-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Abdominal trauma and wandering spleen - case report
Authors: Milan Viskupič 1; Petr Krátký 2; Yanakis Lefa 3; Lepold Pleva 1
Authors place of work: Klinika úrazové chirurgie FN Ostrava Poruba 1; Chirurgické oddělení, Jesenická nemocnice, Jeseník 2; Radiologické oddělení, Jesenická nemocnice, Jeseník 3
Published in the journal: Úraz chir. 26., 2018, č.2
Category: Kazuistika
Summary
The authors refer to the case of an 18-year-old man with severe mental retardation and severe cerebral palsy with motor anxiety and tendency to self-harm who has stomped his abdomen at the edge of the bed. Both ultrasonic and CT findings are suspected to be tortuous and infarcted wandering spleen.
Keywords:
Wandering spleen
Introduction
Abdominal injury is still a source of significant morbidity and lethality in both blunt and penetrating injuries. Organ injury is caused by direct violence acting on the abdominal wall or indirectly by deceleration, especially when falling from height and in the involvement in car crashes. The diagnosis of these injuries leans against anamnestic data (basic information about the injury from the injured and his surroundings, including injury mechanism, time-to-injury data, time of starting to attend to the injured), and overall physical examination, including per rectum examination. Paraclinical examinations are dominated by MDCT with contrast medium administration, ultrasound examination of the abdominal cavity (FAST), laboratory examination [8]. Assuming hemodynamic stability of the injured but also in the case of injured with haemodynamic instability with continued volumic resuscitation suspected of intra-abdominal injury. Urgent laparotomy is indicated for haemodynamic instability and urgent development of severe shock or signs of peritoneal irritation.
The spleen is one of the most frequently injured intra-abdominal organs. It is located in the left subbranchial cavity to the left of the stomach, in the area called saccus lienalis, where it is fixed by lig. phrenicolienale, lig. pancreaticolienale, lig. gastrolienale [1]. Spleen injury should always be considered in patients with left chest and left upper abdominal quadrant trauma. The spleen is especially often injured in fractures of the seventh to ninth rib (Saegesser ribs). It is also necessary to think of the possibility of a two-stage rupture of the spleen, where severe bleeding occurs even several days after the injury, where the rupture of the subcapsular splenic hematoma is the source of bleeding. Wandering spleen is a rare anatomical anomaly of unknown etiology. It becomes clinically symptomatic only when the vascular stem is torsioned.
Case report
Man, 18 years old, with severe mental retardation, severe hypotonic form of cerebral palsy, with no genetic or metabolic defect detected, prone to self-harm, insomnia, motor unrest, difficult to control by medication. A history of single-stage spleen rupture was found 11 years ago, followed by conservative treatment, spleen ectopy was not described at that time.
He comes with her mother in a surgical clinic for two days of abdominal pain, TT 38.5°. C, with diarrheaous odorous stool. Mother says that 3–4 days ago he hit the bedside with his abdomen.
The patient was hospitalized, circulatory stable on admission, TT 38.4 °C. Hemoglobin 149 g/l, Lecocytes 16.5x10 9, CRP elevation 365 mmol/l in blood chemistry. An ultrasound examination of the abdominal cavity and the urinary tract was performed, showing free fluid in the abdominal cavity and ectopic distal spleen of heterogeneous echoarchitecture. Due to the unclear ultrasound finding, MDCT examination with contrast (Fig. 1) was added, where a migrating spleen 10x5.5x13 m in size, caudally in the left mesogastrium laterally from the colon descendens was found. Part of the spleen does not saturate and has low densities. The spleen stem is long wound, laterally paracolic.
Fig. 1. CT finding of migrating torsioned spleen 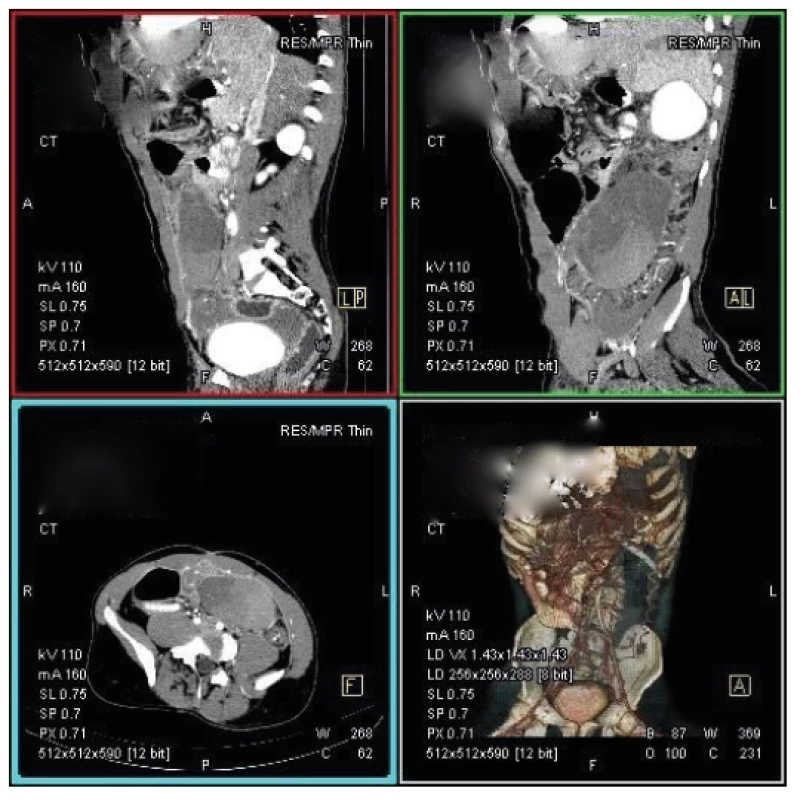
Given the results of clinical and paraclinical examinations and increasing abdominal pain with signs of peritoneal irritation, laparotomy was performed 3 hours after admission. The mean laparotomy exploring the abdominal cavity with the finding of serosanguinolent effusion and ectopically located spleen, 15x10 m in size, with signs of infarction, in the left mesogastrium on the torsioned vascular stem with a length of 25 m, did not find any other pathology in the abdominal cavity (Fig. 2, 3). Splenectomy was performed. Postoperatively, the patient was hospitalized in the ICU and subsequently in a standard inpatient department, where the next course was without complications.
Fig. 2. Intraoperative finding 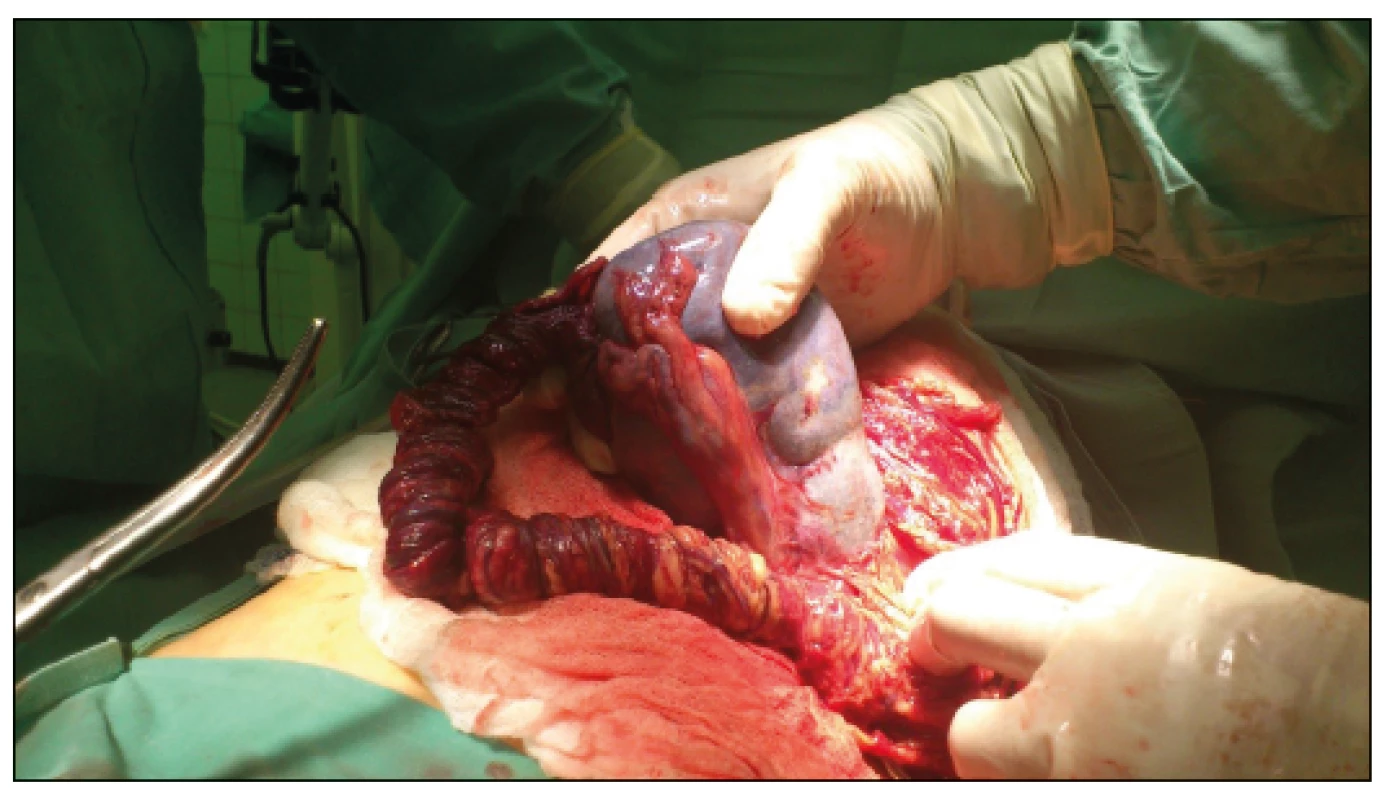
Fig. 3. Spleen with vascular stem 
Discussion
The spleen originates by the proliferation of the celoma epithelium, which is differentiated very soon in the mesenchyme, into which the v. Omphalomesenterica sinistra (v. portae) branches grow, as the base of the vena lienalis, which branch out in the mesenchyme. A little later, a branch of a. coeliaca as arteria lienalis grows into the mesenchyme. By further development, it arches from the dorsal mesogastrium to the left into the peritoneal cavity where it is fixed by its attachments [6].
Wandering spleen is a rare finding described in 0.2-0.5 of splenectomies [3]. The first written mention is from 1667, described by Dutch physician Von Horn. Normally, the spleen is located in the left subfrenium where it is fixed lig. phrenicolienale, lig. pancreaticolienale, lig. gastrolienale [1]. The congenital form of the wandering spleen occurs by their imperfect development, where the vascular stem is elongated with the possibility of spleen migration in the peritoneal cavity. It is mainly diagnosed in children. The acquired form is observed in adults, predominantly in women aged 20–40 years, where the incidence is 70–80 [2]. It is associated with hormonal changes during pregnancy leading to increased laxity of the abdominal wall and spleen attachments.
Chronic or acute torsion of the wandering spleen leads to venous congestion or necrosis. Patients are usually asymptomatic, with palpable resistance in mesogastrium and hypogastrium, or with occasional abdominal pain associated with change of position, changes in intraabdominal pressure when breathing or induced by peristalsis. These chronic problems are caused by intermittent rotation and spontaneous derotation of the long vascular stem. Acute torsion is manifested by nausea, vomiting, fever or signs of peritoneal irritation, which are caused by infarction or spleen necrosis. It may rarely clinically present as acute pancreatitis, in which the tail of the pancreas makes part of the torsion of the splenic vascular stem.
Ultrasound examination usually confirms the absence of spleen in the left subfrenic space with resistance found in left hypogastrium with a typical spleen structure. Duplex sonography can confirm blood flow in the vascular stem. Contrast CT scans usually confirm the diagnosis of wandering spleen and possible infarction, which can also by achieved by MRI angiography.
Patients with asymptomatic wandering spleen can be treated conservatively. Patients with short-term torsion with no signs of splenic infarction can be subjected to detorsion and splenopexia. Splenectomy is fully indicated for infarction.
Splenectomy is associated with a potential risk of decreased immunity - OPSI syndrome. Bacterial blood clearance, IgM level and opsonin activity required for phagocytosis decreases. This life-threatening complication manifests itself especially in younger individuals. The risk of OPSI syndrome is lifelong, occurring in 3–5 of splenectomies with a maximum incidence within 5 years of the surgery. The most common agents are S. pneumoniae, H.influenzae, N. meningitidis. For these reasons, these patients should be periodically actively immunized with an antipneumococcal, antihemophilic and antimeningococcal vaccine after surgery [7].
Conclusion
Wandering spleen usually causes clinical signs of torsion, with no apparent triggering moment. However, cases of torsion or even avulsion of wandering spleen after a blunt trauma of the abdominal wall, both high-energy and with a history of minimal trauma to the abdominal wall, have also been described. Torsion is a known complication of wandering spleen and torsion symptoms depend on the degree of torsion [3, 5]. Severe torsion results in splenic infarction and presents with signs of sudden abdominal event. Therapy then requires laparotomy. If there are no signs of spleen infarction, splenopexy is possible; splenectomy is indicated for signs of infarction or avulsion. Laparotomy has an alternative in laparoscopy with a possible rescue (organ preserving) surgery.
MUDr. Milan Viskupič
Zdroje
- ČIHÁK, R. Anatomie III. Praha : Grada Publishing, 2016. 708 s. ISBN 978-80-247-5636-3
- Dahiya, N., Karthikeyan, D., Vijay, S. et al. Wandering spleen : Unusual presentation and course of events. Indian J Radiol Imaging. 2002, 12, 359-362. ISSN 0971-3026
- Chauhan, NS, Kumar, S. Torsion of a Wandering Spleen Presenting as Acute Abdomen. Pol J Radiol. 2016, 81, 110–113. ISSN 1899-0967
- Pokorný, Vl. a kol. Traumatologie. 1. Vyd. Praha : Triton, 2002. 307 s. ISBN 80-7254-277-x
- Seong, ChK, Dae, YK, In-Koo, K. From the Division of Pediatric Surgery. Seoul, Korea : University of Ulsan College of Medicine and Asan Medical Center. on-line https://www.researchgate.net/profile/Sae_Choi.
- Vacek, Z. Embryologie pro pediatry. 2. dopl. vyd. Praha : Karolinum,1992. 316 s. ISBN 80-7066-562-9 https://www.databazeknih.cz/images_books/16_/161842/embryologie-pro-pediatry-161842.jpg 41
- Vyhnánek, F. Postup při poranění břicha. Rozhl Chir. 2012, 91, 632–638. ISSN 0036-9351
- Wendsche, P., Veselý, R. et al. Traumatologie. Praha : Galén, 2015. 344 s. ISBN 9788074922114
Štítky
Chirurgie všeobecná Traumatologie Urgentní medicína
Článek vyšel v časopiseÚrazová chirurgie
Nejčtenější tento týden
2018 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Stillova choroba: vzácné a závažné systémové onemocnění
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
-
Všechny články tohoto čísla
- Abdominal trauma and wandering spleen - case report
- Addressing of trochanteric femoral fractures using a revision femoral stem with a cervicocapital prosthesis – coxofemoral by-pass
- Complex Response of the Organism to Trauma
- Results of Achilles tendon rupture repair. Classical open approach versus percutaneous suture
- Kelly MJ., Holton AE., Cassar-Gheiti AJ., Hanna SA., Quinlan JF., Molony DC.: The aetiology of posterior glenohumeral dislocation and occurrence of associated injuries. A systematic review.
- Úrazová chirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Results of Achilles tendon rupture repair. Classical open approach versus percutaneous suture
- Complex Response of the Organism to Trauma
- Addressing of trochanteric femoral fractures using a revision femoral stem with a cervicocapital prosthesis – coxofemoral by-pass
- Abdominal trauma and wandering spleen - case report
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



