-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Midline catheters for geriatric patients in Postacute Care Facility
Midline katétr u geriatrických nemocných v centru následné péče
Cíl: Geriatričtí pacienti přijatí do centra následné péče potřebují často dlouhodobé podávání infuzí a intravenózních léků. Zavedení spolehlivého žilního vstupu je proto důležitou součástí jejich sledování a léčby. Cílem studie bylo zhodnocení midline katétru u těchto nemocných.
Metodika: Hodnocení proveditelnosti, účinnosti a bezpečnosti zavedení 20 cm dlouhého midline katétru pacientům přijatým do centra následné péče v letech 2017–2019 sestrami cévního týmu FN Motol.
Výsledky: Dvě stě sedmdesát pacientů přijatých do centra bylo indikováno k zavedení midline katétru. U 15 pacientů (5,5 %) nebylo možné katétr zavést z důvodu absence vhodné žíly při ultrazvukovém vyšetření. Dvě stě devadesát midline katétrů bylo zavedeno 255 pacientům ve věku 81,5 ± 5,8 roku (rozmezí 66–94). Nebyla zaznamenána žádná komplikace při zavádění katétru. Medián doby zavedení midline katétru byl 32 dní (rozmezí 2–142). Komplikace průběhu využívání katétru byla zaznamenána u 58 z nich (5,8/1000 katétrových dnů). Dislokace katétru byla přítomna u 35, obstrukce u 9, lokální zánět u 7, infekce u 3 a trombóza v ipsilaterální žíle u 6 pacientů.
Závěr: Midline katétr představuje vhodný žilní vstup pro geriatrické nemocné přijaté do LDN.
Klíčová slova:
geriatrický pacient – žilní vstup – midline katétr – komplikace cévních vstupů – centrum následné péče
Authors: Martina Nováková 1; Kateřina Lisová 2; Kateřina Pavelková 2; Sabina Pálová 2; Jiří Charvát 2
Authors place of work: Postacute Care Facility of Faculty Hospital Prague Motol, Prague, Czech Republic 1; Department of Internal Medicine Second Faculty of Medicine, Charles University and Faculty Hospital Prague Motol, Prague, Czech Republic 2
Published in the journal: Geriatrie a Gerontologie 2022, 11, č. 2: 90-94
Category: Původní práce
Summary
Background: The geriatric patients admitted to Postacute Care Facility (PAF) often need the prolonged application of infusions and intravenous medicaments. The introduction of a reliable vascular device is therefore an important part of their management.
Methods: Evaluation of feasibility, effectiveness and safety of 20cm long midline catheter inserted to the patients in PAF during years 2017–2019 by nurses of vascular team.
Results: Two hundred and seventy patients admitted to PAF have been indicated for insertion of midline catheter. In 15 patients (5.5 %) midline catheter could not be inserted due to absence of a suitable vein during ultrasound examination. Two hundred and ninety midline catheters were inserted to 255 patients who were 81.5±5.8 years old (range 66 94). No complication during catheter insertion was recorded. Median of midline catheters dwelling time was 32 days (range 2–142). The complication was recorded in 58 midline catheters (5.8/1000 catheter days). The catheter dislodgment was present in 35, catheter obstruction in 9, local inflammation in 7, catheter infection in 3 and thrombosis in ipsilateral vein in 6 patients.
Conclusion: Midline catheter is a suitable vascular device for the elderly patients in PAF who need the prolonged peripheral vascular access.
Keywords:
venous access – Postacute Care Facility – midline catheter – complications of vascular device
Introduction
Some patients admitted to hospital suffering from a serious illness cannot be discharged home immediately after stabilization. They need long-term care in the Postacute Care Facility (PAF), where their treatment continues under close supervision.(1–5) Such a situation is common in elderly people. The administration of infusions and intravenous drugs can take weeks or even months.(1,2) The insertion of a reliable vascular device is therefore very important.
The peripheral cannula is only suitable for a short time, which in a long-term patient leads to a frequent need to replace it, which can be painful and associated with complications.(6) Midline catheter inserted under ultrasound navigation can be useful in this situation because it may be dwelled in a vein for a long time.(7–9)
The aim of this study was to evaluate the feasibility, effectiveness and safety of midline catheters inserted in elderly patients in PAF by members of vascular team after instruction and training of nurses in PAF about midline catheter management.
The patients and methods
The patients admitted to PAF of Faculty hospital whom was midline catheter inserted since 2017 to 2019 were included into study. The study protocol was carried out in accordance with the ethical principles of the Helsinki Declaration and was approved by the Ethics Committee of Faculty Hospital Prague Motol, Czech Republic.
Inclusion criteria:
• The patient admitted to PAF who agreed with midline catheter insertion.
• Age ≥ 65 years.
• Peripheral venous access indicated for at least 7 days in nonDIVA patients – it means the infusion solution with pH between 5 and 9, osmolarity up to 800 mOsm/l and no vesicant or irritant drugs.
• Peripheral venous access in DIVA patients.
• A suitable vein detected by ultrasound examination.
• Exclusion criteria:
• The patient younger than 65 years.
• Peripheral vascular access indicated for shorter period than 7 days in non-DIVA patient.
• Need for central vascular access.
• Contraindication to midline catheter insertion – no suitable vein, anatomical and functional changes interfering with catheter insertion.
• Midline catheter already inserted before admission to PAF.
Study protocol
The patient was first informed about the procedure. Before catheter insertion the patient signed the informed consent. The optimal vein with a diameter of at least 4 mm in the middle part of the arm was selected by ultrasound examination. If a vein of at least 4 mm in size was found only in the upper third of the arm, subcutaneous tunneling of the catheter from the upper to the middle part of the arm was performed. All the midline catheters were inserted by nurses of vascular team.
Procedure of midline catheter insertion consisted of the following steps:
1. Hands washing of operator.
2. Sterile precautions – operator in sterile gown, sterile gloves, surgical mask and cap. Disinfection of the insertion site with 2% chlorhexidine solution with sufficient exposition time.
3. Large sterile cover of puncture site.
4. Ultrasound detection of the selected vein.
5. Insertion of 20 cm midline catheter (Medcomp, Harleysville, PA, USA) under ultrasound navigation by modified Seldinger method.
6. Ultrasound location of the distal tip of midline catheter in the right or left axilary or subclavian vein.
7. Catheter flushing and locking with sterile physiological solution.
8. Catheter fixation with Stat-Lock (Bard Access System, Salt lake City, UT, USA), the application of glue on the insertion site and transparent dressing.
9. The patient evaluation of the patiens discomfort (Numeric pain scale 1-10, 1 minimum, 10 maximum of discomfort).
10. Performance documentation with instructions for nursing staff in PAF.
After insertion, the patient was monitored by nurses in PAF who were instructed and trained in midline catheter management. Daily they inspected the site of insertion to assess stability and intact dressing of midline catheter, recorded any signs of local infection, the patient discomfort and respected the following instructions.
1. When using midline catheter, hand hygiene prior to touching catheter and the surrounded site. The hub of needle-free connector had to be cleaned with 2% chlorhexidine gluconate for 15 seconds at least. Catheter flushing was made by push-pause method. Prefilled 0.9% NaCl syringes were used for catheter flushing and locking.
2. The application of new sterile semipermeable transparent dressing that remains dry and intact every 7 days or earlier (in case of contamination or dressing dislodgement).
3. All the complications related to midline catheter were recorded.
The catheter was removed if there was no need for its use any more or if the complication could not be corrected. The catheter associated infection, thrombosis in ipsilateral vein, catheter occlusion, catheter dislodgment, local changes at puncture site were recorded and if possible corrected.
In case of infection catheter was removed and antibiotic treatment applied. When thrombotic complication appeared therapeutic dosage of low molecular heparin was started and continued until catheter removal and 3 months afterwards. In case of catheter occlusion low dosage of fibrinolytic agent was given into lumen of catheter (2 mg Actilyse, Boehringer Ingelheim, Germany). Dislodgment of catheter was indication for its extraction. Local changes were managed by dressing modification.
The midline catheter dwelling time and frequency of complications were evaluated.
Statistical evaluation
Descriptive statistics for characterising the study population and midline–associated complications were used. The significance of the selected parameters of patient characteristics and midline catheter insertion for the presence of complications was analysed by Cox proportional hazard model. Age, gender, the selected vein, size of vein, number of punctures during insertion and time of insertion procedure were evaluated as independent predictors of complications.
Results
Two hundred and seventy patients admitted to PAF have been indicated for insertion of midline catheter. In 15 patients (5.5 %) midline catheter could not be inserted due to absence of a suitable vein during ultrasound examination.
Two hundred and ninety midline catheters were inserted to 255 patients. The age of patients was 82±6 years (range 66–97), 140 women (55 %) and 115 men (45 %). Fifty-nine patients (23 %) passed away during admission in PAF.
Thirty-five patients had two midline catheters. In 10 cases (3.5 %), tunneling from the upper to the middle of the arm was necessary. The data about midline catheter insertion are summarized in Table 1. The score of discomfort associated with the insertion of midline catheter evaluated by the patients was 2.1 in average (range 1–4) according to numeric pain scale 1-10. Two hundred and ninety midline catheters were dwelled in vein of 255 patients in PAF for 9946 days. Median of midline catheters dwelling time was 32 days (range 2–142).
Tab. 1. Midline catheter insertion data 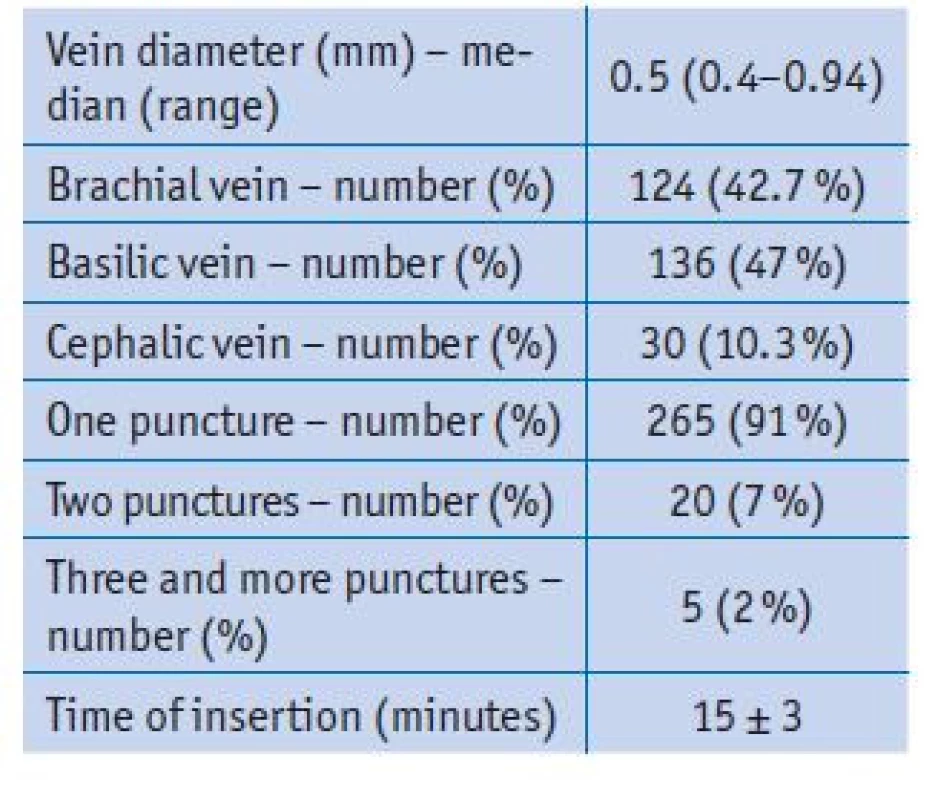
Some complication was detected in 58 midline catheters (20 %; 5.8/1000 catheter days). The catheter dislodgment was present in 35 (3.5/1000 catheter days), obstruction in 9 (0.9/1000 catheter days), local inflammation in 7 (0.7/1000 catheter days), catheter infection in 3 (0.3/1000 catheter days) and thrombosis in ipsilateral vein in 6 patients (0.6/1000 catheter days). The relation of midline complications to the selected parameters is summarized in Table 2.
Tab. 2. The relation of midline complications to the selected parameters 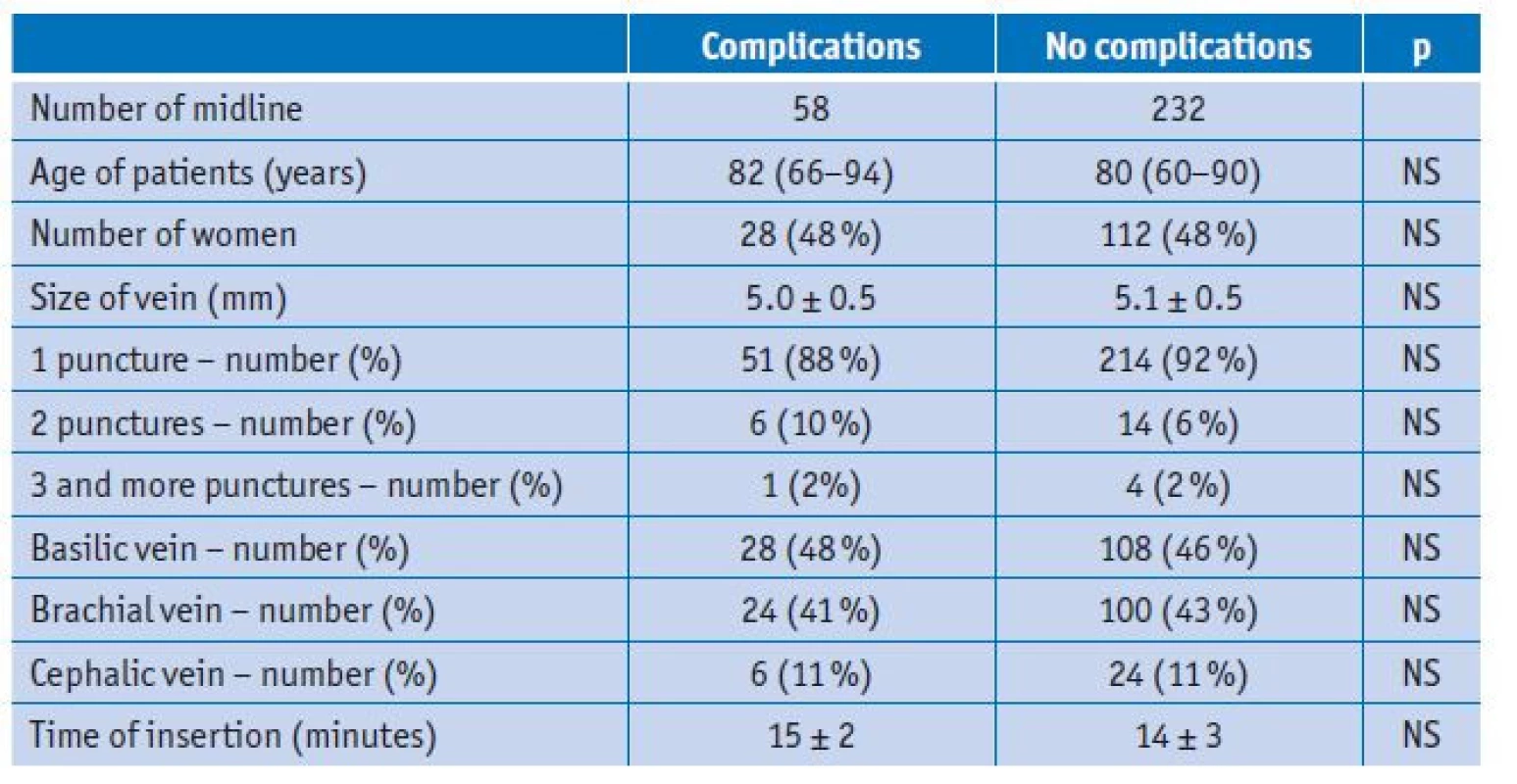
In 17 patients (7 %), midline was replaced by PICC or CICC due to worsening of the clinical condition and the need for central vein administration.
Discussion
Compared to a peripheral cannula and a centrally inserted central venous catheter without tunneling (CICC), PICCs and midline catheters can be inserted into a vein for a long period of time, weeks, or even months.(10,11) Previous studies have shown a low rate of complications associated with these vascular devices during acute disease.(11–13) However, little information is available about the midline catheter in health care facilities that care for elderly patients in the post-acute period.(1,2) In the elderly, degenerative changes in the venous system occur over the years, vascular access is more difficult, and complications associated with insertion of a vascular device are more common.(14) Repeated insertion of a peripheral cannula can be associated with painful sensations and a number of other complications.( 6) It therefore seems reasonable to insert a venous device that can be left for a long time.
A midline or long peripheral catheter is indicated in patients who need vascular access for more than 7 days and in DIVA patients.(12,13,15) During an acute situation, a long peripheral catheter 6 to 15 cm in length is preferred.(13,17) However if a peripheral vascular access is needed for more than 1 month, a midline about 20 cm is more stable and suitable.(2) On the other hand, an associated thrombosis may be more severe in comparison with a long peripheral catheter.(18)
In accordance with previous studies,( 7–9,14) the insertion of a midline catheter under ultrasound navigation was successful in our patients without procedural complications within a few minutes. In case of catheter tunneling, we did not encounter any complications as well and the insertion of midline was also well tolerated.
Complications during use occurred in a fifth of patients with an indwelling catheter. Most of them were not serious. These were most often random dislodgment for which catheter was removed and another one inserted. Other less serious complications included catheter obstruction, which were mostly resolved by applying low-dose thrombolytic therapy. With one exception, local inflammatory changes around the catheter exit site disappeared after changing the dressing material.
Catheter infection and venous thrombosis around the indwelling catheter must be considered as serious complications.
Catheter infection occurred only in three patients. After removal of the catheter and the use of antibiotic treatment, the condition improved in all three cases.
The prevalence of thrombotic complications in older subjects admitted to long-term care facilities is reported to be significantly higher in comparison to acute hospitalization.(19–21) However in our observation only 2 % of patients suffered from upper limb thrombotic complication associated with midline catheters. The explanation is not clear but the most patients in PAF received preventive anticoagulation if not contraindicated. The low rate of upper limb thrombosis associated with PICC insertion in skilled nursing facilities was reported also in another study.(1)
In our experience, the insertion of a midline catheter is sufficient for most patients in PAF who need a long-term venous access. In the period from 2017 to 2019, only 82 elderly patients in PAF were indicated for central catheter insertion. Many patients in PAF, especially the elderly, mainly need hydration, improvement in pain, some nutrition support and another symptomatic treatment, which can be provided by peripheral access. Insertion of a midline catheter is easier and cheaper compared to PICC.(15)
In conclusion the result of our study support the use of midline catheters in patients admitted to PAF when long-term vascular access is indicated. The midline insertion is feasible and well tolerated in the majority of elderly patients, can be used for a long period of time with low frequency of the serious complications.
MUDr. Martina Nováková
Promovala na 1. lékařské fakultě UK v roce 1992, atestovala z vnitřního lékařství v roce 1995 a v r. 2000, atestaci z geriatrie složila v roce 2011. Od roku 1992 do roku 2012 pracovala na Interní klinice FN Motol, kde se věnovala především angiologii a konziliární činnosti. Od dubna 2012 je primářkou Centra následné péče ve FN Motol. Podílí se na výuce geriatrie v rámci 2. LF UK, od roku 2020 studuje postgraduálně doktorský program Longevity studies na Fakultě humanitních studií UK. Je místopředsedkyní výboru České gerontologické a geriatrické společnosti se zaměřením na následnou a dlouhodobou péči.
Funding: This study is supported by Ministry of Health, Czech Republic-conceptual development of research organisation, University Motol, Prague, Czech Republic 00064203
Address for correspondence:
Jiří Charvát
Department of Internal Medicine of 2nd Faculty of Medicine
Charles University and Faculty Hospital
Prague Motol
V Úvalu 84, 150 06 Prague 5, Czech Republic
e-mail: jiri.charvat@fnmotol.cz
Zdroje
1. Chopra V, Montoya A, Joshi D, et al. Peripherally Inserted Central Catheter Use in Skilled Nursing Facilities: A Pilot Study. J Am Geriatr Soc 2015; 63(9): 1894–1899.
2. Magnani C, Calvieri A, Giannarelli D, et al. Peripherally inserted central catheter, midline and “short” midline in palliative care: Patient - reported outcome measures to assess impact on quality of care. JVA 2019; 20(5): 475 – 481.
3. Bortolussi R, Zotti P, Conte M, et al. Quality of Life, Pain Perception, and Distress Correlated to Ultrasound-Guided Peripherally Inserted Central Venous Catheters in Palliative Care Patients in a Home or Hospice Setting. JPSM 2015; 50(1): 118–123.
4. Harrod M, Montoya A, Mody L, et al. Challenges for Nurses Caring for Individuals with Peripherally Inserted Central Catheters in Skilled Nursing Facilities. J Am Geriatr Soc 2016; 64(10): 2059 – 2064.
5. Davidson GH, Austin E, Thornblade L, et al. Improving transitions of care across the spectrum of healthcare delivery: A multidisciplinary approach to understanding variability in outcomes across hospitals and skilled nursing facilities. Am J Surg 2017; 213(5): 910–914.
6. Moureau N, Chopra V. Indications for peripheral, midline and central catheters: summary of the MAGIC recommendations. Br J Nurs 2016; 25(8): S15–S24.
7. Constantino TG, Parikh AK, Satz WA and Fojtik JP. Ultrasonography - guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med 2005; 46(5): 456 – 461.
8. Brannam L, Blaivas M, Lyon M and Flake M. Emergency nurses utilization of ultrasound guidance for placement of peripheral intravenous lines in difficult-access patients. Acad Emerg Med 2004; 11(12): 1361–1363.
9. Resnick JR, Cydulka RK, Donato J, et al. Success of ultrasound - -guided peripheral intravenous access with skin marking. Acad Emerg Med 2008; 15(8): 723 – 730.
10. Adams DZ, Little A, Vinsant C, Khandelwal S. The midline catheter: a clinical review. J Emerg Med 2016; 51(3): 252–258.
11. Woller SC, Stevens SM and Evans RS. The Michigan Appropriateness Guide for intravenous catheters (MAGIC) initiative: a summary and review of peripherally inserted central catheter and venous catheter appropriate use. J Hosp Med 2016; 11(4): 301–310.
12. Cotogni P, Pittirutti M. Focus on peripherally inserted central catheters in critically ill patients. World J Crit Care Med 2014; 3(4): 80–94.
13. Gilardi E, Giannuzzi R, Wolde - Sellasie K, et al. Mini-midline in difficult intravenous access patients in emergency department: A prospective analysis. JVA 2020; 21(4): 449–455.
14. Leonardsen AL, Lunde EM, Smith ST, Olsen GL. Patient experiences with peripherally inserted venous catheters. A cross-sectional, multicentre study in Norway. Nurs Open 2020; 7(3): 760–767.
15. Mushtaq A, Navalkele B, Kaur M, et al. Comparison of complications in midlines versus central venous catheters: Are midlines safer than central venous lines? Am J Infect Control 2018; 46(7): 788 – 792.
16. Xu X, Wang B, Ren CH, et al. Age - -related impairment of vascular structure and functions. Aging Dis 2017; 8(5): 590–610.
17. Qin KR, Nataraja RM, Pacilli M. Long peripheral catheters: Is it time to address the confusion? JVA 2019; 20(5): 457–460.
18. Lisova K, Hromadkova J, Pavelkova K, et al. The incidence of symptomatic upper limb venous thrombosis associated with midline catheter: Prospective observation. JVA 2018; 19(5): 492 – 495.
19. Bosson J, Labarere J, Sevestre M, et al. Deep vein thrombosis in elderly patients hospitalized in subacute care facilities. A multicenter cross-sectional study of risk factors, prophylaxis, and prevalence. Arch Intern Med 2003; 163 : 2613–1618.
20. Sellier E, Labarere J, Sevestre M, et al. Risk factors for deep vein thrombosis in older patients. A multicenter study with systematic compression ultrasonography in postacute care facilities in France. J Am Geriatr Soc 2008; 56 : 224–230.
21. Chopra V, Ratz D, Kuhn I. Peripherally inserted central catheter-related deep vein thrombosis: Contemporary pattern and predictors. J Throm Haemost 2014; 12 : 847–854.
Štítky
Geriatrie a gerontologie Praktické lékařství pro dospělé Protetika
Článek vyšel v časopiseGeriatrie a Gerontologie
Nejčtenější tento týden
2022 Číslo 2- Alergie na antibiotika u žen s infekcemi močových cest − poznatky z průřezové studie z USA
- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Magnosolv a jeho využití v neurologii
- Trazodon pohledem praktického lékaře
-
Všechny články tohoto čísla
- Editorial
- Lékové interakce v gerontopsychiatrii – výběr antipsychotik a antidepresiv pro geriatrické pacienty
- Nemelanomové kožní nádory – bazaliom, spinaliom. Přehled o onemocnění a léčbě
- Inkontinence moče ve stáří
- Koagulopatie asociovaná s infekcí covid-19 a riziko tromboembolismu – známe jejich vzájemnou souvislost a následné řešení?
- Midline katétr u geriatrických nemocných v centru následné péče
- Neočekávaný průběh anti Xa aktivity po suicidálním požití rivaroxabanu u staršího nemocného
- Odešel internista a geriatr MUDr. Jan Zeman…
- Geriatrie a Gerontologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Nemelanomové kožní nádory – bazaliom, spinaliom. Přehled o onemocnění a léčbě
- Midline katétr u geriatrických nemocných v centru následné péče
- Lékové interakce v gerontopsychiatrii – výběr antipsychotik a antidepresiv pro geriatrické pacienty
- Inkontinence moče ve stáří
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




