-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Challenges and opportunities in understanding dementia and delirium in the acute hospital
In an Essay, Andrew Jackson and colleagues discuss challenges in the diagnosis and management of older people with dementia and delirium in acute hospitals.
Published in the journal: . PLoS Med 14(3): e32767. doi:10.1371/journal.pmed.1002247
Category: Essay
doi: https://doi.org/10.1371/journal.pmed.1002247Summary
In an Essay, Andrew Jackson and colleagues discuss challenges in the diagnosis and management of older people with dementia and delirium in acute hospitals.
Summary points
Dementia in acute hospitals is common and associated with poor health outcomes.
Dementia in acute hospitals is intricately linked with delirium, and the two should always be considered together when developing future policy.
The decline in health and function after hospitalization among people with dementia may be influenced by discrete disease processes but also by the hospital environment and care itself.
Opportunities for further research into the specific acute hospital management of dementia and its complications are many.
What is the problem?
Dementia in general hospitals
Dementia is very common in patients admitted to acute hospitals, affecting one in four patients, with 6% of people living with dementia being inpatients in acute hospitals at any given time [1,2]. Dementia is often unrecognised by doctors and other hospital staff and frequently complicated by delirium. Deficiencies in care have been highlighted by national audit and numerous reports [3].
“Intellectual failure” is recognised as one of the “geriatric giants.” Both delirium and dementia are disorders of cognitive function, are associated with adverse health outcomes, and are intricately linked [4]. Understanding how to assess, manage, and follow up older people with cognitive impairment in hospitals is vital to improving their care.
This essay discusses the clinical manifestation and complications of delirium and dementia in acute hospitals. Diagnosis of both conditions can be uncertain, and treatments are limited, but effective actions and management may improve outcomes. We also highlight areas for future research and suggest policy interventions to improve hospital care.
Prevalence, presentation, and recognition
Estimates of the prevalence of dementia in hospitals vary across published studies [5] but range between 15% to 42% [6–10]. To put this in context, if two-thirds of hospital bed-days are in people over 65 years of age, then 25% of people in general hospitals will have dementia. However, published reports vary in ascertainment method and whether they distinguish between delirium and dementia.
People with dementia and cognitive impairment are hospitalised for many reasons, but typically in crises. Admission problems include immobility (73%), falls (64%), pain (54%), and breathlessness (23%) [11]. Patients in hospital with dementia are 4 to 7 years older, more likely to be women, and more likely to live in a care home than those without dementia [5]. Three-quarters of hospitalised patients with dementia have been defined as frail, compared to one-quarter of similar people without dementia [7].
Although dementia prevalence is high, the proportion undiagnosed or unrecognised by health care staff is approximately 56% (data in S1 Table) [6–8,12]. In older patients with delirium, only 36% of those with dementia had a recognised diagnosis [13]. Extrapolating these figures to a typical 500-bed general hospital suggests there would be at least 70 inpatients with unrecognised dementia at any one time.
Severity
Hospitalised people with dementia typically have more advanced disease than those in the community. A Functional Assessment Staging Scale (FAST) stage of 6d (nearly mute, immobile, and incontinent) or above is present in 46% of hospitalised patients with dementia [14]. Three-quarters of patients with dementia in hospital had behavioural and psychological symptoms of dementia (BPSDs), and 43% had symptoms that challenged the staff involved [14]. These rates are much higher than would be expected in a general population with dementia in community settings. Patients with dementia in hospital also have a lower quality of life [15]. BPSDs in hospitals are often treated pharmacologically with antipsychotic drugs or benzodiazepines, which is associated with a nearly 3-fold increased risk of hospital mortality [16].
Adverse outcomes
Dementia in general hospitals is associated with more inpatient adverse events, principally mortality, falls, and delirium [17], with increased costs of care [18]. Studies suggest a mortality rate of 31% at 6 months and 40% at 12 months, with a large increase in care-home residence at 12 months [19]; of the patients studied, 24% were new institutionalisations, and 42% were readmissions [20]. Even abnormal scores on single tests (either the Mini-Mental State examination or the Clock Drawing Test) were associated with mortality at 1 year (hazard ratio [HR] 2.9 [95% CI 1.3–6.4]) [21].
The worst outcomes seen in people with dementia may be avoidable if they are due to poorer standards of care provision. Hospital staff can struggle to meet the complex care needs of people with dementia, often leading to a negative perception of such patients [22]. Iatrogenic and/or hospital environmental factors may lead to significant harm, and the inpatient care of people with dementia could be seen as a quality indicator for hospitals (as cited in the United Kingdom Francis report). However, biological factors also impact upon outcomes. It has been hypothesized that the interaction of an acute inflammatory event may accelerate functional and cognitive decline in this vulnerable population (as shown in Fig 1). Research to understand these mechanisms and to develop intervention strategies to minimise these outcomes is urgently needed. S2 Table summarises key studies presented above.
Fig. 1. Schematic representation of dementia disease trajectory over time influenced by hospital admission. 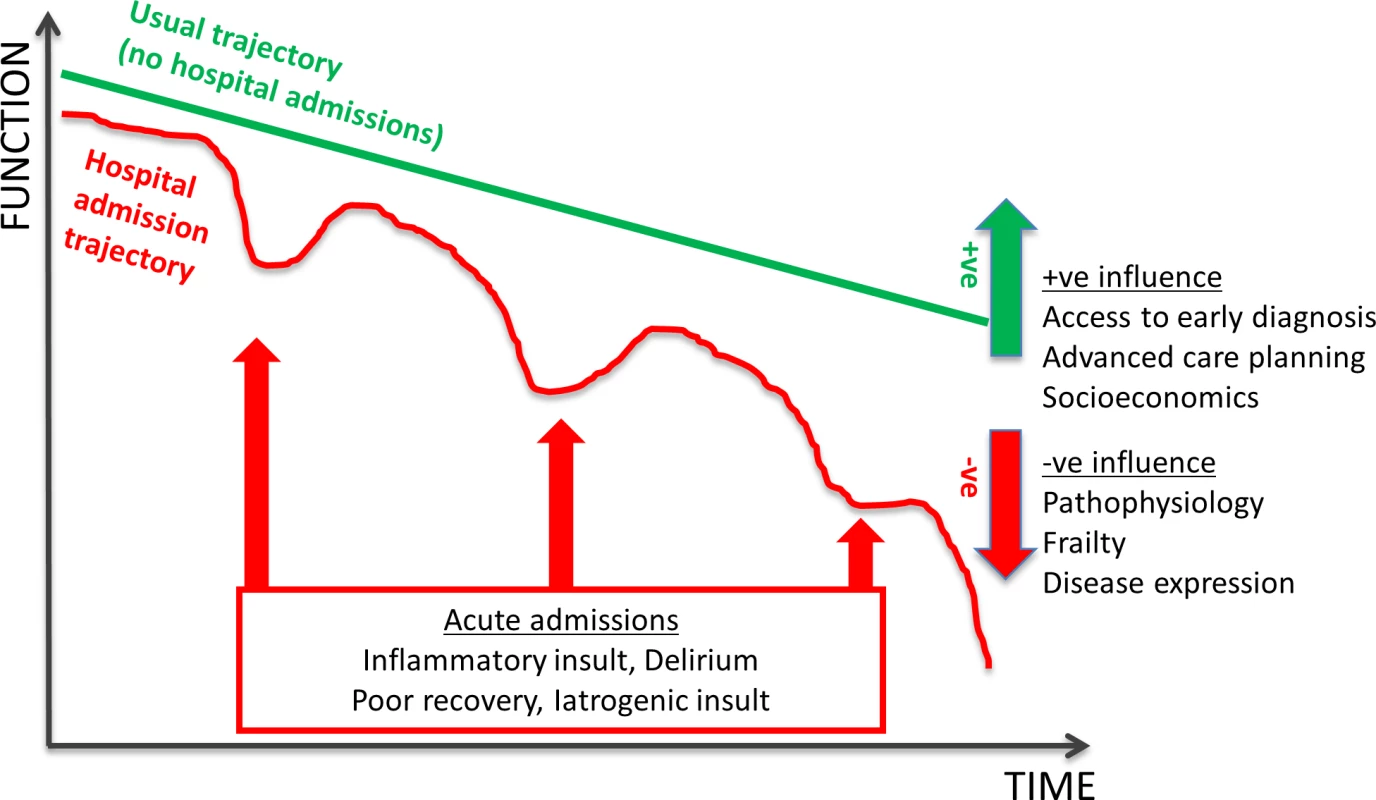
Dementia disease trajectories between a person with no hospital admissions (green line) and multiple hospital admissions (red line) are illustrated. The disease trajectory is negatively influenced by baseline frailty and disease expression. However, it may be positively tempered by early diagnosis, leading to better access to services, and advanced care planning. The “multiple hospital admissions” trajectory is further influenced by specific hospital interactions—importantly, delirium—but there are other effects from an acute inflammatory insult, subsequent recovery, and in-hospital iatrogenic insults. Impact of delirium on older people in hospital with dementia
Delirium is an acute, severe neuropsychiatric syndrome seen mainly in older people in hospital and associated with increased morbidity and mortality [23]. Dementia is the strongest risk factor for developing delirium [24], with delirium superimposed on dementia accounting for 65% of delirium cases in hospital [25]. Delirium is associated with worsening of dementia and is a risk factor for subsequent dementia [26,27], with only 19% of people with delirium free from cognitive deficits 3 months later [13]. Those with dementia and delirium have the poorest outcomes [28]. In the context of the acute general hospital, dementia and delirium are intricately linked, and it is difficult to effectively recognise, investigate, manage, and suggest policy about one without the other, although the UK National Dementia Strategy only briefly mentioned delirium [29].
Delirium Superimposed on Dementia (DSD)
The diagnostic challenge in an older person presenting with “confusion” is to disentangle whether they have delirium, dementia, or both. Persistent delirium is also possible [30]. Delirium in people with dementia is especially likely to go unrecognised [31]. There is a major need for better fundamental research to characterise these conditions biologically and clinically to improve care. However, although no simple diagnostic criteria exist, there are clinical processes that enable accurate diagnosis.
Diagnosing delirium in people with dementia
Arousal and alertness are usually abnormal in delirium, but these domains are also increasingly affected in severe dementia. Diagnosing delirium in a person with dementia requires competence in cognitive testing, mental state examination, and informant questioning. Few screening tests have tried to detect delirium in the context of dementia; the Confusion Assessment Method (CAM) and the 4AT are examples [25,32].
There are four core challenges when diagnosing delirium in dementia. First, dementia with Lewy bodies (DLB) causes around 4% of all cases of dementia [33] and typically presents with a more rapid onset and with fluctuating degrees of cognitive impairments, attentional deficits, visual hallucinations, and paranoid delusions. This presentation may be similar to delirium, especially persistent delirium. Secondly, the impact of the hospital environment and sleep deprivation can lead to sleepiness by day, irritability, and behavioural “challenge” even in the absence of delirium. Thirdly, the progression of vascular dementia can deteriorate suddenly. Fourthly, BPSDs in dementia, typically including altered arousal, hallucinations, and agitation, are present in 75% of people with dementia in hospital [14]. However, given the seriousness of delirium, best practice is to assume delirium and manage as such until proven otherwise.
Diagnosing dementia in people with delirium
By definition, manifestations of delirium follow an acute and fluctuating course; therefore, traditional tools to detect dementia by measuring cognitive deficits assumed to be stable are not useful. Many tools available to detect dementia in hospitals have not been validated in patients with delirium [34]. Obtaining information about baseline premorbid cognition from an informant is critical, but this requires attention and skill and is often badly done. The Informant Questionnaire of Cognitive Decline in the Elderly short form (IQCODE-SF) and the AD8: The Washington University Dementia Screening Test (AD8) have been validated to detect pre-existing dementia in older people with delirium [35]. Defining the duration of delirium is difficult, and current health services are rarely configured to review cognition after an acute episode.
What is the solution?
Management of people with dementia in hospital
Despite the clear need, little research is available on how best to provide care. The patient and carer experience of care is often negative, with deterioration in health, perceived poor care, and unrealistic expectations cited [36,37]. However, outcomes in dementia can be improved. For example, comprehensive geriatric assessment of patients with hip fracture and dementia leads to better functional mobility [38]. In-hospital fall prevention strategies can reduce falls, including in those with cognitive impairment [39]. Delirium prevention strategies have shown a reduction in delirium and falls [40]. Research specifically in delirium prevention for dementia populations is scarce [41]; however, it is reasonable to assume a general effect that extends to people with dementia.
Evidence to inform nutritional support [42] and specific therapy interventions related to discharge planning are lacking but may be crucial to provide patients with the best chance to be discharged home, as opposed to inappropriate institutionalisation. Engaging and listening to families is vital to ensure appropriate discharge planning at an early stage [43]. Families can also be enabled to recognize delirium in people with dementia, as well as to ensure recognition of its resolution or lack thereof, during the inpatient stay.
Joint units with geriatric medicine and psychiatry may reduce length of stay and readmissions [44]. One randomised controlled trial of a specialist unit for older patients admitted to hospital with confusion found no impact on length of stay or institutionalisation when compared with usual care but did show improvements in care interactions, carer satisfaction, and cost-effectiveness [45,46]. Efforts to improve care are hampered by the lack of specific treatments for delirium with dementia, either pharmacological or nonpharmacological.
Managing undifferentiated cognitive impairment in hospital
The typical approach to manage cognitive impairment has been to attempt to diagnose delirium, dementia, both, or something else. There is a case for recognising these in-hospital conditions as a complex discrete syndrome, not least because some aspects of management are the same whatever the underlying diagnosis may be [47]. Undifferentiated cognitive impairment management includes treating patients as if they have delirium and possibly dementia. Unless the history is very clear, this should involve detailed characterisation of symptoms and impairments without necessarily giving a label, performed as part of comprehensive geriatric assessment. Therefore, management can be need driven, rather than diagnosis driven.
What needs to happen next?
Assessing cognitive impairment, adverse events risk, and BPSDs should become routine. Delirium prevention, active management of underlying precipitants, and a patient safety approach to minimise harms are especially important [48]. Hospital care requires appropriate environmental adjustments (colour, light, visual interest, orientation, and furniture) and processes (person-centred care, attention to meals, activity, and sleep promotion), delivered by increased and upskilled staff. Proper attention should be given to legal aspects, especially around consent, and to risk enablement [49]. The recent interdisciplinary collaboration between the American Delirium Society and the American Nurses Association is an example of moving this evidence into practice [50]. Delirium and dementia patients will be slower to recover, and return to home living should be based on “adaptive” rather than “restorative” rehabilitation.
Dementia is a long-term condition for which the aim is to “live well.” Given that outcomes after hospitalisation are poor, an acute hospital admission should trigger a palliative needs assessment with discussions about goals and expectations of treatments, as part of a shared decision-making process. These discussions are time consuming and difficult in the face of uncertainty but reflect best practice.
There is a dearth of treatments for dementia and delirium and as yet no reliable and meaningful biomarkers to guide management. Evidence is lacking on how best to incorporate carers into hospital care as well as how to best train a fit-for-purpose workforce [51]. Assistive technology may in the future enhance dementia care [52], and further trials of specialized units are needed. However, any trials would need to be carefully designed with outcomes that are important to very physically and cognitively frail people, half of whom are in the last year of life.
Conclusions
Despite challenges, the proactive diagnosis of dementia and delirium in hospitals is likely to improve patient experience and outcomes. Because cognitive impairment is so common in hospitals and impacts so substantially on long-term outcomes, there is a pressing need for (1) joined-up care to alter a trajectory of decline and (2) more research to improve diagnostics and management, whatever the specific underlying diagnosis.
Supporting Information
Zdroje
1. Alzheimer's Society. Counting the cost: Caring for people with dementia on hospital wards. London, UK: 2009.
2. Briggs R, Coary R, Collins R, Coughlan T, O'Neill D, Kennelly SP. Acute hospital care: how much activity is attributable to caring for patients with dementia? QJM. 2016;109(1):41–4. doi: 10.1093/qjmed/hcv085 25956392
3. Royal College of Psychiatrists. Who Care's Wins: Improving the outcome for older people admitted to the general hospital. London: Faculty of Old Age Psychiatry, Royal College of Psychiatrists, 2005.
4. Fong TG, Davis D, Growdon ME, Albuquerque A, Inouye SK. The interface between delirium and dementia in elderly adults. The Lancet Neurology. 2015;14(8):823–32. doi: 10.1016/S1474-4422(15)00101-5 26139023
5. Mukadam N, Sampson EL. A systematic review of the prevalence, associations and outcomes of dementia in older general hospital inpatients. Int Psychogeriatr. 2011;23(3):344–55. doi: 10.1017/S1041610210001717 20716393
6. Sampson EL, Blanchard MR, Jones L, Tookman A, King M. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry. 2009;195(1):61–6. doi: 10.1192/bjp.bp.108.055335 19567898
7. Briggs R, Dyer A, Nabeel S, Collins R, Doherty J, Coughlan T, et al. Dementia in the acute hospital: the prevalence and clinical outcomes of acutely unwell patients with dementia. QJM. 2016;110(1):33–37. doi: 10.1093/qjmed/hcw114 27486262
8. Travers C, Byrne G, Pachana N, Klein K, Gray L. Prospective observational study of dementia and delirium in the acute hospital setting. Intern Med J. 2013;43(3):262–9. doi: 10.1111/j.1445-5994.2012.02962.x 22998322
9. Nightingale S, Holmes J, Mason J, House A. Psychiatric illness and mortality after hip fracture. Lancet. 2001;357(9264):1264–5. doi: 10.1016/S0140-6736(00)04421-4 11418154
10. Crowther GJ, Bennett MI, Holmes JD. How well are the diagnosis and symptoms of dementia recorded in older patients admitted to hospital? Age Ageing. 2017; 46(1):112–118. doi: 10.1093/ageing/afw169 27614081
11. Glover A, Bradshaw LE, Watson N, Laithwaite E, Goldberg SE, Whittamore KH, et al. Diagnoses, problems and healthcare interventions amongst older people with an unscheduled hospital admission who have concurrent mental health problems: a prevalence study. BMC geriatrics. 2014;14 : 43. doi: 10.1186/1471-2318-14-43 24694034
12. Laurila JV, Pitkala KH, Strandberg TE, Tilvis RS. Detection and documentation of dementia and delirium in acute geriatric wards. Gen Hosp Psychiatry. 2004;26(1):31–5. 14757300
13. Jackson TA, MacLullich AM, Gladman JR, Lord JM, Sheehan B. Undiagnosed long-term cognitive impairment in acutely hospitalised older medical patients with delirium: a prospective cohort study. Age Ageing. 2016;45(4):493–9. doi: 10.1093/ageing/afw064 27076525
14. Sampson EL, White N, Leurent B, Scott S, Lord K, Round J, et al. Behavioural and psychiatric symptoms in people with dementia admitted to the acute hospital: prospective cohort study. Br J Psychiatry. 2014;205(3):189–96. doi: 10.1192/bjp.bp.113.130948 25061120
15. Sheehan BD, Lall R, Stinton C, Mitchell K, Gage H, Holland C, et al. Patient and proxy measurement of quality of life among general hospital in-patients with dementia. Aging & mental health. 2012;16(5):603–7.
16. White N, Leurent B, Lord K, Scott S, Jones L, Sampson EL. The management of behavioural and psychological symptoms of dementia in the acute general medical hospital: a longitudinal cohort study. Int J Geriatr Psychiatry. 2017; 32 : 297–305. doi: 10.1002/gps.4463
17. Mecocci P, von Strauss E, Cherubini A, Ercolani S, Mariani E, Senin U, et al. Cognitive impairment is the major risk factor for development of geriatric syndromes during hospitalization: results from the GIFA study. Dement Geriatr Cogn Disord. 2005;20(4):262–9. doi: 10.1159/000087440 16103670
18. Bail K, Goss J, Draper B, Berry H, Karmel R, Gibson D. The cost of hospital-acquired complications for older people with and without dementia; a retrospective cohort study. BMC health services research. 2015;15 : 91. doi: 10.1186/s12913-015-0743-1 25890030
19. Sheehan B, Lall R, Gage H, Holland C, Katz J, Mitchell K. A 12-month follow-up study of people with dementia referred to general hospital liaison psychiatry services. Age Ageing. 2013;42(6):786–90. doi: 10.1093/ageing/aft139 24166239
20. Bradshaw LE, Goldberg SE, Lewis SA, Whittamore K, Gladman JR, Jones RG, et al. Six-month outcomes following an emergency hospital admission for older adults with co-morbid mental health problems indicate complexity of care needs. Age Ageing. 2013;42(5):582–8. doi: 10.1093/ageing/aft074 23800454
21. Torisson G, Minthon L, Stavenow L, Londos E. Cognitive impairment is undetected in medical inpatients: a study of mortality and recognition amongst healthcare professionals. BMC geriatrics. 2012;12(1):47.
22. Tadd W, Hillman A, Calnan S, Calnan M, Bayer T, Read S. Right place—wrong person: dignity in the acute care of older people. Quality in Ageing and Older Adults. 2011;12(1):33–43.
23. Maclullich AM, Anand A, Davis DH, Jackson T, Barugh AJ, Hall RJ, et al. New horizons in the pathogenesis, assessment and management of delirium. Age Ageing. 2013;42(6):667–74. doi: 10.1093/ageing/aft148 24067500
24. Ahmed S, Leurent B, Sampson EL. Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age Ageing. 2014;43(3):326–33. doi: 10.1093/ageing/afu022 24610863
25. Morandi A, McCurley J, Vasilevskis EE, Fick DM, Bellelli G, Lee P, et al. Tools to detect delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2012;60(11):2005–13. doi: 10.1111/j.1532-5415.2012.04199.x 23039270
26. Davis DH, Muniz Terrera G, Keage H, Rahkonen T, Oinas M, Matthews FE, et al. Delirium is a strong risk factor for dementia in the oldest-old: a population-based cohort study. Brain. 2012;135(Pt 9):2809–16. doi: 10.1093/brain/aws190 22879644
27. Davis DJ, Muniz-Terrera G, Keage HD, Stephan BC, Fleming J, Ince PG, et al. Association of delirium with cognitive decline in late life: A neuropathologic study of 3 population-based cohort studies. JAMA Psychiatry. Published online January 18, 2017. doi: 10.1001/jamapsychiatry.2016.3423
28. Jackson TA, Wilson D, Richardson S, Lord JM. Predicting outcome in older hospital patients with delirium: a systematic literature review. Int J Geriatr Psychiatry. 2016;31(4):392–9. doi: 10.1002/gps.4344 26302258
29. Burns A, Robert P. The National Dementia strategy in England. BMJ. 2009;338:b931. doi: 10.1136/bmj.b931 19276132
30. Cole MG. Persistent delirium in older hospital patients. Current opinion in psychiatry. 2010;23(3):250–4. doi: 10.1097/YCO.0b013e32833861f6 20224406
31. Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002;50(10):1723–32. 12366629
32. Bellelli G, Morandi A, Davis DH, Mazzola P, Turco R, Gentile S, et al. Validation of the 4AT, a new instrument for rapid delirium screening: a study in 234 hospitalised older people. Age Ageing. 2014;43(4):496–502. doi: 10.1093/ageing/afu021 24590568
33. Vann Jones SA, O'Brien JT. The prevalence and incidence of dementia with Lewy bodies: a systematic review of population and clinical studies. Psychol Med. 2014;44(4):673–83. doi: 10.1017/S0033291713000494 23521899
34. Jackson TA, Naqvi SH, Sheehan B. Screening for dementia in general hospital inpatients: a systematic review and meta-analysis of available instruments. Age Ageing. 2013;42(6):689–95. doi: 10.1093/ageing/aft145 24100618
35. Jackson TA, MacLullich AM, Gladman JR, Lord JM, Sheehan B. Diagnostic test accuracy of informant-based tools to diagnose dementia in older hospital patients with delirium: a prospective cohort study. Age Ageing. 2016;45(4):505–11. doi: 10.1093/ageing/afw065 27076526
36. Porock D, Clissett P, Harwood RH, Gladman JR. Disruption, control and coping: responses of and to the person with dementia in hospital. Ageing Soc. 2015;35(1):37–63. doi: 10.1017/S0144686X13000561 25878366
37. Jurgens FJ, Clissett P, Gladman JR, Harwood RH. Why are family carers of people with dementia dissatisfied with general hospital care? A qualitative study. BMC geriatrics. 2012;12(1):57.
38. Prestmo A, Saltvedt I, Helbostad JL, Taraldsen K, Thingstad P, Lydersen S, et al. Who benefits from orthogeriatric treatment? Results from the Trondheim hip-fracture trial. BMC geriatrics. 2016;16 : 49. doi: 10.1186/s12877-016-0218-1 26895846
39. Oliver D, Connelly JB, Victor CR, Shaw FE, Whitehead A, Genc Y, et al. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ. 2007;334(7584):82. doi: 10.1136/bmj.39049.706493.55 17158580
40. Hshieh TT, Yue J, Oh E, Puelle M, Dowal S, Travison T, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175(4):512–20. doi: 10.1001/jamainternmed.2014.7779 25643002
41. Siddiqi N, Harrison JK, Clegg A, Teale EA, Young J, Taylor J, et al. Interventions for preventing delirium in hospitalised non-ICU patients. The Cochrane database of systematic reviews. 2016;3(3):CD005563.
42. Abdelhamid A, Bunn D, Copley M, Cowap V, Dickinson A, Gray L, et al. Effectiveness of interventions to directly support food and drink intake in people with dementia: systematic review and meta-analysis. BMC geriatrics. 2016;16(1):26.
43. King BJ, Gilmore-Bykovskyi AL, Roiland RA, Polnaszek BE, Bowers BJ, Kind AJ. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc. 2013;61(7):1095–102. doi: 10.1111/jgs.12328 23731003
44. George J, Adamson J, Woodford H. Joint geriatric and psychiatric wards: a review of the literature. Age Ageing. 2011;40(5):543–8. doi: 10.1093/ageing/afr080 21784760
45. Goldberg SE, Bradshaw LE, Kearney FC, Russell C, Whittamore KH, Foster PER, et al. Care in specialist medical and mental health unit compared with standard care for older people with cognitive impairment admitted to general hospital: randomised controlled trial (NIHR TEAM trial). BMJ 2013;347:f4132. doi: 10.1136/bmj.f4132 23819964
46. Tanajewski L, Franklin M, Gkountouras G, Berdunov V, Harwood RH, Goldberg SE, et al. Economic Evaluation of a General Hospital Unit for Older People with Delirium and Dementia (TEAM Randomised Controlled Trial). PLoS ONE. 2015;10(12):e0140662. doi: 10.1371/journal.pone.0140662 26684872
47. Reynish E. O-093: Prevalence, mortality and readmission of people with dementia, delirium and other cognitive spectrum disorders in the general hospital. European Geriatric Medicine. 2015;6:S177–S8.
48. George J, Long S, Vincent C. How can we keep patients with dementia safe in our acute hospitals? A review of challenges and solutions. J R Soc Med. 2013;106(9):355–61. doi: 10.1177/0141076813476497 23759885
49. Manthorpe J, Moriarty J. Nothing ventured, nothing gained: risk guidance for people with dementia. Department of health, HMG. London: 2010.
50. American Nurses Association. Delirium: Prevent, Identify, Treat 2017. http://www.nursingworld.org/MainMenuCategories/ThePracticeofProfessionalNursing/Delirium.
51. Surr CA, Smith SJ, Crossland J, Robins J. Impact of a person-centred dementia care training programme on hospital staff attitudes, role efficacy and perceptions of caring for people with dementia: A repeated measures study. Int J Nurs Stud. 2016;53 : 144–51. doi: 10.1016/j.ijnurstu.2015.09.009 26421910
52. Fleming R, Sum S. Empirical studies on the effectiveness of assistive technology in the care of people with dementia: a systematic review. Journal of Assistive Technologies. 2014;8(1):14–34.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2017 Číslo 3- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Antikoagulační léčba u pacientů před operačními výkony
-
Všechny články tohoto čísla
- 2016 Reviewer and Editorial Board Thank You
- , , and mutations in early-onset Alzheimer disease: A genetic screening study of familial and sporadic cases
- Differential associations of plasma lipids with incident dementia and dementia subtypes in the 3C Study: A longitudinal, population-based prospective cohort study
- Mixed pathologies and neural reserve: Implications of complexity for Alzheimer disease drug discovery
- -related risk of mild cognitive impairment and dementia for prevention trials: An analysis of four cohorts
- Neuropathological diagnoses and clinical correlates in older adults in Brazil: A cross-sectional study
- Early diagnosis of mild cognitive impairment and mild dementia through basic and instrumental activities of daily living: Development of a new evaluation tool
- Potentially modifiable lifestyle factors, cognitive reserve, and cognitive function in later life: A cross-sectional study
- Association between fatty acid metabolism in the brain and Alzheimer disease neuropathology and cognitive performance: A nontargeted metabolomic study
- Fine-mapping of the human leukocyte antigen locus as a risk factor for Alzheimer disease: A case–control study
- What’s the “Take Home” from Research on Dementia Trends?
- Cultural representations of dementia
- Dementia and aging populations—A global priority for contextualized research and health policy
- Dementia in the oldest old: Beyond Alzheimer disease
- Rehabilitation for people living with dementia: A practical framework of positive support
- Dementia in low-income and middle-income countries: Different realities mandate tailored solutions
- Challenges and opportunities in understanding dementia and delirium in the acute hospital
- Dementia incidence trend over 1992-2014 in the Netherlands: Analysis of primary care data
- Association between delirium superimposed on dementia and mortality in hospitalized older adults: A prospective cohort study
- Development of an adaptive, personalized, and scalable dementia care program: Early findings from the Care Ecosystem
- Genetic assessment of age-associated Alzheimer disease risk: Development and validation of a polygenic hazard score
- Age-related cognitive decline and associations with sex, education and apolipoprotein E genotype across ethnocultural groups and geographic regions: a collaborative cohort study
- The impact of individual Cognitive Stimulation Therapy (iCST) on cognition, quality of life, caregiver health, and family relationships in dementia: A randomised controlled trial
- Effectiveness of an intervention to facilitate prompt referral to memory clinics in the United Kingdom: Cluster randomised controlled trial
- Subjective and objective cognitive function among older adults with a history of traumatic brain injury: A population-based cohort study
- Association of lifelong exposure to cognitive reserve-enhancing factors with dementia risk: A community-based cohort study
- Multimorbidity and healthcare utilization among home care clients with dementia in Ontario, Canada: A retrospective analysis of a population-based cohort
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Effectiveness of an intervention to facilitate prompt referral to memory clinics in the United Kingdom: Cluster randomised controlled trial
- , , and mutations in early-onset Alzheimer disease: A genetic screening study of familial and sporadic cases
- Challenges and opportunities in understanding dementia and delirium in the acute hospital
- Early diagnosis of mild cognitive impairment and mild dementia through basic and instrumental activities of daily living: Development of a new evaluation tool
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



