-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
NEO-PHALLOPLASTY WITH RE-INNERVATED LATISSIMUS DORSI FREE FLAP: A FUNCTIONAL STUDY OF A NOVEL TECHNIQUE
Autoři: R. Ranno 1; J. Veselý 1; P. Hýža 1; I. Stupka 1; I. Justan 1; Z. Dvořák 1; N. Monni 1; P. Novák 1; S. Ranno 2
Působiště autorů: Clinic of Plastic and Aesthetic Surgery, St. Anna University Hospital, Masaryk University in Brno Czech Republic, and 1; Clinic of Urology, University of Catania, Italy 2
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 49, 1, 2007, pp. 3-7
INTRODUCTION
Penis reconstruction in female-to-male transsexual is common operation in specialized centres, but we have to confirm that not all of the transsexuals require this surgery. Needs of the patients are different in the concepts of expected result of penis reconstruction.
Hoopes in 1969 thought that from the view of the patient, a simple abdominal tube pedicle flap phallus not containing a urethra provides considerable physiological security, a phallus serving a urinary function is entirely satisfactory, and a phallus capable of sexual activity is too much to be hoped for. He considered the “fear of discovery” a strongly motivating factor in many of these patients (12, 13).
Edgerton and Meyer in 1973 stated that some patients express an interest only in achieving the ability to function sexually like a male, whereas others are more concerned with obtaining patterns of voiding like a male (7).
Later on, in 1983, Edgerton reported to have experienced that virtually all patients undergoing this type of reconstruction wish, almost equally, to be able to 1 – stand voiding, 2 – have sufficient rigidity in the penile shaft that they may engage in sexual intercourse (8).
Although there appears to be an evolution in the wishes and goals of the patients, the boundaries of technical expertise have always influenced the interpretation by the surgeon of the patient’s desire (27, 35). Davies and Matti, for example, in 1988 still commented that from patient’s interviews, the operations provide a major goal for female gender reassignment, giving a patient the male symbol of a phallus even if it does not function correctly (6).
Several different neo-phallus techniques were described in past years. Bogoras in 1936 was the first to report a total penile reconstruction, using a single abdominal tube (3). After him, many authors described and published several different procedures with local flaps (5, 9, 14, 16, 17, 21). But in 1980s, neo-phalloplasty changed direction. Actually the introduction of microvascular free flap has changed common opinion about operation selection. Free flap phalloplasty now represents the condition to obtain the best result in this procedure (2, 4, 10, 11, 18, 19, 22). Nevertheless, useful techniques with local flaps are used by some authors, mainly for those cases of neo-phalloplasty where microsurgery is not possible (15, 20).
Formerly, various methods, mostly radial forearm free flap either itself or in combination with other flaps, were used for total phalloplasties with urethra in female-to-male transsexuals at the Clinic of Plastic and Aesthetic Surgery, Masaryk University in Brno (23–26). However, the difficulties with obtaining functional urethra, mainly repeated surgeries for closures of fistulae, discouraged some transsexual patients from urethral reconstruction. Lately, main concern of some patients was to obtain sufficient rigidity of the neo - phallus.
Since December 2001, free re-innervated LD musculocutaneous flap has been employed to enable patients to have sexual intercourse and soft flaccid penis in quiescent phase. The technique used has been similar to that described by Adimian et al. (1). The purpose of this study is to quantify function, size and shape changes of the neo-phallus.
MATERIALS AND METHODS
All patients undergoing the neo-phalloplasty with re-innervated LD myocutaneous free flap were operated by one senior surgeon. The patients were followed-up for 26.4 months at mean and evaluated, measuring the size and dimension of the neo-phallus in relaxed and contracted positions.
Surgical technique
A longitudinal lazy “S” or transverse incision along the medial region of the thigh is done to expose recipient vessels and motor nerve of gracilis muscle (medial circumflex femoral vessels and a branch of the obturator nerve to gracilis). A LD myocutaneous free flap of both length and width approximately 14 cm with approximately 12 x 4 cm calf of muscle is designed on the back (Fig. 1a, b). Distance of the skin paddle is set about 13 cm from axilla. The pedicle is elongated by intramuscular dissection of the lateral branch of thoracodorsal artery from the entry of thoracodorsal artery to the latissimus dorsi muscle for about 3 to 4 cm. The skin paddle is designed over lower three/quarters of the muscle calf; the upper quarter of the muscle, which remains outside the cutaneous paddle, is later used for attachment to the pubic area.
Fig. 1. a – Design of the flap on the back, b – Elevation of the flap, c – Flap rolled into the shape of the neo-phallus, d – Neo-phallus transferred to the recipient site 
Lateral branches of the thoracodorsal vessels are carefully protected. After the flap is harvested, it is rolled into a cylinder to obtain the desired shape (Fig. 1c). Skin margins are sutured together with absorbable intradermal running suture (3–4/0 braided lactomer 9–11). The neurovascular thoracodorsal pedicle is divided at its origin or elongated with subscapular vessels. The donor site is in part sutured directly, and in part skin mesh grafted. The flap is transferred and sutured to the recipient pubic area after the patient is turned into supine position (Fig. 1d). The muscle calf is attached with non-absorbable stitches (2–3/0 polypropylene) to the anterior layer of rectus abdominis sheath. The thoracodorsal pedicle is passed through a subcutaneous tunnel to the thigh and anastomosed to recipient vessels; motor nerve suture is sutured to the anterior branch of obturator nerve which runs to the gracilis muscle.
Postoperatively, the patients were advised to have done electrostimulation of motor nerve and of muscle of the flap with a frequency of at least 3 times a week. After beginning of active muscle movement, electrogymnastics continued 3 times a week until satisfactory voluntary movement of the muscle was obtained.
Patient’s examination
Patients were asked to perform several contractions of the neo-phallus by adducting the thigh and flexing the calf. The presence of muscle movement was documented by the physician. In the studied patients, when a satisfactory voluntary movement of the muscle was obtained, the neo-phallus dimensions (length and circumference) were measured in the relaxed and contracted positions and data recorded. The ability of having sexual intercourse and onset of muscle movement was examined by the questionnaire.
RESULTS
All the flaps used for penile reconstruction in female to male transsexuals during given period survived. The onset of muscle movement was noted at mean 4.25 months (ranged from 3 to 13 months). The range of neo-phallus length in relaxed position was between 7 and 17 cm (mean 12.2 cm); its circumference in the same position had a range between 13 and 20 cm (mean 13.7 cm) (Fig. 2a, b). All examined patients were able to voluntarily contract the transferred LD muscle with an average length reduction of 3.08 cm and an average circumference augmentation of 4 cm which represents augmentation of 0.6 cm in diameter (Table 1, Fig. 3a, b). The ability of sexual intercourse is also shown in Table 1.
Fig. 2. Neo-phallus: a – relaxed, b – contracted 
Fig. 3. Measurement of the neo-phallus: a – relaxed, b – contracted 
Tab. 1. Neo-phallus length, circumference, and ability of sexual intercourse 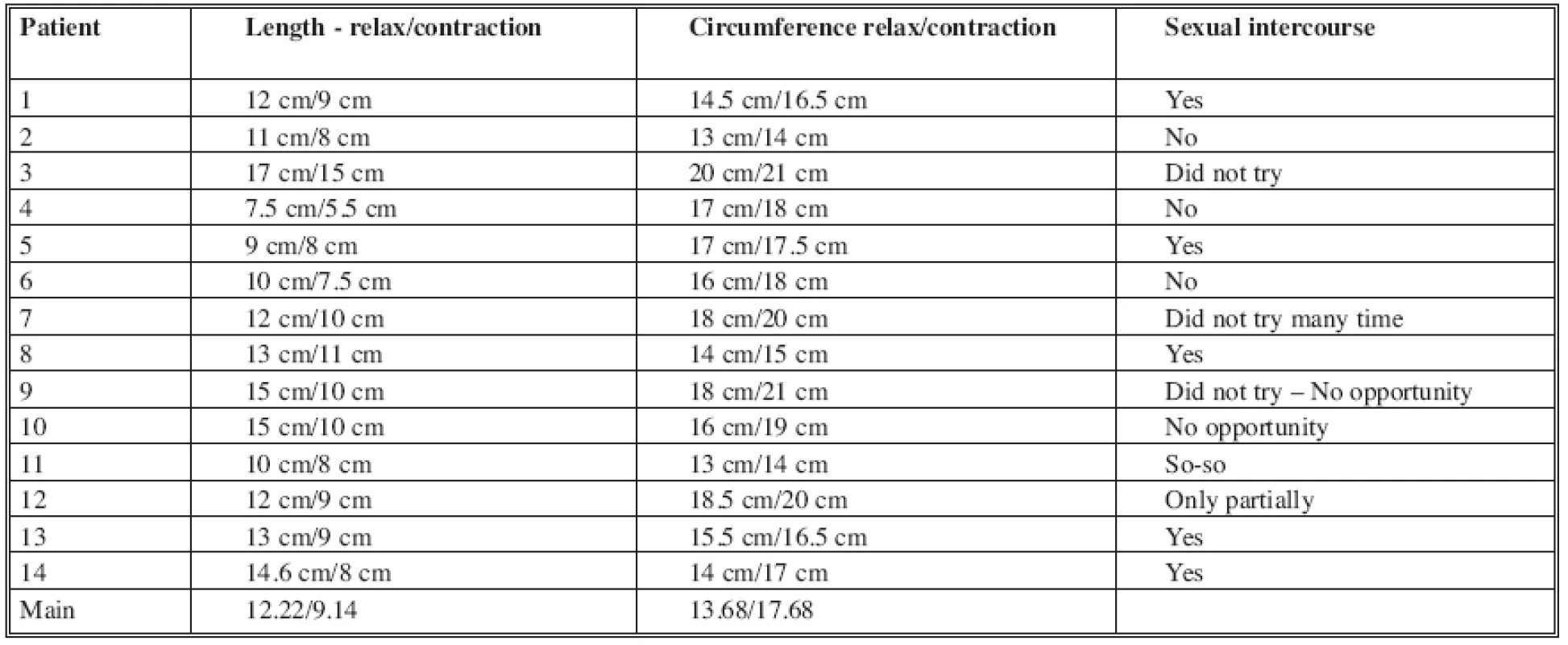
DISCUSSION
In the Clinic of plastic and aesthetic surgery of St. Anna University Hospital in Brno, Czech Republic, 38 patients with gender dysphoria underwent the sex reassignment using a novel technique. All the patients were operated by one surgeon. The re-innervated LD free flap was used to allow voluntary rigidity. The re-innervation was permitted suturing the anterior branch of obturator nerve of gracilis with thoracodorsal motor nerve. After the follow-up period, all of the examined patients were able to contract and elevate the neo-penis. Flexion of the calf and adduction of the thigh induced muscle contraction; repeated contractions were also possible. Although the muscle contraction shortened and widened the neo-phallus, it became suitable for sexual intercourse. The significance of the extent of this movement may be matter of discussion. Nevertheless, the muscle contraction produced significant stiffening of the neo-phallus. This “paradox” or “reverse” erection (stiffening, but shortening and widening of the neo-phallus) enabled sexual intercourse by inserting either contracted or non-contracted neo-phallus into vagina and subsequent repeated intermittent contractions and releases of the muscle. The size of the neo-phallus has shown to be crucial in the view of the ability of penetration. Some difficulties arose in overweight patients when the neo-phallus was too thick. Five of the patients, who performed sexual intercourse, used the muscle contraction to stiffen the penis. Some of them also moved the muscle by adducting the thigh and flexing the calf during sexual intercourse, which produced changes of size and shape of the phallus. Seven of the patients didn’t have the opportunity for sexual intercourse, and 2 performed only partially (see Tab. 1). We consider the selection of recipient obturator nerve as favourable, because the contraction of adductors and gracilis muscles permits strong intentional movement of the transplanted muscle, but does not cause negligible involuntary movements of neo-phallus during walking. However, certain limitations were seen from fading of the muscle after prolonged repeated contractions.
CONCLUSION
The chance of this safe technique to achieve voluntary rigidity in order to allow sexual intercourse by means of the transplanted muscle’s activation, without the use of any prosthesis, make it our first choice procedure in phallic reconstruction for female-to-male gender dys-phoria, when it is indicated. The muscle contraction of the neo-phallus leads to the changes of diameter length and shape – the “paradox erection” (stiffening but widening and shortening of the neo-penis); some patients are able to take advantage of these properties for sexual intercourse.
Address for correspondence:
Raul L. M. Ranno, MD.
Via Francicanava 22
95030, Sant’Agata Li Battiati (CT)
Italy
E-mail: raulranno@hotmail.com
Zdroje
1. Adamian R., Zelyanin N., Milanov NO. Total phalloplasty in the treatment of transsexuals. In Proceedings of 8th Annual Meeting of European Association of Plastic Surgeons Euraps, Amsterdam, The Netherlands. May 15–17, 1996.
2. Biemer E. Penile construction by the radial arm flap. Clin. Plast. Surg., 15, 1988, p. 425.
3. Bogoras N. Über die volle plastische Wiederherstellung eines zum Koitus fahigen Penis (Peni plastica totalis). Zentralbl. Chir., 22, 1936, p. 1271.
4. Chang TS., Hwang WY. Forearm flap in one-stage reconstruction of the penis. Plast. Reconstr. Surg., 74, 1984, p. 251.
5. Cheng KX., Hwang WY., Eid AE., et al. Analysis of 136 cases of reconstructed penis using various methods. Plast. Reconstr. Surg., 95, 1995, p. 1070.
6. Davies DM., Matti BA. A method of phalloplasty using the deep inferior epigastric flap. Br. J. Plast. Surg., 41, 1988, p. 165.
7. Edgerton MT. Transsexualism – a surgical problem? Plast. Reconstr. Surg., 52, 1973, p. 74.
8. Edgerton MT. Female to male transsexual conversion: a 15-year follow up (Discussion). Plast. Reconstr. Surg., 72, 1983, p. 240.
9. Gillies HD., Harrison RJ. Congenital absence of the penis. Br. J. Plast. Surg., 1, 1948, p. 8.
10. Hage JJ., de Graaf FH., van den Hoek J., Bloem JJ. Phallic construction in female-to-male transsexuals using a lateral upper arm sensate free flap and a bladder mucosa graft. Ann. Plast. Surg., 31, 1993, p. 275.
11. Harashina T., Inoue T., Tanaka I., et al. Reconstruction of the penis with free deltoid flap. Br. J. Plast. Surg., 43, 1990, p. 217.
12. Hoopes JE. Operative treatment of the female transsexual. In Green R, Money J (Eds), Transsexualism and sex reassignment. Baltimore: John Hopkins, 1969, pp 335–354.
13. Hoopes JE. Surgical construction of the male external genitalia. Clin. Plast. Surg., 1(2), 1974, p. 325–334.
14. Matti BA., Matthews RN., Davies DM. Phalloplasty using the free radial forearm flap. Br. J. Plast. Surg., 41, 1988, p. 160.
15. Mutaf M. Nonmicrosurgical use of the radial forearm flap for penile reconstruction. Plast. Reconstr. Surg., 107, 2001, p. 80.
16. Orticochea MA. New method of total reconstruction of the penis. Br. J. Plast. Surg., 25, 1972, p. 347.
17. Perovic S. Phalloplasty in children and adolescents using the extended pedicle island groin flap. J. Urol., 154, 1995, p. 848.
18. Pukett CL., Reinish JF., Montie JE. Free flap phalloplasty. J. Urol., 128, 1982, p. 294.
19. Sadove RC., McRoberts JW. Total phallic reconstruction with the free fibula osteocutaneous flap. Plast. Reconstr. Surg., 89, 1992, p. 1001.
20. Santanelli F., Scuderi N. Neo-phalloplasty in female-to-male transsexuals with the island tensor fasciae latae flap. Plast. Reconstr. Surg., 105, 2000, p. 1990.
21. Santi P., Berrino P., Canadese G., et al. Immediate reconstruction of the penis using an inferiorly based rectus abdominis myocutaneous flap. Plast. Reconstr. Surg., 81, 1988, p. 961.
22. Upton J., Mutimer KL., Loughlin K., et al. Penile reconstruction using the lateral arm flap. J. R. Coll. Surg. Edinb., 97, 1987, p. 97.
23. Veselý J., Bařinka L., Santi P., et al. Reconstruction of the penis in transsexual patients. Acta Chir. Plast., 34, 1992, p. 44.
24. Veselý J., Procházka V., Válka J., et al. Use of two microsurgical flaps in one stage reconstructive surgery. Acta Chir. Plast., 36, 1994, p. 99.
25. Veselý J., Kučera J., Hrbatý J., et al. Our standard method of reconstruction of the penis and urethra in female transsexuals. Acta Chir. Plast., 41, 1999, p. 39.
26. Veselý J., Haage J. From the history of penis reconstruction. Acta Chir. Plast., 41, 1999, p. 43.
Štítky
Chirurgie plastická Ortopedie Popáleninová medicína Traumatologie
Článek ČESKÉ SOUHRNY
Článek vyšel v časopiseActa chirurgiae plasticae
Nejčtenější tento týden
2007 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Neodolpasse je bezpečný přípravek v krátkodobé léčbě bolesti
- Léčba akutní pooperační bolesti z pohledu ortopeda
-
Všechny články tohoto čísla
- COMBINATION OF POSTERIOR INTEROSSEOUS AND HYPOGASTRIC FLAP FOR SKIN DEFECT RECONSTRUCTION IN HAND INJURIES
- BURIED UMBILICUS: AN IATROGENIC CAUSE OF A DISCHARGING UMBILICAL WOUND
- A new method of skin erythrosis evaluation in digital images
- ČESKÉ SOUHRNY
- NEO-PHALLOPLASTY WITH RE-INNERVATED LATISSIMUS DORSI FREE FLAP: A FUNCTIONAL STUDY OF A NOVEL TECHNIQUE
- AN OBJECTIVE EVALUATION OF CONTRACTION POWER OF NEO-PHALLUS RECONSTRUCTED WITH FREE RE-INNERVATED LD IN FEMALE-TO-MALE TRANSSEXUALS
- Acta chirurgiae plasticae
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- NEO-PHALLOPLASTY WITH RE-INNERVATED LATISSIMUS DORSI FREE FLAP: A FUNCTIONAL STUDY OF A NOVEL TECHNIQUE
- AN OBJECTIVE EVALUATION OF CONTRACTION POWER OF NEO-PHALLUS RECONSTRUCTED WITH FREE RE-INNERVATED LD IN FEMALE-TO-MALE TRANSSEXUALS
- A new method of skin erythrosis evaluation in digital images
- COMBINATION OF POSTERIOR INTEROSSEOUS AND HYPOGASTRIC FLAP FOR SKIN DEFECT RECONSTRUCTION IN HAND INJURIES
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



