-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
AN OBJECTIVE EVALUATION OF CONTRACTION POWER OF NEO-PHALLUS RECONSTRUCTED WITH FREE RE-INNERVATED LD IN FEMALE-TO-MALE TRANSSEXUALS
Autoři: R. Ranno 1; P. Hýža 1; J. Veselý 1; L. A. Dessy 2; Z. Kadaňka 3
Působiště autorů: Clinic of Plastic and Aesthetic Surgery, and 3Department of Neurology, St. Anna University Hospital, Masaryk University, Brno, Czech Republic, and 1; Department of Plastic Surgery, University “La Sapienza”, Rome, Italy 2
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 49, 1, 2007, pp. 8-12
INTRODUCTION
Despite the anatomic and clinical advantages of current techniques for phalloplasty, the outcome of reconstruction is still far from an optimal result. Particularly, natural sexual function of the neo-phallus is not easily achievable. The use of transplants and implants in order to obtain sufficient rigidity for penetration has often led to complications, and failures of different free and pedicle flaps (8, 10, 12). Autologous cartilage and bone transplants, used to avoid these complications, cause a permanent rigidity which is embarrassing to the patient. Moreover, these tissues could tend to reabsorb, bend or fracture (8). Alloplastic prostheses have the possibility to give an erection to the neo-phallus, although they are expensive and have a tendency to tissue erosion and extrusion, infection, tissue atrophy, penile fibrosis and mechanical failure.
In the attempt to reduce complications, surgeons modified existing techniques or introduced new ones (2–7, 9, 11, 13, 16, 18–21, 23, 24, 26). Adamian was the first to use re-innervated latissimus dorsi (LD) free flap for total phalloplasty (1).
Overtime, various techniques have been used for total phalloplasties in female-to-male transsexuals in the Plastic and Aesthetic Surgery Clinic of Masaryk University in Brno (26–29). Since 2001, the free re-innervated LD musculocutaneous flap has been performed in order to obtain sufficient rigidity of neo-phallus for sexual intercourse due to voluntary contraction of the LD muscle and soft flaccid penis in the quiescent phase. Some patients are able to have sexual intercourse with this type of reconstruction, while others are not. The conditions under which the reconstruction is successful are not fully understood and contraction strength of the muscle, which provides rigidity of the neo-phallus, might be a significant factor.
The aim of this study was objective evaluation of the contraction power of the transplanted muscle in the neo-phallus for further assessment of functional results.
MATERIALS AND METHODS
From December 2001 to September 2005, twenty two female-to-male transsexuals underwent neo-phalloplasty using the above mentioned technique in the Clinic of Plastic and Aesthetic surgery of the St. Anna University Hospital in Brno. Mean patients’ age was 28.6 years (ranged from 24 to 38 years) and the average follow-up was 26.4 months. All operated patients were invited for examinations, 14 of them collaborated and were included in this study; the contraction power of the neo-phallus was objectively evaluated (Table 1).
Tab. 1. Objective data obtained through EMG and power assessment in the studied group of patients 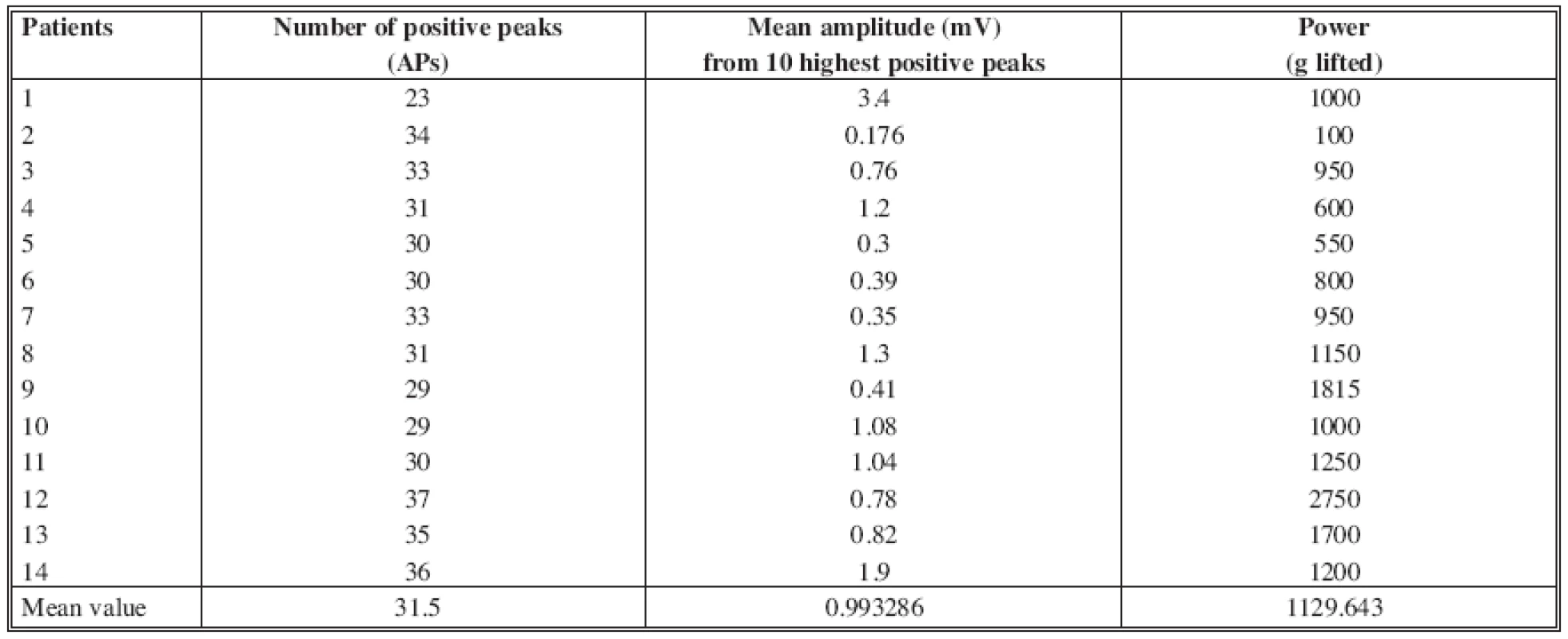
Surgical technique
The penis was built on the back from musculocutaneous latissimus dorsi flap by rolling up the cutaneous part of the flap into a cylindric shape. The longitudinal strip of muscle inside the neo-phallus constituted the motoric unit of the neo-phallus. The vascular pedicle and motoric nerve of the free flap was anastomosed end-to-end to the main vascular pedicle of the gracilis muscle and its motoric nerve coming from obturator nerve on the left thigh.
Rehabilitation
Starting after skin healing, all patients were subjected to a rehabilitation protocol of the transferred muscle. The protocol included electro-stimulation of the motor nerve and the LD muscle of the neo-phallus with a frequency of at least 3 times a week for at least 6 months. After beginning of active muscle movement, electro-gymnastic continued 3 times a week until satisfactory voluntary movement of the muscle was obtained.
Physical examination
Postoperatively, the patients were examined by the surgeon in regular intervals of 2 to 3 months. Patients were asked to perform several contractions of the neo-phallus by adducting the thigh and flexing the calf. The onset of voluntary contraction of the neo-phallus was recorded.
Objective evaluation
In the studied patients, the neo-phallus contraction power was objectively evaluated by measuring the maximum weight lifted, and by electromyography (EMG). For power evaluation, patients were asked to voluntarily lift different weights with the neo-phallus. The weights started from 50 g up to the maximum possible weight; the elevation of at least 2 cm was considered as successful contraction which had lifted given weight.
Electromyography
The neo-phallus muscle activity was registered using an electromyograph Keypoint (Dantec, Denmark), with a bipolar needle electrode, settings 10 ms/div., 0.1 and 1 mV/div. The number of positive peaks (APs) from the record of 100 ms and the amplitude values (in mV) of 10 highest positive peaks were counted.
RESULTS
Conventional physical examination test revealed the viability of the transplanted muscle in this series of patients, being able to contract and elevate the neo-penis (Fig. 1a, b). Flexion of the calf and adduction of the thigh induced muscle contraction with shortening and widening of the neo-penis; repeated contractions were possible for at least 3 minutes in all patients who demonstrated muscle contraction. The onset of muscle movement was noted after an average of 4.25 months (ranging from 3 to 13 months). Electro-stimulation was continued to obtain a satisfactory voluntary movement of the muscle for an average period of 5.5 months (ranging from 3 to 10 months).
Fig. 1. Movement of the neo-phallus: a – relaxed neo-phallus, b – contracted neo-phallus 
Objective evaluation
In the 14 studied patient, the average weight lifted was 1129 g (min 100 g, max 2750 g) (Fig. 2a, b). After electromyography, the mean number of APs in the 100 ms period was 31.5 (min 23, max 37, Fig. 3). The mean amplitude from 10 highest positive peaks, measured peak-to-peak, was 0.99 mV (min 0.176 mV, max 3.4, see Fig. 3).
Fig. 2. Measurement of the muscle power by elevation of the weight: a – relaxed neo-phallus, b – contracted neo-phallus 
Fig. 3. Electromyographic record of the muscle contraction 
DISCUSSION
The goals of total phalloplasty represent a continuous challenge for plastic surgeons. These aim to both cosmetic and functional results, but none of the techniques reported in the literature can fully satisfy them.
An ideal neo-phallus should permit the patient urinate in a standing position and to engage in sexual intercourse with erogenous sensations. In addition, one-stage predictably reproducible procedure with minimal donor site morbidity is the desired goal of this reconstruction.
The need of a proper penile stiffness for the sexual intercourse has been managed in two ways: prosthetic devices (penile implants, external stiffeners, temporary stiffeners) or autologous materials. The prosthesis has the possibility to give a voluntary erection to the penis, and so permitting to engage in sexual intercourse, although they have certain disadvantages already mentioned.
Resorption, softening or fracture of autologous materials such as cartilage or bone grafts led to unsatisfactory results (8). Also, a permanent rigidity can make the patient uncomfortable or embarrassed. However, recent study of Sengezer showed persuasive results and long term stability of vascularized fibula flap used for penile reconstruction (22).
We think that the best reconstruction should be done with autologous tissues. Another requirement is the ability of the neo-phallus to voluntary change in stiffness to allow sexual intercourse.
In this study, the voluntary contraction power of the neo-phallus reconstructed with the re-innervated free LD flap was analysed with objective instruments to give data for assessment and comparison.
The first successful functional muscle transplantation was reported in 1970 (25). We selected the functional LD free flap for the amount of the skin and muscular paddle, as well as for the length of the pedicle. Besides, the scar on the back is usually well accepted by the patients. We believe that the most critical part of the functional muscle transfer is the nerve selection and adjustment (14, 15, 17). In order to minimize the time of muscle denervation, the nerve coaptation was placed as closely as possible to the neuromuscular junction. As a recipient nerve the anterior branch of the obturator nerve proved to be the best for its proximity. To achieve best functional result, the electro-stimulation began soon after the surgery and continued until satisfactory voluntary contraction was obtained. Then, the electro-stimulation was followed by electro-gymnastic for several months to improve muscle movement. The contraction of the adductors and gracilis muscles permits deliberate contraction of the transplanted muscle and cause negligible involuntary movements during walking.
Electromyographic findings document that contraction and movement of the artificial penis are based on re-innervation and subsequent contraction of the transferred muscle in it. The contraction power reached makes the neo-phallus suitable for sexual intercourse by its stiffening and movement, although the muscle contraction shortens and widens the neo-phallus. This voluntary “paradox erection” enables sexual intercourse by inserting either contracted or non-contracted neo-phallus into vagina and subsequent repeated intermittent contractions and releases of the muscle. This fact is one of the reasons that nowadays make the neo-phalloplasty with re-innervated LD free flap the method preferred by most of our patients.
CONCLUSION
In conclusion, this neo-phalloplasty technique gives the patient ability for having sexual intercourse without the need for prosthesis. The voluntary contraction of the neo-phallus appears soon after the surgery. We believe that early rehabilitation protocol is one of the necessary conditions for successful re-innervation of the transplanted muscle. Our findings document objectively that this voluntary contraction of the artificial penis is a consequence of the re-innervation of the transferred muscle and the contraction is strong enough to stiffen the neo-phallus. Also, the data obtained represent useful tool for clinical assessment and comparison.
Address for correspondence:
Raul L. M. Ranno, MD.
Via Francicanava 22
95030, Sant’Agata Li Battiati (CT)
Italy
E-mail: raulranno@hotmail.com
Zdroje
1. Adamian R., Zelyanin N., Milanov NO. Total phalloplasty in the treatment of transsexuals. In Proceedings of 8th Annual Meeting of European Association of Plastic Surgeons Euraps, Amsterdam, The Netherlands. May 15–17, 1996.
2. Akoz T., Kargi E. Phalloplasty in a female-to-male transsexual using a double-pedicle composite groin flap. Ann. Plast. Surg., 48, 2002, p. 423.
3. Chen YB., Chen HC. Penile reconstruction for a victim of electrical injury with bilateral below-elbow amputations. Plast. Reconstr. Surg., 87, 1991, p. 771.
4. Davies DM., Matti BA. A method of phalloplasty using the deep inferior epigastric flap. Br. J. Plast. Surg., 41, 1988, p. 165.
5. Gilbert DA., Horton CE, Terzis J-K, et al. New concepts in phallic reconstruction. Ann. Plast. Surg., 18, 1987, p. 128.
6. Gilbert DA., Schlossberg SM., Jordan GH. Ulnar forearm phallic construction and penile reconstruction. Microsurgery, 16, 1995, p. 314.
7. Hage JJ. Metaidoioplasty: an alternative phalloplasty technique in transsexuals. Plast. Reconstr. Surg., 97, 1996, p. 161.
8. Hage JJ., Bloem JJ., Bouman FG. Obtaining rigidity in the neophallus of female-to-male transsexuals: a review of the literature. Ann. Plast. Surg., 30, 1993, p. 327.
9. Hage JJ., de Graaf FH., van den Hoek J., Bloem JJ. Phallic construction in female-to-male transsexuals using a lateral upper arm sensate free flap and a bladder mucosa graft. Ann. Plast. Surg., 31, 1993, p. 275.
10. Hage JJ. Dynaflex prosthesis in total phalloplasty. Plast. Reconstr. Surg., 99, 1997, p. 479.
11. Harashina T., Inoue T., Tanaka I., et al. Reconstruction of the penis with free deltoid flap. Br. J. Plast. Surg., 43, 1990, p. 217.
12. Jordan GH., Alter GJ., Gilbert DA., et al. Penile prosthesis implantation in total phalloplasty. J. Urol., 152, 1994, p. 410.
13. Koshima I., Tai T., Yamasaki M. One-stage reconstruction of the penis using an innervated radial forearm osteocutaneous flap. J. Reconstr. Microsurg., 3, 1986, p. 19.
14. Manktelow RT., Zuker RM. The principles of functioning muscle transplantation: Applications to the upper arm. Ann. Plast. Surg., 22, 1989, p. 275.
15. McKee NH., Kuzon, MW. Jr. Functioning free muscle transplantation: Making it work? What is known? Ann. Plast. Surg., 23, 1989, p. 249.
16. Mutaf MA. New surgical procedure for phallic reconstruction: Istanbul flap. Plast. Reconstr. Surg., 105, 2000, p. 1361.
17. Ninkovic M., Sucur D., Starovic B., Markovic S. A new approach to persistent traumatic peroneal nerve palsy. Br. J. Plast. Surg., 47, 1994, p. 185.
18. Perovic S. Phalloplasty in children and adolescents using the extended pedicle island groin flap. J. Urol., 154, 1995, p. 848.
19. Sadove RC., Sengezer M., McRoberts JW., Wells MD. One-stage total penile reconstruction with a free sensate osteocutaneous fibula flap. Plast. Reconstr. Surg., 92, 1993, p. 1314.
20. Sasaki K., Nozaki M., Morioka K., et al. Penile reconstruction: combined use of an innervated forearm osteocutaneous flap and big toe pulp. Plast. Reconstr. Surg., 104, 1999, p. 1054.
21. Semple JL., Boyd JB., Farrow GA., Robinette MA. The “cricket bat” flap: a one-stage free forearm flap phalloplasty. Plast. Reconstr. Surg., 88, 1991, p. 514.
22. Sengezer M., Vztrk S., Deveci M., Odabas Z. Long-term follow-up of total penile reconstruction with sensate osteocutaneous free fibula flap in 18 biological male patients. Plast. Reconstr. Surg., 114, 2004, p. 439.
23. Shenaq SM., Dinh TA. Total penile and urethral reconstruction with an expanded sensate lateral arm flap: case report. J. Reconstr. Microsurg., 5, 1989, p. 245.
24. Sun GC., Huang JJ. One-stage reconstruction of the penis with composite iliac crest and lateral groin skin flap. Ann. Plast. Surg., 15, 1985, p. 519.
25. Tamai S., Komatsu S., Sakamoto H., et al. Free muscle transplants in dogs, with microsurgical neurovascular anastomoses. Plast. Reconstr. Surg., 46, 1970, p. 219.
26. Veselý J., Bařinka L., Santi P., et al. Reconstruction of the penis in transsexual patients. Acta Chir. Plast., 34, 1992, p. 44.
27. Veselý J., Procházka V., Válka J., et al. Use of two microsurgical flaps in one stage reconstructive surgery. Acta Chir. Plast., 36, 1994, p. 99.
28. Veselý J., Kučera J., Hrbatý J., et al. Our standard method of reconstruction of the penis and urethra in female transsexuals. Acta Chir. Plast., 41, 1999, p. 39.
29. Veselý J., Haage J. From the history of penis reconstruction. Acta Chir. Plast., 41, 1999, p. 43.
Štítky
Chirurgie plastická Ortopedie Popáleninová medicína Traumatologie
Článek ČESKÉ SOUHRNY
Článek vyšel v časopiseActa chirurgiae plasticae
Nejčtenější tento týden
2007 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Léčba bolesti po jednodenní chirurgii
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Neodolpasse je bezpečný přípravek v krátkodobé léčbě bolesti
-
Všechny články tohoto čísla
- COMBINATION OF POSTERIOR INTEROSSEOUS AND HYPOGASTRIC FLAP FOR SKIN DEFECT RECONSTRUCTION IN HAND INJURIES
- BURIED UMBILICUS: AN IATROGENIC CAUSE OF A DISCHARGING UMBILICAL WOUND
- A new method of skin erythrosis evaluation in digital images
- ČESKÉ SOUHRNY
- NEO-PHALLOPLASTY WITH RE-INNERVATED LATISSIMUS DORSI FREE FLAP: A FUNCTIONAL STUDY OF A NOVEL TECHNIQUE
- AN OBJECTIVE EVALUATION OF CONTRACTION POWER OF NEO-PHALLUS RECONSTRUCTED WITH FREE RE-INNERVATED LD IN FEMALE-TO-MALE TRANSSEXUALS
- Acta chirurgiae plasticae
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- NEO-PHALLOPLASTY WITH RE-INNERVATED LATISSIMUS DORSI FREE FLAP: A FUNCTIONAL STUDY OF A NOVEL TECHNIQUE
- AN OBJECTIVE EVALUATION OF CONTRACTION POWER OF NEO-PHALLUS RECONSTRUCTED WITH FREE RE-INNERVATED LD IN FEMALE-TO-MALE TRANSSEXUALS
- A new method of skin erythrosis evaluation in digital images
- COMBINATION OF POSTERIOR INTEROSSEOUS AND HYPOGASTRIC FLAP FOR SKIN DEFECT RECONSTRUCTION IN HAND INJURIES
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



