK [48]. Both of these provider characteristics were associated with poorer practice performance under a pay-for-performance scheme. Deprived areas had a disproportionate share of the lowest performing general practices. In other words, location was linked to performance among UK general practitioners, perhaps through health workforce inequalities. While this remains to be explored in future research, it implies (as does our work) that the pursuit of efficiency through provider accountability may be at odds with pervasive structural inequalities.
Such inequalities can be addressed through countervailing policies. For example, in the UK, geographically targeted approaches have been taken to overcome regional inequalities under “deprivation payment” schemes [49]. In the US, there is no comprehensive strategy to address regional resource inequalities as they might affect health care delivery, although various policies have supported health care in rural areas and in the so-called “safety net,” which includes institutions providing care to low income people [11],[50],[51].
Despite claims that “the world is flat” [52]—that place is irrelevant in a globally networked world—our work suggests that location is a critical input to health care quality. Holding providers accountable is not an unreasonable approach to quality improvement. However, it must be done in a way that attends to the profound inequalities in local circumstances that shape life in the twenty-first century [14].
Supporting Information
Zdroje
1. RolandM
2004 Linking physicians' pay to the quality of care — A major experiment in the United Kingdom. New Engl J Med 351 1448 1454
2. ScottIA
2007 Pay for performance in health care: strategic issues for Australian experiments. Med J Australia 187 31 35
3. ChengT-M
2009 Lessons from Taiwan's universal national health insurance: a conversation with Taiwan's Health Minister Ching-Chuan Yeh. Health Aff 28 1035 1044
4. RosenthalMB
FernandopulleR
SongHR
LandonB
2004 Paying for quality: providers' incentives for quality improvement. Health Aff 23 127 141
5. US Department of Health and Human Services, Centers for Medicare and Medicaid Services 2007 Report to Congress: plan to implement a Medicare hospital value-based purchasing program. November 2007. Available: http://www.cms.hhs.gov/AcuteInpatientPPS/downloads/HospitalVBPPlanRTCFINALSUBMITTED2007.pdf. Accessed 5 November 2008
6. US Department of Health and Human Services, Centers for Medicare and Medicaid Services 2009 Roadmap for implementing value driven health care in the traditional Medicare fee-for-service program. January 9, 2009. Available: http://www.cms.hhs.gov/QualityInitiativesGenInfo/downloads/VBPRoadmap_OEA_1-16_508.pdf. Accessed 8 July 2009
7. MayesR
BerensonRA
2006 Medicare prospective payment and the shaping of U.S. health care Baltimore Johns Hopkins University Press
8. RogerFH
2003 Case mix use in 25 countries: a migration success but international comparisons failure. Int J Med Inform 70 215 219
9. LewinME
AltmanSH
Institute of Medicine (US) Committee on the Changing Market 2000 America's safety net: intact but endangered Washington (D.C.) National Academy Press
10. BazzoliGJ
ClementJP
LindroothRC
ChenH
AydeyeSK
2007 Hospital financial condition and operational decisions related to the quality of care. Med Care Res Rev 64 148 168
11. RickettsTC
2005 Workforce issues in rural areas: a focus on policy equity. Am J Public Health 95 42 47
12. RosenblattRA
AndrillaCHA
CurtinT
HartLG
2006 Shortages of medical personnel at community health centers: implications for planned expansion. JAMA 249 1042 1049
13. American College of Physicians 1995 Rural primary care. Ann Intern Med 122 380 390
14. MasseyDS
1996 The age of extremes: concentrated affluence and poverty in the twenty-first century. Demography 33 395 412
15. World Bank 2005 World Bank development report 2006: equity and development Washington (D.C.) World Bank
16. BerryCR
GlaeserEL
2005 The divergence of human capital level across cities. Papers Region Sci 84 407 444
17. RauchJE
1993 Productivity gains from geographic concentration of human capital: evidence from the cities. J Urban Econ 34 380 400
18. AcsZJ
ArmingtonC
2004 The impact of geographic differences in human capital on service firm formation rates. J Urban Econ 56 244 278
19. KrumholtzHM
MerrillAR
SchoneEM
SchreinerGC
ChenJ
2009 Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circulation cardiovascular quality and outcomes, published online July 9, 2009. Available: http://circoutcomes.ahajournals.org. Accessed 11 July 2009
20. RyanA
2009 Hospital-based pay-for-performance in the United States. Health Econ 18 1109 1114
21. TenenbaumSJ
2009 Pay for performance in Medicare: evidentiary irony and the politics of value. J Health Politics, Policy and Law 35 717 746
22. Hospital Compare Database Available www.hospitalcompare.hhs.gov. Accessed 1 January 2009
23. Medicare Cost Reports (MCR) 2003 US Department of Health and Human Services, Center for Medicare and Medicaid Services. Available: http://www.cms.hhs.gov/CostReports. Accessed 2 May 2009
24. Area Resource File (ARF) 2007 Rockville (Maryland): US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions
25. WachterRW
FlandersSA
FeeC
PronovostPJ
2008 Public reporting of antibiotic timing. Ann Intern Med 149 29 32
26. Centers for Medicare and Medicaid Services and the Joint Commission. Specifications manual for national hospital quality measures. Available: www.qualitynet.org. Accessed 10 October 2009
27. WernerRM
GoldmanLE
DudleyRA
2008 Comparison of change in quality of care between safety-net and non–safety-net hospitals. JAMA 299 2180 2187
28. JhaAK
OravJE
ZhengJ
EpsteinAM
2008 The characteristics and performance of hospitals that care for elderly hispanic Americans. Health Aff 27 528 537
29. Hasnain-WyniaR
BakerDW
NerenzD
FeinglassJ
BealAC
2007 Disparities in health care are driven by where minority patients seek care: examination of the Hospital Quality Alliance measures. Arch Intern Med 67 1233 1239
30. CMS HQI Demonstration Project: composite score methodology overview. Available: http://www.cms.hhs.gov/HospitalQualityInits/downloads/HospitalCompositeQualityScoreMethodologyOverview.pdf. Accessed 30 October 2008
31. Shortage Designation: HPSAs, MUAs & MUPs. Health Resources and Services Administration. Available: http://bhpr.hrsa.gov/shortage. Accessed 30 October 2008
32. US rurality: 2004 typology codes. US Department of Agriculture website. Available: http://www.ers.usda.gov/briefing/rurality/typology/. Accessed 30 October 2008
33. AyanianJZ
WeissmanJS
2002 Teaching hospitals and the quality of care. Milbank Quart 80 267 593
34. BelsleyDA
KuhE
WelschRE
1980 Regression diagnostics: identifying influential data and sources of collinearity New York John Wiley and Sons
35. BradleyEH
CurryLA
WebsterTR
MatteraJA
RoumanisSA
2006 Achieving rapid door-to-balloon times: how top hospitals improve complex clinical systems. Circulation 113 1079 1085
36. BradleyEH
HerrinJ
MatteraJA
HolmboeES
WangY
2005 Quality improvement efforts and hospital performance: rates of beta-blocker prescription after acute myocardial infarction. Med Care 43 282 292
37. BradleyEH
HolmhoeE
MatteraJA
RoumaisSA
RadfordMJ
2001 A qualitative study of increasing beta-blocker use after acute myocardial infarction: why do some hospitals succeed? JAMA 285 2604 2611
38. DevarajS
KohliR
2003 Performance impacts of information technology: is actual usage the missing link? Manage Sci 49 273 289
39. EllerbeckEF
BhimarajA
HallS
2006 Impact of organizational infrastructure on beta blocker and aspirin therapy for acute myocardial infarction. Am Heart J 152 579 584
40. GoldmanLE
HendersonS
DohanDP
TalaveraJA
DudleyRA
2007 Public reporting and pay-for-performance: safety-net hospital executives' concerns and policy suggestions. Inquiry 44 137 145
41. MilgateK
ChengSB
2006 Pay for performance: the MedPAC perspective. Health Aff 25 413 419
42. PisarskiAF
2007 Real numbers: commuting in America. Issues Sci Technol 23 76 80
43. National Association of Counties. An overview of county government. Available: http://www.naco.org/Content/NavigationMenu/About_Counties/County_Government/A_Brief_Overview_of_County_Government.htm. Accessed 20 January 2010
44. CasalinoLP
EsterA
EisenbergA
LewisE
MontgomeryJ
2007 Will pay for performance and quality reporting affect health care disparities? Health Aff 26 x405 w414
45. BlusteinJ
2008 Who is accountable for racial equity in health care? JAMA 299 814 816
46. ChopraM
MunroS
LavisJB
VistG
BennettS
2008 Effects of policy options for human resources for health: an analysis of systemic reviews. Lancet 371 668 674
47. World Health Organization 2009 Report from the joint WHO/AAAH conference on getting committed health workers to underserved areas: a challenge for health systems Geneva WHO. Available: http://whqlibdoc.who.int/hq/2009/WHO_HRH_HMR_2009.06_eng.pdf. Accessed 30 March 2010
48. DoranT
FullwoodC
KontopantelisE
ReevesD
2008 Effect of financial incentives on inequalities in the deliver of primary care in England: analysis of clinical activity indicators for the quality and outcomes framework. Lancet 372 728 736
49. Department of Health, National Health Service General Medical Services 1990 Statement of fees and allowances payable to general medical practitioners in England and Wales from 1 April 1990. London: Department of Health, 1990. Available: http://www.sfa.scot.nhs.uk/. Accessed 20 January 2010
50. Medicare Rural Hospital Flexibility Program. The Social Security Act, Title XVIII, Sections 1814 and 1820. Available: http://www.ssa.gov/OP_Home/ssact/title18/1820.htm. Accessed 30 March 2010
51. Felt-LiskS
GimmG
PetersonS
2007 Making pay-for-performance work in Medicaid. Health Aff 26 w516 w527
52. FriedmanTL
2005 The world is flat: a brief history of the twenty-first century New York Farrar, Straus and Giroux
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2010 Číslo 6- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Antikoagulační léčba u pacientů před operačními výkony
-
Všechny články tohoto čísla
- Studies Needed to Address Public Health Challenges of the 2009 H1N1 Influenza Pandemic: Insights from Modeling
- The Association of Factor V Leiden and Prothrombin Gene Mutation and Placenta-Mediated Pregnancy Complications: A Systematic Review and Meta-analysis of Prospective Cohort Studies
- Evaluating the Quality of Research into a Single Prognostic Biomarker: A Systematic Review and Meta-analysis of 83 Studies of C-Reactive Protein in Stable Coronary Artery Disease
- Gestational Age at Delivery and Special Educational Need: Retrospective Cohort Study of 407,503 Schoolchildren
- Closing the Gaps: From Science to Action in Maternal, Newborn, and Child Health in Africa
- Sub-Saharan Africa's Mothers, Newborns, and Children: How Many Lives Could Be Saved with Targeted Health Interventions?
- Secondary Prevention of Suicide
- The Prevalence and Drug Sensitivity of Tuberculosis among Patients Dying in Hospital in KwaZulu-Natal, South Africa: A Postmortem Study
- Estimating the Global Clinical Burden of Malaria in 2007
- Long-Term Biological and Behavioural Impact of an Adolescent Sexual Health Intervention in Tanzania: Follow-up Survey of the Community-Based MEMA kwa Vijana Trial
- Where to for Sexual Health Education for Adolescents in Sub-Saharan Africa?
- Incidence and Reproduction Numbers of Pertussis: Estimates from Serological and Social Contact Data in Five European Countries
- Hospital Performance, the Local Economy, and the Local Workforce: Findings from a US National Longitudinal Study
- Sub-Saharan Africa's Mothers, Newborns, and Children: Where and Why Do They Die?
- Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT Statement
- Developing ANDI: A Novel Approach to Health Product R&D in Africa
- Maternal Health: Time to Deliver
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Gestational Age at Delivery and Special Educational Need: Retrospective Cohort Study of 407,503 Schoolchildren
- Evaluating the Quality of Research into a Single Prognostic Biomarker: A Systematic Review and Meta-analysis of 83 Studies of C-Reactive Protein in Stable Coronary Artery Disease
- Closing the Gaps: From Science to Action in Maternal, Newborn, and Child Health in Africa
- Secondary Prevention of Suicide
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



