-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
SATISFACTION AND COMPLICATIONS IN POST-BARIATRIC SURGERY ABDOMINOPLASTY PATIENTS
Autoři: M. Larsen 3; F. Polat 1; F. P. Stook 2; R. J. Oostenbroek 1; P. W. Plaisier 1; Hesp W. L.e.m. 1
Působiště autorů: Department of Plastic Surgery, Free University Medical Centre3, Amsterdam, The Netherlands ; Departments of Surgeray1 and Plastic Surgery2, Albert Schweitzer Hospital, Dordrecht, and
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 49, 4, 2007, pp. 95-98
INTRODUCTION
Bariatric surgery procedures have increased markedly, from 13,000 in 1998 to a projected 100,000 in 2003 in the USA (8). With an increase in bariatric surgery, more patients are presenting to complete their treatment course by seeking removal of the surplus skin and soft tissue left after massive weight loss. Body contouring is an important aspect to the overall treatment of the morbidly obese patient (9). Quality of life improves after bariatric surgery and is significantly enhanced after further body contouring, with improved body image (4, 10). Bariatric surgery, as opposed to dietary or lifestyle changes or pharmacologic interventions, offers sustained long-term weight reduction. After massive weight loss, the pannus can interfere with clothing, physical activity and hygiene, as well as be a cause for recurrent infection. There are, therefore, clear advantages to excision of remaining excess tissue. In this study, we retrospectively evaluated functional and aesthetic outcomes after abdominoplasty following laparoscopic adjustible gastric banding (LAGB) and correlated these to known preoperative risk factors. Specifically we aimed to find whether this patient population was more susceptible to postoperative complications than the general population seeking abdominal body contouring. Also, our concern that this procedure has no long-term benefit in terms of BMI reduction is investigated.
MATERIALS AND METHODS
A retrospective study was conducted by chart review and a questionnaire (in Dutch) sent to the 39 patients who had undergone LAGB and abdominoplasty (LAGB only, N=631) at our hospital between 1995 and 2004. The LAGB and abdominoplasty procedures were performed by the same surgeons, respectively. Patients who returned completed questionnaires were included in the study. The questionnaire included the following items: length, weight at present, weight before and after LAGB and abdominoplasty, secondary corrective procedures, risk factors and comorbidities (smoking, diabetes, arthrosis, alcohol consumption, sleep apnea, pyrosis, depression, asthma, cardiovascular history, varicosis, panniculitis, hypertension, hypercholesterolemia, age at onset of obesity), immediate and late postoperative complaints, complications (infection, wound breakdown, deep venous thrombosis, seroma, blood transfusion), satisfaction (change in hygiene, mobility, general activity level), weight change after abdominoplasty (change in operated or non-operated area and change in clothing size), and changes in lifestyle (general activity level, diet, productivity, health level compared to that before LAGB and before abdominoplasty). Finally patients were asked to qualify their current appearance and their results in general, and to indicate which procedures they would undergo again or advise to friends and family. All open-ended questions were accompanied by a choice of answers (for example, none, mild, moderate or severe discomfort postoperatively).
Abdominoplasty was performed only when stable weight loss after LAGB had occurred. In practical terms, this meant a BMI as close to the ideal body weight as possible, sustained over a period of three months. Patients were instructed to cease smoking three months preoperatively. The abdominoplasty technique was standard: removal of excess skin and subcutaneous tissue in an ellipse from both iliac crests over the suprapuberal margin with undermining to the costal margin and excision above the umbilicus. The latter was left intact and sutured to the superior skin flap. Wounds were closed in three layers and silicone drains left in the wound bed for 2–3 days. Complications such as seromas, infections (requiring antibiotics), blood transfusions, wound breakdown or re-exploration as well as the number of body contouring procedures, weight gain or loss after abdominoplasty and general satisfaction were noted from chart review. Statistical analysis was performed using JMP statistical software (SAS Institute Inc., Cary, NC).
RESULTS
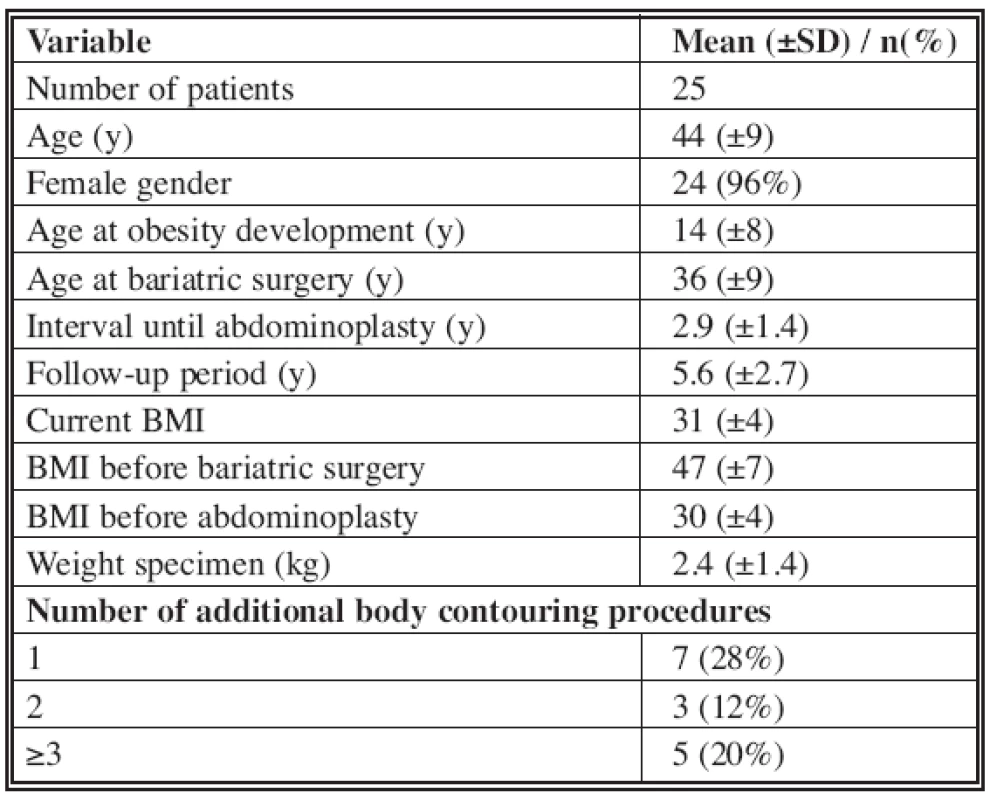
The response rate to the questionnaire was 64%, thus 25 patients could be included, with a mean age of 44 years and a median follow-up period after abdominoplasty of 5.6 years. All patient demographics are noted in Tab. 1. Noteworthy is that all patients were morbidly obese before LAGB (mean BMI: 47), but still obese both before and after abdominoplasty (BMI 30 and 31, respectively, range 24.9–39.3), despite 60% having undergone additional body contouring procedures. Eleven patients (44%) experienced a form of complication (Tab. 2). The only major complications were a wound breakdown in two patients. The most frequent complication was seroma formation, occurring in 25% of patients. Those who experienced a complication had a slightly higher BMI (31.1) before abdominoplasty than patients who did not (30.1), although this was not significant (ANOVA, p=0.53). Preoperative risk factors encountered were smoking (28%), diabetes (4%), depression (40%), varicose veins (24%), recurrent panniculitis (56%) and hypertension (20%). The likelihood ratio ÷2 test found no statistical relationship between any of these factors and the incidence of complications. Two thirds of patients experienced some form of discomfort postoperatively (mild, 24%; moderate, 36%; severe, 8%). In 44% the discomfort lasted for more than one week. Most patients noted an improvement in personal hygiene (68%), mobility (72%) and general functional capabilities (80%). Most also regained weight after abdominoplasty (64%), ranging from <2.5 kg (8%), 2.5–5 kg (8%), 5–7 kg (8%), to >7 kg (29%). The same weight was reported by 28%, and 44% lost weight after abdominoplasty: <2.5 kg (12%), 2.5–5 kg (8%), 5–7 kg (4%), and >7 kg (20%). These groups are not mutually exclusive, indicating fluctuations in post-contouring BMI. Weight gain was reported in the secondarily treated areas by 44% of patients, mostly in the abdomen. New areas of weight gain were seen by 24%. Most of the secondary weight changes occurred after the first 6 months post-abdominoplasty (56%). Clothing size changed in 84% post-abdominoplasty, in all cases a reduction, by an average of 2.4 European sizes. In terms of physical activity, the same level was kept by 52% and a higher level by 32%. Most patients (80%) did not alter their diet compared to pre-abdominoplasty, while 12% reported an improvement in their diet. Productivity at work was improved in 40% and reduced in 12%. Post-abdominoplasty general health was better (44%), stayed the same (44%), or was diminished (12%). The respective figures for post-LAGB are 96%, 0% and 4%. Physical appearance was graded excellent (12%), very good (12%), good (36%), moderate (28%) or bad (12%), while satisfaction with the general result was classified as very satisfied (40%), satisfied (44%), not satisfied (12%) and very unsatisfied (4%). Despite these outcomes, almost all patients would undergo the procedures again (LAGB, 92%; abdominoplasty, 96%), and would recommend them to family members (LAGB, 92%; abdominoplasty, 92%).
Tab. 2. Complications 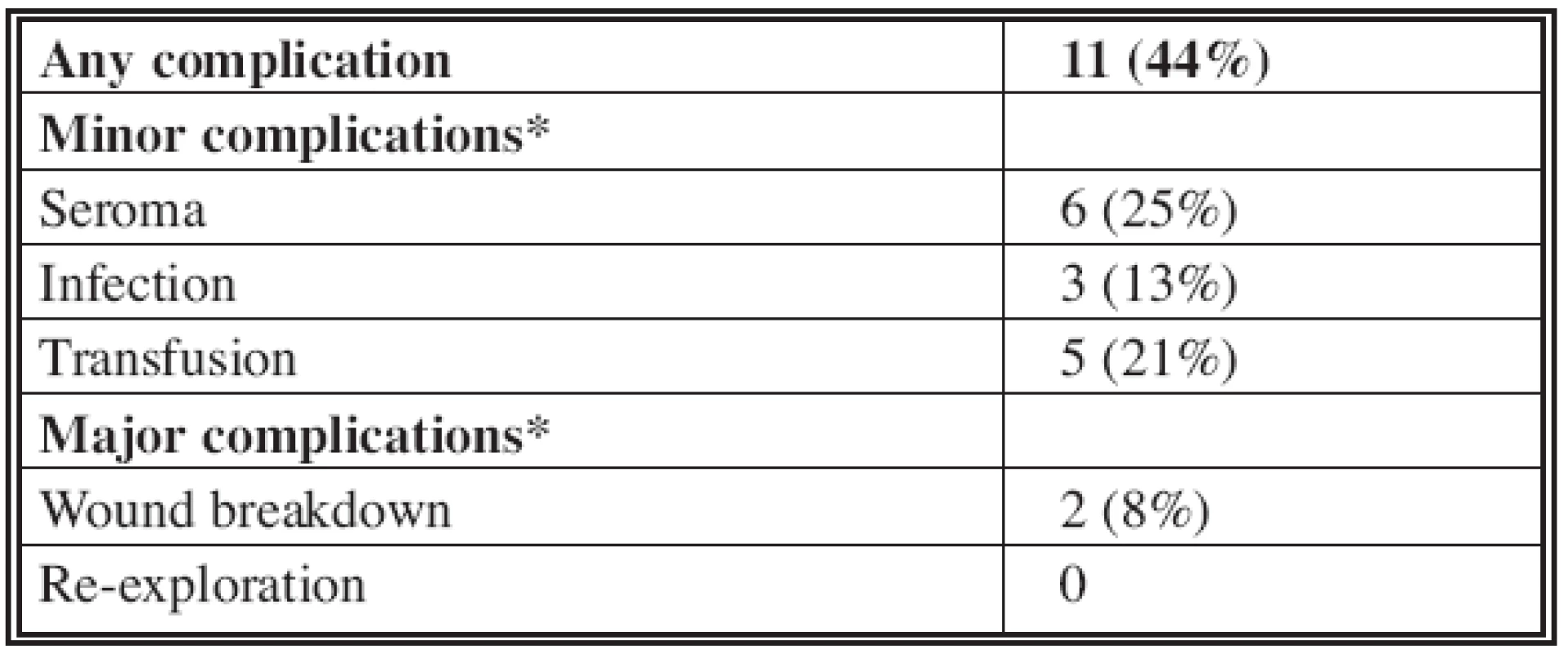
* Complications are not mutually exclusive. DISCUSSION
LAGB procedures lead to a significant improvement in quality of life, weight reduction and marked decrease in comorbid conditions (2). The LAGB procedure is the safest bariatric operation, with a 0.05% mortality rate, and carries less risk of protein, vitamin, mineral or other nutrient deficiency (6). Potentially, this will have an effect on wound healing after body contouring procedures, although we do not have data from other bariatric procedures or from the literature to verify this. In one study, no additional risk of postoperative wound infection was found in patients undergoing different types of bariatric surgery compared to obese patients undergoing general elective surgery procedures of similar invasiveness (12). By contrast, wound complication rates in obese patients undergoing abdominoplasty are more than doubled when compared to non-obese patients, irrespective of any previous bariatric surgery (13). General surgical procedures on obese patients also result in more complications (5). A complication such as wound infection or dehiscence does not amount to surgical failure, and abdominoplasty is a procedure with a high success rate that provides adequate improvement to quality of life. However, the post-bariatric surgery population is at increased risk for postoperative complications, so that maximal reduction in BMI should be stressed to these patients before undergoing abdominoplasty (1).
Post-LAGB body contouring patients are challenging and require intensive follow-up (11). Bariatric surgery and the subsequent weight loss require an additional 2–3 years commitment towards body contouring procedures. There are proven psychological benefits to post-weight loss body contouring. In a recent study, the body image characteristics of post-bariatric surgery patients and those seeking additional body contouring were compared (4). The post-bariatric group showed a marked improvement in attitude towards body weight and shape, and a normalization of the body image. However, the post-bariatric group seeking additional surgery showed still compromised weight and shape attitudes similar in scale to those of pre-bariatric patients. In these patients, after cosmetic surgery, body image awareness and self-efficacy were improved, without necessarily improving body satisfaction. We also found this difference in improved self-efficacy versus largely unaffected body satisfaction in our post-body contouring patients. Neither we nor other authors have been able to explain this discrepancy. Interestingly, another study found that a normalization of body image-related concerns occur in the face of most patients remaining overweight or obese, suggesting that mediating factors may be involved (3). This correlates well with our study population, as we found the current mean BMI to be greater than that before abdominoplasty. No further psychological evaluation was performed, however, and it would be interesting to find whether despite improved body image, more dissatisfaction occurs with other parts of the body in our population, as other authors have found recently (10).
The post-bariatric surgery population is at higher risk than the general population seeking abdominoplasty, with morbidity ranging from 20% to 50% (1, 7, 11, 13). We also found a complication rate (44%) within this range. The only significant predictor for postoperative complications reported in the literature is the pre-abdominoplasty BMI, with more than three times the risk for patients with a BMI greater than 25 kg/m2 (1). We found a similar trend in our population, although this was not significant.
A limitation to our study is that it is retrospective and certain data such as intra - and postoperative complications can be difficult to identify by medical record review. The complication rate may therefore be underestimated. Another clear drawback is that patient responses are subject to bias. Where LAGB is a safe procedure with marked improvement in comorbidity and body image, the results and complications from abdominoplasty after bariatric surgery may be improved by an emphasis on optimal weight reduction preoperatively. Patients should be told to expect a difference in body satisfaction post-abdominoplasty than post-bariatric surgery, and be aware of that their post-abdominoplasty BMI may not decrease in the long term.
Address for correspondence:
Dr. P. W. Plaisier
Department of Surgery
Albert Schweitzer Hospital
P.O. Box 444, 3300 AK Dordrecht
The Netherlands
E-mail: p.w.plaisier@asz.nl
Zdroje
1. Arthurs ZM., Cuadrado D., Sohn V., Wolcott K., Lesperance K., Carter P., Sebesta J. Post-bariatric panniculectomy: pre-panniculectomy body mass index impacts the complication profile. Am. J. Surg., 193, 2007, p. 567–570; discussion 70.
2. Champault A., Duwat O., Polliand C., Rizk N., Champault GG. Quality of life after laparoscopic gastric banding: Prospective study (152 cases) with a follow-up of 2 years. Surg. Laparosc. Endosc. Percutan. Tech., 16, 2006, p. 131–136.
3. Hrabosky JI., Masheb RM., White MA., Rothschild BS., Burke-Martindale CH., Grilo CM. A prospective study of body dissatisfaction and concerns in extremely obese gastric bypass patients: 6 - and 12-month postoperative outcomes. Obes. Surg., 16, 2006, p. 1615–1621.
4. Pecori L., Serra Cervetti GG., Marinari GM., Migliori F., Adami GF. Attitudes of morbidly obese patients to weight loss and body image following bariatric surgery and body contouring. Obes. Surg., 17, 2007, p. 68–73.
5. Rogliani M., Silvi E., Labardi L., Maggiulli F., Cervelli V. Obese and nonobese patients: complications of abdominoplasty. Ann. Plast. Surg., 57, 2006, p. 336–338.
6. Salameh JR. Bariatric surgery: past and present. Am. J. Med. Sci., 331, 2006, p. 194–200.
7. Sanger C., David LR. Impact of significant weight loss on outcome of body-contouring surgery. Ann. Plast. Surg., 56, 2006, p. 9–13.
8. Santry HP., Gillen DL., Lauderdale DS. Trends in bariatric surgical procedures. JAMA, 294, 2005, p. 1909–1917.
9. Schechner SA., Jacobs JS., O’Loughlin KC. Plastic and reconstructive body contouring in the post-vertical banded gastroplasty patient: a retrospective review. Obes. Surg., 1, 1991, p. 413–417.
10. Song AY., Rubin JP., Thomas V., Dudas JR., Marra KG., Fernstrom MH. Body image and quality of life in post massive weight loss body contouring patients. Obesity (Silver Spring). 14, 2006, p. 1626–1636.
11. Taylor J., Shermak M. Body contouring following massive weight loss. Obes. Surg., 14, 2004, p. 1080–1085.
12. Topaloglu S., Avsar FM., Ozel H., Babacan M., Berkem H., Yildiz Y., Hengirmen S. Comparison of bariatric and non-bariatric elective operations in morbidly obese patients on the basis of wound infection. Obes. Surg., 15, 2005, p. 1271–1276.
13. Vastine VL., Morgan RF., Williams GS., Gampper TJ., Drake DB., Knox LK., Lin KY. Wound complications of abdominoplasty in obese patients. Ann. Plast. Surg., 42, 1999, p. 34–39.
Štítky
Chirurgie plastická Ortopedie Popáleninová medicína Traumatologie
Článek vyšel v časopiseActa chirurgiae plasticae
Nejčtenější tento týden
2007 Číslo 4- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Neodolpasse je bezpečný přípravek v krátkodobé léčbě bolesti
- Léčba akutní pooperační bolesti z pohledu ortopeda
-
Všechny články tohoto čísla
- TREPHINATIONS – OLD SURGICAL INTERVENTION
- ČESKÉ SOUHRNY
- CONTENTS
- INDEX
- Our First Experience with Primary Lip Repair in Newborns with Cleft Lip and Palate
- DENTURE RECONSTRUCTION OF THE EDENTULOUS UPPER JAW IN CLEFT PALATE USING IMPLANTS – CLINICAL REPORT
- SATISFACTION AND COMPLICATIONS IN POST-BARIATRIC SURGERY ABDOMINOPLASTY PATIENTS
- NECROTIZING FASCIITIS AFTER LIPOSUCTION
- Acta chirurgiae plasticae
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Our First Experience with Primary Lip Repair in Newborns with Cleft Lip and Palate
- TREPHINATIONS – OLD SURGICAL INTERVENTION
- NECROTIZING FASCIITIS AFTER LIPOSUCTION
- SATISFACTION AND COMPLICATIONS IN POST-BARIATRIC SURGERY ABDOMINOPLASTY PATIENTS
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání