-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Why Are Some Population Interventions for Diet and Obesity More Equitable and Effective Than Others? The Role of Individual Agency
Jean Adams and colleagues argue that population interventions that require individuals to use a low level of agency to benefit are likely to be most effective and most equitable.
Published in the journal: . PLoS Med 13(4): e32767. doi:10.1371/journal.pmed.1001990
Category: Essay
doi: https://doi.org/10.1371/journal.pmed.1001990Summary
Jean Adams and colleagues argue that population interventions that require individuals to use a low level of agency to benefit are likely to be most effective and most equitable.
Summary Points
Public health interventions can be described according to where they lie on two continuums: the population and high-risk approaches anchor one continuum, while the other continuum captures the personal resources (or “agency”) individuals have to use to benefit from interventions.
Population interventions that require individuals to use a high level of agency to benefit tend to be favoured by governments around the world.
Population interventions that require individuals to use a low level of agency to benefit are likely to be most effective and most equitable. More effort is required to develop, evaluate, and implement population interventions that require low levels of agency for individuals to benefit.
We now find ourselves in a world in which one in three adults is overweight or obese [1]. Unhealthy diets are an important determinant of overweight and obesity and also contribute directly to a variety of other causes of disability and death. In fact, together with physical inactivity, dietary risk factors are responsible for 10% of disability-adjusted life years lost globally [2]. Like many risk factors, unhealthy diets are not evenly distributed in the population. In most developed countries, and increasingly in developing countries too, obesity and unhealthy diets are more common in more socioeconomically disadvantaged groups [3,4]. Socioeconomic inequalities in health and disease are at least partly due to these inequalities in diet and obesity.
Many governments have responded to the challenge of unhealthy diets and obesity with strategies that focus on advice, guidance, and encouragement to adopt healthier lifestyles. In England, the government’s current “flagship” obesity prevention programme is Change4Life. This social marketing campaign uses mass media and other avenues to inform and educate the public about the harms of excess weight and the benefits of being more active and eating more healthfully. Simple strategies for changing behaviour are also offered. Similar programmes operate elsewhere, including MangerBouger in France and Let’s Move in the United States.
The obvious assumption of these programmes is that advice, guidance, and encouragement will change the population’s diet and activity behaviours. We explore why this is unlikely to be the case and why such strategies are unlikely to reduce inequalities in diet and obesity. We propose a framework that captures a wider range of intervention strategies and discuss how these may be used to improve diet, reduce obesity, and tackle inequalities.
The Population and High-Risk Approaches to Prevention
Mass-media social marketing initiatives draw on Geoffrey Rose’s population approach to prevention [5]. This approach involves interventions that are delivered across the whole population, or whole population groups, without first identifying those at increased risk of disease. The aim of the population approach is to reduce risk factor levels by a small amount in everyone. In contrast, the high-risk approach identifies and targets those individuals at high risk of disease, aiming to reduce risk factors by a large amount in only these people. Rose argued that a greater overall benefit would be achieved by modest reductions in risk in many people than by large reductions in just a few people.
Unfortunately, not all population approaches are the same [6]. Population approaches that rely on individuals engaging with information are unlikely to achieve the full potential of Rose’s insights.
Population Interventions Differ in the Degree of “Agency” Individuals Must Use to Benefit
Population interventions like Change4Life that focus on providing advice, guidance, and encouragement rely heavily on individuals being able and motivated to engage with this advice, guidance, and encouragement. These types of interventions have been described as highly “agentic” [7,8]: recipients must use their personal resources, or “agency,” to benefit. The effectiveness and equity of these interventions has been questioned [7,8].
In contrast, population interventions that require recipients to use little or no agency to benefit may be more effective and equitable. When food manufacturers reduce the salt content of bread, decreased salt intake occurs without individuals having to consciously engage with any information or actively change their behaviour [9]. So-called “nudge” interventions are one class of lower agency interventions. In the context of changing health-related behaviours, “nudges” have been defined as changes to the placement or properties of objects at the microenvironmental level—for example, changing the placement of healthier options in a buffet [10]. Low-agency population interventions can operate at all levels and not just at the microenvironmental level.
The amount of agency individuals must use to benefit from an intervention is a fundamental determinant of how, and for whom, it will work.
Intervention “Agency” Influences Intervention Effectiveness and Equity
There is some evidence that high-agency population interventions are less effective, overall, than those that require less agency [7,11,12]. By reducing the need for individual decisions, there is less room in low-agency interventions for attrition at each of the many steps from intervention delivery to health outcome. For example, for an information leaflet encouraging women trying to conceive to take folic acid supplements (a high-agency population intervention) to have an effect, women must see and read the leaflet, understand the information presented, and then purchase and take supplements. Attrition might be expected at each of these steps. In contrast, if all commercial wheat flour is fortified with folic acid (a low-agency population intervention), one of the few, if only, steps at which attrition can occur is the decision to keep consuming products made with commercial wheat flour. This is illustrated schematically in Fig 1. There is also accumulating evidence that high-agency population interventions are likely to reinforce, or even worsen, socioeconomic inequalities in health [13–16]. For example, information campaigns about the importance of folic acid intake during pregnancy (a high-agency intervention) exacerbate socioeconomic inequalities in folate status more than supplementing food with folic acid (a low-agency intervention) [15].
Fig. 1. Illustration of the intervention pathway in low- (top) and high-agency (bottom) population interventions. 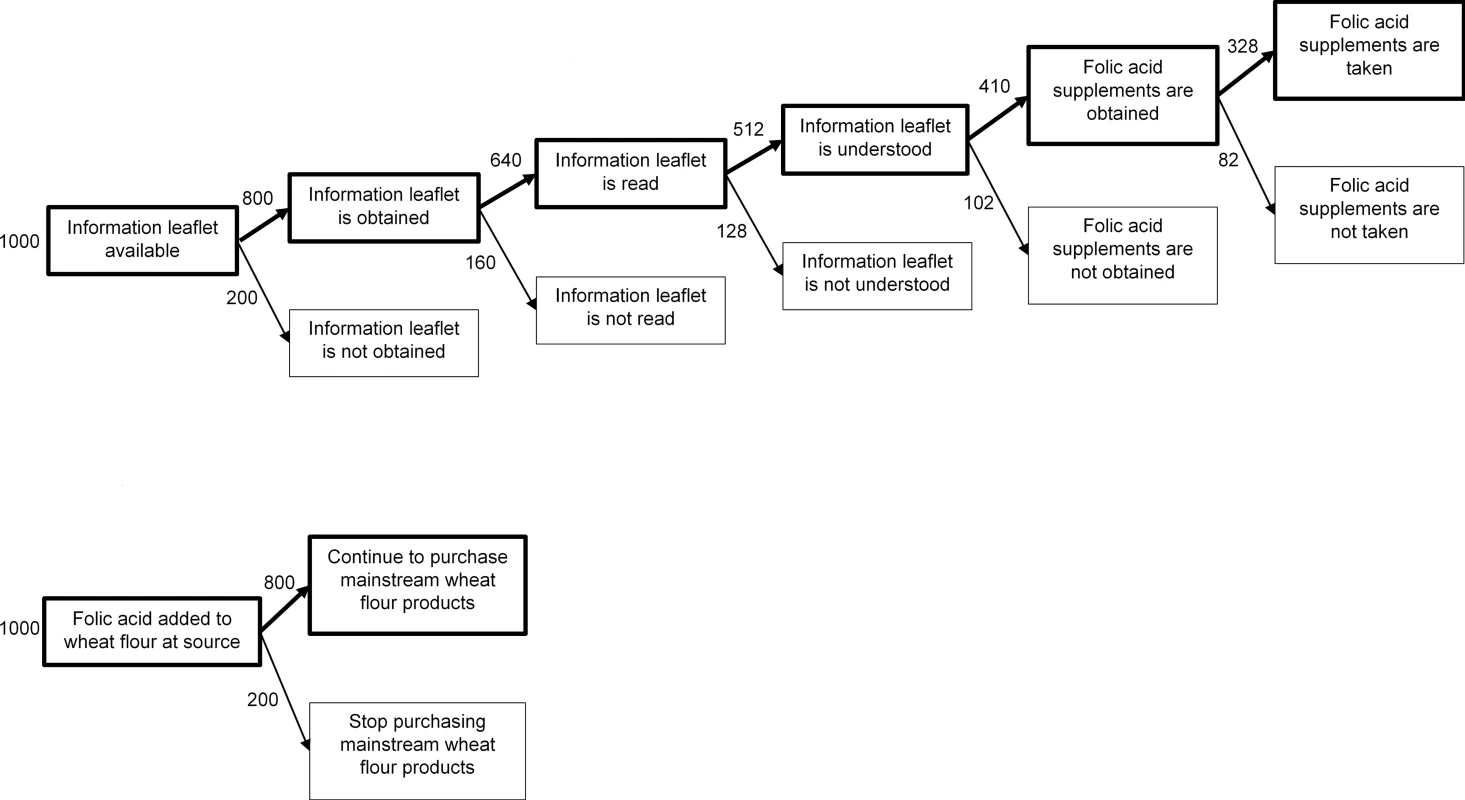
Both examples illustrate population interventions to increase folate in women trying to conceive. The top panel illustrates an information leaflet encouraging women to take folic acid supplements (a high-agency population intervention). The bottom panel illustrates the universal addition of folic acid to mainstream wheat flour (a low-agency intervention). Numbers are illustrative and indicate how many women might be in each pathway if it is hypothetically assumed that there is 20% attrition at each step. The steps shown in both cases are illustrative and not necessarily exhaustive. There are a number of reasons why high-agency population interventions may reinforce socioeconomic inequalities. Exerting agency requires individuals to rally their cognitive, psychological, time, and material resources [7]—all of which tend to be socioeconomically patterned. More socioeconomically advantaged people, with better health literacy (a cognitive resource) [17], may find it easier to make sense of the information provided in public health messages. More affluent parents may have more strategies for resisting their children’s “pester power” for less healthy foods (a psychological resource) [18]. More affluent people are more likely to have the material resources to be able to afford more expensive but healthier foods [19] and the time resources to source and prepare them [20]. Small inequalities at each intervention step illustrated in Fig 1 may multiply to become large inequalities in outcomes [16].
A New Framework for Public Health Interventions
Our examples above focus on diet, including diet’s role in obesity, but all public health interventions could be placed on a continuum that describes the amount of agency individuals must use to benefit from an intervention. Similarly, while Rose dichotomised preventive interventions as high risk or population, it seems more likely that this too is a continuum. Local planning arrangements restricting proliferation of hot food takeaways near schools target “vulnerable populations” (i.e., children) [8]. This places such interventions somewhere between high-risk interventions targeted at those known to be at high baseline risk and population interventions available to all.
When combined, these two continuums provide a framework for describing the whole range of public health interventions. Fig 2 illustrates this with examples of diet and obesity interventions.
Fig. 2. Two continuums describe all public health interventions, with examples related to diet and obesity. 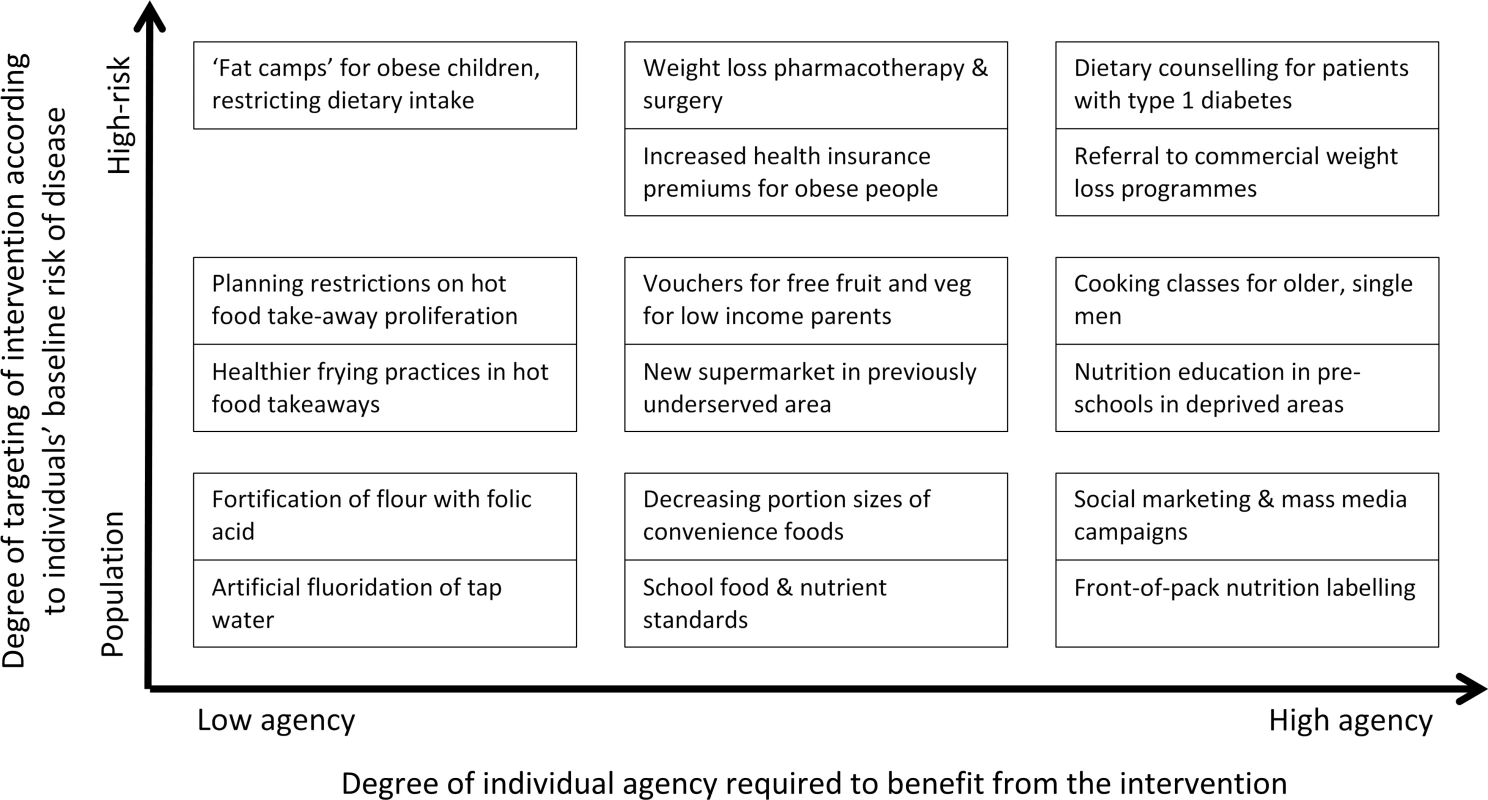
Interventions grouped together fall at similar points on the two continuums; we have not attempted to make fine-grained distinctions of where interventions fall on each continuum. Low-Agency Population Interventions Should Be the Backbone of Public Health Strategies
Low-agency population interventions are most likely to achieve the twin public health aims of preventing disease and minimising inequalities. These interventions should, therefore, form the backbone of public health strategies.
This is not to say that high-agency population interventions are not valuable. Whilst information and encouragement are often not sufficient to change diet [21], they may still be necessary in some cases. It is also possible that high - and low-agency population interventions act synergistically. For example, a hypothetical intervention involving fortification of flour with folic acid (a low-agency population intervention) that is highly publicised and discussed may raise awareness of the benefits of taking folic acid supplements during pregnancy and so prompt greater engagement with information leaflets about prenatal health (a high-agency population intervention).
Why Are Low-Agency Population Interventions Underused?
Given the clear value of low-agency population interventions, why do high-agency ones still dominate? One reason may be a perception that low-agency population interventions are less acceptable to various interested parties. In the case of diet and obesity interventions, these parties include politicians, who may enact interventions; the public, who are the recipients of interventions; and food companies, whose commercial interests may be affected by interventions.
Low-agency interventions are sometimes considered to be synonymous with limiting free choice [11]. However, it is unlikely that many people genuinely do make “free choices” about what they eat. Food “choices” are strongly influenced by habits, what food is available and affordable, and cultural norms [22]. Low-income parents often struggle to afford the fruit and vegetables they know to be important for their children’s health [23]. Using subsidies to make healthier food more affordable is a low-agency population intervention that may increase the choices available to these parents.
Public acceptability of low-agency population interventions is dependent not only on how much these interventions are felt to intrude on personal autonomy. Instead, how effective interventions are perceived to be, the importance of the public health “problem” targeted, and personal familiarity with interventions all influence intervention acceptability [24]. England’s experience with banning smoking in public places, in which acceptability increased after the ban was enforced [25], shows that public acceptability of low-agency population interventions is not immutable. The public health community needs to put more effort into learning about, and doing, effective “hearts and minds” work to build public acceptability of low-agency population interventions.
It may seem obvious that low-agency population interventions would be particularly unacceptable to food suppliers, manufacturers, and retailers with vested commercial interests in maintaining current dietary patterns. There is now growing scientific evidence confirming the efforts that those with commercial vested interests can make to avoid low-agency population interventions and the impact these efforts can have on policy [26]. Organisations with vested commercial interests may also have substantial resources at their disposal to circumvent, or undermine, any low-agency public health interventions that are implemented. There is often public cynicism about the actions of food companies [27]. This cynicism could be exploited to give politicians and policy makers the “space” they need to enact low-agency population interventions.
Conclusion
Much current policy for improving diet and reducing obesity focuses on population interventions that require individuals to use a high level of individual agency to benefit. These are likely to be less effective, and less equitable, than interventions requiring less agency. Although we have focused here on diet and obesity, these arguments ring true across many areas of public health.
Whilst action across the full spectrum of the framework described in Fig 2 is required, more attention should be given to the development and implementation of low-agency population interventions. Many before us have made similar arguments (e.g., [7,21,28]), yet action to implement low-agency population interventions remains limited. Politicians, civil servants, researchers, and others may shy away from low-agency interventions, as they see these as more politically difficult. We all need to have more courage to argue the case that these interventions can be publically acceptable, support people to live healthier lives, and reduce inequalities in health. Low-agency population interventions should be central to public health action on diet and obesity.
Zdroje
1. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2014;384(9945):766–81. doi: http://dx.doi.org/10.1016/S0140-6736(14)60460-8
2. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60. Epub 2012/12/19. doi: 10.1016/s0140-6736(12)61766-8 23245609; PubMed Central PMCID: PMCPmc4156511.
3. Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87(5):1107–17. Epub 2008/05/13. 18469226.
4. Jones-Smith JC, Gordon-Larsen P, Siddiqi A, Popkin BM. Is the burden of overweight shifting to the poor across the globe? Time trends among women in 39 low - and middle-income countries (1991–2008). Int J Obes (Lond). 2012;36(8):1114–20. Epub 2011/09/14. doi: 10.1038/ijo.2011.179 21912397; PubMed Central PMCID: PMCPmc3516372.
5. Rose G. The strategy of preventive medicine. Guildford: Oxford University Press; 1992.
6. Tsai AC. A typology of structural approaches to HIV prevention. Social science & medicine (1982). 2012;75(9):1562–71. doi: 10.1016/j.socscimed.2012.06.033 PMC3443954.
7. Capewell S, Graham H. Will Cardiovascular Disease Prevention Widen Health Inequalities? PLoS Med. 2010;7(8):e1000320. doi: 10.1371/journal.pmed.1000320 20811492
8. McLaren L, McIntyre L, Kirkpatrick S. Rose's population strategy of prevention need not increase social inequalities in health. Int J Epidemiol. 2010;39(2):372–7. doi: 10.1093/ije/dyp315 19887510
9. He FJ, Pombo-Rodrigues S, MacGregor GA. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open. 2014;4(4). doi: 10.1136/bmjopen-2013-004549
10. Hollands GJ, Shemilt I, Marteau TM, Jebb SA, Kelly MP, Nakamura R, et al. Altering micro-environments to change population health behaviour: towards an evidence base for choice architecture interventions. BMC Public Health. 2013;13 : 1218. Epub 2013/12/24. doi: 10.1186/1471-2458-13-1218 24359583; PubMed Central PMCID: PMCPmc3881502.
11. Frieden TR. A Framework for Public Health Action: The Health Impact Pyramid. Am J Public Health. 2010;100(4):590–5. doi: 10.2105/ajph.2009.185652 20167880
12. Cappuccio FP, Capewell S, Lincoln P, McPherson K. Policy options to reduce population salt intake. BMJ. 2011;343:d4995. doi: 10.1136/bmj.d4995 21835876
13. Beauchamp A, Backholer K, Magliano D, Peeters A. The effect of obesity prevention interventions according to socioeconomic position: a systematic review. Obes Rev. 2014;15(7):541–54. doi: 10.1111/obr.12161 24629126
14. Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health. 2012;67(2):190–3. doi: 10.1136/jech-2012-201257 22875078
15. Sumar N, McLaren L. Impact on social inequalities of population strategies of prevention for folate intake in women of childbearing age. Am J Public Health. 2011;101(7):1218–24. Epub 2011/05/14. doi: 10.2105/ajph.2010.300018 21566037; PubMed Central PMCID: PMCPmc3110217.
16. White M, Adams J, Heywood P. How and why do interventions that increase health overall widen inequalities within populations? In: Babones S, editor. Social inequality and public health. Bristol: Policy Press; 2009. p. 65–82.
17. Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, et al. Health literacy among medicare enrollees in a managed care organization. J Am Med Assoc. 1999;281(6):545–51. doi: 10.1001/jama.281.6.545
18. Campbell S, James EL, Stacey FG, Bowman J, Chapman K, Kelly B. A mixed-method examination of food marketing directed towards children in Australian supermarkets. Health Promot Int. 2014;29(2):267–77. Epub 2012/11/17. doi: 10.1093/heapro/das060 23154998.
19. Monsivais P, Aggarwal A, Drewnowski A. Are socioeconomic disparities in diet quality explained by diet cost? J Epidemiol Community Health. 2012;66(6):530–5. doi: 10.1136/jech.2010.122333 PMC3951975.
20. Jabs J, Devine CM. Time scarcity and food choices: an overview. Appetite. 2006;47(2):196–204. Epub 2006/05/16. doi: 10.1016/j.appet.2006.02.014 16698116.
21. Backholer K, Beauchamp A, Ball K, Turrell G, Martin J, Woods J, et al. A framework for evaluating the impact of obesity prevention strategies on socioeconomic inequalities in weight. Am J Public Health. 2014;104(10):e43–50. Epub 2014/08/15. doi: 10.2105/ajph.2014.302066 25121810.
22. Nuffield Council on Bioethics. Public health: ethical issues. Cambridge, UK: Nuffield Council on Bioethics, 2007.
23. National Obesity Observatory. Knowledge and attitudes towards healthy eating and physical activity: what the data tell us. London: National Obesity Observatory, 2011.
24. Diepeveen S, Ling T, Suhrcke M, Roland M, Marteau T. Public acceptability of government intervention to change health-related behaviours: a systematic review and narrative synthesis. BMC Public Health. 2013;13 : 756. doi: 10.1186/1471-2458-13-756 23947336
25. Platt S, Amos A, Godfrey C, Martin C, Ritchie D, White M, et al. Evaluation of Smokefree England: a longitudinal, qualitative study London: Public Health Research Consortium, 2009.
26. Moise N, Cifuentes E, Orozco E, Willett W. Limiting the consumption of sugar sweetened beverages in Mexico's obesogenic environment: A qualitative policy review and stakeholder analysis. J Public Health Policy. 2011;32(4):458–75. doi: 10.2307/41342698 21654826
27. Gollust SE, Barry CL, Niederdeppe J. Americans' opinions about policies to reduce consumption of sugar-sweetened beverages. Prev Med. 2014;63 : 52–7. doi: http://dx.doi.org/10.1016/j.ypmed.2014.03.002 24631499
28. Blankenship KM, Friedman SR, Dworkin S, Mantell JE. Structural Interventions: Concepts, Challenges and Opportunities for Research. J Urban Health. 2006;83(1):59–72. doi: 10.1007/s11524-005-9007-4 16736355
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2016 Číslo 4- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Antikoagulační léčba u pacientů před operačními výkony
-
Všechny články tohoto čísla
- Why Are Some Population Interventions for Diet and Obesity More Equitable and Effective Than Others? The Role of Individual Agency
- Risk of Bias in Systematic Reviews of Non-Randomized Studies of Adverse Cardiovascular Effects of Thiazolidinediones and Cyclooxygenase-2 Inhibitors: Application of a New Cochrane Risk of Bias Tool
- The Vast and Varied Global Burden of Norovirus: Prospects for Prevention and Control
- The Association between Sulfonylurea Use and All-Cause and Cardiovascular Mortality: A Meta-Analysis with Trial Sequential Analysis of Randomized Clinical Trials
- Disentangling the Association between Statins, Cholesterol, and Colorectal Cancer: A Nested Case-Control Study
- Gender Differences in Homicide of Neonates, Infants, and Children under 5 y in South Africa: Results from the Cross-Sectional 2009 National Child Homicide Study
- Mobile Phones As Surveillance Tools: Implementing and Evaluating a Large-Scale Intersectoral Surveillance System for Rabies in Tanzania
- Building Learning Health Systems to Accelerate Research and Improve Outcomes of Clinical Care in Low- and Middle-Income Countries
- The Future of the RTS,S/AS01 Malaria Vaccine: An Alternative Development Plan
- Birth “Out-of-Hours”: An Evaluation of Obstetric Practice and Outcome According to the Presence of Senior Obstetricians on the Labour Ward
- A Nested Case–Control Study of Metabolically Defined Body Size Phenotypes and Risk of Colorectal Cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC)
- Development and Validation of a New Prognostic System for Patients with Hepatocellular Carcinoma
- Underweight, Markers of Cachexia, and Mortality in Acute Myocardial Infarction: A Prospective Cohort Study of Elderly Medicare Beneficiaries
- The Impact of Hotspot-Targeted Interventions on Malaria Transmission in Rachuonyo South District in the Western Kenyan Highlands: A Cluster-Randomized Controlled Trial
- Experimental Treatment of Ebola Virus Disease with TKM-130803: A Single-Arm Phase 2 Clinical Trial
- Is There Evidence of Poorer Birth Outcomes for Mothers and Babies When the Most Senior Obstetrician Is Not On Site?
- Clinical Implications of Cancer Genomics: A Call for Papers
- The ITA.LI.CA Staging System: A Novel Staging System for Hepatocellular Carcinoma
- Observational Evidence of For-Profit Delivery and Inferior Nursing Home Care: When Is There Enough Evidence for Policy Change?
- Child Homicide: A Global Public Health Concern
- The Chernobyl Disaster and Beyond: Implications of the Sendai Framework for Disaster Risk Reduction 2015–2030
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Observational Evidence of For-Profit Delivery and Inferior Nursing Home Care: When Is There Enough Evidence for Policy Change?
- Experimental Treatment of Ebola Virus Disease with TKM-130803: A Single-Arm Phase 2 Clinical Trial
- The Chernobyl Disaster and Beyond: Implications of the Sendai Framework for Disaster Risk Reduction 2015–2030
- Is There Evidence of Poorer Birth Outcomes for Mothers and Babies When the Most Senior Obstetrician Is Not On Site?
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



