-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaProspective use of EuroSCORE for the short−term risk evaluation of consecutive cardiac surgery candidates: are there any differences in prediction of perioperative risk versus risk of nonsurgical treatments?
Role EuroSCORE pro prospektivní odhad krátkodobého rizika u kandidátů pro kardiochirurgickou operaci: Je přesnost EuroSCORE pro odhad perioperačního rizika stejná jako pro odhad rizika nechirurgické léčby?
V éře moderní medicíny je pro praxi kardiochirurga i kardiologa stále důležitější stratifikace perioperačního rizika.
Cíl:
Cílem této studie bylo zhodnocení přesnosti stratifikačního modelu EuroSCORE pro odhad krátkodobé mortality u české populace dospělých pacientů prezentovaných na kardiochirurgickém indikačním semináři.Metodika:
Studie zahrnuje všechny pacienty (n = 460) prezentované na indikačním semináři jako kardiochirurgické kandidáty během 6měsíčního období. K posouzení rizika byly použity aditivní a logistické EuroSCORE. Všechna úmrtí od operace až do 30 dnů od propouštění byla prospektivně zaznamenána. Skutečná mortalita byla porovnána s mortalitou odvozenou z EuroSCORE.Výsledky:
57 % pacientů podstoupilo kardiochirurgickou operaci, zatímco 43 % pacientů bylo kardiochirurgem odmítnuto. Mezi skutečnou a odvozenou mortalitou nebyl ani u jedné podskupiny zjištěn významný rozdíl. Aditivní i logistické EuroSCORE ukázalo dobrou diskriminační schopnost pro předpověď krátkodobého úmrtí (AUC = 0,755 a AUC = 0,762 pro chirurgickou skupinu; AUC = 0,695 a AUC = 0,716 pro odmítnutou skupinu).Závěr:
EuroSCORE má dobrou diskriminační schopnost pro predikci časného úmrtí u pacientů po kardiochirurgické operaci a rovněž i u pacientů odmítnutých kardiochirurgem. Obě formy EuroSCORE pro predikci rizika jsou vhodné pro předpověď úmrtí u českých kardiologických pacientů.Klíčová slova:
aditivní EuroSCORE – logistické EuroSCORE – předpověď úmrtí – pacienti indikovaní k operaci – pacienti odmítnutí k operaci
Authors: M. Klinčeva 1; P. Widimský 1; A. Dohnalová 2
Authors place of work: Cardiocenter, University Hospital Královské Vinohrady, Prague, head prof. MUDr. Petr Widimský, DrSc., FESC 1; Institute of Physiology, First Medical faculty of Charles University, Prague, head prof. MUDr. Otomar Kittnar, CSc. 2
Published in the journal: Vnitř Lék 2006; 52(12): 1156-1161
Category: Původní práce
Summary
Background:
In the era of modern medicine, the relevance of perioperative risk stratification with respect to the practice of cardiac surgeons and cardiologists worldwide has increased. Aim: This study aims at estimating the validity of a preoperative risk stratification model EuroSCORE in predicting short-term mortality in Czech adult cardiac population.Methods:
All consecutive patients (n = 460) presented to cardiac surgeons as surgery candidates during a six-month period were enrolled in this study. The Additive and logistic EuroSCORE were used for the risk assessment. The operative mortality, as well as the mortality within 30 days from discharge were recorded. The observed and predicted mortality derived from the EuroSCORE were compared.Results:
Fifty-seven percent of the patients underwent cardiac surgery, while 43 % was refused for surgery by the cardiac surgeon. There was no significant difference between the observed and predicted mortality in both subgroups. EuroSCORE showed good discriminatory ability in predicting short-term mortality (C statistic 0.755 vs. 0.762 for the surgery subgroup and 0.695 vs. 0.716 for the refused subgroup).Conclusions:
The EuroSCORE has a good discriminatory ability in predicting early mortality after cardiac surgery as well as in patients rejected for cardiac surgery. Both EuroSCORE risk prediction model forms are a suitable mortality predictor in Czech cardiac patients.Key words:
additive EuroSCORE – logistic EuroSCORE – mortality prediction – operated patients – non-operated patientsIntroduction
In the era of modern medicine, the relevance of perioperative risk stratification with respect to the practice of cardiac surgeons and cardiologists worldwide has increased.
This may be attributed to a higher public scrutiny of the results of cardiac surgeons and institutions as well as to a higher risk profile of the cardiac surgery candidate patients. Victor Parsonnet and colleagues published their risk stratification system in 1989 [1]. Since than, several other risk stratification scores have been developed [2–5]. The European System for Cardiac Operative Risk Evaluation (EuroSCORE) yielded the highest predictive value [6,7].
Nashef et al introduced the Euro-SCORE in 1999, as a tool in order to score the early mortality after cardiac surgery in cardiac patients with numerous risk factors [8]. The EuroSCORE was based on a large and tightly controlled database, comprising 19,030 patients drawn from 128 surgical centers in eight European countries. The system used univariate and logistic regression analysis to identify and give appropriate weight to the various risk factors related to early mortality and survival regarding adult cardiac surgery [9].
The additive (standard) form was first applied, using a number of points for each risk factor. It estimates the percentage of the predicted operative mortality for a patient undergoing a particular operation. Recently, the logistic model became available and proved to be a better risk predictor, especially in high risk patients (table 1) [10,11]. The logistic EuroSCORE model is calculated using the following formula:
Tab. 1. European System of Cardiac Operative Risk Evaluation (EuroSCORE) risk factors. 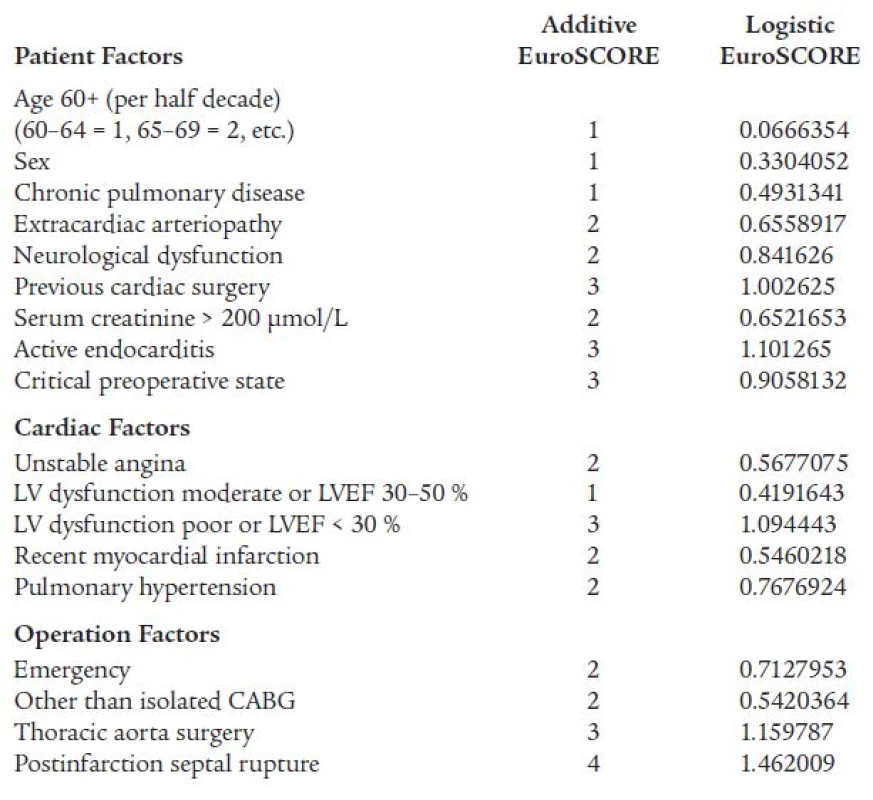
LV – left ventricular, LVEF – left ventricular ejection fraction, CABG – coronary artery bypass grafting There have been several studies from individual centers as well as regional studies examining the effectiveness of the EuroSCORE at the local level. To our knowledge this is the first study in the literature which tests the validity of a preoperative risk stratification model in predicting short-term mortality in Czech adult cardiac population. The higher risk profile of cardiac surgery candidate patients inspired us to test the validity of both forms of the EuroSCORE system in all patients referred to any type of cardiac surgery as well as of those which were refused.
Methods
Study population
Data were prospectively collected from a total of 460 consecutive patients who were presented to the cardiac surgeon as cardiac surgery candidates between September 2004 and March 2005 at the Cardiocenter, University Hospital Královské Vinohrady, Prague, the Czech Republic. From this group, 272 patients (59 %) were indicated for cardiac surgery and 188 patients (41%) were refused for cardiac surgery. Cardiac surgery candidate patients were refused due to: diffuse coronary atherosclerosis too extensive for surgery (n = 40; 22 %), high operative risks (n = 89; 47 %) or other reasons (n = 59; 31 %). The group of patients refused for cardiac surgery due to high operative risks comprised patients with a combination of polymorbidity, higher age (> 75 years), and ejection fraction less than 30 %. The group of patients refused due to other reasons involved either patients with borderline (intermediate) atherosclerosis lesions, a mild, minimal and stable symptoms at the time of referral to surgery or patient who refused the surgery.
Diffuse coronary atherosclerosis indicates a diffuse stenosis approaching the periphery of the coronary blood vessels. High operative risk due to polymorbidity means coexistence of advanced stages of multiple organ diseases (e.g. CNS, pulmonary, renal, peripheral arteries, hepatic etc). There were no exclusion criteria. The measured outcome was the mortality, defined as death within 30 days from operation or later than 30 days if still in hospital, while for refused patients mortality was defined as death during the hospital stay or 30 days after discharge.
To assess the risk factors for mortality in patients candidates for cardiac surgery we used both additive and logistic model of the European system for Cardiac Operative Risk Evaluation (EuroSCORE). Definitions of the risk factors were identical to the EuroSCORE definitions [8]. The additive EuroSCORE has been routinely calculated at the bedside of all patients presented to the cardiac surgeon, while the logistic model has been calculated by a calculator downloaded from the Euro-SCORE website (www.euroscore.org). Thirty-day mortality information was obtained by contacting the patient or a family member by telephone. The result from the surgery, were taken into account in the operated patients.
Statistical analysis
Quantitative and score variables were summarized in terms of mean values and SDs. Chi square test was used to compare categorical values between groups. Changes in quantitative variables between the groups were assessed with the student t test. Discrete variables are expressed as counts and percentages. Using the Univariate Cox regression analysis we tested whether the survival time depends on the standard and the logistic EuroSCORE.
The C statistic method (receiver operating curve) was used to assess the discriminatory ability of standard and logistic EuroSCORE. The area under the receiver operating characteristics curve was calculated as an indicator for how well the Euro-SCORE could discriminate patients who lived from those who died. The discriminatory power of the model is deemed excellent if the area under the receiver operating characteristic curve is 0.80, very good if it is greater than 0.75 and good if greater than 0.70. Statistical analyses were performed using the statistical SPSS 13.0 Software A p value of less than 0.05 was considered significant.
Results
Study population
Table 2 compares the variables utilized by the EuroSCORE model. Refused patients experienced poorer left ventricular function (EF < 30 %), chronic pulmonary disease, serum creatinin > 200 μmol/l and significantly higher EuroSCORE (p < 0.001). Eleven patients (4 %) of the patients indicated for cardiac surgery refused to be operated. They were included in the group of refused patients. Two patients indicated for cardiac surgery died before the operation. These deaths were excluded from the study, leaving a total of 458 patients for evaluation.
Tab. 2. Baseline characteristics of the patients candidates for cardiac surgery. 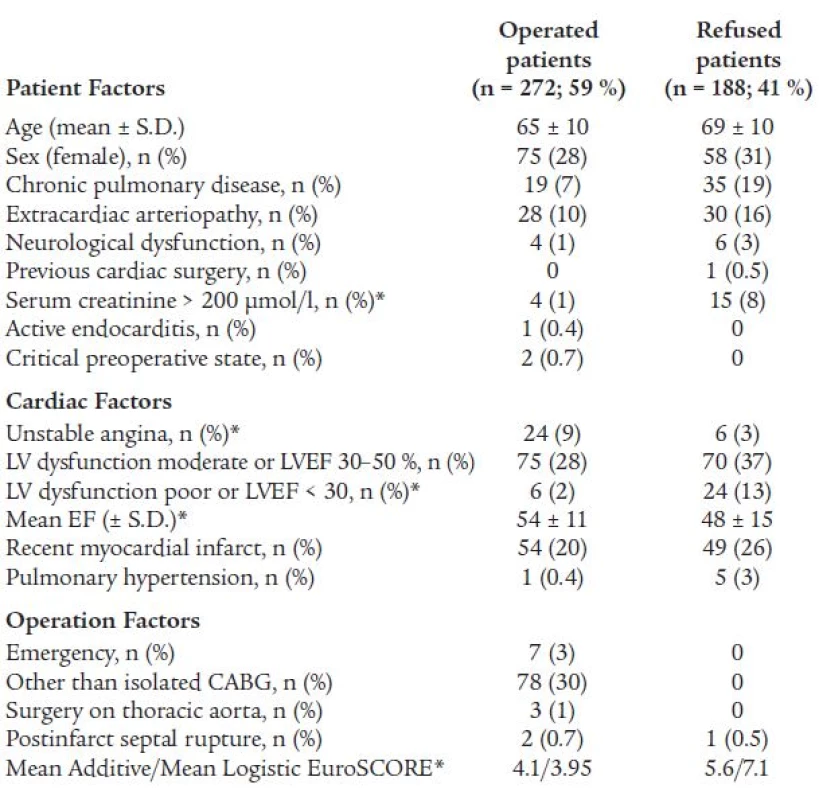
*p < 0.001, S.D. – Standard Deviation Finally, 259 patients (57 %) were operated and 199 patients (43 %) were refused for cardiac surgery (125 patients – 63 % – were treated conservatively and 74 patients – 37 % – were treated by percutaneous coronary intervention – PCI). One hundred eighty patients (69 %) underwent coronary artery bypass surgeries, 54 patients (21 %) underwent valve operations, 3 patients (1 %) underwent thoracic aorta surgery and 22 patients (9 %) underwent combined surgeries. Sixty-one patients (82 %) treated by PCI received at least one stent, the mean number of implanted stents was 1.3 ± 0.5. The implantation failed in 4 patients (5 %) and dissection of the coronary vessel was performed in one patient (1 %). Two patients (3 %) had a nonfatal periprocedural myocardial infarction, None of the patients died during the first 24 hours after the PCI intervention. The patients treated conservatively received only medications.
Clinical outcome
The mean follow up was 36 ± 10 days. The overall observed mortality was 26 patients (6 %). Out of them, inhospital mortality was 17 patients (65 %), and overall observed mortality after discharge in or out of hospital was 9 patients (35 %).
Validation of EuroSCORE
There was no significant difference between the observed and predicted mortality neither the entire cohort nor in the subgroups. Mean Additive EuroSCORE in the entire cohort was 4.6, while the logistic EuroSCORE was 5 %. Of the 259 operated patients, there were 12 deaths or 5 %. Both the Additive EuroSCORE and the logistic Euro-SCORE predicted 10 deaths (4 %). The chi square test P value of the total number of observed versus expected deaths in the subgroup of operated patients was 0.663 in both cases (table 3). Among the 199 refused patients, we observed a mortality of 14 deaths (7 %). The additive Euro-SCORE predicted 10 deaths (5 %), while the logistic EuroSCORE predicted 13 deaths (7 %). The chi square test P value of the total number of observed versus expected deaths was 0.400 and 0.842 respectively (table 3). The deceased patients had a statistically higher additive and logistic EuroSCORE than the survivors in the surgical subgroup (p < 0.001), as well as the survivors in the subgroup of the refused patients (p < 0.05).
Tab. 3. Predicted vs. observed mortality in the entire cohort, in operated and refused patients. 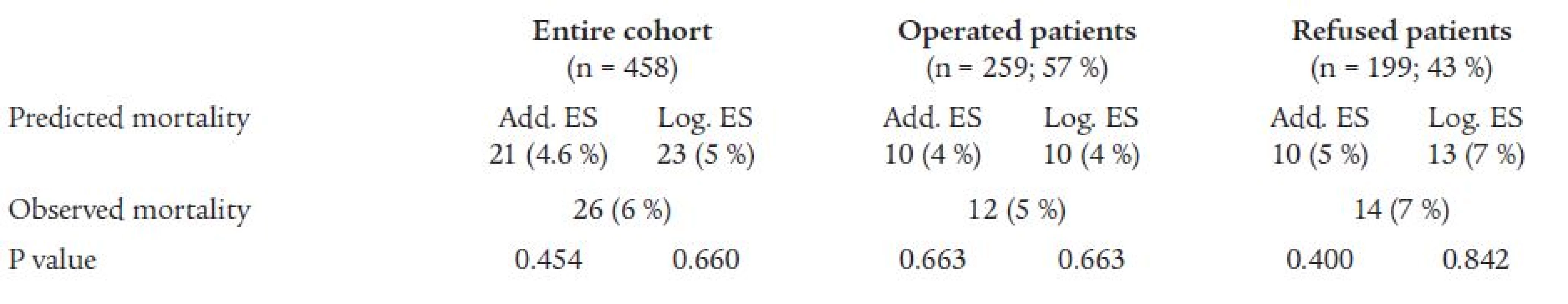
Add. – Additive, ES – EuroSCORE, Log. – Logistic. The patients with additive Euro-SCORE > 5 had a significantly worse prognosis than patients with EuroSCORE ≤ 5 in both subgroups (fig. 1).
Figure 1. Mortality according to the EuroSCORE level in both subgroups. 
Open bars – patients with EuroSCORE ≤ 5, closed bars – patients with EuroSCORE > 5. *p < 0.01, **p < 0.05 Discriminatory ability – C statistic
EuroSCORE showed good discriminatory ability in predicting shortterm mortality.
Fig. 2 and Fig. 3 show the areas under the receiver operating characteristic curves for both the standard and the logistic EuroSCORE in both subgroups of patients.
Figure 2. Receiver operating characteristic curves for short-term mortality after cardiac surgery. 
Figure 2a. Additive EuroSCORE: area 0.755 (0.659–0.850) Figure 2b. Logistic EuroSCORE: area 0.762 (0.668–0.857) Figure 3. Receiver operating characteristic curves for short-term mortality in the refused patients. 
Figure 3a. Additive EuroSCORE: area 0.695 (0.562–0.828) Figure 3b. Logistic EuroSCORE: area 0.716 (0.590-0.842) Discussion
This prospective study was designed to estimate the performance of both forms of the risk stratification system EuroSCORE in adult Czech cardiac population referred to the cardiac surgeon as cardiac surgery candidates. It was shown that both forms of the EuroSCORE correlate with the mortality in both subgroups of patients, i.e. those undergoing cardiac surgery as well as those denied for it. Studies performed in different cardio surgery centers in Europe, North America, Japan defined the EuroSCORE as an accurate risk prediction model of mortality. However, the validity of this model in Australian and Lithuanian population undergoing cardiac surgery was not confirmed, overestimating the mortality, especially when using the logistic model [6,12-16]. Our single center estimation of the validity of both forms of EuroSCORE in Czech adult cardiac population confirmed that EuroSCORE has a good discriminatory ability in predicting short-term mortality in cardiac surgical as well as in cardiac non-surgical patients. Most risk stratification models in cardiac surgery use early mortality as an end-point. The EuroSCORE identifies a number of risk factors, which help to predict short or longterm mortality (in percent), morbidity and length of intensive care unit stay after cardiac surgery [17-21]. The present study tests the discriminatory ability of both forms of EuroSCORE in predicting short-term mortality. As previously demonstrated, both forms, standard and logistic EuroSCORE, can be considered as applicable models (C statistic 0.755 vs. 0.762 for the surgery subgroup and 0.695 vs. 0.716 for the refused subgroup). Other published studies have shown C statistic values from 0.73 to 0.84 for standard EuroSCORE in CABG treated patients [18,22–24]. Different studies have demonstrated that EuroSCORE can be applied as a suitable predictor of mortality after cardiac, as well as thoracic aortic surgery and redo operations [25,26]. In this study we included patients that underwent coronary bypass surgery, valve surgery, thoracic aortic surgery and a combination thereof. No redo operation has been done. Overall EuroSCORE was proven to be a valid risk predictor of short-term mortality.
As many studies have shown the logistic EuroSCORE is a more accurate risk predictor of mortality in high-risk patients than the additive EuroSCORE, while for less risky patients it overestimates the risk. Our study confirmed almost the same validity of both forms. Our primary focus, though, was not on the differences between the two EuroSCORE forms; rather it was on their applicability on each of the subgroups.
Conclusions
The EuroSCORE has demonstrated good discriminatory ability in predicting early mortality after cardiac surgery as well as in patients refused to it. Both forms of EuroSCORE risk prediction model are suitable predictors of mortality in cardiac patients. However, in order to achieve excellent predictive capabilities, the existing model might need to be modified.
Acknowledgements
This paper was supported by the research project number: MSM 0021620817.
Milka Klinčeva, M.D.
www.fnkv.cz
e-mail: mklinceva@yahoo.com
Doručeno do redakce: 8. 6. 2006
Přijato po recenzi: 17. 8. 2006
Zdroje
1. Parsonnet V, Dean D, Bernstein AD. A method of uniform stratification of risk for evaluating the results of surgery in acquired adult heart disease. Circulation 1990; 82 : 1078.
2. Higgins TL, Estafanous FG, Loop FD et al. Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity score. JAMA 1992; 267 : 2344–2348.
3. Roques F, Gabrielle F, Michel P et al. Quality of care in adult heart surgery: proposal for a self-assessment approach based on a French multicenter study. Eur J Cardiothorac Surg 1995; 9 : 433–439
4. Tu JV, Jaglal SB, Naylor CD. Multicenter validation of a risk index for mortality, intensive care unit stay, and overall hospital length of stay after cardiac surgery. Steering Committee of the Provincial Adult Cardiac Care Network of Ontario. Circulation 1995; 91 : 677–684.
5. Pons JM, Granados A, Espinas JA et al. Assessing open heart surgery mortality in Catalonia (Spain) through a predictive risk model. Eur J Cardiothorac Surg 1997;11 : 415–423.
6. Kawachi Y, Nakashima A, Toshima Y et al. Risk stratification analysis of operative mortality in heart and thoracic aorta surgery: comparison between Parsonnet and EuroSCORE additive model. Eur J Cardiothor Surg 2001; 20 : 961–966.
7. Geissler H, Hölzl P, Marohl S et al. Risk stratification in heart surgery: comparison of six score systems. Eur J Cardiothor Surg 2000; 17 : 400–406.
8. Nashef SA, Roques F, Michel P et al. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg 1999; 16 : 9–13.
9. Roques F, Nashef SA, Michel P et al. Risk Factors and outcome in European cardiac surgery analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothor Surg 1999; 15 : 816–822.
10. Michel P, Roques F, Nashef SA. Euro - SCORE Project Group. Logistic or additive EuroSCORE for high-risk patients? Eur J Cardiothorac Surg 2003; 23 : 684–687.
11. Jin R, Grunkemeier GL. Providence Heath System Cardiovascular Study Group. Additive vs. Logistic risk models for cardiac surgery mortality. Eur J Cardiothorac Surg 2005; 28 : 240–243.
12. Roques F, Nashef SA, Michel P et al. The EuroSCORE Study Group. Does EuroSCORE work in individual countries? Eur J Cardiothor Surg 2000; 18 : 27–30.
13. Nashef SA, Roques F, Michel P et al. Coronary surgery in Europe: comparison of the national subsets of the European system for cardiac operative risk evaluation database. Eur J Cardiothor Surg 2000; 17 : 396–399.
14. Nashef SA, Roques F, Hammill BG et al. Validation of European system for cardiac operative risk evaluation (EuroSCORE) in North American cardiac surgery. Eur J Cardiothor Surg 2002; 22 : 101–105.
15. Vanagas G, Kinduris S. Assessing the validity of cardiac surgery risk stratification systems for CABG patients in a single center. Med Sci Monit 2005; 11: CR215–CR218.
16. Vanagas G, Kinduris S, Buivydaite K. Assessment of validity for EuroSCORE risk stratification system. Scand Cardiovasc J 2005; 39 : 67–70.
17. Toumpoulis IK, Anagnostopoulos CE, DeRose JJ et al. European system for cardiac operative risk evaluation predicts long-term survival in patients with coronary artery bypass grafting. Eur J Cardiothorac Surg 2004; 25 : 51–58.
18. Toumpoulis IK, Anagnostopoulos CE, DeRose JJ et al. Does EuroSCORE predict length of stay and specific postoperative complications after coronary artery bypass grafting? Int J Cardiol 2005; 105 : 19–25.
19. Toumpoulis IK, Anagnostopoulos CE, Toumpoulis SK et al. EuroSCORE predicts long-term mortality after heart valve surgery. Ann Thorac Surg 2005; 79 : 1902–1908.
20. Toumpoulis IK, Anagnostopoulos CE, DeRose JJ et al. European system for cardiac operative risk evaluation predicts long-term survival in patients with coronary artery bypass grafting. Eur J Cardiothorac Surg 2004; 25 : 51–58.
21. Nilsson J, Algotsson L, Hoglund P et al. EuroSCORE predicts intensive care unit stay and costs of open heart surgery. Ann Thorac Surg. 2004; 78 : 1528–1534.
22. Sergeant P, de Worm E, Meyns B. Single centre, single domain validation of the EuroSCORE on a consecutive sample of primary and repeat CABG. Eur J Cardiothorac Surg 2001; 20 : 1176–1182.
23. Karthik S, Srinivasan AK, Grayson AD et al. Limitations of additive Euro - SCORE for measuring risk stratified mortality in combined coronary and valve surgery. Eur J Cardiothorac Surg 2004; 26 : 318–322.
24. Zingone B, Pappalardo A, Dreas L. Logistic versus additive EuroSCORE. A comparative assessment of the two models in an independent population sample. Eur J Cardiothorac Surg 2004; 26 : 1134–1140.
25. Roques F, Nashef SA, Michel P. The EuroSCORE study group. Risk factors for early mortality after valve surgery in Europe in the 1990s: lessons from the EuroSCORE pilot program. J Heart Valve Dis 2001; 10 : 572–577.
26. Goodwin A, Ooi A, Kitcat J et al. Outcomes in emergency redo cardiac surgery: cost, benefit and risk assessment. Interact Cardiovasc Thoracic Surg 2003; 2 : 227–230.
Štítky
Diabetologie Endokrinologie Interní lékařství
Článek vyšel v časopiseVnitřní lékařství
Nejčtenější tento týden
2006 Číslo 12- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Pregabalin je účinné léčivo s příznivým bezpečnostním profilem pro pacienty s neuropatickou bolestí
-
Všechny články tohoto čísla
- Několik slov ke XIII. sjezdu České internistické společnosti
- Aktuální přístupy k diagnostice a terapii hemoptýzy: editorial
- Alogenní transplantace krvetvorných buněk u nemocných s chronickou myeloidní leukemií: editorial
- Prognostické markery u CLL - „watch and wait“ i transplantace: editorial
- Ultrasound mapping of lower-limb vascular system with regard to occurrence and anatomy of additional front great saphenous vein
- Prospective use of EuroSCORE for the short−term risk evaluation of consecutive cardiac surgery candidates: are there any differences in prediction of perioperative risk versus risk of nonsurgical treatments?
- Postavení embolizace bronchiální tepny v terapii klinicky významné hemoptýzy
- Allogeneic hematopoietic stem cell transplantation in patients with chronic myeloid leukemia in the Czech Republic - a retrospective analysis of results in years 1988–2005
- The electrocardiogram in acute myocardial infarction with reperfusion: current concepts regarding Q waves and their dynamics
- Nearytmická terapie komorových tachyarytmií a náhlá srdeční smrt po akutním infarktu myokardu
- Statins and osteoporosis
- ZAP-70 in B-cell chronic lymphocytic leukemia: clinical significance and methods of detection
- Collagenofibrotic glomerulopathy – rare glomerulonephritis
- Z odborné literatury
- X. kongres o ateroskleróze Špindlerův Mlýn, 7.-9. prosinec 2006
- Vnitřní lékařství
- Archiv čísel
- Aktuální číslo
- Pouze online
- Informace o časopisu
Nejčtenější v tomto čísle- Aktuální přístupy k diagnostice a terapii hemoptýzy: editorial
- Postavení embolizace bronchiální tepny v terapii klinicky významné hemoptýzy
- Statins and osteoporosis
- Ultrasound mapping of lower-limb vascular system with regard to occurrence and anatomy of additional front great saphenous vein
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




