-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Subacute thyroiditis confused with dental problem
Subakutní tyreoiditida zaměněna za zubní problém
Subakutní tyreoiditida je zánětlivé onemocnění štítné žlázy často předcházené virovými infekcemi. Obvyklé příznaky bývají zvýšené teploty, napětí v žláze a okolí doprovázené bolestí. Iniciální hypertyreóza může byt doprovázená dočasnou periodou hypotyreózy s jinak příznivou prognózou. Je známo, že toto onemocnění je často zaměněno za faryngitidu, ale recentně provedená rešerše v Medline s klíčovým slovy: „subacute thyroiditis and dental pain“ s nulovým výsledkem poukazuje na menší obvyklost případu subakutní tyreoiditidy zaměněné za potíže zubního původu. V této kazuistice popisujeme případ subakutní tyreoiditidy zaměněné za potíže zubního původu. Cílem tohoto sdělení je upozornit na nutnost pomýšlet i na problémy spojené se štítnou žlázou u pacientů přicházejících s nevysvětlitelnými zubními bolestmi.
Klíčová slova:
subakutní tyreoiditida, zubní bolest, diferenciální diagnóza a léčba.
Authors: H. Tesfaye 1; R. Cimermanova 2; M. Cholt 3; P. Sýkorová 4; M. Pechová 1; R. Prusa 1
Authors place of work: Department of Clinical Biochemistry and Pathobiochemistry, Faculty Hospital Motol, nd Faculty of Medicine, Charles University, Prague, Czech Republic 1; Division of Primary Care, Faculty Hospital Motol, 2nd Faculty of Medicine, Charles University, Prague, Czech Republic 2; Department of Imaging Methods, Faculty Hospital Motol, 2nd Faculty of Medicine, Charles University, Prague, Czech Republic 3; Department of Nuclear Medicine and Endocrinology, Faculty Hospital Motol, 2nd Faculty of Medicine, Charles University, Prague, Czech Republic 4
Published in the journal: Čas. Lék. čes. 2009; 148: 438-441
Category: Kazuistika
Summary
Subacute thyroiditis is an inflammatory disease of the thyroid gland, most probably preceded by viral infection. Common symptoms include fever, thyroid tenderness associated pain, and initial hyperthyroidism sometimes followed by a transient period of hypothyroidism with generally favourable outcomes as self-limited entity. It was known that it may be confused with pharyngitis; however search on Medline using key words (dental pain, subacute thyroiditis, and differential diagnosis) in combination recently produced no reports. Herein, we report a case of subacute thyroiditis associated pain, which was initially mistaken and treated as pain of dental origin after otorhinolaryngologic examination revealed no pathology. The aim of this communication is to remind that thyroiditis as part of differential diagnosis should be considered in patients with unexplained dental pain to avoid unnecessary diagnostic procedures, which increase expenses and may delay appropriate therapeutic measures.
Key words:
subacute thyroiditis, dental pain, differential diagnosis and treatment.Introduction
Thyroiditis is generally an inflammation of the thyroid gland that may be painful and tender, when caused by infection, radiation, or trauma, or painless when caused by autoimmune conditions, medications, or an idiopathic fibrotic process. The most common forms are Hashimoto’s disease, subacute granulomatous thyroiditis, postpartum thyroiditis in women, subacute lymphocytic thyroiditis, and drug-induced thyroiditis (caused by amiodarone, lithium, interferon-alfa, and interleukin-2). Subacute granulomatous thyroiditis usually is attributed to a viral infection. The summer peak incidence of thyroiditis coincides with the peak incidences of coxsackievirus groups A and B and echovirus infections (1, 2). Symptoms and signs of subacute granulomatous thyroiditis usually include a prodrome of myalgias, pharyngitis, low-grade fever, and fatigue, followed by a tender, diffuse goitre and neck pain that often radiates up to the ear. Neck pain characteristically shifts from side to side and may settle in one area, frequently radiating to the jaw and ears. As the disease progresses there may be a “march” of tenderness across the gland, with new parts of the thyroid becoming painful and tender as previously involved portions become less painful. Symptoms of hyperthyroidism are common in early stage of the disease because of hormone release from the disrupted follicles. However, earlier report by Volpe and Johnston (3) stated that recognizing subacute thyroiditis based on presenting complaints is not an easy task. About two decades later, Carenfelt (4) published that subacute thyroiditis is often unrecognized and patients may be treated for pharyngitis, laryngitis, otitis media or similar disorders connected with otorhinolaryngology, illustrating difficulties encountered in making a correct diagnosis of course leading to useless therapy in consecutive patients initially misdiagnosed. Herein, we describe the manifestation, course, treatment, and outcomes of subacute thyroidits confused with dental pain.
Case Presentation
A 41years old male with unremarkable family and personal thyroid disease history visited his dentist in September 2008, with apparently mild left side dental pain at the beginning. Dental caries was excluded including by periapical (wall-mounted) x-ray examination of the painful side. Few days later the pain progressed so that it led to another visit to hospital dentist with chief complaints of dental and mild anterior left lateral neck pain. The panoramic x-ray examination proved no dental pathology (Fig. 1).
Fig. 1. Panoramic x-ray demonstrating normal findings in a patient complaining of unbearable dental pain. 
However, interdental drainage was performed for three consenscutive days under local mesocaine use. Whatever the intervention was, the patient continued complaining. Finally, the patient was referred to otorhinolarnygology department, where the ear, nose, throat (ENT) examination findings were reportedly normal. Fortunately, ultrasound examination of the neck was requested and the result showed engagement of left lobe, hyperaemic, hypoechogenic, and non-homogenic structure within the thyroid gland (Fig. 2). With this result the patient was referred to the department of endocrinology and nuclear medicine, where thyroid gland was found to be swollen and tender on physical examination.
Fig. 2. Ultrasound examination with colour Doppler demonstrating left lobe (L) hyperaemic and hypoechogenic non-homogenous structure with enlargement compared to mild right side 
Initially, the patient was non-febrile, free triiodothyronine (FT3) and free tetraiodothyronine (FT4) were within the reference range, while anti-thyroglobulin antibody (TgAb) level was very slightly elevated only to 82 kU/L (upper reference range up to 60 units). Levothyroxine 50 μg per tablet /day was prescribed assuming that usually hypothyroidism may follow. However, sleeping disturbance and extreme sweating led to levothyroxine withdrawal by the patient himself. The patient requested recheck earlier than previously planed as the pain in the anterior neck became intensive and fever of 37.3 to 38 °C was recorded despite regular use of non-steroid anti-inflammatory drug (NSAID) namely, Ibuprofen (Ibalgin tablet) initially 400 mg every 12 hours and later every 8 hours. Then, the neck pain shifted from the left side to the right side and was more severe in intensity than the previous, more radiating to the jaws, occipital regions and ears. Ultrasound control (re-examination) also revealed significant pathological changes (diffusely hyperaemic, hypoechogenic, and non-homogenic structure) in the right lobe compared with previous image. Among other laboratory findings, C-reactive protein (CRP) was elevated up 36–39 mg/L, whereas free T3 and T4 levels were significantly high indicating that the patient had hyperthyroidism phase of the inflammatory event. Further more, an increase in FT4 and FT3 was followed by a marked decrease in TSH level (0.008 mIU/L). Auto antibody against thyroglobulin (TgAb), which was only slightly elevated at the beginning, reached extremely high value > 500 kU/L (above the quantification limit of the determination method) persistently for several weeks. Anti-thyroid peroxidase antibody (TPOAb) was negative. Blood cells count and differential was unremarkable. The radioactive iodine uptake (RAIU) test was not performed in our case since all symptoms verified the entity as subacute thyroiditis. Erythrocytes sedimentation rate (ESR) also was not done, but based on CRP (39 mg/L), fever, and deteriorating symptoms, a wide spectrum antibacterial drug, namely deoxymycoin was recommended in addition to NSAID. Five days later the patient reported unbearable pain and difficulties in swallowing due to progressive tenderness and swollening of the gland more in the right side. Prednisone 30 mg/day was advised to start. Remarkable improvement of pain release was reported within two days of therapy with corticoid. Then the dose was gradually tapered up to 10 mg per day to stop completely after six weeks. Control FT3, FT4, and TSH showed typical expectations after the recovery (Table 1, Fig. 3). Meanwhile, the patient is without drug therapy and no further complaints were recorded on follow-up or no sign of reoccurrence is observed to date.
Tab. 1. Illustration of initial euthyroid phase followed by hyperthyroid phase and gradual increase of thyroid stimulating hormone (TSH) as a result of relative decrease of free triiodothronine (FT3) and free tetraiodothyrinine (FT4) levels at recovery, whereas antibody against thyroglobulin (TgAb) level is persistently high in a patient with subacute thyroiditis on follow-up 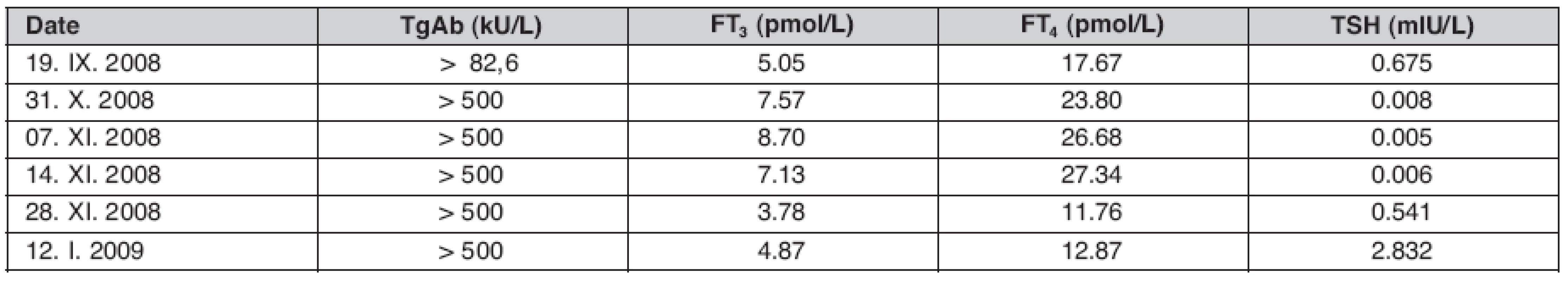
Fig. 3. Typical free T<sub>4</sub>, T<sub>3</sub>, and TSH profiles during the course of subacute thyroidistis, while the arrow indicates the date corticosteroid therapy started in the demonstrated case 
Discussion
Thyroid disease affects relatively high number of people in different age groups as recently well described in the review work of Limanova (5) indicating even a rising tendency in relation to diseases like diabetes mellitus. The same author (6) emphasised the necessity of interdisciplinary approach for diagnosis and management of the thyroid pathology in patients suffering from other diseases. Differentiating the various forms of thyroiditis can be difficult as they often mimic other disease processes. Diagnosis requires an awareness of the distinguishing characteristics of each type of thyroiditis as well as the overlapping features (7). Subacute thyroiditis (also known as giant cell thyroiditis or granulomatous thyroiditis) is the most common cause of thyroid pain. It affects four times more women than men, and most often occurs at the age of 40 to 50 years (8). History of an antecedent viral upper respiratory infection (URI) is common before clinical manifestation as thyroid disease, so that diagnosis is primarily clinical, based on finding an enlarged and tender thyroid in patients with the appropriate clinical history. But the history of URT infection immediately before the manifestation of the disease symptoms was absent in our patient. Thyroid function testing with TSH and free T3 and T4 is usually done, whereas radioactive iodine may be measured to confirm the diagnosis. When the diagnosis is uncertain, fine needle aspiration biopsy is useful, though invasive. Histological studies demonstrate less lymphocyte infiltration of the thyroid than in Hashimoto’s thyroiditis or silent thyroiditis, but there is characteristic giant cell infiltration and follicular disruptions. Thyroid ultrasound with colour Doppler usually shows reduced blood flow in contrast to our case (Fig. 2). Laboratory findings early in the disease include an increase in free T4 and T3, and a marked decrease in TSH, which is similar with what is observed in the present case. Treatments with high doses of NSAIDs or with corticosteroids in protracted cases are usual options. However, antibiotic coverage was our choice provided the patient’s symptoms in addition to laboratory findings, since literally existing atypical laboratory manifestation (9) corresponding to acute suppurative thyroiditis could not be excluded. Ultrasound is widely available, relatively rapid and safe method to visualize the whole anterior neck and it can aid in clinical decision making as already published (10). Differentiating the various forms of thyroiditis can also be challenging in some cases provided that features may be overlapping. For instance, Cho et al. (11) reported a case of patient, who was diagnosed with subacute thyroiditis based on clinical manifestation and laboratory results, treated with glucocorticoides for six weeks, and then followed-up for 12 months, where the final diagnosis ended up with rare Riedel’s thyroiditis, the disease, which may also develop in the course of subacute thyroiditis. The fact that hyperthyroidism is seen in one half of affected individuals is explained by that activated cytotoxic T lymphocytes damage the thyroid follicular cells, resulting in the unregulated release of large amounts of thyroxine (T4) and tri-iodthyronine (T3) into the circulation. This process usually is transient, lasting three to six weeks and ceasing when the thyroid stores are exhausted. A triphasic sequence is commonly observed that patients have a transitional phase of hyperthyroidism characterised by elevated free T4 and suppressed thyroid-stimulating hormone (TSH) levels, after which hypothyroidism with low free T4 and high TSH levels follows. Then, euthyroid state of recovery may occur under favourable conditions, which was exactly demonstrated in our patient. The disease is usually reported to resolve spontaneously within months, which is also observed in the present case, except persisting high level of TgAb. Nevertheless, measurement of free T4, T3, and TSH at 4 or 3 weekly follow-up intervals accordingly may be appropriate to monitor the disease status in general and to identify patients progressing in to hypothyroidism in particular. In the present case the patient is euthyroid so far and the follow-up may continue in long time intervals to determinate, whether permanent hormone maintenance therapy is needed or not.
Conclusions
Our case observation demonstrates that patients with unexplained dental pain and otherwise normal ORL findings deserve examination targeting thyroid gland to rule out thyroiditis or other conditions. Careful differential diagnosis workup can avoid unnecessary measures and non-benefiting treatment, which only leads to undesired outcomes and loss of scarce health care resources.
Address for correspondence:
Hundie Tesfaye, MD, PhD.
Faculty Hospital Motol, 2nd Faculty of Medicine, Charles University, Prague
V Úvalu 84, 155 06 Prague 5, Czech Republic
e-mail: hundie.tesfaye@fnmotol.cz
Zdroje
1. Martino E, et al. High prevalence of subacute thyroiditis during summer season in Italy. J Endocrinol Invest 1987; 10 : 321–323.
2. Bindra A, Braunstein GD. Thyroiditis. Am Fam Physician. 2006; 73 : 1769–1776.
3. Volpe R, Johnston MW. Subacute thyroiditis: a disease commonly mistaken for pharyngitis. Can Med Assoc J 1957; 77 : 297–307.
4. Carenfelt C. Subacute thyroiditis. A diagnosis in otolaryngology. ORL J Otorhinolaryngol Relat Spec 1975; 37 : 118–127.
5. Limanova Z. The thyroid gland – running the show behind the scenes, 1st Part. Čas Lék čes 2009; 148 : 83–85 (article in Czech).
6. Limanova Z. The thyroid gland – running the show behind the scenes, 2nd Part. Čas Lék čes 2009; 148 : 124–128 ([article in Czech).
7. Schubert MF, Kountz DS. Thyroiditis. A disease with many faces. Postgrad Med 1995; 98 : 101–103, 107–108, 112.
8. Fatourechi V, et al. Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmstead County, Minnesota, study. J Clin Endocrinol Metab 2003; 88 : 2100–2105.
9. Szabo SM, Allen DB. Thyroiditis. Differentiation of acute suppurative and subacute. Case report and review of the literature. Clin Pediatr (Phila) 1989; 28 : 171–174.
10. Hegedüs L. Thyroid ultrasound Endocrinol Metab Clin North Am. 2001; 30 : 339–360
11. Cho MH, et al. Riedel‘s thyroiditis in a patient with recurrent subacute thyroiditis: a case report and review of the literature. Endocr J 2007; 54 : 559–562.
Štítky
Adiktologie Alergologie a imunologie Angiologie Audiologie a foniatrie Biochemie Dermatologie Dětská gastroenterologie Dětská chirurgie Dětská kardiologie Dětská neurologie Dětská otorinolaryngologie Dětská psychiatrie Dětská revmatologie Diabetologie Farmacie Chirurgie cévní Algeziologie Dentální hygienistka
Článek vyšel v časopiseČasopis lékařů českých
Nejčtenější tento týden
- Psilocybin je v Česku od 1. ledna 2026 schválený. Co to znamená v praxi?
- Horní limit denní dávky vitaminu D: Jaké množství je ještě bezpečné?
- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejčastější nežádoucí účinky venlafaxinu během terapie odeznívají
-
Všechny články tohoto čísla
- On the debate about ethicotherapy
- Receiver Operating Characteristic analysis and the Cost – Benefit analysis in determination of the optimal cut-off point
- Pocty pro členy české lékařské společnosti Jana Evangelisty Purkyně
- Analysis of symptoms and case history data in the set of 353 patients with lung cancer in 1st Pulmonary department of Charles University, Prague
- Reduction of stuttering through bronchodilatation with β2 sympathomimetic drug formoterol
- Fractional exhaled nitric oxide and its correlation with bioptic results in chronic cough patients
- Serious cutaneous toxicity following ifosfamide, gemcitabine and vinorelbine therapy in a patient with relapsed Hodgkin lymphoma and ichthyosis
- Význam infekce pro tight junction
- Vztah mezi bariérou a antimikrobiálními peptidy
- Subacute thyroiditis confused with dental problem
- Spolek lékařů českých v Praze
- Protect children from computers and computers from children
- JAK SE HLÁSIT NA VZDĚLÁVACÍ AKCE IPVZ
- První desetiletí PET v důkazech Nemocnice Na Homolce, Praha, 4. září 2009
- 2. trilaterální sympozium s mezinárodní účastí Rožnov pod Radhoštěm, 17.–19. června 2009
- Olomoucké hematologické dny s mezinárodní účastí
- Seminář o metodologii výzkumu nikotinu a tabáku
- Zoonózy – nákazy s přírodní ohniskovostí
- 8. celostátní konference dětské pneumologie v Praze
- Blahopřání Mistru Josefu Sukovi k narozeninám
- LAUREÁTI NOBELOVY CENY
- Časopis lékařů českých
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Receiver Operating Characteristic analysis and the Cost – Benefit analysis in determination of the optimal cut-off point
- Subacute thyroiditis confused with dental problem
- Fractional exhaled nitric oxide and its correlation with bioptic results in chronic cough patients
- Zoonózy – nákazy s přírodní ohniskovostí
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



