-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaCharacterising the Mucosal and Systemic Immune Responses to Experimental Human Hookworm Infection
The mucosal cytokine response of healthy humans to parasitic helminths has never been reported. We investigated the systemic and mucosal cytokine responses to hookworm infection in experimentally infected, previously hookworm naive individuals from non-endemic areas. We collected both peripheral blood and duodenal biopsies to assess the systemic immune response, as well as the response at the site of adult worm establishment. Our results show that experimental hookworm infection leads to a strong systemic and mucosal Th2 (IL-4, IL-5, IL-9 and IL-13) and regulatory (IL-10 and TGF-β) response, with some evidence of a Th1 (IFN-γ and IL-2) response. Despite upregulation after patency of both IL-15 and ALDH1A2, a known Th17-inducing combination in inflammatory diseases, we saw no evidence of a Th17 (IL-17) response. Moreover, we observed strong suppression of mucosal IL-23 and upregulation of IL-22 during established hookworm infection, suggesting a potential mechanism by which Th17 responses are suppressed, and highlighting the potential that hookworms and their secreted proteins offer as therapeutics for human inflammatory diseases.
Published in the journal: . PLoS Pathog 8(2): e32767. doi:10.1371/journal.ppat.1002520
Category: Research Article
doi: https://doi.org/10.1371/journal.ppat.1002520Summary
The mucosal cytokine response of healthy humans to parasitic helminths has never been reported. We investigated the systemic and mucosal cytokine responses to hookworm infection in experimentally infected, previously hookworm naive individuals from non-endemic areas. We collected both peripheral blood and duodenal biopsies to assess the systemic immune response, as well as the response at the site of adult worm establishment. Our results show that experimental hookworm infection leads to a strong systemic and mucosal Th2 (IL-4, IL-5, IL-9 and IL-13) and regulatory (IL-10 and TGF-β) response, with some evidence of a Th1 (IFN-γ and IL-2) response. Despite upregulation after patency of both IL-15 and ALDH1A2, a known Th17-inducing combination in inflammatory diseases, we saw no evidence of a Th17 (IL-17) response. Moreover, we observed strong suppression of mucosal IL-23 and upregulation of IL-22 during established hookworm infection, suggesting a potential mechanism by which Th17 responses are suppressed, and highlighting the potential that hookworms and their secreted proteins offer as therapeutics for human inflammatory diseases.
Introduction
The hookworms Necator americanus and Ancylostoma duodenale infect an estimated 740 million people, mostly in tropical regions of the world, causing significant burden of disease [1]. As for most Neglected Tropical Diseases (NTDs), there is currently no prophylactic or therapeutic vaccine against hookworm infection, although clinical trials are underway on a number of promising candidate antigens [2]. Despite efforts to eliminate this disease from developing countries, experimentally-induced hookworm infection offers potential as an anti-inflammatory therapy for human autoimmune [3] and allergic [4], [5] diseases. However, despite their importance in regards to disease burden in resource poor countries (especially in children and women of child bearing years) and their potential as an anti-inflammatory therapy for use in industrialized countries, little is known about the mucosal immune responses of humans to hookworm, or indeed any other gastrointestinal (g.i.) helminths parasites.
Unlike many other human g.i. helminths, despite a robust, parasite-specific immune response, naturally acquired protection against hookworm is only partially effective at best; indeed, in endemic areas the oldest people often have the heaviest worm burdens [6], [7]. Nonetheless, previous studies on people naturally infected with hookworm have identified associations between reduced egg counts and Th2 responses. For example, IL-5 production correlates positively with resistance to reinfection after anthelmintic drug cure [8], and levels of IgE reactive against defined larval antigens are negatively associated with hookworm egg counts [9].
A small number of experimental infections in hookworm naive, healthy human volunteers have been conducted, with an exclusive focus on the systemic immune response at both the humoral and cellular levels [10]–[12], and gross observations of the gut via capsule endoscopy [3]. These earlier observations described the onset of eosinophilia, production of parasite specific IgG and IgE, and secretion of both Th1 (IFN-γ and TNF-α) and Th2 (IL-5 and IL-13) cytokines. With the onset of patency, IL-10 was produced and T cell proliferation was blunted and was not restored until long after curative therapy [7], [11].
Most of our understanding of mucosal immunity to g.i. nematodes comes from studies in laboratory mice. Th2 cytokines are required for resistance to many g.i. helminths, as seen in mice that are genetically deficient in Th2 cytokines and associated signalling molecules [13], [14]. In the draining lymph node, Th2 cytokines are responsible for class-switching of B cells to IgG1 and IgE, as well as recruiting and activating innate immune cells and blocking parasite effector molecules [15]. At the site of adult worm residence in mice, the duodenum, Th2 cytokines are responsible for increased mucus and fluid production in the gut and smooth muscle contractility, which increases ejection of parasites [16], [17]. They also lead to recruitment, expansion and differentiation of innate immune cells such as eosinophils, alternatively activated macrophages, mast cells and basophils in the gut which can directly or indirectly lead to ejection of parasites [15]. Thus differentiation of Th2 cells and production of Th2 cytokines, both systemically and in the mucosa, may be important for intestinal parasite clearance in mice.
Th1 (and Th17) responses are also induced during some helminth parasite infections. In the absence of a Th2 response, or where Th1/Th17 responses have been artificially upregulated, an uncontrolled Th1/Th17 response to schistosomes leads to acute pathology and ultimately death in mice [18], [19]. Thus, it has been proposed that the Th2 response generated during schistosomiasis may downregulate Th1/Th17 responses, leading to suppression of immunopathology and survival of the host [15]. Suppression of Th17 responses by Th2 cytokines in the mucosa has also been shown in mice infected with g.i. nematodes [20], prompting the suggestion that nematodes may ameliorate inflammatory gut diseases by dampening pro-inflammatory Th17 responses.
We previously reported a study using human hookworm infection to treat celiac disease [21]. Although no overt suppression of clinical pathology was detected, suppression of gluten-specific inflammatory Th1 and Th17 responses was seen in the mucosa [22]. After established hookworm infection but prior to challenge with gluten, samples were taken from control and hookworm infected individuals, and here we prospectively collected data on the hookworm-specific cytokine responses in the peripheral circulation and, for the first time, the duodenal mucosa, of hookworm naive individuals before and after controlled experimental infection with N. americanus. This is the first description of the mucosal immune response of humans to hookworms; indeed, other than a case study where an individual patient with active ulcerative colitis was treated with whipworm and the mucosal immune response was assessed [23], this is the first report of the mucosal immune response in healthy volunteers in a clinical trial to experimental infection with helminths, and provides valuable information to support the development of both vaccines against hookworm infection and hookworm-derived peptidic therapies for inflammatory diseases.
Methods and Materials
Ethics statement
The Princess Alexandra Hospital, Queensland Institute of Medical Research and Townsville Hospital Human Research Ethics Committees approved the study. Written informed consent was obtained from all subjects.
Clinical protocol
The methods used for our placebo-controlled, blinded clinical trial using hookworm to treat celiac disease have been described elsewhere [21]. Briefly, twenty confirmed HLA-DQ2+ celiac disease sufferers on a long-term gluten-free diet (and therefore in remission for celiac disease) were recruited, randomised into 2 groups and either infected with 10 infective larvae (L3) of N. americanus (“hookworm” group) or given a placebo of topical chilli (Tabasco sauce) (“control” group). Twelve weeks later, a booster infection of 5 infective larvae (or a placebo infection) was administered. At week 20 post-prime infection, all individuals were given a gluten challenge consisting of four slices of white bread per day for 5 days. This trial will herein be referred to as “Trial 1”. Approximately 6 months after the end of Trial 1 (during which all participants returned to a strict gluten-free diet), seven of the ten control subjects (those who did not receive hookworm in Trial 1) participated in a continuation trial: two could not participate due to other commitments, and one could not participate due to raised tissue transglutaminase antibodies. These 7 participants were infected with N. americanus, boosted and challenged with gluten in an identical manner to that described for Trial 1. This trial will herein be referred to as “Trial 2”.
In both trials hookworm infection was confirmed in all subjects by either fecal egg counts and/or identification of adult parasites in the duodenum during endoscopy [21]. The structure of the trials is summarised in Figure 1.
Fig. 1. Trial design. 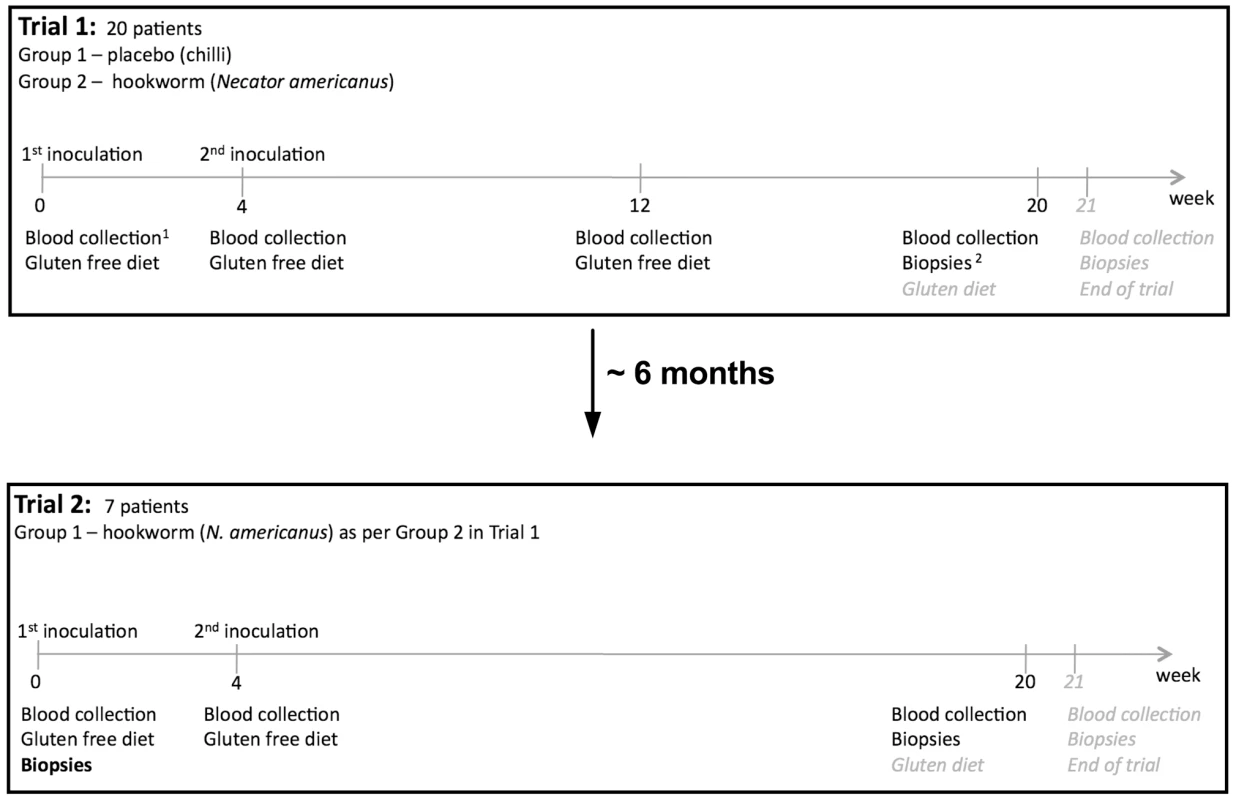
For Trial 1, 20 patients were chosen according to selection criteria [21] and divided into two groups of 10, placebo control and hookworm infected (HW). All 20 patients completed the trial. For Trial 2, seven of the 10 patients from Group 1 in Trial 1 (placebo) chose to participate in the next trial and received hookworm infection and gluten challenge in an identical manner to that described for Group 2 in Trial 1. The only difference was that gut biopsies were taken at week 0 (prior to hookworm infection; denoted in bold font) in addition to biopsies taken at weeks 20 and 21. For the purposes of this study, sample collection ceased at week 20 (prior to gluten administration) and tissues from week 21 were not utilized, except for samples taken from the worm attachment site which were collected at week 21; week 21 tissues were critical for assessment of the effect of hookworm on the anti-gluten response in celiac disease and are therefore highlighted in italicised grey font and have been reported in relevant publications [21], [22]. 1Forty millilitres of blood per person were collected at weeks 0, 4, 12 (Trial 1 only), 20 and 21. 2Gut biopsies were taken at weeks 0 (Trial 2 only), 20 (pre-gluten ingestion) and 21 (post-gluten ingestion) using a gastroscope as described elsewhere [21]. Peripheral blood mononuclear cell acquisition and antigen restimulation
Peripheral blood mononuclear cells (PBMCs) were isolated from blood drawn into heparinised tubes over a Ficoll-Paque Plus gradient (GE Healthcare) as described in Figure 1. Cells were cultured for 120 h at 37°C, 95% O2/5% CO2 at 2.5×105 cells/well in round-bottom 96-well plates in Tissue Culture Medium (Med: RPMI 1640, 10% fetal bovine serum, 100 U/µl penicillin, 100 µg/ml streptomycin and 2 mM L-glutamine), in the absence (“Med”) or presence of 10 µg/ml N. americanus excretory/secretory proteins (NaES). NaES was prepared as previously described [24], and was depleted of endotoxin using two rounds of phase separation using Triton-X114 [25]. Endotoxin levels in NaES after depletion were assessed using E-toxate (Sigma); levels were below the detection limit of the assay (<0.05–0.1 EU/ml) for stock solution of NaES at a concentration of 1.77 mg/ml. Cell-free supernatants were collected and analysed using a Cytometric Bead Array (CBA; BD Biosciences). Antigen-specific production of cytokines was determined by subtraction of baseline cytokine levels from unstimulated PBMCs (Med) from those stimulated with NaES.
Biopsy culture
Duodenal biopsies were taken from week 20 post-prime infection (prior to gluten challenge) in both groups from Trial 1, and also from sites adjacent to (within 0.5 cm) a hookworm attachment site where adult hookworms were found in the upper duodenum (5 of 10 hookworm-infected individuals) by endoscopy [21]. In Trial 2, biopsies were taken at week 0 (prior to infection) and at week 20 post-prime infection. Whole biopsies were placed in wells of a 24-well plate containing 500 µl MED alone or MED containing 10 µg/ml NaES, and cultured for 24 h in 95% O2/5% CO2 at 37°C. Cell-free supernatants were taken and analysed using a Cytometric Bead Array (BD Biosciences). Biopsies were then placed into Trizol (Invitrogen) and RNA was purified following the manufacturer's protocols.
Quantitative real-time RT-PCR
For quantitative real-time RT-PCR (qPCR), RNA was prepared from biopsies in Trial 2 by the phenol-chloroform method (Trizol). mRNA quality was tested using a Bioanalyzer (Agilent) or agarose gel electrophoresis prior the reverse-transcription step. cDNA was prepared using Superscript III reverse transcriptase (Invitrogen) according to the manufacturer's protocol. PBMCs from a healthy donor were cultured for 24 h in 95% O2/5% CO2 at 37°C with phytohemagglutinin-A (PHA) and used to create standard curves and positive controls. Levels of transcripts were normalised to the housekeeping gene β-actin and are presented as arbitrary units. SyBr Green mastermix (Qiagen) was used in a Rotor-Gene Q thermal cycler (Qiagen) according the manufacturer's protocol. Primers used for each gene product are listed in Table S1.
Statistical analyses
All analyses were carried out using Prism 5.0 (Graphpad). Paired data were compared by Wilcoxon matched-pairs signed rank test; 3 or more sets of paired data were compared by the Kruskal-Wallis non-parametric ANOVA. Unless otherwise indicated, differences were not significantly different. N.S. = Not Significant, * = p<0.05, ** = p<0.01, *** = p<0.001. All error bars show the standard error of the mean.
Results
Th2 immune responses to hookworm infection
All volunteers infected with hookworm were confirmed to have active infections using a combination of capsule endoscopy (to visualize adult worms in the gut) and/or the presence of eggs in the feces [21]. PBMCs from volunteers infected with 15 third-stage larvae (L3) of N. americanus were restimulated with NaES and showed increased antigen-specific production of the Th2 cytokines IL-4, IL-5 and IL-13, compared with PBMCs from uninfected controls, reaching a peak 12 weeks after infection (Figure 2A–C), although increases in IL-4 levels did not reach statistical significance. These data indicate that, as expected, hookworm infection induces a systemic Th2 response.
Fig. 2. Systemic production of hookworm-specific cytokines. 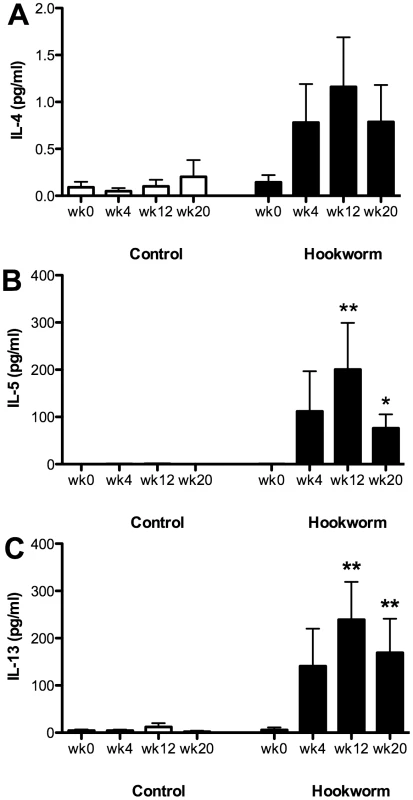
Peripheral blood mononuclear cells were harvested from subjects in Trial 1 and cultured for 120 h at 37°C in either tissue culture medium (MED) or MED containing 10 µg/ml Necator americanus ES products (NaES). Cell supernatants were removed and levels of IL-4 (A), IL-5 (B) and IL-13 (C) determined using a Cytometric Bead Array. Cytokine levels from PBMCs stimulated with just MED alone were subtracted from those stimulated with NaES. Data were analysed by Kruskal-Wallis non-parametric ANOVA, comparing time points at weeks 4, 12 and 20 to week 0 within each group. To establish whether this Th2 response was present at the site of adult worm residence, duodenal biopsies were taken at week 20 after hookworm infection (immediately prior to gluten challenge). Biopsies were also taken from directly adjacent to the hookworm attachment site at week 21 (after gluten challenge) from 5 of the 10 hookworm-infected individuals where adult worms were observed by endoscopy. All biopsies were cultured without stimulation and supernatants were removed for cytokine analysis. Biopsies from both control and hookworm infected individuals produced similar levels of IL-4 and IL-13 (Figure 3A and C). However, significantly increased levels of IL-5 were produced by biopsy cells from hookworm-infected individuals, especially those biopsies taken adjacent to the hookworm attachment site (Figure 3B). The increased levels of IL-5 at the hookworm attachment sites were not the result of gluten challenge, because at week 21, biopsies from sites distal to the hookworm attachment sites produced decreased levels of IL-5 (12.77 pg/ml +/ − 13.90) compared to biopsies from week 20 (23.47 pg/ml +/ − 31.88) or the hookworm attachment site (41.18 pg/ml +/ − 21.33).
Fig. 3. Production of Th2 cytokines in the duodenal mucosa of hookworm infected individuals. 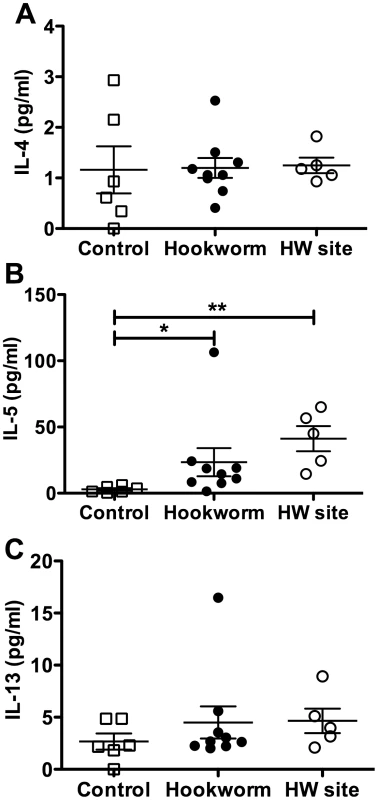
Duodenal biopsies from Trial 1, taken from either the duodenum at week 20 post-infection or from directly adjacent to an adult hookworm attachment site (HW site – determined by endoscopy) at week 21 in the hookworm group only, were cultured for 24 h in tissue culture medium at 37°C with 95% O2/5% CO2. Cell supernatants were removed and levels of IL-4 (A), IL-5 (B) and IL-13 (C) were determined using a Cytometric Bead Array. Data were analysed by Mann-Whitney U test. Characterisation of the mucosal immune response before and after hookworm infection
Figures 2 and 3 show that experimental hookworm infection induces a systemic, Necator antigen-specific, Th2 response, and a weak but detectable basal mucosal Th2 response. In order to further characterise this response, duodenal biopsies were taken before (week 0) and after an established hookworm infection (week 20 post-prime infection) from infected individuals in Trial 2. Cytokines were measured in the supernatants of duodenal biopsies cultured for 24 h in medium only. There was no significant difference in the protein levels of IL-2, IFN-γ, TNF-α, IL-17A, IL-4, IL-5, IL-10 and IL-13 when comparing wk 0 (pre-infection) to wk 20 (post-infection) (Fig. S1). RNA transcripts were obtained to assess gene expression levels in the absence of ex vivo stimulation for a range of cytokines and transcription factors associated with different T helper cell phenotypes. Levels of mRNA encoded by the Th2/Th9 genes IL-4, IL-5, IL-13, IL-9 and GATA-3 appeared unaffected by hookworm infection using this technique (Figure 4A–E). Accumulation of mRNA transcribed by the regulatory T cell associated gene Foxp3 (Figure 4F), or the gene encoding the immunosuppressive cytokine TGF-β (Figure 4G), were also unaffected, although levels of Foxp3 mRNA were below the detection limits of the assay in the majority of the samples tested. However, accumulation of mRNA encoded by the ALDH1A2 gene was significantly increased after hookworm infection (Figure 4H). ALDH1A2 encodes retinaldehyde dehydrogenase, an enzyme that is important for production of retinoic acid from vitamin A metabolites. Transcription of the Th1 cytokine gene IFN-γ (Figure 4I) and the T cell proliferative cytokine gene IL-15 (Figure 4J) were also upregulated after hookworm infection. Levels of the Th17-associated genes, IL-17A and RORγt, were both extremely low, close to or below the detection limit of the assay, but nevertheless appeared unchanged after hookworm infection (Figure 4K and M). Accumulation of mRNA transcribed by the Th17 inducing and stabilising cytokine IL-23, however, was strongly down-regulated after hookworm infection (9.6-fold decrease in the mean value) (Figure 4L).
Fig. 4. Ex vivo cytokine gene expression in the duodenal mucosa of hookworm infected individuals. 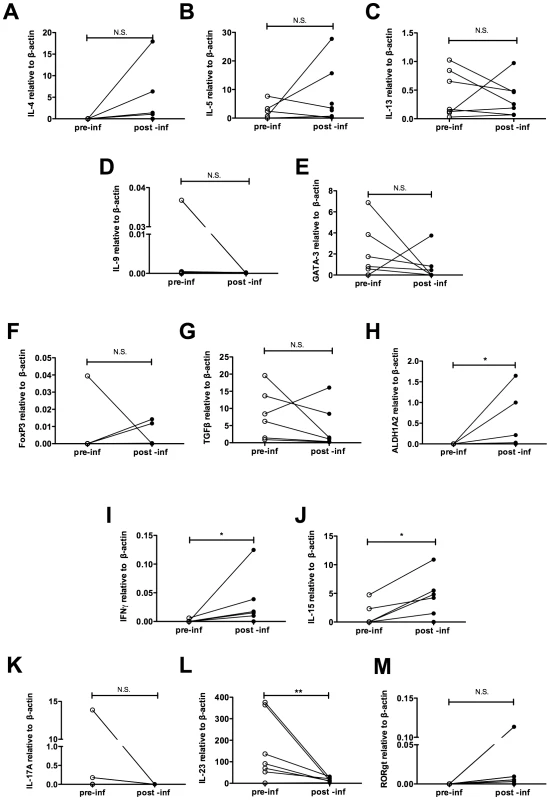
Duodenal biopsies from Trial 2 were taken before (week 0) and 20 weeks after hookworm infection, and RNA was prepared ex vivo. Levels of IL-4 (A) IL-5 (B), IL-13 (C), IL-9 (D), GATA-3 (E), Foxp3 (F), TGF-β (G), ALDH1A2 (H), IFN-γ (I), IL-15 (J), IL-17A (K), IL-23 (L) and RORγt (M) transcripts were determined by quantitative real time RT-PCR. Hookworm antigen-specific systemic and mucosal responses
In Trial 1, PBMCs that were restimulated with NaES from hookworm-infected individuals but not uninfected controls produced Th2 cytokines (Figure 2). PBMCs and duodenal biopsies were cultured with NaES or MED alone from all individuals in Trial 2 before and after hookworm infection. Supernatants from both cultures were taken for soluble cytokine analysis, and restimulated biopsies were taken after culture for RNA preparation and qPCR. In pre-infection biopsies (wk0), there was no significant difference in IL-2, IFN-γ, TNF-α, IL-17A, IL-4, IL-5, IL-10 and IL-13 produced after restimulation in culture with NaES compared to medium only (Figure S2). When PBMCs from hookworm-infected participants were restimulated with NaES they produced IL-4, IL-5 and IL-13 (Figure 5A, D, G), as previously shown (Figures 2A–C). We then extended these studies to show that restimulated biopsies also produced these cytokines, both at the levels of secreted protein (Figure 5B, E and H) and RNA transcripts (Figure 5C, F and I), although we did not detect a change for IL-4 transcript levels. PBMCs and biopsies from infected individuals also produced IL-9 and IL-10 in response to NaES (Figure 5J–O), however increased IL-10 production to NaES was not detectable by qPCR.
Fig. 5. Systemic and mucosal hookworm specific immune responses. 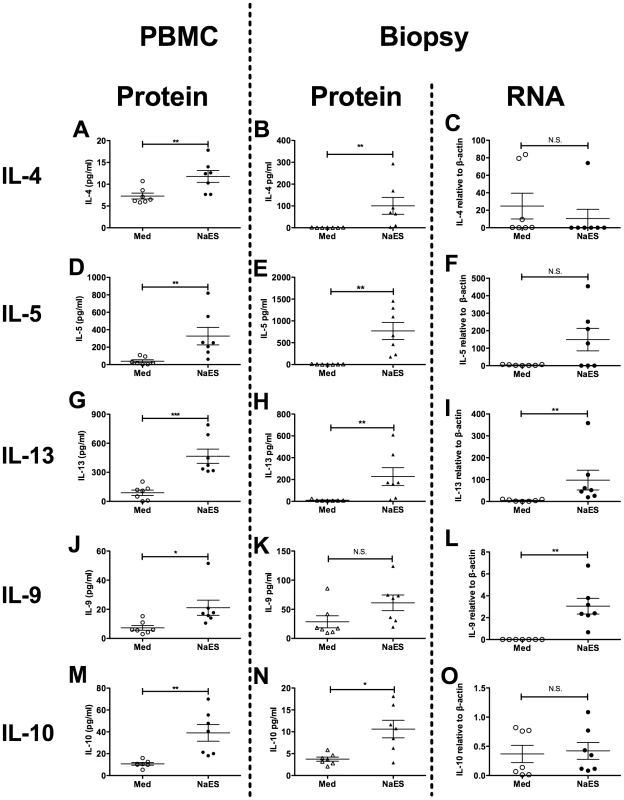
Peripheral blood mononuclear cells (PBMCs) from Trial 2 were cultured for 120 h with either tissue culture medium (Med) or Med containing 10 µg/ml Necator americanus ES products (NaES). Duodenal biopsies were also taken at week 20 post-infection, and cultured for 24 h at 37°C, 95% O2/5% CO2, in either Med alone or 10 µg/ml NaES in Med. Cell-free supernatants were taken from both PBMCs and biopsy cultures and levels of soluble cytokines were determined by cytometric bead array. RNA was also prepared from biopsies after stimulation and quantitative real time RT-PCR was used to determine levels of cytokine gene transcripts. Soluble cytokines released from PBMCs are shown in panels A, D, G, J and M. Biopsy-derived soluble cytokines are shown in panels B, E, H, K and N. Biopsy cytokine transcripts are shown in panels C, F, I, L and O. Cytokine levels determined were IL-4 (A–C), IL-5 (D–F), IL-13 (G–I), IL-9 (J–L) and IL-10 (M–O). The qPCR data from unstimulated biopsies taken before and after hookworm infection indicated that infection may induce a Th1 response, while suppressing a Th17 response (Figure 4). We also assessed the levels of inflammatory cytokines produced by PBMCs and biopsy cultures when stimulated with NaES. As shown in Figure 6, restimulation with NaES induced upregulation of the proliferative cytokine IL-2 in both PBMCs and biopsy cultures at the protein level (Figure 6A and B), but corresponding levels of mRNA were too low to detect by qPCR (Figure 6C). Restimulation with NaES also induced production of the Th1 cytokine IFN-γ from PBMCs (Figure 6D), but not from biopsy cultures, either at the protein (Figure 6E) or RNA (Figure 6F) levels. We did not detect upregulation of the Th17 cytokine IL-17A from cultures of PBMCs or biopsies restimulated with NaES (Figure 6G–I). The accumulation of mRNA transcribed by another T cell proliferative cytokine gene, IL-15 (Figure 6J), the immunosuppressive cytokine gene TGF-β (Figure 6K) and the wound healing cytokine IL-22 (Figure 6L), were also increased in NaES restimulated biopsies. Again, biopsies taken prior to hookworm infection did not produce upregulated expression of any of these cytokines upon NaES stimulation (Figure S2).
Fig. 6. Systemic and mucosal hookworm specific immune responses. 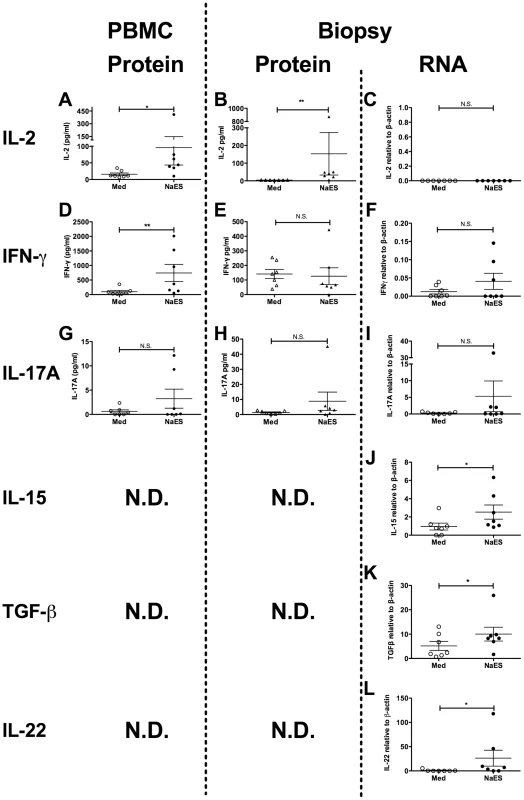
Peripheral blood mononuclear cells (PBMCs) from Trial 2 were cultured for 120 h with either tissue culture medium (Med) or Med containing 10 µg/ml Necator americanus ES products (NaES). Duodenal biopsies were also taken at week 20 post-infection, and cultured for 24 h at 37°C, 95% O2/5% CO2, in either Med alone or 10 µg/ml NaES in Med. Cell-free supernatants were taken from both PBMCs and biopsy cultures and levels of soluble cytokines determined by Cytometric Bead Array. RNA was also prepared from biopsies after stimulation and quantitative real time RT-PCR was used to determine levels of cytokine gene transcripts. Soluble cytokines released from PBMCs are shown in panels A, D and G. Biopsy-derived soluble cytokines are shown in panels B, E and H. Biopsy cytokine transcripts are shown in panels C, F, I, J and K. Cytokine levels determined were IL-2 (A–C), IFN-γ (D–F), IL-17A (G–I), IL-15 (J), TGF-β (K) and IL-22 (L). Discussion
Here, we present the first description of the mucosal cytokine response of healthy humans to either an experimental or naturally acquired helminth infection. As all individuals in this trial were infected when in established remission of their celiac disease whilst maintaining a strict gluten-free diet, and all analyses presented in this study were performed with blood and tissue collected prior to gluten challenge (excepting data acquired from the adult hookworm attachment site, Figure 3), we regard the subjects as being representative of normal, healthy individuals, and treat our results accordingly.
The polarisation of the T cell response in hookworm infection is of some debate, with some studies showing a mixed Th1/Th2 response, while others report only a polarised Th2 response [12], [26]. These conflicting results might be explained by differences in methods used to assess cytokine levels and antigen preparation [26]. We found a robust Th2 response produced to hookworm antigen as expected, with some evidence of a systemic, but not mucosal hookworm-specific Th1 response. Using qPCR with unstimulated biopsies taken before and after hookworm infection, we showed upregulation of IFN-γ transcripts. However, restimulation of post-infection biopsies with NaES did not result in increased IFN-γ production. Thus, although an innate IFN-γ response develops after hookworm infection, we could not identify antigen-specific memory Th1 cells in the duodenal mucosa.
We did not detect a significant alteration of levels of mRNAs encoded by the Th17 cytokine IL-17A or transcription factor RORγt in PBMCs or biopsies. This is surprising, as we observed increased levels of ALDH1A2 and IL-15 mRNAs in unstimulated mucosa with further enhancement of IL-15 mRNA accumulation following stimulation with NaES. Although retinaldehyde dehydrogenase (encoded by ALDH1A2) produces the normally immunosuppressive retinoic acid, which imprints gut homing on T cells [27] and switches the pro-inflammatory Th17 to a regulatory response [28], in active celiac disease the impact appears quite the opposite whereby elevated retinoic acid and IL-15 promotes Th1/17 responses in the gut mucosa [29]. We did not detect an increase in Treg markers in response to hookworm infection in this study, or when previously measured by FACS and immunohistochemistry [22], despite a wealth of evidence of Treg induction following experimental helminth infections and administration of ES proteins in mouse models [30]–[32], and naturally acquired infections of humans with other helminths [33], [34].
In active celiac disease, IL-15 is considered a crucial cytokine in maintaining autoimmune (Th1/Th17) pathology, a relationship now recognized somewhat incongruously as being dependent on retinoic acid [29]. In isolation, our IL-15 and ALDH1A2 data would argue against the potential for hookworm infection to protect against gluten toxicity in celiac disease, the primary incentive for undertaking this clinical trial [21], [22]. However, in contrast to the increased accumulation of IL-2, IL-15 and ALDH1A2, accumulation of mRNA encoding the innate Th17-inducing and stabilising IL-23 was potently suppressed by hookworm infection, potentially neutralising the impact of these Th17 promoting cytokines. Consistent with suppression of IL-23 mRNA accumulation, Th17 inflammation did not occur. IL-23 is produced by antigen presenting cells under the influence of microbial signals, and is a key cytokine in driving intestinal inflammation [35]. Moreover, IL-23 was recently shown to induce production of pro-inflammatory cytokines by innate lymphoid cells in the gut of patients with Crohn's disease [36]. Thus we hypothesise that hookworm infection suppresses pro-inflammatory cytokine production (such as IL-23) by innate cells in the gut, similarly to that seen in H. polygyrus infection in mice where a suppressive dendritic cell subset is expanded in the mucosa [37], and ES proteins from the parasite suppress activation of these cells and subsequent cytokine production [38].
IL-22, an IL-23 dependent Th17 cytokine, acts via the IL-22R expressed on intestinal epithelial cells, promoting innate immunity against bacteria, cell regeneration and tissue healing. In inflammatory bowel disease, high levels of IL-22 are present in inflamed tissue [39]. Interestingly, Broadhurst et al. described a case study of a patient with ulcerative colitis who deliberately ingested thousands of eggs of the whipworm Trichuris trichuria in which infection ameliorated disease activity, and this effect correlated with increased expression of Th2 cytokines and IL-22 [23]. In our study, biopsies from patients infected with a small number of N. americanus larvae showed upregulation of IL-22 mRNA levels after restimulation with NaES in vitro. It is beyond the scope of this discussion to attempt to define what cytokine milieu determines when and what Th17 complex drives inflammation or regulation. It does seem, however, that helminth-stimulated IL-22, perhaps derived from a non-Th17 source, such as NK cells or CD11c+ cells, contributes to the biological relationship between parasite and host, whilst conditioning and promoting a less inflammatory phenotype [23], [40], [41].
Both the regulatory cytokines, TGF-β and IL-10, were induced by hookworm infection, but this was only evident in mucosa restimulated with NaES. During H. polygyrus infection in mice, Th2 responses are induced in lamina propria T cells, and Th1 responses in these T cells are inhibited by parasite-induced TGF-β - and IL-10-producing T cells [42]. We may have identified a similar regulatory process, possibly adapted to further fine tune Th2 associated damage at the hookworm attachment site. If the rate of progression and the severity of damage to the mucosa accompanying the worm's attachment is central to determining which population of parasites a particular host will sustain, as has been suggested in an earlier endoscopic study of N. americanus survival in experimentally infected humans [3], these inflammation-modifying cytokines almost certainly have a role.
Herein we characterised the systemic and mucosal immune responses to an anthropophilic hookworm infection. As expected, we detected a systemic and mucosal hookworm-specific Th2 response in experimentally infected people. Our data indicate that although an antigen-specific Th1 response was detectable in the blood, no antigen-specific IFN-γ was detectable in the mucosa. Therefore the increased IFN-γ we detected in the mucosa most likely comes from an innate source, possibly NK cells [24]. Despite enhanced production of IL-15 and ALDH1A2, levels of IL-23 were dramatically suppressed after hookworm infection, possibly accounting for the absence of a Th17 response via suppression of antigen presenting cell function.
Supporting Information
Zdroje
1. HotezPJBrookerSBethonyJMBottazziMELoukasA 2004 Hookworm infection. N Engl J Med 351 799 807
2. HotezPJBethonyJMDiemertDJPearsonMLoukasA 2010 Developing vaccines to combat hookworm infection and intestinal schistosomiasis. Nat Rev Microbiol 8 814 826
3. CroeseJO'NeilJMassonJCookeSMelroseW 2006 A proof of concept study establishing Necator americanus in Crohn's patients and reservoir donors. Gut 55 136 137
4. BlountDHooiDFearyJVennATelfordG 2009 Immunologic profiles of persons recruited for a randomized, placebo-controlled clinical trial of hookworm infection. Am J Trop Med Hyg 81 911 916
5. FearyJVennABrownAHooiDFalconeFH 2009 Safety of hookworm infection in individuals with measurable airway responsiveness: a randomized placebo-controlled feasibility study. Clin Exp Allergy 39 1060 1068
6. BethonyJBrookerSAlbonicoMGeigerSMLoukasA 2006 Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet 367 1521 1532
7. LoukasAConstantSLBethonyJM 2005 Immunobiology of hookworm infection. FEMS Immunol Med Microbiol 43 115 124
8. QuinnellRJPritchardDIRaikoABrownAPShawMA 2004 Immune responses in human necatoriasis: association between interleukin-5 responses and resistance to reinfection. J Infect Dis 190 430 438
9. BethonyJLoukasASmoutMBrookerSMendezS 2005 Antibodies against a secreted protein from hookworm larvae reduce the intensity of hookworm infection in humans and vaccinated laboratory animals. FASEB J 19 1743 1745
10. MaxwellCHussainRNutmanTBPoindexterRWLittleMD 1987 The clinical and immunologic responses of normal human volunteers to low dose hookworm (Necator americanus) infection. Am J Trop Med Hyg 37 126 134
11. GeigerSMFujiwaraRTSantiagoHCorrea-OliveiraRBethonyJM 2008 Early stage-specific immune responses in primary experimental human hookworm infection. Microbes Infect 10 1524 1535
12. WrightVBickleQ 2005 Immune responses following experimental human hookworm infection. Clin Exp Immunol 142 398 403
13. BarnerMMohrsMBrombacherFKopfM 1998 Differences between IL-4R alpha-deficient and IL-4-deficient mice reveal a role for IL-13 in the regulation of Th2 responses. Curr Biol 8 669 672
14. UrbanJFJrNoben-TrauthNDonaldsonDDMaddenKBMorrisSC 1998 IL-13, IL-4Ralpha, and Stat6 are required for the expulsion of the gastrointestinal nematode parasite Nippostrongylus brasiliensis. Immunity 8 255 264
15. AnthonyRMRutitzkyLIUrbanJFJrStadeckerMJGauseWC 2007 Protective immune mechanisms in helminth infection. Nat Rev Immunol 7 975 987
16. UrbanJFJrNoben-TrauthNSchopfLMaddenKBFinkelmanFD 2001 Cutting edge: IL-4 receptor expression by non-bone marrow-derived cells is required to expel gastrointestinal nematode parasites. J Immunol 167 6078 6081
17. MaddenKBYeungKAZhaoAGauseWCFinkelmanFD 2004 Enteric nematodes induce stereotypic STAT6-dependent alterations in intestinal epithelial cell function. J Immunol 172 5616 5621
18. HoffmannKFCheeverAWWynnTA 2000 IL-10 and the dangers of immune polarization: excessive type 1 and type 2 cytokine responses induce distinct forms of lethal immunopathology in murine schistosomiasis. J Immunol 164 6406 6416
19. RutitzkyLILopes da RosaJRStadeckerMJ 2005 Severe CD4 T cell-mediated immunopathology in murine schistosomiasis is dependent on IL-12p40 and correlates with high levels of IL-17. J Immunol 175 3920 3926
20. ElliottDEMetwaliALeungJSetiawanTBlumAM 2008 Colonization with Heligmosomoides polygyrus suppresses mucosal IL-17 production. J Immunol 181 2414 2419
21. DavesonAJJonesDMGazeSMcSorleyHCloustonA 2011 Effect of hookworm infection on wheat challenge in celiac disease–a randomised double-blinded placebo controlled trial. PLoS One 6 e17366
22. McSorleyHGazeSDavesonAJJonesDMAndersonR 2011 Suppression of inflammatory immune responses in celiac disease by experimental hookworm infection. PLoS One 6 e24092
23. BroadhurstMJLeungJMKashyapVMcCuneJMMahadevanU 2010 IL-22+ CD4+ T cells are associated with therapeutic Trichuris trichiura infection in an ulcerative colitis patient. Sci Transl Med 2 60ra88
24. HsiehGCLoukasAWahlAMBhatiaMWangY 2004 A secreted protein from the human hookworm necator americanus binds selectively to NK cells and induces IFN-gamma production. J Immunol 173 2699 2704
25. AidaYPabstMJ 1990 Removal of endotoxin from protein solutions by phase separation using Triton X-114. J Immunol Methods 132 191 195
26. McSorleyHJLoukasA 2010 The immunology of human hookworm infections. Parasite Immunol 32 549 559
27. IwataMHirakiyamaAEshimaYKagechikaHKatoC 2004 Retinoic acid imprints gut-homing specificity on T cells. Immunity 21 527 538
28. MucidaDParkYKimGTurovskayaOScottI 2007 Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science 317 256 260
29. DePaoloRWAbadieVTangFFehlner-PeachHHallJA 2011 Co-adjuvant effects of retinoic acid and IL-15 induce inflammatory immunity to dietary antigens. Nature 471 220 224
30. CuellarCWuWMendezS 2009 The hookworm tissue inhibitor of metalloproteases (Ac-TMP-1) modifies dendritic cell function and induces generation of CD4 and CD8 suppressor T cells. PLoS Negl Trop Dis 3 e439
31. FinneyCATaylorMDWilsonMSMaizelsRM 2007 Expansion and activation of CD4(+)CD25(+) regulatory T cells in Heligmosomoides polygyrus infection. Eur J Immunol 37 1874 1886
32. ElliottDESetiawanTMetwaliABlumAUrbanJFJr 2004 Heligmosomoides polygyrus inhibits established colitis in IL-10-deficient mice. Eur J Immunol 34 2690 2698
33. NauschNMidziNMduluzaTMaizelsRMMutapiF 2011 Regulatory and activated T cells in human Schistosoma haematobium infections. PLoS One 6 e16860
34. MetenouSDembeleBKonateSDoloHCoulibalySY 2010 At homeostasis filarial infections have expanded adaptive T regulatory but not classical Th2 cells. J Immunol 184 5375 5382
35. UhligHHMcKenzieBSHueSThompsonCJoyce-ShaikhB 2006 Differential activity of IL-12 and IL-23 in mucosal and systemic innate immune pathology. Immunity 25 309 318
36. GeremiaAArancibia-CarcamoCVFlemingMPRustNSinghB 2011 IL-23-responsive innate lymphoid cells are increased in inflammatory bowel disease. J Exp Med 208 1127 1133
37. MaizelsRMHewitsonJPMurrayJHarcusYMDayerB 2011 Immune modulation and modulators in Heligmosomoides polygyrus infection. Exp Parasitol. Aug 22. [Epub ahead of print]
38. SeguraMSuZPiccirilloCStevensonMM 2007 Impairment of dendritic cell function by excretory-secretory products: a potential mechanism for nematode-induced immunosuppression. Eur J Immunol 37 1887 1904
39. SarraMPalloneFMacdonaldTTMonteleoneG 2010 IL-23/IL-17 axis in IBD. Inflamm Bowel Dis 16 1808 1813
40. GibsonPRMuirJG 2005 Reinforcing the mucus: a new therapeutic approach for ulcerative colitis? Gut 54 900 903
41. ZenewiczLAYancopoulosGDValenzuelaDMMurphyAJStevensS 2008 Innate and adaptive interleukin-22 protects mice from inflammatory bowel disease. Immunity 29 947 957
42. InceMNElliottDESetiawanTMetwaliABlumA 2009 Role of T cell TGF-beta signaling in intestinal cytokine responses and helminthic immune modulation. Eur J Immunol 39 1870 1878
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2012 Číslo 2- Stillova choroba: vzácné a závažné systémové onemocnění
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
- Diagnostika virových hepatitid v kostce – zorientujte se (nejen) v sérologii
- Choroby jater v ordinaci praktického lékaře – význam jaterních testů
- Infekční komplikace virových respiračních infekcí – sekundární bakteriální a aspergilové pneumonie
-
Všechny články tohoto čísla
- Mechanisms of Pathogenesis, Infective Dose and Virulence in Human Parasites
- Structural and Functional Insights into the Pilotin-Secretin Complex of the Type II Secretion System
- Characterising the Mucosal and Systemic Immune Responses to Experimental Human Hookworm Infection
- Population Genetic Analyses Reveal the African Origin and Strain Variation of var.
- How Do Microbial Pathogens Make s?
- Substance P Causes Seizures in Neurocysticercosis
- Phagosomal Rupture by Results in Toxicity and Host Cell Death
- Absence of HIV-1 Evolution in the Gut-Associated Lymphoid Tissue from Patients on Combination Antiviral Therapy Initiated during Primary Infection
- Five Questions about Viral Trafficking in Neurons
- Selecting an Invertebrate Model Host for the Study of Fungal Pathogenesis
- A Co-Opted DEAD-Box RNA Helicase Enhances Tombusvirus Plus-Strand Synthesis
- Biochemical Properties of Highly Neuroinvasive Prion Strains
- ClpP1 and ClpP2 Function Together in Protein Degradation and Are Required for Viability and During Infection
- Discrete Cyclic di-GMP-Dependent Control of Bacterial Predation versus Axenic Growth in
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Discrete Cyclic di-GMP-Dependent Control of Bacterial Predation versus Axenic Growth in
- Characterising the Mucosal and Systemic Immune Responses to Experimental Human Hookworm Infection
- How Do Microbial Pathogens Make s?
- Substance P Causes Seizures in Neurocysticercosis
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



