-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Nailing osteosynthesis of proximal humeral fractures
Authors: Jan Polášek 1; Radek Veselý 2; Radim Suchomel 2
Authors place of work: Nemocnice Ivančice 1; Úrazová nemocnice v Brně, Klinika traumatologie LF MU Brno 2
Published in the journal: Úraz chir. 27., 2020, č.1
Summary
Introduction: One of the surgical methods to manage proximal humeral fractures is the nailing osteosynthesis, which reports good results for certain spectre of fractures. At the Trauma Hospital in Brno is has therefore become the method of choice for type A fractures and a part of type B fractures according to the AO.
Objective: The objective of our work was to evaluate clinical results of osteosynthesis of proximal humeral fractures managed by nailing osteosynthesis.
Method: 95 patients operated for proximal humeral fracture by antegrade nailing at the Trauma Hospital in Brno in 2014-2018 were enrolled in the retrospective study. Healing time, resulting mobility range, and number of complications were evaluated.
Results: The nailing osteosynthesis was used in 34 % of all 391patients operated due to proximal humeral fracture. The average age was 61 years. 95 patients were included in the study. Complete extraction of metal was performed in 7 patients and partial extraction was performed in 7 patients. Pseudoarthrosis formed in 2 patients; necrosis of the head occurred in 4 patients. No significant differences in results were found in two most frequently used nails.
Conclusion: Nailing osteosynthesis of proximal humeral fractures is a reliable method for the indicated fractures, with results comparable to those of plating osteosynthesis, particularly in respect of type AO A2 and B fractures.
Keywords:
complications – nail – Proximal humeral fracture – necrosis of the head – pseudoarthrosis (false joint)
INTRODUCTION
Proximal humeral fractures represent almost 6 % of all fractures [5]. 80 % of the patients are older than 50 and women are represented in more than 70 %; osteoporosis plays and important role [24]. The injury mechanism is mostly a normal low-energy fall, while the type of fracture usually depends on the position of the limb in respect of the body at the moment of the injury.
Diagnostics primarily rely on x-ray examination in two projections. However, accurate classification of multifragmental fractures using the x-ray is considerably complex and unreliable; CT examination is therefore frequently added.
Codmann/Neer classification is the oldest and very often used classification [10]; it is based on the most frequent four fragments copying anatomic bodies (greater tuberosity, lesser tuberosity, head, and diaphysis) and their mutual position is evaluated with only a fragment with dislocation greater than 1 cm or over 45° being defined as a separate fragment.
This classification serves as a basis for the extended AO/OTA classification used in our work [18], which subdivides the three basic types into additional subgroups according to dislocation and impact. The most robust classification is the “LEGO” classification subdividing the fractures into 12 basic groups according to the type of head comminution [22]. Predictors for the risk of head ischemia were defined based on this classification; however, some studies did not subsequently prove them [2].
Due to heterogeneity of the proximal humeral fractures there is no gold standard for the therapy. Conservative therapy has its place in slightly dislocated fractures and in patients with lower demands. In the overwhelming majority they are fixations by a modification of the Desaultʼs bandage, at present primarily in a form of orthoses. Abduction plates and hanging case and semi-conservation technique of closed reposition in anesthesia under sciascopic control are rather minority techniques.
Surgical therapy is generally indicated for dislocation of tubercles over 5 mm, varicous dislocation of the head exceeding 20°, valgous dislocation of the head exceeding 40°, while the indication is significantly individual with regard to various requirements, skeletal condition and general condition of the patients. Preserving operating techniques used at present include the cannulated screw osteosynthesis, K-wire transfixation, plating osteosynthesis in a form of anatomic LCP plates – nowadays the most frequently used method, and osteosynthesis using the intra-marrow nails, which our work deals with. As to the shoulder joint replacements, there is the head hemiarthroplasty and total endoprosthesis, which in its reverse variant manifests the best functional results of all the replacements.
METHODOLOGY
The goal of the work is to evaluate the success rate - results of nailing osteosynthesis in a retrospectively evaluated set of patients.
Patients operated for proximal humeral fracture by antegrade nailing at the Trauma Hospital in Brno in 2014-2018 were enrolled in the retrospective study. Data were obtained from the hospital system according to the corresponding MKN classification and according to the type of surgical procedure. A surgical procedure at a different site and pathological fracture were the exclusion criteria. Patients who were not monitored until healed or at least for 12 months from the injury were also excluded from the study.
During the specified period, a total of 391 patients diagnosed with a proximal humeral fracture were operated at the Trauma Hospital in Brno, with distribution of implants as follows (see Figure 1).
Fig. 1. Proportions of all types of surgical solution of the proximal humerus 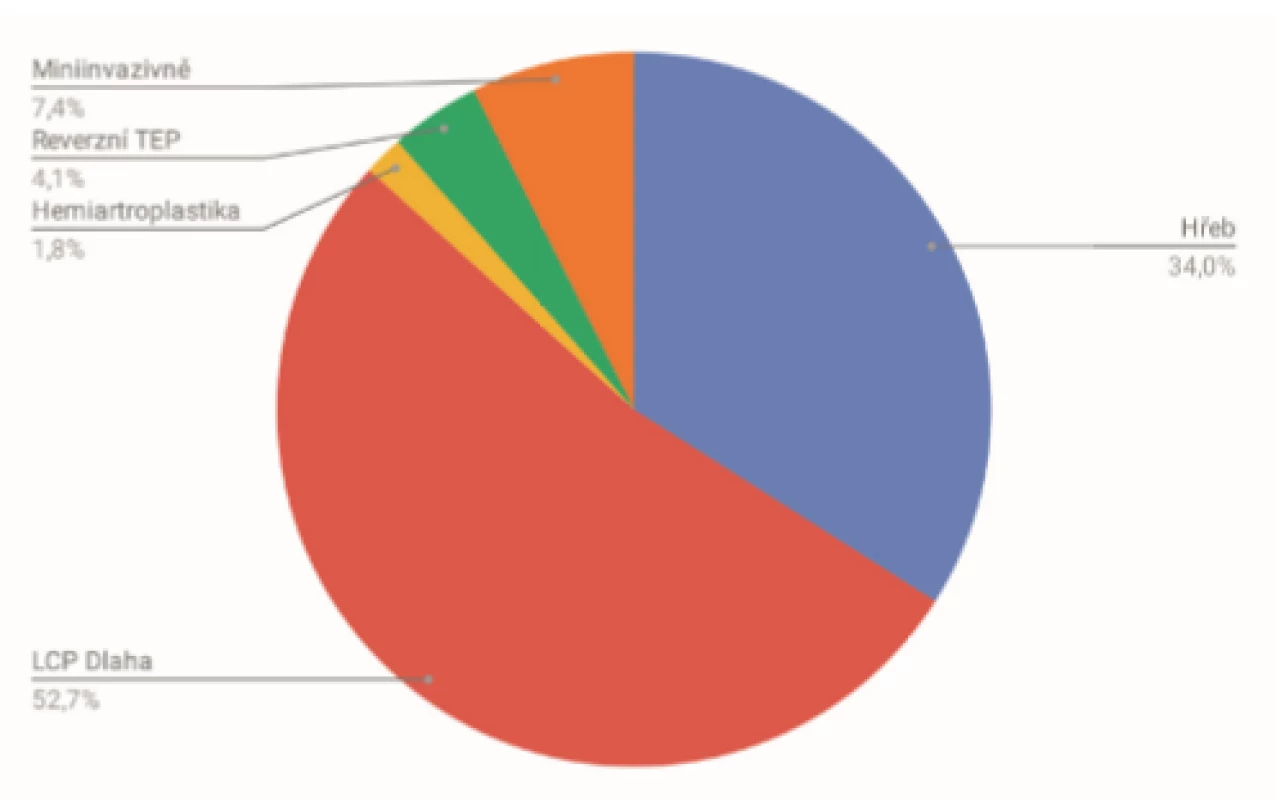
Findings from outpatient follow-up visits were evaluated in the hospital system including x-rays at week 3, 12, 24 and 48, or the last follow-up visit, if appropriate. The above-mentioned visit scheme was adjusted due to decision of the operating surgeon in approx. 20 %. X-ray signs of healing were evaluated, i.e. the presence of a callus on at least three cortical bones in both anteroposterior and lateral projection. The expected healing period of 4-9 months was taken as a basis.
We also focused on the condition of the humeral head and its resorption, if appropriate, and potential migration of the OS material, which required its extraction, whether complete or partial, and the eventual subsequent reoperations.
The AO classification was used to categorize the fractures [18]. To evaluate the type of fracture, we used the available x-ray or CT documentation, as appropriate, which for B1.2 and C fractures is supplied as a routine. We also evaluate the interval between the primary procedure and date of injury and the length of hospitalisation.
In post-operation period, the presence of post-operation infection, healing period according to x-ray, and mobility at the last follow-up visit were evaluated.
Those proximal humeral fractures were indicated for the antegrade nailing osteosythesis, where close repositioning successfully restored the proper position of the head fragments.
Nails from four various manufacturers were used for the nailing osteosynthesis – dominantly (91.6 %) two types of straight nails, the remaining nails were angular. The type of nail was chosen by the operating surgeon depending on the type of fracture – the straight type was chosen more frequently with regard to better bone strength in the osteoporotic skeleton in the area of the humeral head apex, which is higher than the one in the area of the greater tuberosity where the entrypoint of angular nails is located. This was also the one to interfere more frequently with the fracture area in B1 type fractures. They were most frequently inserted in the beach chair position from the anterolateral access via m. supraspinatus, which was subsequently reconstructed at the end of the surgery. Both the proximal and distal locking was performed via a targeting device, when proximally it was locked with at least two screws and distally with one or two screws.
Rehabilitation was initiated individually depending on the character of the fracture with the possibility for the patient to perform passive exercises with the limb in hanging position one day after the surgery or at the first outpatient post-operation follow-up visit. Active mobilisation was commenced upon the first x-ray signs of healing. Extraction of the material was planned in case of its migration, failure or suspected contribution to impingement only.
RESULTS
A total of 133 patients with proximal humeral fracture were treated in the given period at the Trauma Hospital in Brno, which is 34 % of all the 391 patients operated with proximal humeral fracture (Figure 1).
95 patients were enrolled to the resulting set, in this a total of 63 women and 32 men with the average age of 61.1 years (men 58.6, women 62.2); for age distribution see Figure 2.
Fig. 2. Age distribution with the men/women proportion in the set 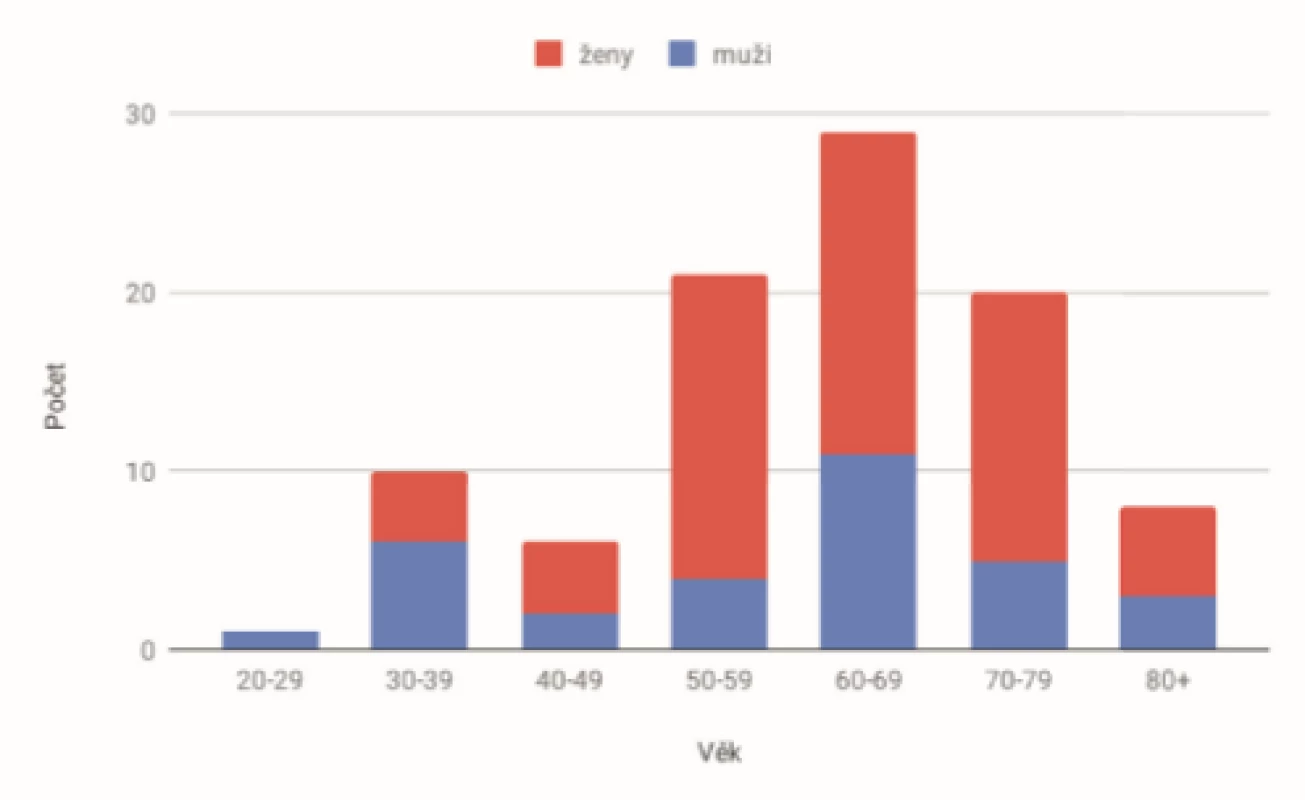
In the total of 133 operated patients, two were excluded from the set due to a false joint operation; in one case it was a re-osteosynthesis from other site. The remaining 35 patients did not return for all the necessary enrolment checks, while only five were assumed to be monitored at their (remote) residence.
Within the AO classification, type B (62) fractures prevailed over type A (28) and C (5). Fractures were classified using the x-ray and CT images (Figure 3).
Fig. 3. Representation of fracture types according to AO 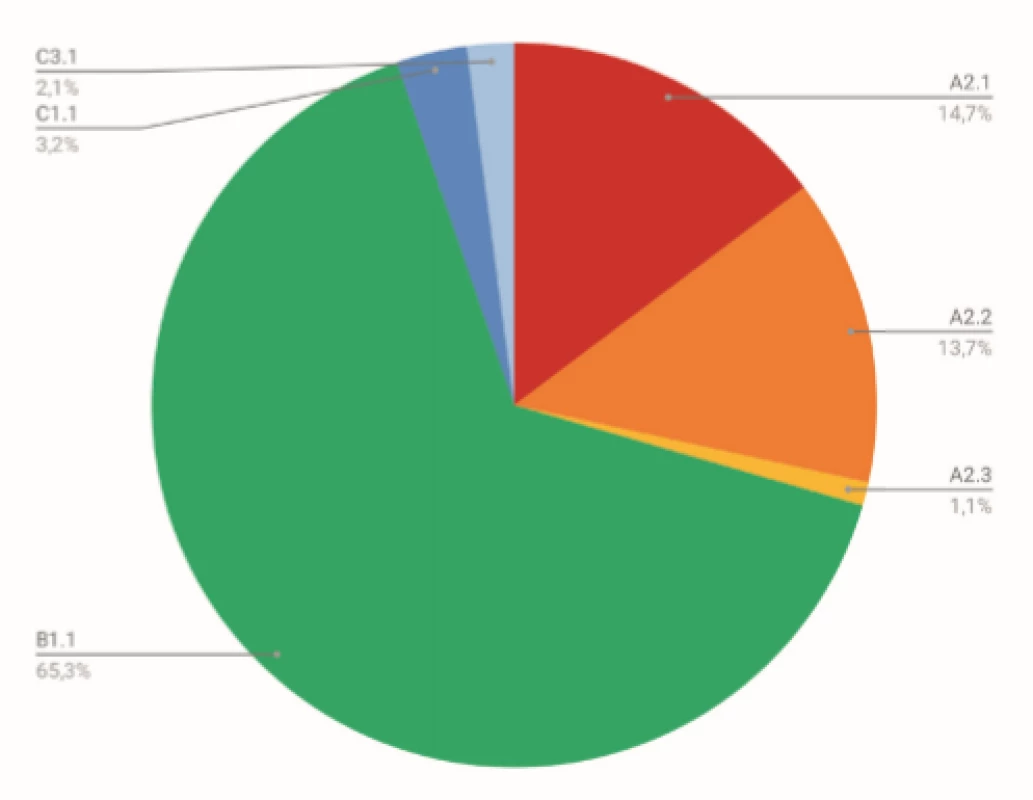
Extraction of at least a part of the osteosynthetic material was performed in a total of 14 patients, out of which 7 patients had a partial extraction (prominent screws in the head in the event of proximal locking) and 7 patients had a complete extraction.
Two patients developed a false joint in the area of the surgical humeral neck. Avascular head necrosis developed in 4 patients. Four patients were suggested an arthroscopic procedure with joint redress due to limited movement, but it took place only once for this indication (in the remaining cases the patients did not want another intervention); there were three redresses without arthroscopy in terms of extraction of proximal locking screws. See Table 1.
Tab. 1. Numbers of complications 
A reverse TEP was suggested to one patient due to head necrosis; however, the patient did not wish the procedure either.
No infection complications were reported in our set; out of neurological complications, paraesthesia in the innervation of n. radialis with complete spontaneous improvement during the treatment was reported in 2 cases; out of other complications, there were 3 cases of instability in the course of tendon of biceps long head, which in one case resulted in the extraction of OS material.
Nail A in our set has angle stable proximal locking screws and it has a proximal extension of its thickness, while nail B has the same thickness along the whole length of the nail and the proximal locking is resolved by conventional screws. The results are very similar except for relatively more frequent prominence of proximal screws for nail B (see Table 3).Healing on-x-ray was confirmed on x-ray in 22.3 weeks on the average, without significant difference between the age groups (see Table). The average scope of the resulting elevation of the operated limb was 138.9°; decline with older age was already manifested here (see Table 2 and Figure 4).
Fig. 4. Resulting elevation depending on age 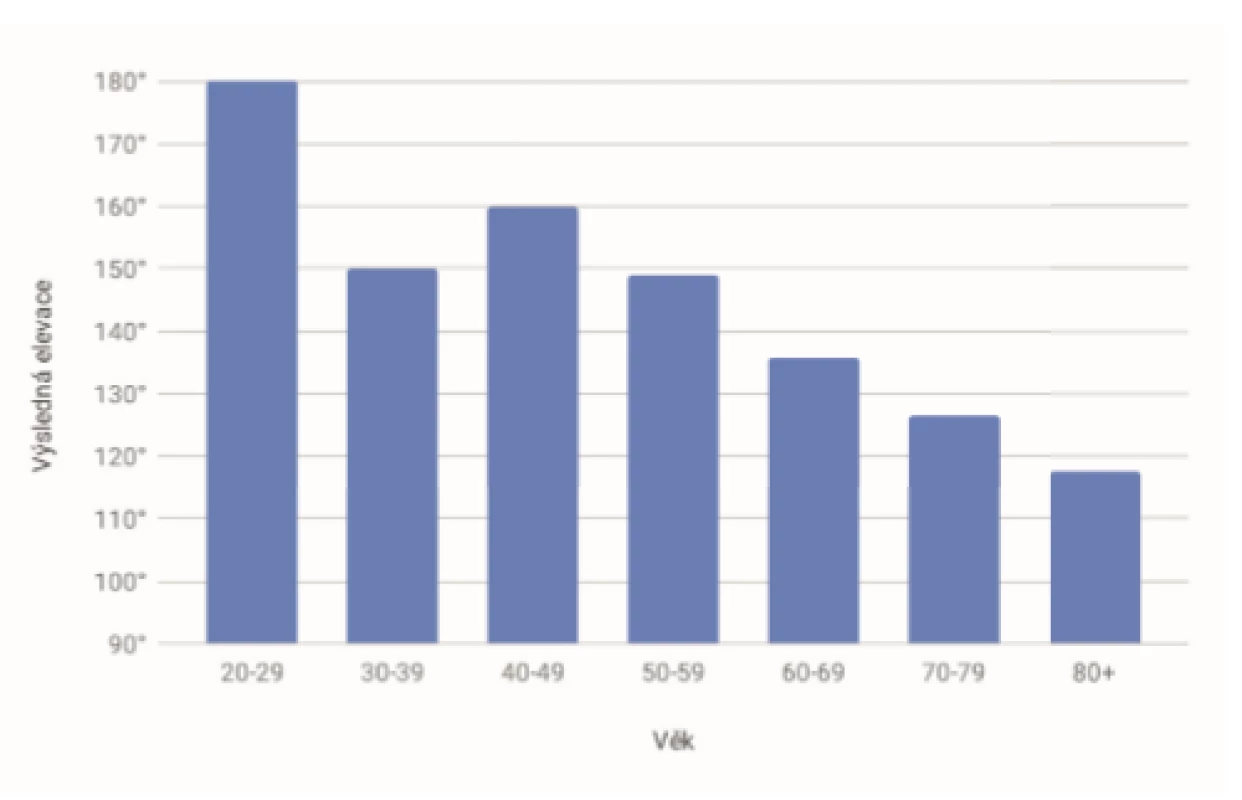
Tab. 2. Resulting elevation and x-ray healing period 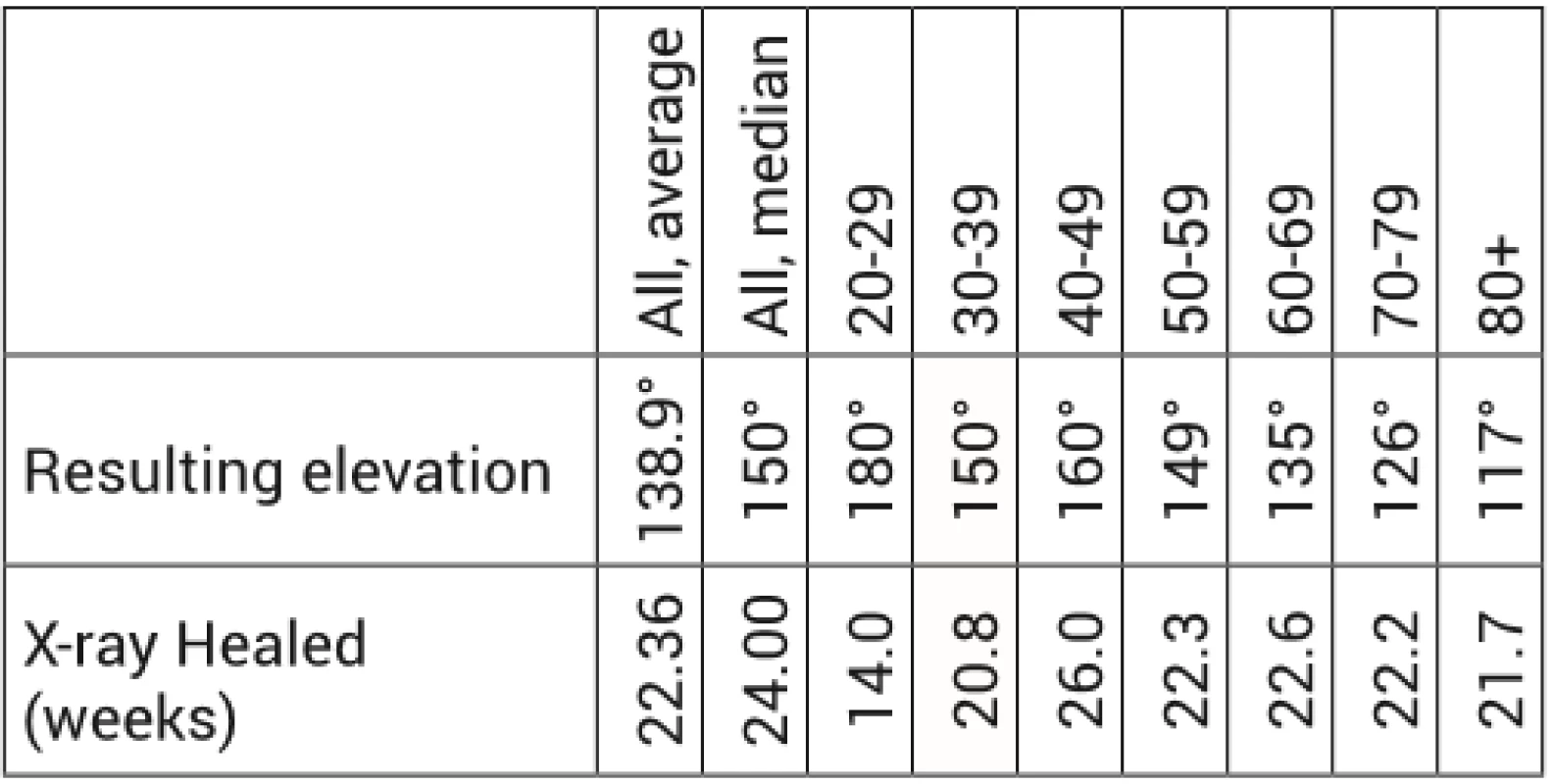
Tab. 3. Comparison of two most frequently used nails 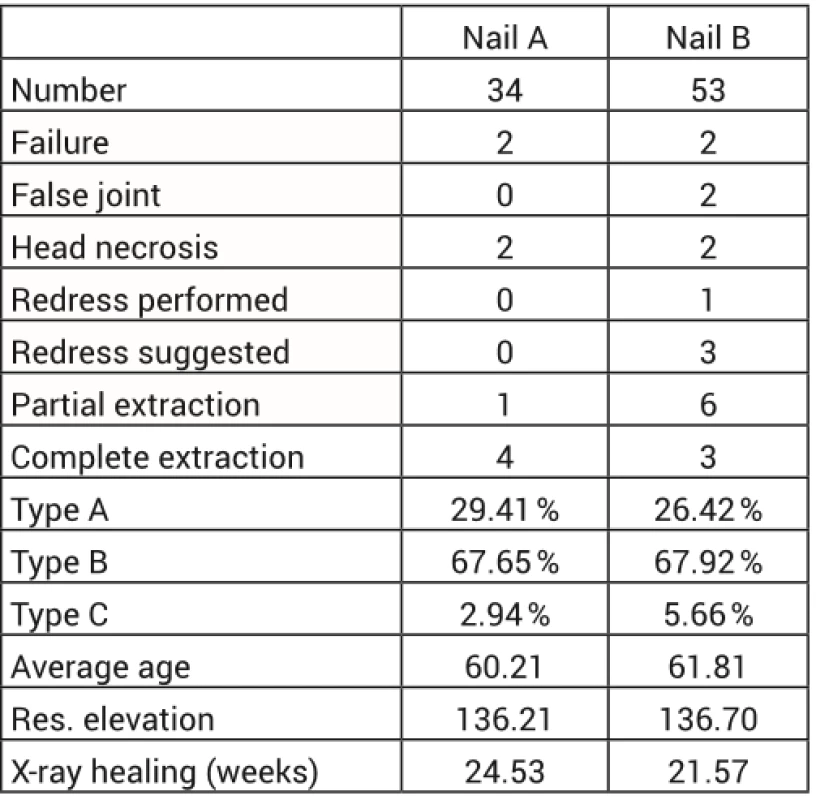
The average length of hospitalisation was 5.2 days (median of 5 days); the average interval of the surgical solution was 2.9 days, but with a 1-day median.
Fig. 5. Woman 58 years old, AO B1.1 fracture, fall due to tripping, operation on day 1 after the injury. X-ray healing in 14 weeks; redress + arthroscopy in 8 months, resulting elevation of 160° 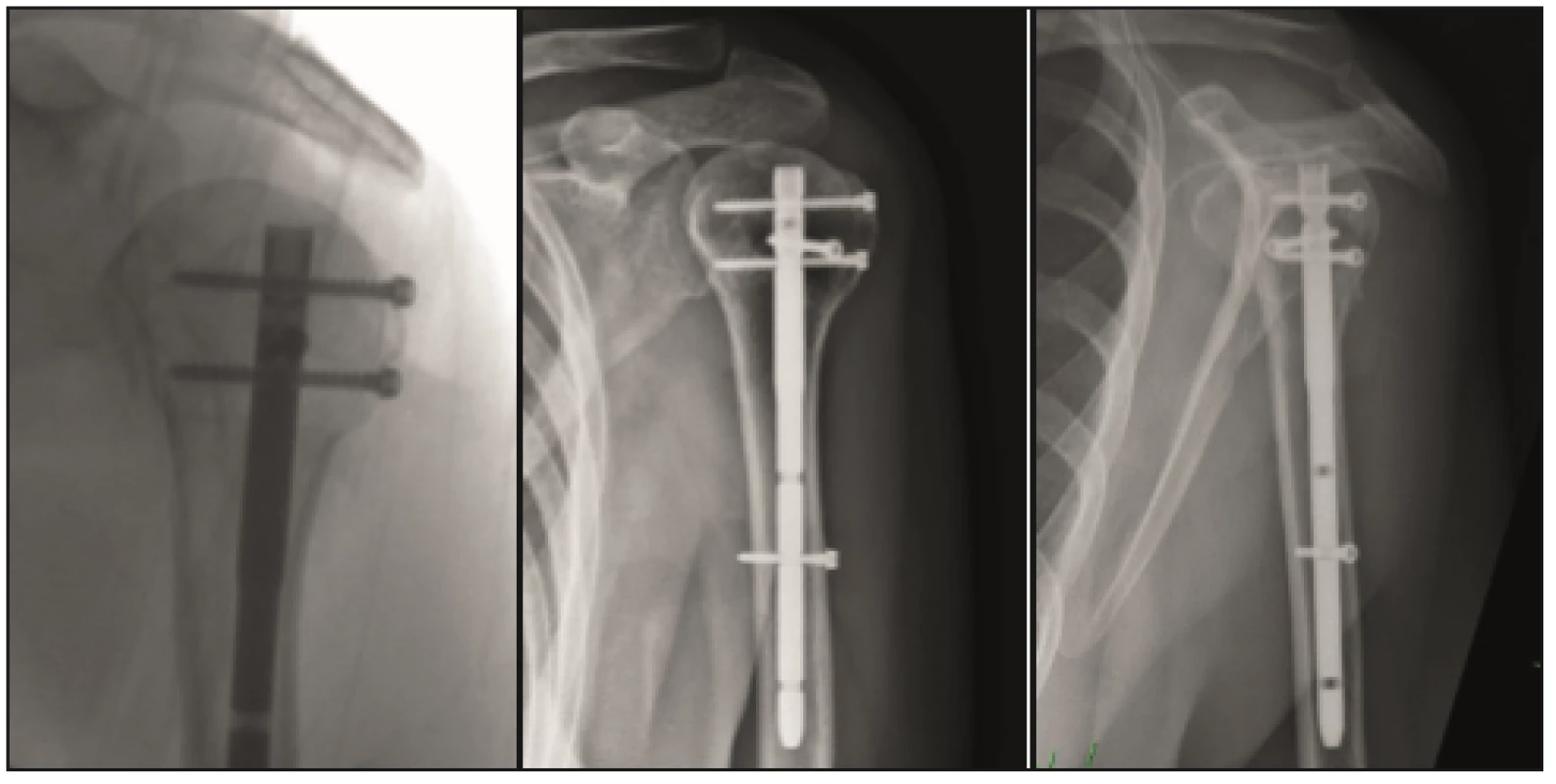
Fig. 6. Woman 76 years old, fall at home, AO C3.1 fracture, operation on day 6 from the injury (transferred from other site + warfarinization), x-ray healing in 24 weeks, resulting elevation of 160° 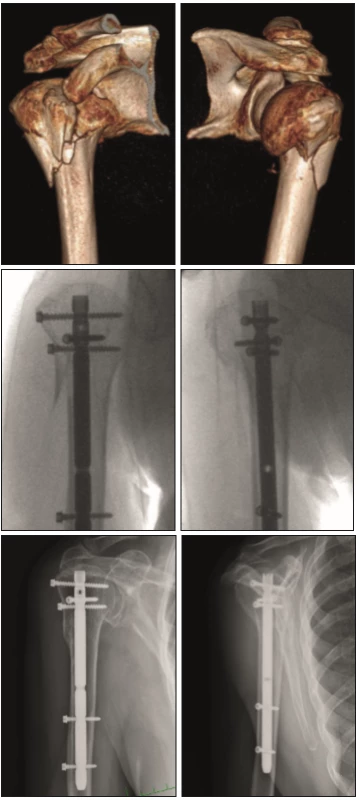
Fig. 7. Man 58 years old, fall in a quarrel, AO B1.1 fracture, operation on the day of injury, insufficient reposition of the head fragment, entrypoint laterally, incomplete reposition and poor retention of the main head fragment. Gradual head necrosis, extraction of the OS material after 3 years from the operation, elevation 90° 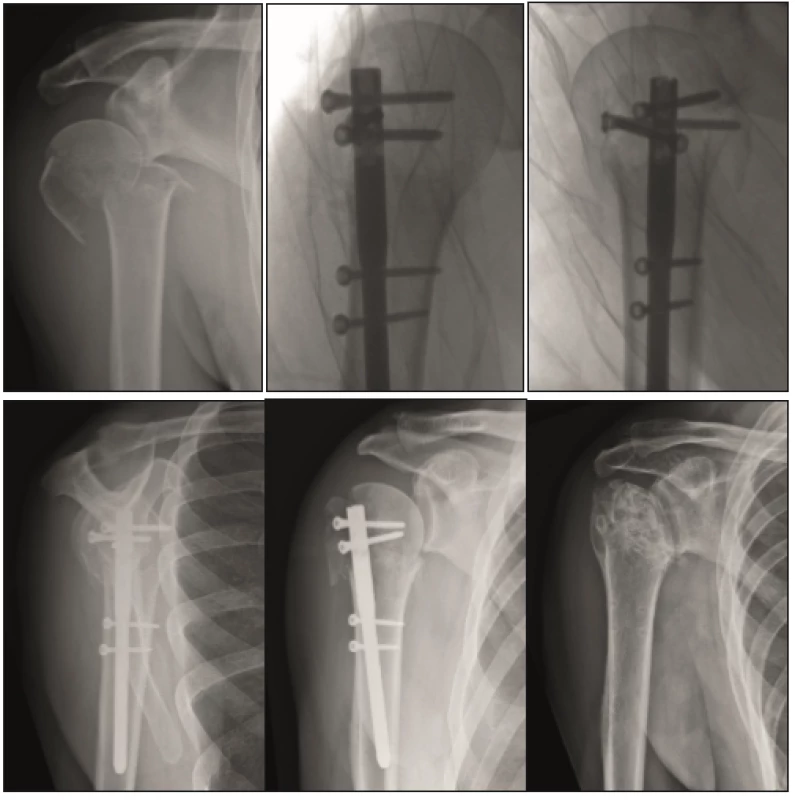
DISCUSSION
In spite of large amount of literature regarding the options of proximal humeral fracture therapy, this topic remain quite controversial.
With regard to frequency of the fractures there are numerous studies dealing with various types of therapy, but they most often have the character of cohort studies. There are very little phase I and II clinical studies. Therefore, evidence based recommendations for the therapy of these fractures are considerably limited. The last Cochrane [6] meta-analysis did not find any significant difference between the surgical and conservative therapy in patients with lower demands with dislocated three - to four-fragment fractures. Recent multi-centric prospective randomized study (PROFHER) [7] did not prove any statistically significant benefit of the surgical solution, but both the data collection and interpretation were disputed here [1]. The results of these meta studies initiated a discussion and prepared the space for additional higher-phase studies, this time ones for more selected subgroups as to age, patientʼs demands or type of fractures [9].
Nailing osteosynthesis is the trend of the recent years and its application in indicated fractures has been increasing in the recent years. As more advanced implants are introduced to the market, such as nails with angle stable locking, nail-in-nail, etc., the spectre of their application grows. With more sophisticate implants, however, the already long learning curve of proper use of the implant, which is already primarily longer than the one for the plating osteosynthesis, grows longer.
No significant differences in the results were found in the studies comparing the plates and nails [26]. Lower percent of post-operation complications as compared with plates in favour of nails was reported in some sets [3]. However, the sets evaluate mostly the A type fractures.
In our set, the nailing osteosynthesis was used in the monitored period in a total of 34 % of the operated patients; the angle stable plate osteosynthesis therefore remains dominant (52 %).
In the set of nailing osteosynthesis there are relatively lower number of type C fractures according to AO (A 30 %, B 65 %, C 5 %) as compared with the comparable sets (A 35.5 %, B 37.5 %, C 25 %) [15], which is given primarily by the site customary practice, where the plating osteosynthesis is preferred for multi-fragment fractures with intraarticular component [19].
Extraction of at least a part of material was performed in our set in a total of 14.7 %; if, however, we divided the set into 2-fragment (10.7 %) and 3 - to 4-fragment (16.4 %) fractures, these numbers would be lower than those in comparable studies (13 % and 30%, respectively) [8, 26]. Indications for extraction included the prominence of material into the joint, its contribution to impingement, or its release.
There is a higher average age – 61 years in our set as compared with the works evaluating the proximal humeral nailing, when compared with studies [12, 26] (55 and 57 years, respectively); nevertheless, a meta-study comprising older studies indicates the average age of 64.3 years [25].
Functional result is harder to evaluate based on the data from HIS because only elevation is reported by the operating surgeons across the board, which in result is 138.9° on the average, but with significant decline with the increasing age of the patient at the time of the operation - on the average 160° in the 4th decade declining evenly to 118° in the 8th decade (Figure 4). The results can be given into correlation with non-decreasing relative constant score [4] with the increasing age from other studies [13]. It is also in accordance with the literature, where the average elevation was 137.4° [25]. However, for a more relevant comparison it would be necessary to add an examination including the scoring systems (Constant score, DASH, VAS score), which unfortunately are not available.
In the event of persisting limited mobility with signs of subacromial impingement, which was not explained by potential prominence of material, patients were offered the arthroscopy with a joint redress, which however was accepted by relatively small percent of patients (25%) only. However, a recent study show a significant potential for improvement in both mobility and reduction of eventual pains (abduction improvement by 37.6° according to the study) [17].
The healing time according to x-ray in our set was 22.3 weeks on the average which is longer than in the comparable sets (e.g. 8.4 weeks) [13]. The amplitude of the difference is given particularly by different time interval of the follow-up visits – follow-up visits in our set were most frequently after 12 weeks, where there were signs of healing, but the image in most cases did not meet the definition of healing yet, and in month 6, where the healing was already completed.
Although there are relatively less type C fractures in our set (a total of 5), the complication level is considerable here – head necrosis occurred in 3 cases (60 %), which is more than reported in available literature, where it is most often reported to be up to 30 % [3, 12, 20]; the number of complications rather appears to correlate with the result of study [14], where there is 60 % of head necroses in four-fragment fractures managed by nails with incorrect reposition according to x-ray.
In spite of non-negligible amount of complications and the risk of head necrosis, four-fragment fractures of active patients aged under 70 are at present indicated at the Trauma Hospital in Brno for osteosynthesis, but the plating one. In older patients, these fractures are indicated only exceptionally and [11, 16] he conservative procedure or reverse endoprosthesis is preferred, if appropriate. Hemiarthroplasty has been gradually abandoned. Our set shows that the risk of head necrosis is low in type A and B fractures, and therefore osteosynthesis is always indicated in the event of a surgical solution.
As mentioned before, with regard to complexity of the issue there is still no universally recommended procedure of solving the proximal humeral fracture. The authors of the publication [23] suggested a comprehensive algorithm, the application of which has already been published in the first study [21]. Interestingly, this algorithm does not include the nailing osteosynthesis at all.
CONCLUSION
Nailing osteosynthesis of proximal humeral fractures is a reliable method for the indicated fractures, with good functional results comparable to those of plating osteosynthesis. Our results confirm suitability of this method in all age groups of patients, particularly for type AO/OTA A2 and B fractures where there is a minimal risk of head necrosis and low risk of the need of another operation. In type C fractures, with the overcoming of the long learning curve and under the precondition of the use of advance implants, there is also an option of using the nailing osteosynthesis, with pre-operation planning and qualify of reposition playing an important role here.
doc. MUDr. Radek Veselý, Ph.D.
email: r.vesely@unbr.cz
Zdroje
1. ANTONIOS, T., BAKTI, N. NZEAKO, O. et al. Outcomes following fixation for proximal humeral fractures. Journal of Clinical Orthopaedics and Trauma [online]. 2019, 10, 3, s. 468–473. ISSN 09765662. Dostupné z: doi:10.1016/j.jcot.2019.01.029
2. BASTIAN, JD, HERTEL, R. Osteosynthesis and hemiarthroplasty of fractures of the proximal humerus: Outcomes in a consecutive case series. Journal of Shoulder and Elbow Surgery [online]. 2009, 18, 2, 216–219. ISSN 10582746. Dostupné z: doi:10.1016/j.jse.2008.09.015
3. BOUDARD, G., POMARES, G., MILIN, L. et al. Locking plate fixation versus antegrade nailing of 3 - and 4-part proximal humerus fractures in patients without osteoporosis. Comparative retrospective study of 63 cases. Orthopaedics & Traumatology: Surgery & Research [online]. 2014, 100, 8, 917–924. ISSN 18770568. Dostupné z: doi:10.1016/j.otsr.2014.09.021
4. CONSTANT, CR., MURLEY, AH. A clinical method of functional assessment of the shoulder. Clinical Orthopaedics and Related Research. 1987, 214, 160–164. ISSN 0009-921X
5. COURT-BROWN, CM., CAESAR, B. Epidemiology of adult fractures: A review. Injury [online]. 2006, 37, 8, 691–697. ISSN 00201383. Dostupné z: doi:10.1016/j.injury.2006.04.130
6. HANDOLL, HH, BRORSON, S. Interventions for treating proximal humeral fractures in adults. Cochrane Database of Systematic Reviews [online]. 2015 [vid. 15. září 2019]. ISSN 14651858. Dostupné z: doi:10.1002/14651858.CD000434.pub4
7. HANDOLL, HH., KEDING, A., CORBACHO, B. et al. Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. The Bone & Joint Journal [online]. 2017, 99-B, 3, 383–392. ISSN 2049-4394, 2049-4408. Dostupné z: doi:10.1302/0301-620X.99B3.BJJ-2016-1028
8. HATZIDAKIS, AM, SHEVLIN, MJ, FENTON, DL et al. Angular-Stable Locked Intramedullary Nailing of Two-Part Surgical Neck Fractures of the Proximal Part of the Humerus: A Multicenter Retrospective Observational Study. The Journal of Bone and Joint Surgery-American Volume [online]. 2011, 93, 23, 2172–2179. ISSN 0021-9355. Dostupné z: doi:10.2106/JBJS.J.00754
9. HOWARD, L., BERDUSCO, R., MOMOLI, F. et al. Open reduction internal fixation vs non-operative management in proximal humerus fractures: a prospective, randomized controlled trial protocol. BMC Musculoskeletal Disorders [online]. 2018, 19, 1, 299. ISSN 1471-2474. Dostupné z: doi:10.1186/s12891-018-2223-3
10. CHARLES, S., NEER, I. Displaced proximal humeral fractures: Part II. Treatment of three-part and four-part displacement. JBJS. 1970, 52, 6, 1090–1103.
11. IYENGAR, JJ, DEVCIC, Z., SPROUL, RC. et al. Nonoperative Treatment of Proximal Humerus Fractures: A Systematic Review: Journal of Orthopaedic Trauma [online]. 2011, 25, 10, 612–617. ISSN 0890-5339. Dostupné z: doi:10.1097/BOT.0b013e3182008df8
12. KLOUB, M. Operační léčba zlomenin proximálního humeru úhlově stabilními hřeby – prospektivní studie. B.m., 2014. Praha : Univerzita Karlova, 2. lékařská fakulta.
13. KLOUB, M., HOLUB, K., KOPAČKA, P. et al. Dlouhodobé výsledky hřebování extraartikulárních zlomenin proximálního humeru. Acta Chir orthop Traum čech. 2013, 80, 203–207.
14. KLOUB, M., HOLUB, K., POLAKOVA, S. Nailing of three - and four-part fractures of the humeral head – Long-term results. Injury [online]. 2014, 45, S29–S37. ISSN 00201383. Dostupné z: doi:10.1016/j.injury.2013.10.038
15. KŘIVOHLÁVEK, M., LUKÁŠ, R., TALLER, S. et al. Použití úhlově stabilních implantátů při ošetření zlomenin proximálního humeru – prospektivní studie. Acta Chir orthop Traum čech. 2008, 75, 212–220.
16. LAUNONEN, AP, LEPOLA, V., FLINKKILÄ, T. et al. Treatment of proximal humerus fractures in the elderly: A systematic review of 409 patients. Acta Orthopaedica [online]. 2015, 86, 3, 280–285. ISSN 1745-3674, 1745-3682. Dostupné z: doi:10.3109/17453674.2014.999299
17. MAROUN, CH., ALIANI, D., HASS, A. et al. Shoulder arthroscopy combined to hardware removal in proximal humeral fractures: a series of 58 cases with a mean follow-up of 2 years. European Journal of Orthopaedic Surgery & Traumatology [online]. 2017, 27, 3, 317–321. ISSN 1633-8065, 1432-1068. Dostupné z: doi:10.1007/s00590-017-1938-4
18. MÜLLER, ME, NAZARIAN, S., KOCH, P. et al. The comprehensive classification of fractures of long bones. B.m.: Springer Science & Business Media, 2012. ISBN 3-642-61261-X.
19. PIKULA, R., IRA, D., KRTIČKA, M. et al. Chirurgické ošetření intraartikulárních zlomenin proximálního humeru. Úrazová chirurgie. 2013, 21, 3, 71–79. ISSN: 1211-7080.
20. PIKULA, R., IRA, D., KRTIČKA, M. et al. Osteonekróza hlavice humeru při operačním řešení intraartikulárních zlomenin proximálního humeru PHILOS dlahou. Úrazová chirurgie. 2013, 21, 3, 80–86. ISSN: 1211-7080.
21. SPROSS, C., MEESTER, J., MAZZUCCHELLI, RA. et al. Evidence-based algorithm to treat patients with proximal humerus fractures—a prospective study with early clinical and overall performance results. Journal of Shoulder and Elbow Surgery [online]. 2019, 28, 6, 1022–1032. ISSN 1058-2746. Dostupné z: doi:10.1016/j.jse.2019.02.015
22. SUKTHANKAR, AV, LEONELLO, DT, HERTEL, RW et al. A comprehensive classification of proximal humeral fractures: HGLS system. Journal of Shoulder and Elbow Surgery [online]. 2013, 22, 7, s. e1–e6. ISSN 10582746. Dostupné z: doi:10.1016/j.jse.2012.09.018
23. TRAIL, IA, FUNK, L., RANGAN, A. et al. Textbook of Shoulder Surgery [online]. Cham: Springer International Publishing, 2019 [vid. 15. září 2019]. ISBN 978-3-319-70098-4. Dostupné z: doi:10.1007/978-3-319-70099-1
24. WILSON, J., BONNER, TJ, HEAD, M et al. Variation in bone mineral density by anatomical site in patients with proximal humeral fractures. The Journal of Bone and Joint Surgery. British volume [online]. 2009, 91-B, 6, 772–775. ISSN 0301-620X, 2044-5377. Dostupné z: doi:10.1302/0301-620X.91B6.22346
25. WONG, J., NEWMAN, JM, GRUSON, KI. Outcomes of intramedullary nailing for acute proximal humerus fractures: a systematic review. Journal of Orthopaedics and Traumatology [online]. 2016, 17, 2, 113–122. ISSN 1590-9999. Dostupné z: doi:10.1007/s10195-015-0384-5
26. ZHU, Y., LU, Y., SHEN, J. et al. Locking Intramedullary Nails and Locking Plates in the Treatment of Two-Part Proximal Humeral Surgical Neck Fractures: A Prospective Randomized Trial with a Minimum of Three Years of Follow-up. The Journal of Bone and Joint Surgery-American Volume [online]. 2011, 93, 2, s. 159–168. ISSN 0021-9355. Dostupné z: doi:10.2106/JBJS.J.00155
Štítky
Chirurgie všeobecná Traumatologie Urgentní medicína
Článek vyšel v časopiseÚrazová chirurgie
Nejčtenější tento týden
2020 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Stillova choroba: vzácné a závažné systémové onemocnění
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Cinitaprid – v Česku nová účinná látka nejen pro léčbu dysmotilitní dyspepsie
-
Všechny články tohoto čísla
- Využití metody stabilní osteosyntézy u pacientů s mnohočetným myelomem a patologickou zlomeninou dlouhých kostí, retrospektivní zhodnocení použité terapie
- Hřebová osteosyntéza zlomenin proximálního humeru
- Léčba luxace akromioklavikulárního skloubení typu III dle Rockwooda
- Zlomenina dens axis u seniorů, náš terapeutický přístup
- Úrazová chirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Léčba luxace akromioklavikulárního skloubení typu III dle Rockwooda
- Hřebová osteosyntéza zlomenin proximálního humeru
- Zlomenina dens axis u seniorů, náš terapeutický přístup
- Využití metody stabilní osteosyntézy u pacientů s mnohočetným myelomem a patologickou zlomeninou dlouhých kostí, retrospektivní zhodnocení použité terapie
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




