-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Případ pozdní brachiální plexopatie po chemoterapii a radioterapii
Autoři: M. G. Şenol; T. Kendirli; M. Saraçoğlu
Působiště autorů: Sciences University, Istanbul, Turkey ; Department of Neurology, Health
Vyšlo v časopise: Cesk Slov Neurol N 2020; 83(2): 205-206
Kategorie: Dopis redakci
doi: https://doi.org/10.14735/amcsnn2020205Souhrn
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Dear Editor,
Radiation-induced plexus neuropathy refers to a rare late complication of radiotherapy administered to the supraclavicular area and upper part of the thoracic wall. Radiation-induced brachial plexopathy (RIBP) has been reported as a result of radiation therapy in the treatment of lung, breast, nasopharynx and thyroid cancer, sarcoma, diffuse large B-cell lymphoma, schwannoma and malignant peripheral nerve sheath tumour (primary plexus tumours) involving the neck, shoulder and upper thorax [1]. The latent period between radiation exposure and clinical manifestations of plexopathy may vary by as much as 1–34 years [2]. Differential diagnosis may prove to be challenging because the symptoms resemble those of the neoplastic involvement of the brachial plexus. Electrophysiological studies are valuable diagnostic tools for the assessment of patients with suspected brachial plexopathy [3].
A 63-year-old female presented with paresthaesias and weakness in her left arm distally to the elbow. She reported experiencing shoulder pain 3 years previously, with motor and sensory deficits in the left arm during the same period. She had undergone physical therapy, resulting in partial improvement of pain, while the motor and sensory deficits persisted. She had undergone left mastectomy approximately 20 years previously, followed by chemotherapy with regional radiotherapy. She was also treated with 50 Gy of radiation in 24 fractions to the internal mammary region and axillary and supraclavicular nodes. Other coexisting conditions included type 2 diabetes mellitus, arterial hypertension and obesity.
During the neurological examination, the patient’s effort was graded on a Medical Research Council scale of 0–5: muscle power 3/5 for the abduction in the left shoulder; 3/5 for the left forearm flexion; 4/5 for the left forearm extension; 1/5 for the left wrist flexion; 1/5 for the left wrist extension; 0/5 for the left thumb abduction and 0/5 for the abduction of the second and the fifth digits of the left hand. Her motor examination revealed the presence of benediction and partial claw hand sign on the left hand, with minimal atrophy in semiflexion posture of the fourth and the fifth digits and abductor digiti minimi muscles (Fig. 1).
Obr. 1. A, B – Benediction sign is a wrist position which is mimicked by ulnar paralysis; C – prominent wrist extensor weakness.
Obr. 1. A, B – Příznak Benediktova syndromu je poloha zápěstí, která se podobá ulnární paralýze; C – nápadná slabost extenzorů zápěstí.
Electromyographic studies are shown in Tab. 1. EMG sensory nerve conduction tests failed to elicit left lateral antebrachial and bilateral medial antebrachial cutaneous nerve responses. Needle EMG examination revealed the presence of denervation potentials in the left abductor pollicis brevis and extensor digitorum communis muscles, while signs of neurogenic involvement were identified in the muscles innervated by C5-6-7-8 and T1. Myokymic discharges were observed from the deltoid, biceps and triceps muscles on needle EMG. Somatosensory evoked potential could not be obtained by stimulation of the left median nerve. These findings were believed to be suggestive of an involvement of the upper-medial trunks and particularly, the medial and posterior cords of the lower trunks of the brachial plexus. MRI of the brachial plexus could not be performed due to the excessive obesity of the patient. In the CT examination, the left axillary/supraclavicular study showed no evidence of tumour infiltration. In CSF examination, the protein level was 46 mg/dL slightly above the limit (20–45 mg/dL) and the cell number was 3 (0–5/mm3) and there was no increase.
Tab. 1. Values of motor nerve conduction study. 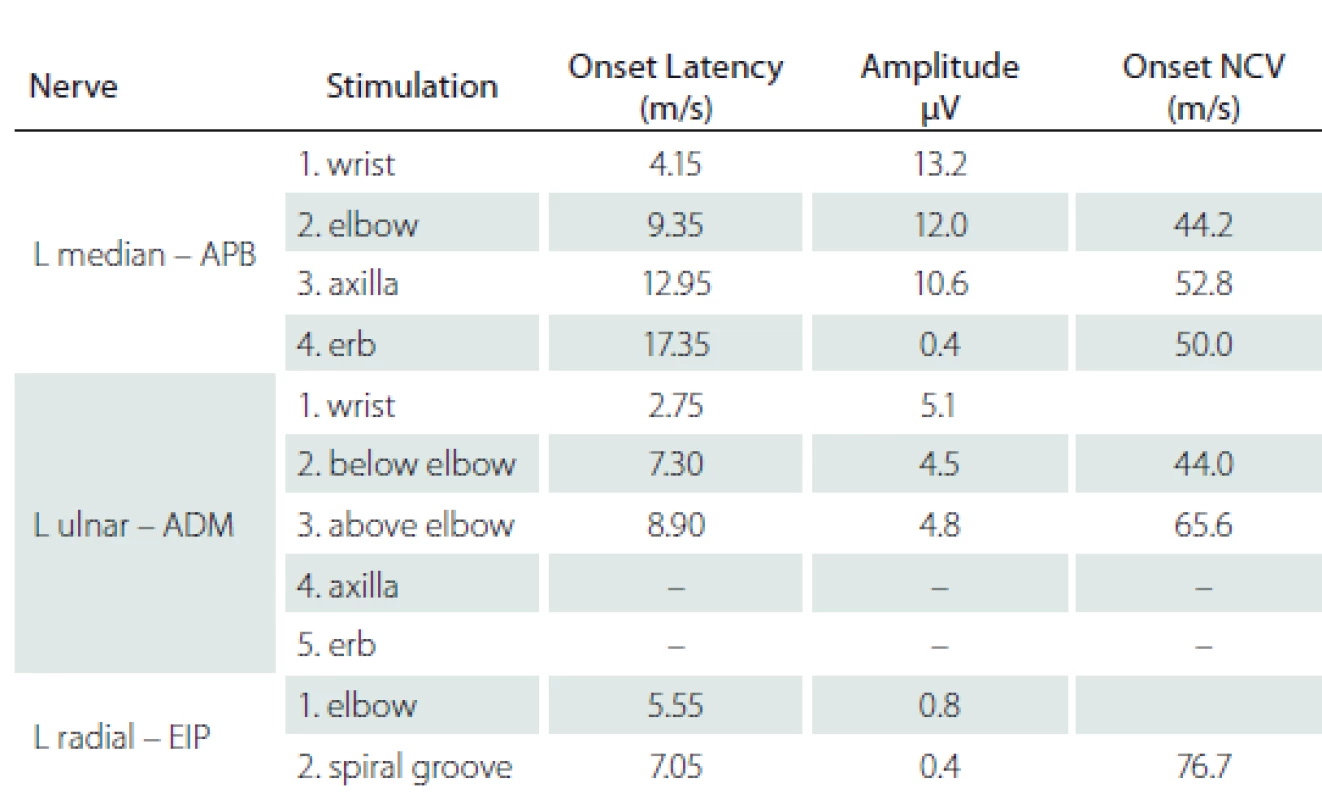
ADM – abductor digiti minimi; APB – abductor pollicis brevis; EIP – extensor indicis proprium; NCV – nerve conduction velocity Radiation-induced brachial plexopathy, which was more common in the past, is now a relatively rare complication of modern radiotherapy, the incidence of which is dependent on several factors including total dose, dose per fraction, patient age and concurrent administration of chemotherapy. Proposed pathophysiological mechanism includes nerve trapping due to radiation-induced fibrosis, chronic oedema, or both. Other implicated factors include a direct toxic effect on neurons and microvascular injury leading to ischaemic injury [4]. In electrodiagnostic studies, 90% of patients exhibited nerve conduction abnormalities and 63% exhibited myokymic discharges [5]. Previous observations suggest that these conditions are more likely to be associated with a prolonged latency period before manifestation and progressive injury; thus, patients who undergo radiotherapy for cancer should be under life-long monitoring for possible complications.
In around 50% of patients with neuralgic amyotrophy (Parsonage-Turner syndrome), a history of a viral disease or immunization and rarely, surgery, trauma, pregnancy, drug dependence or collagen tissue disorder is present [6]. Differential diagnosis includes idiopathic painful amyotrophy or brachial neuritis, which may occur with sudden onset of infection. The pain typically awakens the patient and cannot be localized. The asymmetrical shoulder girdle and arm muscular power loss is generally realized after improvement of the pain [7]. These complaints are followed by atrophy, and sensory symptoms may co-exist. Nerves that arise directly from the roots such as the long thoracic nerve are generally involved. Needle EMG may also show involvement of the brachial plexus. Spontaneous recovery may occur in 1–2 years [8]. Incomplete lesions of the brachial plexus are common and may include the upper part (Erb-Duchenne palsy) or the lower part (Klumpke’s palsy) [6]. In our patient, in particular the distal part of the upper extremity was significantly affected.
Claw hand and benediction posture are characteristic symptoms of hand nerve injury. These are known as the “benediction sign”, resulting from the hyperextension of the metacarpophalangeal joints of the little and ring finger digits and the flexion of the interphalangeal joints. The benediction sign is present in ulnar neuropathy and appears in partial flexion of the last two digits when the patient extends the fingers and hand. This sign is the result of the weakness of the lumbrical muscles in the hyperextension of the metacarpals of the fourth and the fifth fingers, although the unopposed extension of the extensor digitorum communis muscle. In long-term cases of ulnar nerve lesion, claw hand deformation appears [9].
Many cancer patients undergoing radiation to the head, neck and axilla are at risk of developing RIBP. Patients should be informed about this risk before radiation treatment. The progression of the disease is dependent on the nature of the disease, the phase or stage of the disease and the pathway of the disease. Clinical findings play an important role in the differential diagnosis of radiation plexopathy, with myokymic discharges exhibiting typical changes on EMG.
The Editorial Board declares that the manu script met the ICMJE “uniform requirements” for biomedical papers.
Mehmet Güney Şenol, MD
Department of Neurology
Health Sciences University
34668 Istanbul
Turkey
e-mail: mgsenol@yahoo.comAccepted for review: 5. 2. 2019
Accepted for print: 22. 1. 2020
Zdroje
1. Peppoloni G, Baglioni T, Dotti MT et al. Brachial plexopathy due to breast cancer metastases: electrophysiological and imaging findings. Neurol Sci 2018; 39 (8): 1503–1515. doi: 10.1016/s10072-018-3320-7.
2. Johansson S, Svensson H, Denekamp J. Timescale of evolution of late radiation injury after postoperative radiotherapy of breast cancer patients. Int J Radiat Oncol Biol Phys 2000; 48 (3): 745–750. doi: 10.1016/ s0360-3016 (00) 00674-x.
3. Boyaciyan A, Oge AE, Yazici J et al. Electrophysiological findings in patients who received radiation therapy over the brachial plexus: a magnetic stimulation study. Electroencephalogr Clin Neurophysiol 1996; 101 (6): 483–490.
4. Gałecki J, Hicer-Grzenkowicz J, Grudzień-Kowalska M et al. Radiation-induced brachial plexopathy and hypofractionated regimens in adjuvant irradiation of patients with breast cancer – a review. Acta Oncol 2006; 45 (3): 280–284. doi: 10.1080/02841860500371907.
5. Preston DC, Shapiro BE. Basic electromyography: analysis of spontaneous activity. In: Preston DC, Shapiro BE (eds). Electromyography and neuromuscular disorders. 2nd ed. Philadelphia: Elsevier 2005 : 199–213.
6. Harper CM Jr, Thomas JE, Cascino TL et al. Distinction between neoplastic and radiation-induced brachial plexopathy, with emphasis on the role of EMG. Neurology 1989; 39 (4): 502–506. doi: 10.1212/wnl.39.4.502.
7. Addar AM, Al-Sayed AA. Update and review on the basics of brachial plexus imaging. Med Imaging Radiol 2014; 2 : 1. doi: 10.7243/2054-1945-2-1.
8. Khadilkar SV, Khade SS. Brachial plexopathy. Ann Indian Acad Neurol 2013; 16 (1): 12–18. doi: 10.4103/0972-2327.107675.
9. Bertorini TE. CASE 7 – a man with a history of polio who developed hand weakness and numbness. In: Bertorini TE (ed). Neuromuscular case studies. Philadelphia: Butterworth-Heinemann 2008 : 123–128.
Štítky
Dětská neurologie Neurochirurgie Neurologie
Článek Poměr fosforylovaného tau proteinu k beta amyloidu v likvoru predikuje pozitivitu amyloidové PETČlánek Chirurgická léčba benigních neurogenních tumorů mediastina – analýza 7letého souboru pacientůČlánek Dopis redakciČlánek Komentář redakceČlánek Prof. Mraček oslavil 90 letČlánek Odešla MUDr. Olga Baudyšová
Článek vyšel v časopiseČeská a slovenská neurologie a neurochirurgie
Nejčtenější tento týden
2020 Číslo 2- Magnosolv a jeho využití v neurologii
- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Zolpidem může mít širší spektrum účinků, než jsme se doposud domnívali, a mnohdy i překvapivé
- Nejčastější nežádoucí účinky venlafaxinu během terapie odeznívají
-
Všechny články tohoto čísla
- Cévní morfologie, symptomy, diagnostika a léčba ischemických příhod mozkového kmene
- Je koncept vaskulární demence trvale udržitelný?
- Je koncept vaskulární demence trvale udržitelný? NE
- Je koncept vaskulární demence trvale udržitelný? Komenář
- Mezinárodní klasifikace bolestí hlavy (ICHD-3) – oficiální český překlad
- Schwannóm extrakraniálnej časti trojklanného nervu
- Chirurgická léčba mozkových metastáz
- Cavum septi pellucidi, cavum vergae a cavum veli interpositi
- Poměr fosforylovaného tau proteinu k beta amyloidu v likvoru predikuje pozitivitu amyloidové PET
- Provokační faktory a reakce na léčbu juvenilní myoklonické epilepsie – zkušenosti z tertiárního epileptického centra
- Chirurgická léčba benigních neurogenních tumorů mediastina – analýza 7letého souboru pacientů
- Transkraniální sonografie mediotemporálního laloku u pacientů s Alzheimerovou demencí
- Endarterektomie zevní karotické tepny
- Vestibulární funkce u pacientů s kochleárním implantátem
- Cystická hydatidóza mozečku – vzácná kazuistika
- Případ pozdní brachiální plexopatie po chemoterapii a radioterapii
- Spontánní vaginální extruze distálního katetru ventrikuloperitoneálního zkratu
- Opakovaná trombektómia u pacienta so zriedkavou kombináciou etiologických faktorov
- Dopis redakci
- Komentář redakce
- Prof. Mraček oslavil 90 let
- Odešla MUDr. Olga Baudyšová
- K jubileu profesorky Soni Nevšímalové
- Česká a slovenská neurologie a neurochirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Cavum septi pellucidi, cavum vergae a cavum veli interpositi
- Cévní morfologie, symptomy, diagnostika a léčba ischemických příhod mozkového kmene
- Mezinárodní klasifikace bolestí hlavy (ICHD-3) – oficiální český překlad
- Chirurgická léčba mozkových metastáz
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



