-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
The Treatment of Comminutive Intraarticular Calcaneal Fractures by External Fixation
Authors: Vladimír Popelka 1; Vojtech Valkó 2; Vladimír Popelka Jr. 3
Authors place of work: Klinika úrazovej chirurgie, Univerzitná nemocnica Bratislava 2 Klinika traumatológie a ortopédie Trnava 3 Ortopedické oddelenie Topoľčany 1
Published in the journal: Úraz chir. 25., 2017, č.3
Summary
Introduction:
Treatment of comminutive calcaneal fractures can be quite severe problem. The authors prefer surgical procedure – external fixation.
Material a methods:
In the period 10 years from 01/2007 to 12/2016 145 patients with 162 intra-articular calcaneal fractures were treated at The Department of Traumatology University Hospital in Bratislava. The Sanders classification of calcaneal fractures was used for fracture evaluation and 23 fractures were comminuted Sanders IV. Twenty-one fractures (n=21) was treated by external fixation (EF) and 2 by plate (ORIF). External fixation was used in 6 patients with bilateral fractures, in 6 fractures with open calcaneal fracture II° and III° Gustilo Anderson. Seven fractures were recorded in polytraumatized patients.
Outcomes:
In group EF (n=21) postoperative evaluation was based on radiographs and the function results of Ankle-Hindfoot scale AOFAS rating system (A-H score). Excellent and good result were achieved in 9 patients, satisfy in 6 patients and poor in 6 patients. Final A-H score was 74 points in range from 51-96. The Böhler, Preiss angles and calcaneal axis were assessed on radiographs postoperatively with optimal values. Complications: 5 patients were recorded with arthrosis, one with pseudoarthrosis, 2 patients with Sudeck´s syndrome and 4 for Compartment syndrom, five patients had to be treated for superficial infection and skin necrosis.
Conclusion:
Our results show that external fixation can achieve good clinical outcomes in patients with open calcaneal fracture as well as in patients with closed cominutive intraarticular fractures. This method became at our deparment a standard procedure.
Key words:
External fixation (EF).
INTRODUCTION
Comminuted calcaneal fractures present a serious therapeutic problem. Most of these fractures are caused with high-energy trauma, either in patients with polytrauma, or as a part of other serious associated injuries. Among low-energy injuries, this type of fracture is observed only in patients with bone decalcification (diabetic patients, smokers, patients of higher age, etc.).
Regarding the fracture morphology, comminuted fractures may affect the anterior part of the posterior articular surface, and the surrounding of the tarsal sinus. These fractures have the best prognosis, as the major part of the posterior articular surface is preserved, and it is possible to reconstruct the calcaneal shape. With an increasing impact of trauma, the whole posterior articular surface becomes damaged, with preserved tuberous fragment. In these cases, it is not possible to restore the articular surface but only the height, length and axis of the calcaneus. In the third case, an extremely strong impact results in comminution of the whole calcaneal bone, usually with associated fractures of the talus and possibly also the distal tibia. These fractures have the worst prognosis, as the reconstruction of the calcaneus is not possible.
There exist also other serious problems associated with closed comminuted calcaneal fractures, such as impairment of soft tissues resulting form contusion and pressure of the haematoma under the thin skin, with subsequent rapid development of bullae, necrosis at the site oppressed with fragments, and development of a compartment syndrome in the central area of the foot. Open fractures may be associated with complications of wound healing [2, 11]. An example of soft tissue damage is presented in Fig. 1.
Fig. 1. Haemorrhagic bullae and soft tissue damage 
Diagnostics and classification
The diagnostic algorithm of intraarticular calcaneal fractures includes clinical examination of soft tissues, determination of the fracture morphology using two basic X-ray projections and computer tomography (CT), assessment of the general condition of the patient and the patient’s cooperation. The most frequently used classification today is the Essex-Lopresti classification, based upon assessment of radiographs, and Sanders’s classification, based upon CT findings.
At our centre, intraarticular calcaneal fractures are classified according to Sanders; comminuted dislocated fractures are classified as Sanders type IV. (Fig. 2).
Fig. 2. Sanders type IV fractures [14] ![Sanders type IV fractures [14]](https://www.prolekare.cz/media/cache/resolve/media_object_image_small/media/image_pdf/d83a7f2c2d5b85542a45bcd8489d919d.jpeg)
Surgical treatment of Sanders type IV fractures
The priority of surgical treatment is to perform an external reduction (restoration of the height, length, width and axis) of the calcaneal bone. Operable comminuted fractures are those, in which at least a part of the tuberous fragment is preserved. At our centre, these fractures are indicated for external fixation, supplemented with K-wires. Comminuted fractures of the whole calcaneus cannot be practically reconstructed, and only conservative treatment is possible, e.g. reduction according to Omoto [9].
Indications for external fixation
- open calcaneal fractures G-A II, III°,
- bad condition of soft tissues,
- fractures Sanders type IV in polytraumatized patients,
- closed comminuted fractures, Sanders type IV.
Contraindications
- comminuted fractures of the whole calcaneal bone, including the calcaneal tuberosity,
- skin defects at the site of pins anchoring,
- compromised condition of the patient [11, 15].
AIMS
The aim of this work was to describe the indications and our own technique of external fixation in patients with comminuted intraarticular calcaneal fractures, and to present our results after this treatment in a retrospective study.
MATERIAL AND METHODS
Material
In the course of a 10-year period (1/2007-12/2016), a total of 162 intraarticular calcaneal fractures in 145 patients were treated at the Department of Trauma Surgery, University Hospital Bratislava, with the average age of 42 years and female to male ratio 1 : 3. During the respective period, we treated a total of 23 comminuted Sanders type IV fractures. In 21 of these fractures, external fixation was applied; two fractures were treated with plate osteosynthesis. In the group of fractures treated with external fixation, there were 6 open fractures Grade II and III according to the Gustilo-Anderson classification, the other 15 fractures were closed. Both calcaneal bones were affected in six patients. Seven comminuted intraarticular fractures were observed in polytraumatized patients.
Methods
The applied methods consisted of three stages.
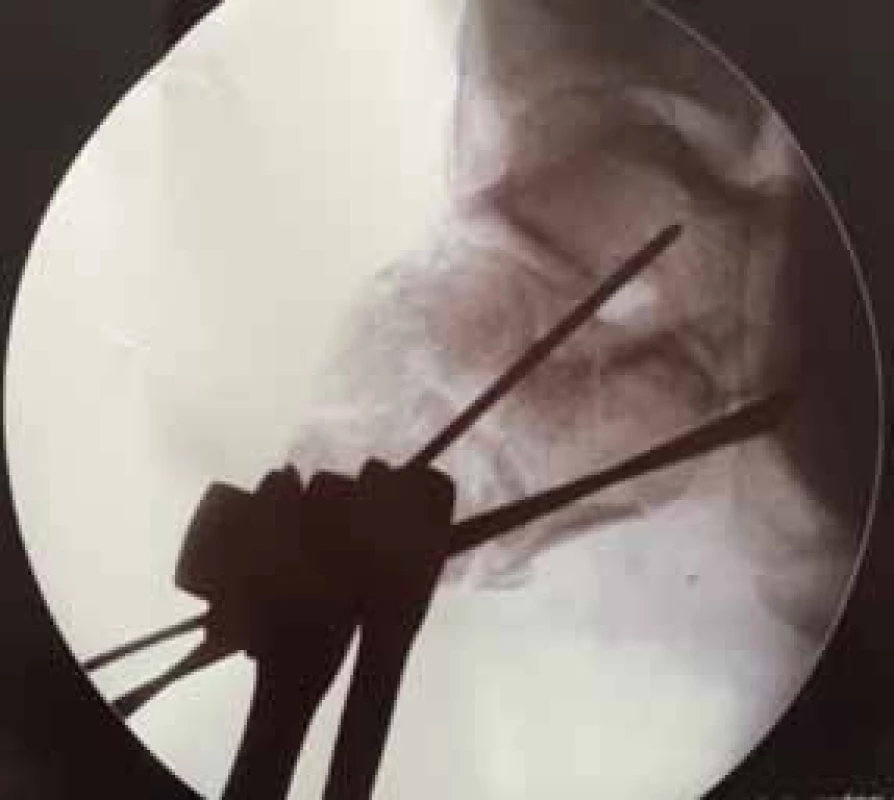
1. Distraction with restoration of the length, height and axis of the calcaneus
This surgical procedure is performed on a patient lying on the stomach, without the use of a tourniquet. Under X-ray control, a K-wire is inserted transversely into the solid fragment, to the depth of 2.2 mm. In the next stage, a metal horseshoe shaped piece is fixed to the inserted K-wire, which is then used to distract the fragments, similarly to the technique recommended by Stehlík, Štulík [12]. The correctness of reduction is controlled in two basic X-ray projections; the medial side and the calcaneal body are adjusted first. After verification of the correct axial position, the solid fragment is transfixed, together with the body, with two or three K-wires, which are inserted, in order to provide sufficient stability, up to the anterior projection of the calcaneus and the talus. In case of impacted fragments and problems with height restoration, it is possible to perform a percutaneous reduction, from a small incision on the lateral side of the calcaneus; fragment elevation is provided with an elevatorium. This procedure results in restoration of the length, height and axis of the calcaneus. In case of unilateral fractures, it is possible to compare the position of fragments and shape of the calcaneus with radiographs of the healthy contralateral extremity. The first stage is concluded with removal of the metal horseshoe-shaped piece (Figs. 3-6).
Figs. 3-6: First stage of surgery, restoration of the height, length and axis, fixation of the body with K-wires
2. Calcaneal body compression
During calcaneal body compression, the width of the calcaneus is restored and minor fragments from the lateral wall are reduced. The width of the calcaneus is verified with an axial X-ray projection, together with fragments at the lateral and medial sides. At our centre, we perform the compression using a thoracic distractor, which compresses the calcaneal body using an opposite mechanism (Figs. 7-8).
Figs. 7-8: Calcaneal body compression using a thoracic distractor
3. Placement of a three-point fixator
After achieving extraarticular reduction (restoration of the height, length, width and axis of the calcaneus), a three-point fixator is applied, which serves for maintaining the position during bone healing. The fixator is fixed from the medial side, and the pins are anchored into the tuberous fragment of the calcaneus, distal diaphysis of the tibia and basis of the Ist metatarsus. After placement of the fixator, the position of fragments is once again verified in Broden’s projections. The surgical procedure is finalized with sterile covering of the wounds. It is always necessary to carefully attend the sites of pin anchoring, as these present the most frequent entry points of infection (Fig. 9).
Fig. 9. External fixator placement 
Timing of surgery and postoperative care
The use of external fixation is indicated either as an emergency procedure (within 6 hours from the injury), or it may be performed as a delayed procedure. Emergency indications for external fixation clearly include open calcaneal fractures Grade II and III according to Gustilo-Anderson classification, which are treated in accordance with all principles of treatment of open fractures. First of all, a thorough debridement of the wound is performed, with rinsing and closing of the wound, followed with fixation. Emergency management is required especially in cases of dislocated fractures, when the fragments and the haematoma press against the skin, and also in comminuted fractures in polytraumatized patients. Delayed management of these types of fractures results in development of skin defects, risk of deep infection, or healing in incorrect position (malunion). Other types of fractures may be treated once the swelling has receded and wrinkles have appeared at the skin, which usually takes 7–10 days [6, 10].
The external fixation is left in place for 6–8 weeks after surgery. During this time frame, soft tissues are healed. After this period, it is possible to exchange the external fixator for an individually made orthosis, which is left in place until definite healing of the fracture, which usually means 10–12 weeks from the injury. Weight loading of the affected extremity is possible only after the fracture has completely healed.
RESULTS
In order to evaluate the functional outcomes in our patients treated with external fixation (n=21), we used the Ankle-Hindfoot scale AOFAS (A-H score) system. The patients were followed until 36 months after injury. The resulting A-H score of our patient population was 74 points, in the range of 51–96 points (tab. 1). We managed to achieve excellent and good functional outcomes in 9 patients and satisfactory outcomes in 6 patients; unsatisfactory outcome was observed in the remaining 6 patients.
Tab. 1: Functional outcome following treatment of Sanders type IV fractures
Sanders IV
A-H
EF 21
74
(51-96)
(Excellent 90–100 p., good 80–89 p., satisfactory 65–79 p., unsatisfactory less than 64 p.)
During X-ray controls, we monitored the Böhler’s and Preiss’ angles of the calcaneal axis.
When comparing the results with patients treated using plate osteosynthesis, in both of whom the fixation failed, we managed to achieve a significantly better position of the fragments in patients treated with external fixator. We did not observe a decrease of the Bohler’s angle below 10° in any patient, or a significant deviation of the calcaneal axis (valgotization over 10° and valgotization over 5°) (tab. 2).
Tab. 2: X-ray results in fractures Sanders type IV
Sanders IV
Böhler’s angle after treatment
Preiss’ angle after treatment
External fixator
22° (13–28°)
18° (17–26°)
Complications following EF procedures
In 5 cases, we had to perform a subtalar arthrodesis due to painful arthrosis, and in one case, we observed a development of pseudoarthrosis. In 4 cases, compartment syndrome was undiagnosed, which was manifested with paresthesias and development of hammertoes. In three patients, it was necessary to perform a tenotomy of the deep flexors of the 2nd to 4th toe, one patient required also Z-plasty of the Great Toe flexor. Sudeck’s syndrome was observed in two cases. Superficial infection was noted in five cases in the area of insertion of K-wires and Schanz screws, followed with a development of skin necrosis after haematomas and blisters.
DISCUSSION
Primary arthrodesis?
There are only sparse publications in the expert literature dealing with the treatment of comminuted calcaneal fractures. Some authors perform plate osteosynthesis from an extended lateral approach, and at the same time perform talo-calcaneal arthrodesis of the subtalar joint with screws [4, 5, 14]. In patients with fractures Sanders type IV, Stehlík, Štulík perform a miniinvasive reduction of the calcaneus; primary arthrodesis is achieved from a limited lateral approach [12].
At our centre, we do not perform primary arthrodesis of the subtalar joint, as we have observed that the main source of problems for patients following calcaneal fractures is an incorrectly performed external reduction, and not incorrect reconstruction of the posterior articular surface (internal reduction). There even exist cases when the patients do not experience pain, despite serious post-injury arthrosis. That is why we consider the reconstruction of the length, height and axis (external reduction) to be primary. We indicate a secondary arthrodesis only in patients complaining about difficulties associated with arthrosis of the subtalar joint. We also consider the use of plate osteosynthesis in cases of fractures Sanders type IV, in which not only bone structures have been affected but also the soft tissues, to be very risky, due to the risk of deep infection. Plate osteosynthesis may also fail in the comminuted terrain, which has been confirmed by the two cases of our patients, in whom the screws became loose. That is why we indicate external fixation not only in patients with open but also closed fractures Sanders type IV.
EF localization and anchoring
From the biomechanical point of view, the way an external fixator is placed is very important. Besch et al., on the basis of their biomechanical analyses, recommend placing the external fixator from the medial side, which does not concern only stability. In this case, if physician decides to perform a plate osteosynthesis, the lateral side of the calcaneus remains intact, and enables an extended lateral approach. According to these authors, it is most advantageous to anchor the pins into the distal third of tibial diaphysis, the basis of the Ist metatarsus, and the calcaneal tuber. When placing the pins in this way, a sufficiently large window appears in the EF construct for X-ray control and treatment of wounds and defects [3, 13]. Also at our centre, we respect these principles and perform pin fixation in this way.
Types of external fixation in calcaneal fractures
Literature sources present the use of various types of external fixation. French authors Bégué et al. use the Hoffmann external fixator by Stryker, which is placed from the medial side. The authors use this fixator for all types of fractures. They have used this construction in a total of 19 fractures, 13 of which were fractures Sanders type II and IV. They managed to reconstruct the height in 13 cases, the length in 17 cases, and the calcaneal axis in all cases [1].
Mc Garvey et al. have treated 11 open and 22 closed fractures with the Ilizarov external fixator. The average AOFAS score was 72 points [8]. Magnan et al. used a calcaneal minifixator by Orthofix in 54 fractures. The fixator was placed from the lateral side; two of the pins were placed into the tuberous fragment, and two into the fragment of posterior articular surface. The advantage of this fixator is the possibility to perform a reduction of the fragments and keep the correct position. The authors managed to achieve excellent and good results in up to 90.7% of patients [7].
At our centre, we most usually use the Hoffmann external fixator by Stryker, and also an older type of tubular Modus fixator made by the Medin Company.
Compartment syndrome
When treating closed fractures Sanders type IV with external fixation, we observed four fractures with a compartment syndrome diagnosed at later stages. Skin infection at the site of K-wire insertion and necrosis at the bullae sites were observed in five cases. We consider the cause of the compartment syndrome to be in the fact that comminuted calcaneal fractures directly communicate with the central area of the foot, where blood leakage and increased pressure occur. This results in oppression of the muscles and the nervous-vascular system. The only way how to prevent this complication is an early diagnostics and decompression using fasciotomy.
Figs.10-16: Radiograph and functional outcome following external fixation in a 38-year-old patient
CONCLUSION
At our centre, we consider external fixation to be a technique of choice in the treatment of open calcaneal fractures Grade II and III according to Gustilo-Anderson classification, and also comminuted closed intraarticular fractures. Our results confirm that, together with additional osteosynthesis using K-wires, EF provides sufficient stability, together with all conditions required for healing of this type of calcaneal fractures.
Zdroje
- BÉGUĚ, T., MEBTOUCHE, N., AUREGAN, J.C. et al. External fixation of the thalamic portion of a fractured calcaneus: A new surgical technique. Orthopedics and Traumatology Surgery and Research. 100, 2014, 429–432.
- BENIRSCHKE, SK., KRAMER, PA. Wound healing complications in closed and open calcaneus fraktures, J Orthop Trauma. 2004, 18, 1–6.
- BESCH, L., SCHMIDT, I., MUELLER, M. et al. A biomechanical evaluation to optimize the configuration of a hinged external fixator for the primary treatment of severely displaced intraarticular calcaneus fractures with soft tissue damage. Foot Ankle Surgery. 47, 2008, 1, 26–33.
- BUCH, BD., MYERSON, MS., MILLER, SD. Primary subtalar arthrodesis for the treatment of comminuted calcaneal fractures. Foot and Ankle Internat. 1996, 17, 61–70.
- COUGHLIN, MJ., MANN, RA., SALTZMAN, ChL. Surgery foot and ankle. eight edition. Mosby Elsevier, 2007. 2073 p.
- LYSÁK, P., GUŘAN, M., BUDOŠ, M. Operační léčba zlomenin patní kosti. Úraz chir. 2016, 24, 12–17. ISSN 1211-7080
- MAGNAN, B., BORTOLAZZI, R., MARANGON, M. et al. External fixation for displaced intra-articular factures of the calcaneum. The Bone and Joint Journal. 2006, 30, 10, 10–21.
- MC GARVEY, WC., BURRIS, MW., CLANTON, TO. et al. Calcaneal Fractures: Indirect Reduction and External Fixation. Foot and Ankle International. 2006, 27, 494–499.
- OMOTO, H., SAKURADA, K., SUGI, M. A new method of manual reduction for intraarticular fracture of calcaneus. Clin Orthop. 1983, 177, 104–111.
- POMPACH, M., CARDA, M., ŽILKA, L. et al. Hřebování patní kosti. Úraz chir. 2015, 23, 31–38, 1211-7080.
- POPELKA, V. Calcaneal fracures [e-book]. Bratislava : Herba, 2017, 130.http://www.knihy.herba.sk/prezentacie/calcaneal-fractures/files/assets/basic -
- STEHLÍK, J., ŠTULÍK, J. Zlomeniny patní kosti. Praha : Galén, 2005. 113 s.
- TAREK, AE, ANDY, ET, RUPERT, DF. Temporary external fixation faciblitates open reduction and internal fixation of intra-articular calcaneal fractures. Acta Ortop Belg. 2015, 79, 738–741.
- SANDERS, R., FORTIN, P., Di PASQUALE, A. Operative treatment in 120 displaced intra-articular calcaneal fractures. Result using a prognostic computed tomographic scan clasification. Clin Orthop. 1993, 290, 87–95.
- ZWIPP, H., RAMMELT, S., BARTHEL, S. Kalkaneusfraktur. Unfallchirurg. 2005, 108, 737–760.
Štítky
Chirurgie všeobecná Traumatologie Urgentní medicína
Článek vyšel v časopiseÚrazová chirurgie
Nejčtenější tento týden
2017 Číslo 3- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Stillova choroba: vzácné a závažné systémové onemocnění
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
-
Všechny články tohoto čísla
- Osteosynthesis of dislocated calcaneal fractures at our centre using the intramedullary C-Nail
- The Treatment of Comminutive Intraarticular Calcaneal Fractures by External Fixation
- Přečetli jsme za vás
- Therapeutic algorithm in a patient with open tibial fracture with extensive laceration of the soft tissue coverage – case report contribution to the discussion about limb salvage
- Bifocal bone transport in the treatment of infected nonunion of the tibia - case report
- Úrazová chirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- The Treatment of Comminutive Intraarticular Calcaneal Fractures by External Fixation
- Therapeutic algorithm in a patient with open tibial fracture with extensive laceration of the soft tissue coverage – case report contribution to the discussion about limb salvage
- Osteosynthesis of dislocated calcaneal fractures at our centre using the intramedullary C-Nail
- Bifocal bone transport in the treatment of infected nonunion of the tibia - case report
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání