-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Acute Human Lethal Toxicity of Agricultural Pesticides: A Prospective Cohort Study
Background:
Agricultural pesticide poisoning is a major public health problem in the developing world, killing at least 250,000–370,000 people each year. Targeted pesticide restrictions in Sri Lanka over the last 20 years have reduced pesticide deaths by 50% without decreasing agricultural output. However, regulatory decisions have thus far not been based on the human toxicity of formulated agricultural pesticides but on the surrogate of rat toxicity using pure unformulated pesticides. We aimed to determine the relative human toxicity of formulated agricultural pesticides to improve the effectiveness of regulatory policy.Methods and Findings:
We examined the case fatality of different agricultural pesticides in a prospective cohort of patients presenting with pesticide self-poisoning to two clinical trial centers from April 2002 to November 2008. Identification of the pesticide ingested was based on history or positive identification of the container. A single pesticide was ingested by 9,302 patients. A specific pesticide was identified in 7,461 patients; 1,841 ingested an unknown pesticide. In a subset of 808 patients, the history of ingestion was confirmed by laboratory analysis in 95% of patients. There was a large variation in case fatality between pesticides—from 0% to 42%. This marked variation in lethality was observed for compounds within the same chemical and/or WHO toxicity classification of pesticides and for those used for similar agricultural indications.Conclusion:
The human data provided toxicity rankings for some pesticides that contrasted strongly with the WHO toxicity classification based on rat toxicity. Basing regulation on human toxicity will make pesticide poisoning less hazardous, preventing hundreds of thousands of deaths globally without compromising agricultural needs. Ongoing monitoring of patterns of use and clinical toxicity for new pesticides is needed to identify highly toxic pesticides in a timely manner.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 7(10): e32767. doi:10.1371/journal.pmed.1000357
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1000357Summary
Background:
Agricultural pesticide poisoning is a major public health problem in the developing world, killing at least 250,000–370,000 people each year. Targeted pesticide restrictions in Sri Lanka over the last 20 years have reduced pesticide deaths by 50% without decreasing agricultural output. However, regulatory decisions have thus far not been based on the human toxicity of formulated agricultural pesticides but on the surrogate of rat toxicity using pure unformulated pesticides. We aimed to determine the relative human toxicity of formulated agricultural pesticides to improve the effectiveness of regulatory policy.Methods and Findings:
We examined the case fatality of different agricultural pesticides in a prospective cohort of patients presenting with pesticide self-poisoning to two clinical trial centers from April 2002 to November 2008. Identification of the pesticide ingested was based on history or positive identification of the container. A single pesticide was ingested by 9,302 patients. A specific pesticide was identified in 7,461 patients; 1,841 ingested an unknown pesticide. In a subset of 808 patients, the history of ingestion was confirmed by laboratory analysis in 95% of patients. There was a large variation in case fatality between pesticides—from 0% to 42%. This marked variation in lethality was observed for compounds within the same chemical and/or WHO toxicity classification of pesticides and for those used for similar agricultural indications.Conclusion:
The human data provided toxicity rankings for some pesticides that contrasted strongly with the WHO toxicity classification based on rat toxicity. Basing regulation on human toxicity will make pesticide poisoning less hazardous, preventing hundreds of thousands of deaths globally without compromising agricultural needs. Ongoing monitoring of patterns of use and clinical toxicity for new pesticides is needed to identify highly toxic pesticides in a timely manner.
: Please see later in the article for the Editors' SummaryIntroduction
Suicide and deliberate self-harm using pesticides is a major but under-recognised public health problem in the developing world. Each year 250,000–370,000 thousand people die from deliberate ingestion of pesticides [1],[2]. These deaths are responsible for about a third of suicides globally [1]; the World Health Organization (WHO) now recognizes pesticide poisoning to be the single most important means of suicide worldwide [3].
Within the rural developing world, high levels of pesticide use with storage at home increases the risk of acute poisoning [4]. One strategy to reduce mortality is to restrict access to more toxic pesticides [5]. As a first line, countries should follow Food and Agriculture Organization (FAO) advice [6] and withdraw the most toxic WHO/US Environmental Protection Agency (EPA) class I pesticides (see Table 1 for description of toxicity classifications) from agricultural practice. Further efforts can range from educating farmers in the use of safer pesticides to imposing regulatory restrictions on the sale and distribution of the most toxic class II pesticides [7],[8]. These strategies would be aided if countries developed pesticide policies that balanced agricultural and economic needs against the public health impact of acute and chronic human toxicity [9]. The development of such a policy should be iterative and based on evidence about which pesticides are major public health concerns [1].
Tab. 1. WHO classification of toxicity <em class="ref">[18]</em>. ![WHO classification of toxicity <em class="ref">[18]</em>.](https://www.prolekare.cz/media/cache/resolve/media_object_image_small/media/image/40aff55ef4f46093d11f4bb6c45fa772.png)
Unfortunately, at present, regulatory decisions are based on a classification of pesticide toxicity that is largely based upon rat oral LD50s. The scientific basis for extrapolating this classification to human poisoning with class II pesticides is weak. Rodents handle xenobiotics differently to humans [10]; as an example, they have greater capacity for metabolic detoxification of organophosphates [11]. And unlike human patients receiving intensive care, they do not receive any treatment in the toxicity studies. It is therefore not clear that a pesticide with low toxicity in rodents should be safe in humans and vice versa.
Information on the acute human toxicity of a wide range of pesticides is needed to complement the animal toxicity data. We therefore set up a prospective cohort of intentional pesticide-poisoned patients admitted to two Sri Lankan hospitals to study the relative toxicity of formulated pesticides in humans. Sri Lanka is an ideal location for this research. Ahead of the FAO recommendations, it has banned all WHO/EPA class I pesticides leaving just class II and III pesticides in agricultural use. Other Asian countries are slowly following suit—within a few years class I pesticides will no longer be used. Therefore, the current situation in Sri Lanka represents the future situation in other Asia countries. Furthermore, because only class II and III pesticides are used in Sri Lanka, the great majority of deaths from pesticide poisoning occur in the secondary referral study hospitals [12],[13]. Bias from prehospital deaths is minimized.
Methods
Ethics Statement
Ethics approval for this data collection has been obtained from Oxfordshire Clinical Research Ethics Committee, Oxford Tropical Medicine Ethics Committee, Colombo University Faculty of Medicine Ethics Committee, Sri Lankan Medical Association, University of Peradeniya, and the Australian National University.
Patients
This was a prospective observational cohort study of patients aged greater than 12 y with deliberate ingestion of a single pesticide who presented to two Sri Lankan rural referral hospitals for an agricultural provincial district of 1.1 million people. The poison ingested was determined from the history given by the patient or relatives, the hospital transfer letter, or from the pesticide bottle if it accompanied the patient. Patients who deliberately ingested more than one substance (except for alcohol) were excluded from this study. Patients were either direct admissions to the study hospital or transfers from smaller primary hospitals. Patient recruitment commenced on 31 March 2002 in Anuradhapura Hospital and 4 June 2002 in Polonnaruwa Hospital. Details of the referring hospital name were documented from 1 June 2006. Data analysis was performed on all patients who had been enrolled up until 17 November 2008.
All patients were enrolled into the cohort at admission by full-time study doctors employed as clinical research assistants. Clinical care followed a standard protocol that emphasized identifying patients poisoned by pesticides that would likely respond to antidotes, in particular organophosphorus (OP) and carbamate insecticides [14]. All patients were seen regularly at least every 4 h. Significant events (intubation, seizures, death) were recorded prospectively. Patients were also seen on a study ward round twice each day and their condition over the previous 12 h recorded. Patients remained under the care of the hospital consultant physicians. Decisions about medical treatment, intubation, and transfer of patients to intensive care were made solely by the hospital staff on the basis of the patient's clinical condition, and independently of the research team.
Statistics
Case fatality was defined as the proportion of deaths over admissions for any given pesticide. Odds ratios (ORs) and the 95% confidence intervals (CIs) of the proportions were calculated using the binomial exact method [15]. The binomial exact method will generate a one-sided CI (97.5% CI) when the proportion of deaths over admissions for a given pesticide is zero.
Logistic regression was used to calculate unadjusted and adjusted (for age and gender) ORs for death relative to the pesticide most commonly ingested (chlorpyrifos).
The potential effect of recently implemented pesticide bans was examined assuming proportional redistribution based upon existing distribution of poisoning across the class after excluding patients who had taken unidentified pesticides. Sensitivity analyses were undertaken by assuming complete redistribution to the next most toxic substitute and to the least toxic substitute.
Results
During the study period, 9,302 patients were admitted following deliberate ingestion of a single pesticide. The pesticide ingested could be identified by history in 7,461 patients; a further 1,841 had ingested an unknown pesticide. Within the unknown group, 497 were considered to have taken a cholinesterase inhibitor (either an OP or carbamate insecticide) on the basis of a typical anticholinesterase clinical syndrome, significant atropine requirement, and/or measured cholinesterase inhibition. A total of 808 patients, whose ingested pesticide was identified by history, had admission samples assayed for other nested studies; history correctly identified the ingested poison in 94.7% of these patients, the other 5.3% were not necessarily misclassifications (more likely to be simply below the level of assay detection). In a subset of the cohort we have also previously shown that analytical assay confirmed history in 92% of symptomatic patients with organophosphate poisoning [16].
The patients were predominately male (67%) and young; the median age was 28 y (interquartile range [IQR] 21–40). The median time to admission to the study hospitals following ingestion was 4 h (IQR 3–7).
The case fatality for the most commonly ingested pesticides is presented in Table 2. The overall mortality for pesticide self-poisoning (including patients who had ingested an unidentified pesticide) was 10.1% (CI 9.5–10.8). From 1 June 2006, 2,608 patients were admitted with a single pesticide ingestion; mortality was 8.9% (61/678) for direct study hospital admissions compared with 7.8% in patients transferred from primary rural hospitals. As 12% of all primary hospital deaths occur in the primary hospitals, there was no clear difference in overall mortality for patients who first presented to a primary rural hospital compared with those presenting to a referral study hospital. Anticholinesterase insecticides and the herbicides paraquat, MCPA, propanil, and glyphosate accounted for 94% of admissions and 98% of deaths. For those ingesting an identified pesticide, just three compounds with relatively high case fatality (paraquat, dimethoate, fenthion) were responsible for 17.6% of total admissions but 47% of the total deaths.
Tab. 2. Case fatality of any pesticide with more than ten admissions or any death. 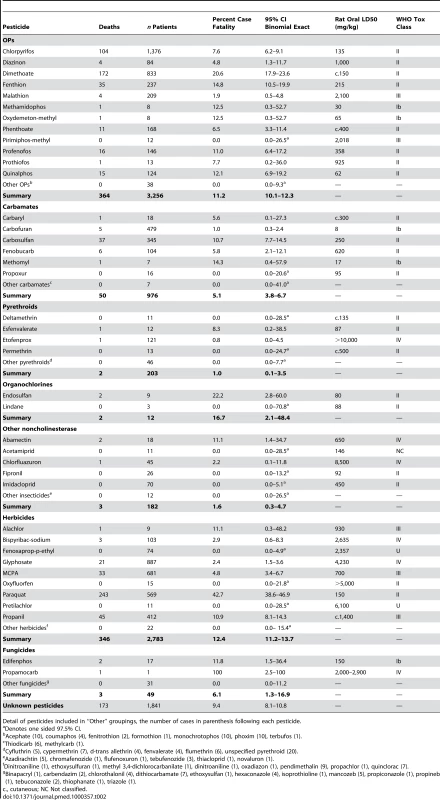
Detail of pesticides included in “Other” groupings, the number of cases in parenthesis following each pesticide. There was a very wide range of lethal toxicity for compounds within the same pesticide classes (e.g., OP insecticides) or with the same agricultural indication (e.g., nonselective herbicides). For example the risk ratio for death after ingestion of the OP insecticides dimethoate versus chlorpyrifos was 2.7 (CI 2.2–3.4) and for the herbicides paraquat versus glyphosate was 18.1 (CI 11.7–27.6). These risk ratios confirm significant differences in pesticides that are in the same WHO class for risk (Figure 1; Table 2) and have comparable agricultural efficacy. There was marked variation in case fatality for OPs with similar LD50s, emphasizing the limited usefulness of animal toxicity data to drive human regulatory decisions (Table 2).
Fig. 1. Plot of case fatality for different pesticides grouped by WHO class. 
Increasing age and male sex was significantly associated with a fatal outcome. However, adjustment for these factors did not result in any major changes in the relative toxicity assessment. For example, the odds of dying from paraquat ingestion was 9.1 (95% CI 7.0–11.8) times that of chlorpyrifos (reference group). When adjusted for age and gender the relative risk of dying from paraquat was moderately greater (OR 15.4; 95% CI 11.6–20.4). Similar moderate increases in ORs were seen for dimethoate and fenthion after adjustment (Table 3).
Tab. 3. Logistic regression of odds of a fatal outcome for each pesticide before and after adjustment for gender and age. 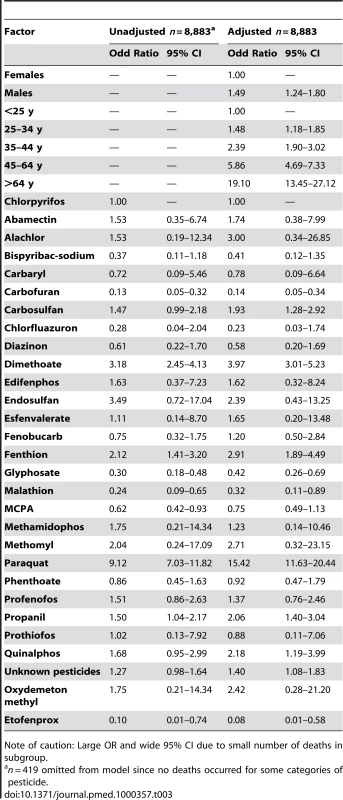
Note of caution: Large OR and wide 95% CI due to small number of deaths in subgroup. The potential effect on mortality of banning the three most lethal pesticides and assuming best and worst case substitutions suggests a reduction in overall pesticide case fatality of between 33% and 65%. The actual fall in case fatality seen after withdrawal of these pesticides will therefore depend substantially on which pesticides replace them in the market (Table 4).
Tab. 4. Modeling the potential effect of dimethoate, fenthion, and paraquat bans in an equal size cohort (7,461 patients with known pesticidea ingestion). 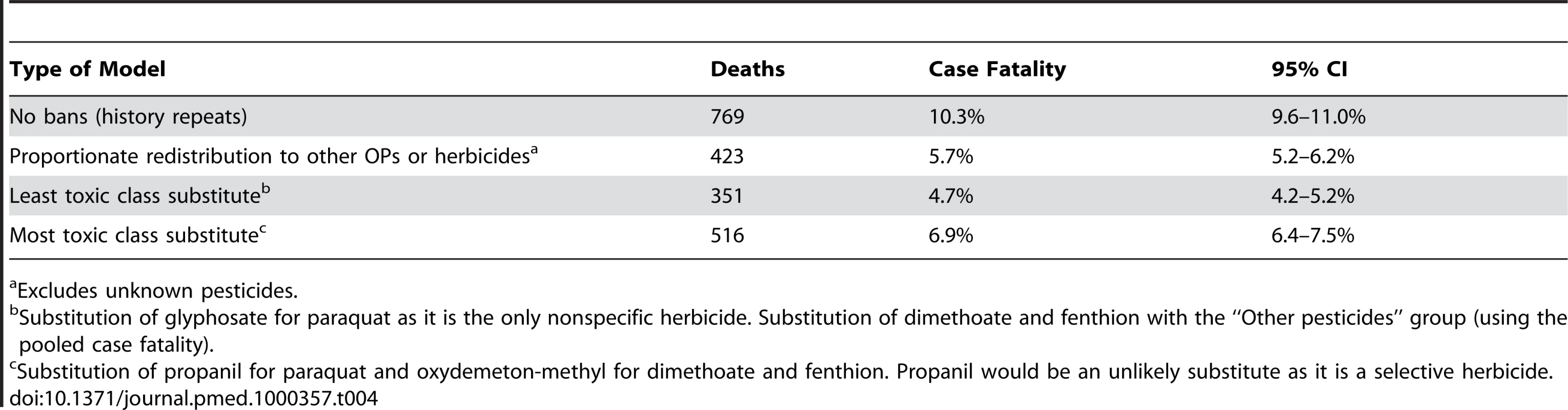
Excludes unknown pesticides. Discussion
This study demonstrates major differences in human case fatality between pesticides that are used for similar agricultural indications. These are the first systematically collected prospective human data, to our knowledge, that allow estimates of relative toxicity for pesticides. The data are much more directly relevant to human risk assessment than the existing animal data from which the WHO/EPA classifications of toxicity used in regulation are derived. Moreover, it provides evidence of very large differences in acute human toxicity within these widely used classifications. These data provide a basis for refining further public health, regulatory, and clinical responses to the problem of acute pesticide poisoning.
Public Health Implications
In regions where pesticide poisoning is a public health problem, pesticide use must be considered in the context of a societal need that balances agricultural benefits with the costs related to human toxicity. Ideally, this requires human toxicity data to be incorporated into regulatory decision making.
This study supports previous observations of the mismatch of human toxicity with animal LD50s for OP insecticides [16],[17]. The current WHO/EPA classification is linked to a number of regulatory mechanisms designed to minimize human risk from pesticides on the basis of occupational or unintentional exposure to pesticides [18]. However, the most important current public health problem of pesticides is deliberate rather than unintentional exposure [19]. There is also an overlap between the two in terms of plausible exposure, and therefore acute self-poisoning data also provide substantial information for risk assessment in unintentional exposure.
The criteria for the classifications have provision for the inclusion of other data to supplement the existing standard means of determining classification based on animal data: “Provision is made for the classification of a particular compound to be adjusted if, for any reason, the acute hazard to man differs from that indicated by LD50 assessments alone” [18]. The data reported here provide a strong argument for utilizing acute human toxicity data in the existing classification scheme that would be a better guide for national regulatory and promotional policy.
The societal and policy question is what threshold should be adopted to move compounds from a class II (moderately hazardous) status to class 1a (extremely hazardous) or class 1b (highly hazardous) status at which point these compounds would fall under the scrutiny of international regulatory guides and agreements. We have previously suggested that a human case fatality of less than 10% using treatments that are widely available and inexpensive could be the threshold for classification of a pesticide formulation into class II [8].
Alternatively, rather than arbitrarily setting a threshold, benchmarking could utilize data on a range of class I agents. In a retrospective Indian study, class I pesticides had case fatality ranging from 17% to 60%, and no class II pesticides were in this range [17]. Thus one might set the threshold at a human case fatality of less than 15% to remain in class II. From a public health perspective it seems irrational for pesticide formulations with estimated case fatalities of 21% (dimethoate EC40), 22% (endosulfan EC35), and 47% (paraquat 20%) to be in the same (moderately hazardous) WHO class as many pesticides with a 20-fold lower human case fatality (see Table 2, case fatality for other class II pesticides cluster in the range 0% to 12.5%).
The public health impact of such a change in classification is supported by past experience of pesticide restriction. In Sri Lanka, the withdrawal of all class I pesticides in the years leading up to 1995 and withdrawal of endosulfan in 1998 coincided with a halving of the number of suicides and even greater reduction in fatal poisonings [7],[20]. These pesticide restrictions were introduced without any adverse effects on agricultural costs or output [21]. In January 2008, the data presented within this paper combined with other studies [22] underpinned a Sri Lankan government policy decision to withdraw paraquat, dimethoate, and fenthion from the Sri Lankan market. Our analysis (Table 3) suggests the decision to withdraw these three pesticides is likely to lead to a further 33% to 65% reduction in deaths from acute poisoning. On the basis of Sri Lankan 2005 figures for deaths from poisoning, this action should translate to a reduction in suicide deaths by about 1,000 lives per year [7]. Similar regulatory activities across Asia would likely reduce the suicide rate in the region by more than 30% contributing to a substantial fall in the global number of suicides.
Clinical Implications
The large variation in mortality within OP and carbamate pesticides suggests variation in toxicokinetics and/or dynamics for compounds that are often regarded as requiring the same medical management [16]. Clinical implications of significant variability within a toxicological class include the need for a more complex risk assessment for individual patients and perhaps specific treatment protocols for individual agents [16]. Previous analysis of the relative toxicity of just three OP insecticides (chlorpyrifos, dimethoate, and fenthion) demonstrated large difference in the time course of toxicity, kinetics and dynamics of the pesticide, and mode of death [16]. Better understanding of factors that are associated with higher mortality will allow clinicians to triage and manage patients more effectively. While this analysis has focused simply upon differences in case fatality, further studies are required to provide more detail on the clinical course of high risk poisonings.
Effects of Resource Limitations in Rural Asian Hospitals
The limited treatment resources in Sri Lankan primary referral hospitals might have increased case fatality [23]. However, such limitations are the norm throughout the developing world. For example, propanil's case fatality of 11% is unexpectedly high for an agent whose toxicity is largely due to methaemoglobinaemia and haemolysis, complications that should be relatively easily treated [24]. However, the difficulty in monitoring treatment response without cooximeters and problems with access to and dose adjustment of the antidote have all been suggested as major contributory causes to the high case fatality [24]. Previous studies have also documented high complication rates from gastrointestinal decontamination in rural hospitals that may increase mortality [25]. Other issues identified in primary hospitals that could impact on care include lack of medication, equipment, and staffing [23]. Resource restrictions are less likely to have an effect on case-fatality estimates for highly toxic pesticides such as paraquat that have no proven effective treatment [22],[26].
These two study hospitals received additional resources in the form of medically qualified research assistants and additional monitoring equipment. These and standardized treatment protocols would be expected to have contributed to a generally lower case fatality than other rural hospitals [27],[28], and thus we believe the estimates of actual lethality and the potential impact of further regulation are both conservative. In addition, for 3 y of this study, dimethoate and fenthion were banned in approximately 25% of the province, contributing to an underestimate of the effects of more widespread pesticide restriction.
Effect of Pesticide Formulation
For some pesticides in particular, mortality may not be just related to the intrinsic toxicity and whether effective antidotes have been developed. Formulation differences can be important. The acute toxicity of the class I agent carbofuran is far higher (rat oral LD50, 8 mg/kg) than the related carbosulfan (250 mg/kg). However, carbofuran has remained on the market as it is sold as 3% granules and therefore has significantly lower case fatality than carbosulfan that is formulated as a 25% emulsifiable concentrate liquid. The benefits of this formulation change have been attenuated by farmers using the granules “off label” to produce a solution. The OP quinalphos has the highest acute rat toxicity of any OP sold in Sri Lanka; as a result, it is formulated at a lower concentration (25%) than most other OPs (40%–50%) to bring its predicted toxicity down. Unfortunately, changes in formulation for paraquat have not led to clinically significant reductions in case fatality [22]. Formulation changes have not yet been attempted for other pesticides.
Comparison with Other Research Studies
There are no other comparable prospective studies of pesticide mortality but previous retrospective studies support our key conclusion that pesticides used for the same agricultural need have very important differences in acute human toxicity.
A retrospective study in South India of 8,040 pesticide ingestion showed an overall mortality from OP insecticides of 22% [17] compared to 11.1% in this study (Table 2). The majority of deaths were due to the class I OP monocrotophos, which had a case fatality of 35%. Similar data have been reported from a retrospective poison center study in Taiwan [29]. Class I OPs in these studies showed higher mortality than all of the class II or III OPs in our study with the exception of dimethoate. While the overall mortality in our cohort was much lower, the results for the few pesticides that were common to these studies were similar despite the different setting; the case fatality in the Indian study was chlorpyrifos (6%), quinalphos (12%), and endosulfan (28%), and in the Taiwan study was chlorpyrifos (4.4%), dimethoate (16.6%), and fenthion (15.3%).
These studies provide strong support for our contention that these results are representative of typical poisonings in the region. However, since relatively few pesticides overlapped, there is a clear need for more large, prospective cohort studies in the region to inform pesticide regulation across the full range of pesticides in agricultural use.
Limitations
The most important limitation of our data is that they were collected from just two rural referral hospitals in one country. However, these hospitals are likely to be representative for many rural hospitals in the developing world where resources may be restricted. Although data were collected from within one country, the pattern of agriculture and related pesticide requirements within the study area are similar to much of rural Asia [30].
Since Sri Lanka has already banned some pesticides (notably all WHO class I pesticides [31]), these data do not include some WHO class I pesticides (such as parathion and monocrotophos) that are still manufactured and available in other countries of the region. The limited human data on such agents suggest they are more toxic than most of the pesticides in our study [29]. It is likely that any country developing a policy based upon including pesticides of minimum risk in acute exposure would first attempt to regulate these class 1 agents.
Another potential limitation is that these data on deaths and poisonings were recorded from secondary referral hospitals. Deaths at home, in primary hospitals, and during transfers will affect both the numerator and denominator of the observed case fatality. Surviving patients not transferred will only reduce the denominator. Data collected for a previous study of all injury in the province identified only 3.8% of deaths from pesticides occurring outside the health system (Table S1) [32]. Our data would not include patients who took trivial nontoxic ingestions of agrochemicals and did not subsequently present for medical treatment. If this occurred it should be more common with the least toxic pesticides and thus to reduce differences observed between agents. It thus could not explain the very large differences in relative toxicity we observed.
We examined primary hospital mortality within two subsets of this cohort. In a small study of 260 patients done in 2002 from within this cohort, 80% of deaths occurred after transfer [12]. Of 471 patients presenting with pesticide poisoning to peripheral hospitals in a 6-mo period in 2005, just three patients died in the peripheral hospital compared to 32 patients dying after transfer. 77% of organophosphate, 84% of carbamate, and 90% of paraquat poisoned patients were transferred to the study hospitals (Table S2) [13].
We prospectively examined all poisonings presenting to all primary hospitals (n = 30) and referral hospitals between September 2008 and December 2009 as part of an RCT of primary hospital educational intervention (ISRCTN73983810). 1,158 people with pesticide poisoning presented to the primary rural hospitals; 77% of these patients were transferred to the referral hospitals. A total of 72 deaths occurred within this group, nine deaths were in the primary hospital, and 63 deaths in referral hospital. (Table S3). Median time to presentation in this study was 55 min (IQR 30–110).
As most deaths occur following referral it is unlikely that patients kept in primary hospitals and not referred would substantially change the overall or relative case fatality. Any bias from nonreferral of less severely poisoned patients would lead to overestimation of toxicity for the least toxic pesticides. None of the data presented (Tables S1, S2, S3) suggests any systematic difference in pesticides causing death in the referral hospital compared with prereferral (primary hospitals and home). Thus this potential referral bias could not explain the very large differences in case fatality between pesticides that we found.
Future research
It is possible that other pesticides with apparently low case fatality based on small numbers may later emerge as important agents in poisoning as their agricultural use in rural Asia increases [20]. This possibility mandates a need for ongoing “toxico-vigilance” studies to follow any change in regulation. It is possible that examination of other important but nonfatal clinical outcomes may also help provide better estimates of the likely human fatal toxicity for these agents. While it is intuitive that a poisoning that never causes symptoms is less likely to be lethal than one that has caused major complications, but no deaths, the methodology for quantifying this hypothesis has not been developed.
Conclusion
There is marked variation in human lethality from acute poisoning within the existing pesticide classifications. Accounting for this in promotional, regulatory, and clinical decision making is likely to have a major impact upon overall mortality from suicide with pesticides and global suicide numbers.
Supporting Information
Zdroje
1. GunnellD
EddlestonM
PhillipsMR
KonradsenF
2007
The global distribution of fatal pesticide self-poisoning: systematic review.
BMC Public Health
7
357
2. GunnellD
EddlestonM
2003
Suicide by intentional ingestion of pesticides: a continuing tragedy in developing countries.
Int J Epidemiol
32
902
909
3. BertoloteJM
FleischmannA
EddlestonM
GunnellD
2006
Deaths from pesticide poisoning: a global response.
Br J Psychiatry
189
201
203
4. EddlestonM
KarunaratneA
WeerakoonM
KumarasingheS
RajapaksheM
2006
Choice of poison for intentional self-poisoning in rural Sri Lanka.
Clin Toxicol (Phila)
44
283
286
5. EddlestonM
BuckleyNA
GunnellD
DawsonAH
KonradsenF
2006
Identification of strategies to prevent death after pesticide self-poisoning using a Haddon matrix.
Inj Prev
12
333
337
6. FAO
2003
International code of conduct on the distribution and use of pesticides
Rome
FAO
9251049149 9251049149
7. GunnellD
FernandoR
HewagamaM
PriyangikaWD
KonradsenF
2007
The impact of pesticide regulations on suicide in Sri Lanka.
Int J Epidemiol
36
1235
1242
8. DawsonA
BuckleyN
2007
Integrating approaches to paraquat poisoning.
Ceylon Med J
52
45
47
9. EddlestonM
KarallieddeL
BuckleyN
FernandoR
HutchinsonG
2002
Pesticide poisoning in the developing world–a minimum pesticides list.
Lancet
360
1163
1167
10. WrightonSA
StevensJC
1992
The human hepatic cytochromes P450 involved in drug metabolism.
Crit Rev Toxicol
22
1
21
11. TangJ
CaoY
RoseRL
BrimfieldAA
DaiD
2001
Metabolism of chlorpyrifos by human cytochrome P450 isoforms and human, mouse, and rat liver microsomes.
Drug Metab Dispos
29
1201
1204
12. EddlestonM
SudarshanK
SenthilkumaranM
ReginaldK
KarallieddeL
2006
Patterns of hospital transfer for self-poisoned patients in rural Sri Lanka: implications for estimating the incidence of self-poisoning in the developing world.
Bull World Health Organ
84
276
282
13. SenarathnaL
2006
How the level of resources and hospital staff attitude in primary care hospitals in rural Sri Lanka affect poisoning patient outcome
University of Newcastle
Available: http://www.sactrc.org/thesis.html Accessed 15 July 2010
14. EddlestonM
DawsonA
KarallieddeL
DissanayakeW
HittarageA
2004
Early management after self-poisoning with an organophosphorus or carbamate pesticide - a treatment protocol for junior doctors.
Crit Care
8
R391
397
15. DeanAGSK
SoeMM
2008
OpenEpi: open source epidemiologic statistics for public health, version 2.2.1.
www.OpenEpi.com. 2.2.1 ed. Accessed 10 August 2009
16. EddlestonM
EyerP
WorekF
MohamedF
SenarathnaL
2005
Differences between organophosphorus insecticides in human self-poisoning: a prospective cohort study.
Lancet
366
1452
1459
17. Srinivas RaoC
VenkateswarluV
SurenderT
EddlestonM
BuckleyNA
2005
Pesticide poisoning in south India: opportunities for prevention and improved medical management.
Trop Med Int Health
10
581
588
18. WHO
2005
The WHO recommended classification of pesticides by hazard and guidelines to classification 2004
Geneva
World Health Organisation
19. KonradsenF
van der HoekW
GunnellD
EddlestonM
2005
Missing deaths from pesticide self-poisoning at the IFCS Forum IV.
Bull World Health Organ
83
157
158
20. RobertsDM
KarunarathnaA
BuckleyNA
ManuweeraG
SheriffMH
2003
Influence of pesticide regulation on acute poisoning deaths in Sri Lanka.
Bull World Health Organ
81
789
798
21. ManuweeraG
EddlestonM
EgodageS
BuckleyNA
2008
Do targeted bans of insecticides to prevent deaths from self-poisoning result in reduced agricultural output?
Environ Health Perspect
116
492
495
22. WilksMF
FernandoR
AriyanandaPL
EddlestonM
BerryDJ
2008
Improvement in survival after paraquat ingestion following introduction of a new formulation in Sri Lanka.
PLoS Med
5
e49
doi:10.1371/journal.pmed.0050049
23. SenarathnaL
AdamsJ
De SilvaD
BuckleyNA
DawsonAH
2008
Personal and professional challenges in the management of deliberate self-poisoning patients in rural Sri Lanka: a qualitative study of rural hospital doctors' experiences and perceptions.
BMC Public Health
8
373
24. EddlestonM
RajapaksheM
RobertsD
ReginaldK
Rezvi SheriffMH
2002
Severe propanil [N-(3,4-dichlorophenyl) propanamide] pesticide self-poisoning.
J Toxicol Clin Toxicol
40
847
854
25. EddlestonM
HaggallaS
ReginaldK
SudarshanK
SenthilkumaranM
2007
The hazards of gastric lavage for intentional self-poisoning in a resource poor location.
Clin Toxicol (Phila)
45
136
143
26. EddlestonM
WilksMF
BuckleyNA
2003
Prospects for treatment of paraquat-induced lung fibrosis with immunosuppressive drugs and the need for better prediction of outcome: a systematic review.
QJM
96
809
824
27. EddlestonM
BuckleyNA
EyerP
DawsonAH
2008
Management of acute organophosphorus pesticide poisoning.
Lancet
371
597
607
28. RobertsDM
AaronCK
2007
Management of acute organophosphorus pesticide poisoning.
BMJ
334
629
634
29. LinTJ
WalterFG
HungDZ
TsaiJL
HuSC
2008
Epidemiology of organophosphate pesticide poisoning in Taiwan.
Clin Toxicol (Phila)
46
794
801
30. JoshiPK
GulatiA
BirthalPS
TewariL
2003
Agriculture diversification in South Asia: patterns, determinants, and policy implications.
Econ Polit Wkly
39
2457
2467
31. GunnellD
FernandoR
HewagamaM
PriyangikaW
KonradsenF
2007
The impact of pesticide regulations on suicide in Sri Lanka.
Int J Epidemiol
36
1235
1242
32. EddlestonM
UdayakumaraN
AdhikariS
de SilvaD
SheriffMH
2007
The importance of poisoning vs. road traffic injuries as a cause of death in rural Sri Lanka.
PLoS One
2
e599
doi:10.1371/journal.pone.0000599
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2010 Číslo 10- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
-
Všechny články tohoto čísla
- Systematic Evaluation of Serotypes Causing Invasive Pneumococcal Disease among Children Under Five: The Pneumococcal Global Serotype Project
- The Persisting Burden of Intracerebral Haemorrhage: Can Effective Treatments Be Found?
- Conflicts of Interest at Medical Journals: The Influence of Industry-Supported Randomised Trials on Journal Impact Factors and Revenue – Cohort Study
- An Urgent Need to Restrict Access to Pesticides Based on Human Lethality
- A Field Training Guide for Human Subjects Research Ethics
- Oral Ondansetron Administration in Emergency Departments to Children with Gastroenteritis: An Economic Analysis
- Being More Realistic about the Public Health Impact of Genomic Medicine
- Epigenetic Epidemiology of Common Complex Disease: Prospects for Prediction, Prevention, and Treatment
- Acute Human Lethal Toxicity of Agricultural Pesticides: A Prospective Cohort Study
- Information from Pharmaceutical Companies and the Quality, Quantity, and Cost of Physicians' Prescribing: A Systematic Review
- Increased Responsibility and Transparency in an Era of Increased Visibility
- Editors, Publishers, Impact Factors, and Reprint Income
- Reflections on Pandemic (H1N1) 2009 and the International Response
- Prenatal Treatment for Serious Neurological Sequelae of Congenital Toxoplasmosis: An Observational Prospective Cohort Study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Epigenetic Epidemiology of Common Complex Disease: Prospects for Prediction, Prevention, and Treatment
- Editors, Publishers, Impact Factors, and Reprint Income
- Oral Ondansetron Administration in Emergency Departments to Children with Gastroenteritis: An Economic Analysis
- Systematic Evaluation of Serotypes Causing Invasive Pneumococcal Disease among Children Under Five: The Pneumococcal Global Serotype Project
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



