-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaSocial Relationships and Mortality Risk: A Meta-analytic Review
Background:
The quality and quantity of individuals' social relationships has been linked not only to mental health but also to both morbidity and mortality.Objectives:
This meta-analytic review was conducted to determine the extent to which social relationships influence risk for mortality, which aspects of social relationships are most highly predictive, and which factors may moderate the risk.Data Extraction:
Data were extracted on several participant characteristics, including cause of mortality, initial health status, and pre-existing health conditions, as well as on study characteristics, including length of follow-up and type of assessment of social relationships.Results:
Across 148 studies (308,849 participants), the random effects weighted average effect size was OR = 1.50 (95% CI 1.42 to 1.59), indicating a 50% increased likelihood of survival for participants with stronger social relationships. This finding remained consistent across age, sex, initial health status, cause of death, and follow-up period. Significant differences were found across the type of social measurement evaluated (p<0.001); the association was strongest for complex measures of social integration (OR = 1.91; 95% CI 1.63 to 2.23) and lowest for binary indicators of residential status (living alone versus with others) (OR = 1.19; 95% CI 0.99 to 1.44).Conclusions:
The influence of social relationships on risk for mortality is comparable with well-established risk factors for mortality.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 7(7): e32767. doi:10.1371/journal.pmed.1000316
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1000316Summary
Background:
The quality and quantity of individuals' social relationships has been linked not only to mental health but also to both morbidity and mortality.Objectives:
This meta-analytic review was conducted to determine the extent to which social relationships influence risk for mortality, which aspects of social relationships are most highly predictive, and which factors may moderate the risk.Data Extraction:
Data were extracted on several participant characteristics, including cause of mortality, initial health status, and pre-existing health conditions, as well as on study characteristics, including length of follow-up and type of assessment of social relationships.Results:
Across 148 studies (308,849 participants), the random effects weighted average effect size was OR = 1.50 (95% CI 1.42 to 1.59), indicating a 50% increased likelihood of survival for participants with stronger social relationships. This finding remained consistent across age, sex, initial health status, cause of death, and follow-up period. Significant differences were found across the type of social measurement evaluated (p<0.001); the association was strongest for complex measures of social integration (OR = 1.91; 95% CI 1.63 to 2.23) and lowest for binary indicators of residential status (living alone versus with others) (OR = 1.19; 95% CI 0.99 to 1.44).Conclusions:
The influence of social relationships on risk for mortality is comparable with well-established risk factors for mortality.
: Please see later in the article for the Editors' SummaryIntroduction
“Social relationships, or the relative lack thereof, constitute a major risk factor for health—rivaling the effect of well established health risk factors such as cigarette smoking, blood pressure, blood lipids, obesity and physical activity”
—House, Landis, and Umberson; Science 1988 [1]
Two decades ago a causal association between social relationships and mortality was proposed after a review of five large prospective studies concluded that social relationships predict mortality [1]. Following the publication of this provocative review, the number of prospective studies of mortality that included measures of social relationships increased exponentially. Although the inverse association between social relationships and nonsuicide mortality has received increased attention in research, neither major health organizations nor the general public recognize it as a risk factor for mortality. This may be due in part to the fact that the literature has become unwieldy, with wide variation in how social relationships are measured across a large number of studies and disappointing clinical trials [2]. “Social relationships” has perhaps become viewed as a fuzzy variable, lacking the level of precision and control that is preferred in biomedical research. Thus, the large corpus of relevant empirical research is in need of synthesis and refinement.
Current evidence also indicates that the quantity and/or quality of social relationships in industrialized societies are decreasing. For instance, trends reveal reduced intergenerational living, greater social mobility, delayed marriage, dual-career families, increased single-residence households, and increased age-related disabilities [3],[4]. More specifically, over the last two decades there has been a three-fold increase in the number of Americans who report having no confidant—now the modal response [3]. Such findings suggest that despite increases in technology and globalization that would presumably foster social connections, people are becoming increasingly more socially isolated. Given these trends, understanding the nature and extent of the association between social relationships and mortality is of increased temporal importance.
There are two general theoretical models that propose processes through which social relationships may influence health: the stress buffering and main effects models [5]. The buffering hypothesis suggests that social relationships may provide resources (informational, emotional, or tangible) that promote adaptive behavioral or neuroendocrine responses to acute or chronic stressors (e.g., illness, life events, life transitions). The aid from social relationships thereby moderates or buffers the deleterious influence of stressors on health. From this perspective, the term social support is used to refer to the real or perceived availability of social resources [6]. The main effects model proposes that social relationships may be associated with protective health effects through more direct means, such as cognitive, emotional, behavioral, and biological influences that are not explicitly intended as help or support. For instance, social relationships may directly encourage or indirectly model healthy behaviors; thus, being part of a social network is typically associated with conformity to social norms relevant to health and self-care. In addition, being part of a social network gives individuals meaningful roles that provide self-esteem and purpose to life [7],[8].
Social relationships have been defined and measured in diverse ways across studies. Despite striking differences, three major components of social relationships are consistently evaluated [5]: (a) the degree of integration in social networks [9], (b) the social interactions that are intended to be supportive (i.e., received social support), and (c) the beliefs and perceptions of support availability held by the individual (i.e., perceived social support). The first subconstruct represents the structural aspects of social relationships and the latter two represent the functional aspects. Notably, these different subconstructs are only moderately intercorrelated, typically ranging between r = 0.20 and 0.30 [9],[10]. While all three components have been shown to be associated with morbidity and mortality, it is thought that each may influence health in different ways [11],[12]. Because it is presently unclear whether any single aspect of social relationships is more predictive than others, synthesis of data across studies using several types of measures of social relationships would allow for essential comparisons that have not been conducted on such a large scale.
Empirical data suggest the medical relevance of social relationships in improving patient care [13], increasing compliance with medical regimens [13], and promoting decreased length of hospitalization [14],[15]. Likewise, social relationships have been linked to the development [16],[17] and progression [18]–[21] of cardiovascular disease [22]—a leading cause of death globally. Therefore, synthesis of the current empirical evidence linking social relationships and mortality, along with clarifications of potential moderators, may be particularly relevant to public health and clinical practice for informing interventions and policies aimed at reducing risk for mortality.
To address these issues, we conducted a meta-analysis of the literature investigating the association between social relationships and mortality. Specifically, we addressed the following questions: What is the overall magnitude of the association between social relationships and mortality across research studies? Do structural versus functional aspects of social relationships differentially impact the risk for mortality? Is the association moderated by participant characteristics (age, gender, health status, cause of mortality) or by study characteristics (length of clinical follow-up, inclusion of statistical controls)? Is the influence of social relationships on mortality a gradient or threshold effect?
Methods
Identification of Studies
To identify published and unpublished studies of the association between social relationships and mortality, we used three techniques. First, we conducted searches of studies from January 1900 to January 2007 using several electronic databases: Dissertation Abstracts, HealthSTAR, Medline, Mental Health Abstracts, PsycINFO, Social Sciences Abstracts, Sociological Abstracts via SocioFile, Academic Search Premier, ERIC, and Family & Society Studies Worldwide. To capture the broadest possible sample of relevant articles, we used multiple search terms, including mortality, death, decease(d), died, dead, and remain(ed) alive, which were crossed with search words related to social relationships, including the terms social and interpersonal linked to the following words: support, network, integration, participation, cohesion, relationship, capital, and isolation To reduce inadvertent omissions, we searched databases yielding the most citations (Medline, PsycINFO) two additional times. Next, we manually examined the reference sections of past reviews and of studies meeting the inclusion criteria to locate articles not identified in the database searches. Finally, we sent solicitation letters to authors who had published three or more articles on the topic.
Inclusion Criteria
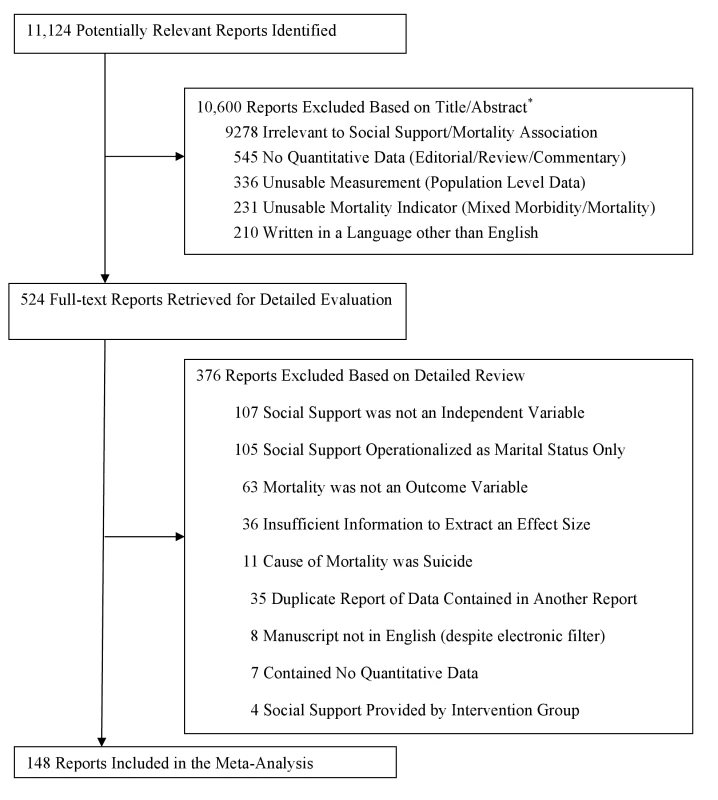
We included in the meta-analysis studies that provided quantitative data regarding individuals' mortality as a function of social relationships, including both structural and functional aspects [23]. Because we were interested in the impact of social relationships on disease, we excluded studies in which mortality was a result of suicide or injury. We also excluded studies in which the only measurement of social support was an intervention provided within the context of the study (e.g., support group), the source of social support was nonhuman (e.g., a pet or higher power), or the social support was provided to others (i.e., giving support to others or measures of others' benefit from the support provided) rather than to the individual tracked for mortality status. We coded studies that included participant marital status as one of several indicators of social support, but we excluded studies in which marital status was the only indicator of social support. We also excluded studies in which the outcome was not explicitly and solely mortality (e.g., combined outcomes of morbidity/mortality). Reports with exclusively aggregated data (e.g., census-level statistics) were also excluded. Manuscripts coded were all written in English, which accounted for 98% of the total retrieved. See Figure 1 for additional details.
Data Abstraction
To increase the accuracy of coding and data entry, each article was initially coded by two raters. Subsequently, the same article was independently coded by two additional raters. Coders extracted several objectively verifiable characteristics of the studies: (a) the number of participants and their composition by age, gender, marital status, distress level, health status, and pre-existing health conditions (if any), as well as the percentage of smokers and percentage of physically active individuals, and, of course, the cause of mortality; (b) the length of follow up; (c) the research design; and (d) the aspect of social relationships evaluated.
Data within studies were often reported in terms of odds ratios (ORs), the likelihood of mortality across distinct levels of social relationships. Because OR values cannot be meaningfully aggregated, all effect sizes reported within studies were transformed to the natural log OR (lnOR) for analyses and then transformed back to OR for interpretation. When effect size data were reported in any metric other than OR or lnOR, we transformed those values using statistical software programs and macros (e.g., Comprehensive Meta-Analysis [24]). In some cases when direct statistical transformation proved impossible, we calculated the corresponding effect sizes from frequency data in matrices of mortality status by social relationship status. When frequency data were not reported, we recovered the cell probabilities from the reported ratio and marginal probabilities. When survival analyses (i.e., hazard ratios) were reported, we calculated the effect size from the associated level of statistical significance, often derived from 95% confidence intervals (CIs). Across all studies we assigned OR values less than 1.00 to data indicative of increased mortality and OR values greater than 1.00 to data indicative of decreased mortality for individuals with relatively higher levels of social relationships.
When multiple effect sizes were reported within a study at the same point in time (e.g., across different measures of social relationships), we averaged the several values (weighted by standard error) to avoid violating the assumption of independent samples. In such cases, the aggregate standard error value for the lnOR were estimated on the basis of the total frequency data without adjustment for possible correlation among the averaged values. Although this method was imprecise, the manuscripts included in the meta-analysis did not report the information necessary to make the statistical adjustments, and we decided not to impute values given the wide range possible. In analyzing the data we used the shifting units of analysis approach [25] which minimizes the threat of nonindependence in the data while at the same time allowing more detailed follow-up analyses to be conducted (i.e., examination of effect size heterogeneity).
When multiple reports contained data from the same participants (publications of the same database), we selected the report containing the whole sample and eliminated reports of subsamples. When multiple reports contained the same whole sample, we selected the one with the longest follow-up duration. When multiple reports with the same whole sample were of the same duration, we selected the one reporting the greatest number of measures of social relationships.
In cases where multiple effect sizes were reported across different levels of social relationships (i.e., high versus medium, medium versus low), we extracted the value with the greatest contrast (i.e., high versus low). When a study contained multiple effect sizes across time, we extracted the data from the longest follow-up period. If a study used statistical controls in calculating an effect size, we extracted the data from the model utilizing the fewest statistical controls so as to remain as consistent as possible across studies (and we recorded the type and number of covariates used within each study to run post hoc comparative analyses). We coded the research design used rather than estimate risk of individual study bias. The coding protocol is available from the authors.
The majority of information obtained from the studies was extracted verbatim from the reports. As a result, the inter-rater agreement was quite high for categorical variables (mean Cohen's kappa = 0.73, SD = 0.13) and for continuous variables (mean intraclass correlation [26] = 0.80, SD = .14). Discrepancies across coding pairs were resolved through further scrutiny of the manuscript until consensus was obtained.
Aggregate effect sizes were calculated using random effects models following confirmation of heterogeneity. A random effects approach produces results that generalize beyond the sample of studies actually reviewed [27]. The assumptions made in this meta-analysis clearly warrant this method: The belief that certain variables serve as moderators of the observed association between social relationships and mortality implies that the studies reviewed will estimate different population effect sizes. Random effects models take such between-studies variation into account, whereas fixed effects models do not [28]. In each analysis conducted, we examined the remaining variance to confirm that random effects models were appropriate.
Results
Statistically nonredundant effect sizes were extracted from 148 studies ([29]–[176]; see Table 1). Data were reported from 308,849 participants, with 51% from North America, 37% from Europe, 11% from Asia, and 1% from Australia. Across all studies, the average age of participants at initial evaluation was 63.9 years, and participants were evenly represented across sex (49% female, 51% male). Of the studies examined, 60% involved community samples, but 24% examined individuals receiving outpatient medical treatment, and 16% utilized patients in inpatient medical settings. Of studies involving patients with a pre-existing diagnosis, 44% were specific to cardiovascular disease (CVD), 36% to cancer, 9% to renal disease, and the remaining 11% had a variety of conditions including neurological disease. Research reports most often (81%) considered all-cause mortality, but some restricted evaluations to mortality associated with cancer (9%), CVD (8%), or other causes (2%). Participants were followed for an average of 7.5 years (SD = 7.1, range = 3 months to 58 years), with an average of 29% of the participants dying within each study's follow-up period.
Tab. 1. Overview of the 148 studies included in the meta-analysis. 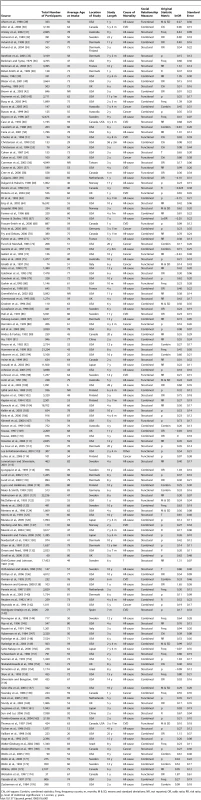
Chi, chi-square; Combin, combined statistics; Freq, frequency counts; m, months; M & SD, means and standard deviations; NR, not reported; OR, odds ratio; RR, risk ratio; p, level of statistical significance; t, t-scores; y, years. Omnibus Analysis
Across 148 studies, the random effects weighted average effect size was OR = 1.50 (95% confidence interval [CI] = 1.42 to 1.59), which indicated a 50% increased likelihood of survival as a function of stronger social relations. Odds ratios ranged from 0.77 to 6.50, with substantial heterogeneity across studies (I2 = 81% [95% CI = 78% to 84%]; Q(147) = 790, p<0.001; τ2 = 0.07), suggesting that systematic effect size variability was unaccounted for. Thus factors associated with the studies themselves (e.g., publication status), participant characteristics (e.g., age, health status), and the type of evaluation of social relationships (e.g., structural social networks versus perceptions of functional social support) may have moderated the overall results. We therefore conducted additional analyses to determine the extent to which these variables moderated the overall results.
To assess the possibility of publication bias [177], we conducted several analyses. First, we calculated the fail-safe N [177] to be 4,274, which is the theoretical number of unpublished studies with effect sizes averaging zero (no effect) that would be needed to render negligible the omnibus results. Second, we employed the “trim and fill” methodology described by Duval and Tweedie [178],[179] to estimate the number of studies missing due to publication bias, but this analysis failed to reveal any studies that would need to be created on the opposite side of the distribution, meaning that adjustment to the omnibus effect size was unnecessary. Third, we calculated both Egger's regression test and the alternative to that test recommended by Peters and colleagues [180] that is better suited to data in lnOR format. The results of both analyses failed to reach statistical significance (p>0.05). Finally, we plotted a contour-enhanced funnel plot (Figure 2) [181]. The data obtained from this meta-analysis were fairly symmetrical with respect to their own mean; fewer than ten studies were “missing” on the left side of the distribution that would have made the plot symmetrical. Based on these several analyses, publication bias is unlikely to threaten the results.
Fig. 2. Contour enhanced funnel plot. 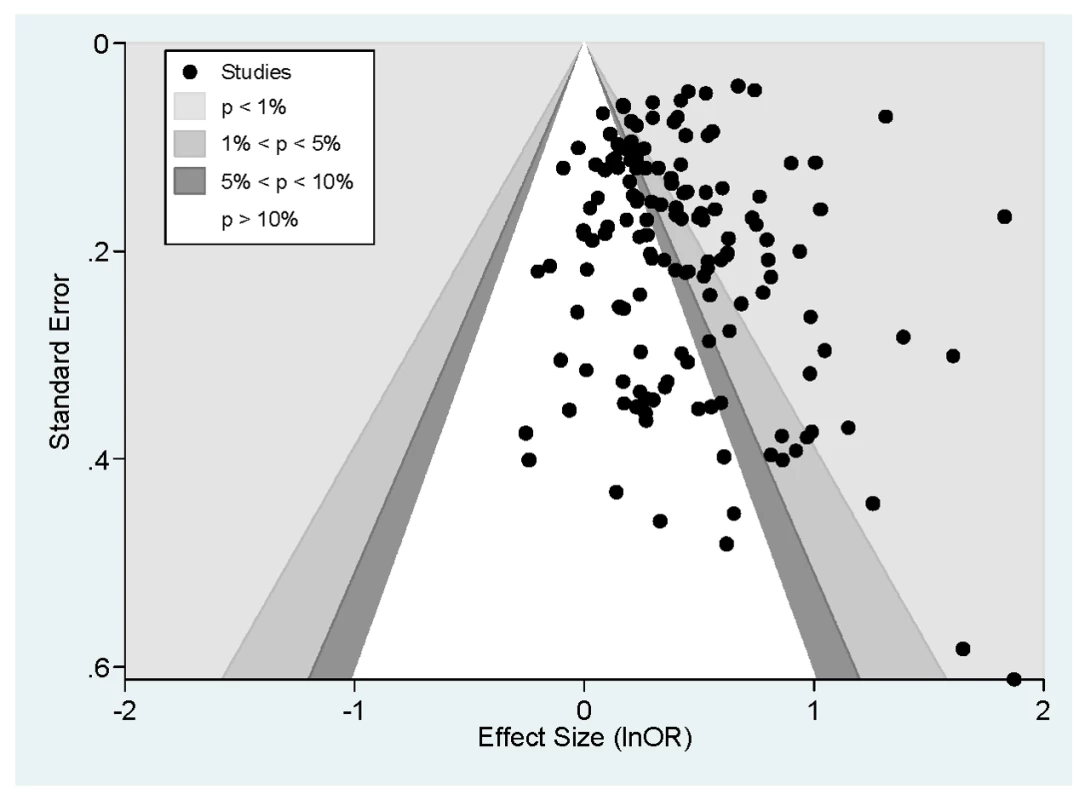
Moderation by Social Relationship Assessment, and by Participant and Study Characteristics
Given that structural versus functional components of social relationships may influence health in different ways [11],[12], the high degree of heterogeneity observed in the omnibus results may have been due in part to differences between the components of social relationships evaluated within and across studies. Hence the remaining analyses separately evaluate effect sizes obtained from structural, functional, and combined (structural and functional) measures of social relationships. Table 2 provides definitions of the types and subtypes of social relationships evaluated.
Tab. 2. Descriptive coding of the measures used to assess social relationships. 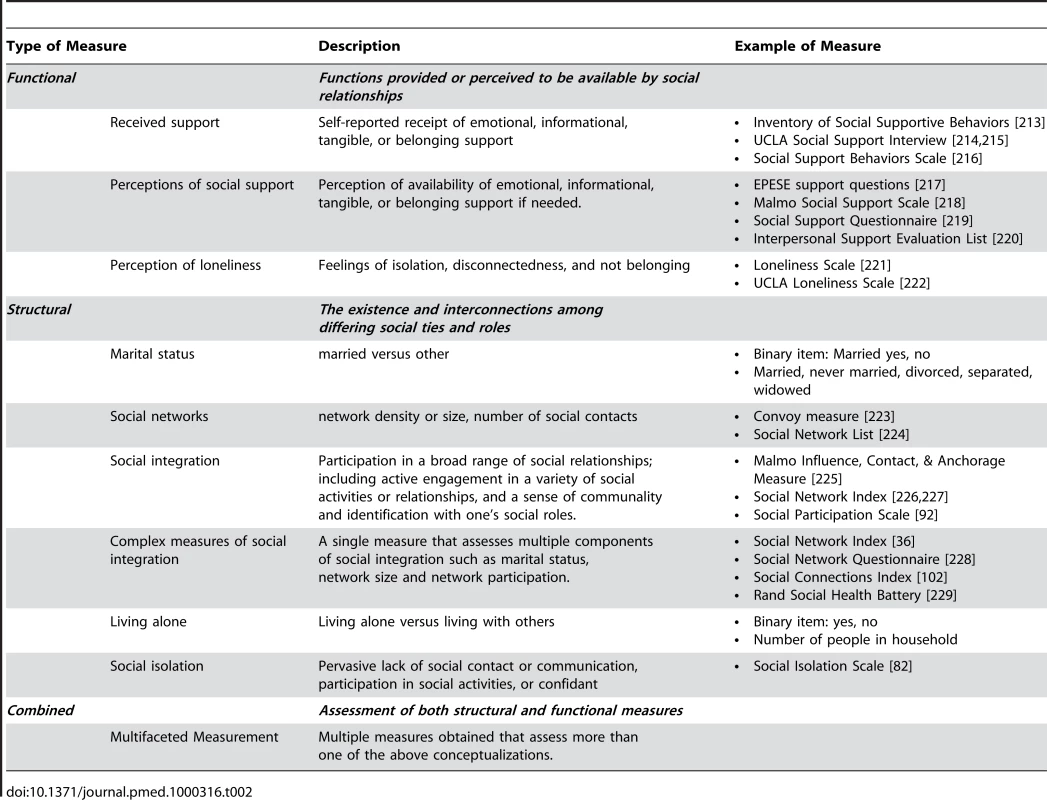
Structural aspects of social relationships
Sixty-three studies had data exclusive to structural measures of social relationships (see Figure 3). Across these studies, the random effects weighted average effect size was OR = 1.57 (95% CI = 1.46 to 1.70), which value fell within the CI of the omnibus results reported previously. The heterogeneity across studies was still quite large (I2 = 84% [95% CI = 80% to 87%]; Q(62) = 390, p<0.001; τ2 = 0.07), so we undertook metaregression with prespecified participant and study characteristics.
Fig. 3. Forest plot of structural measures. 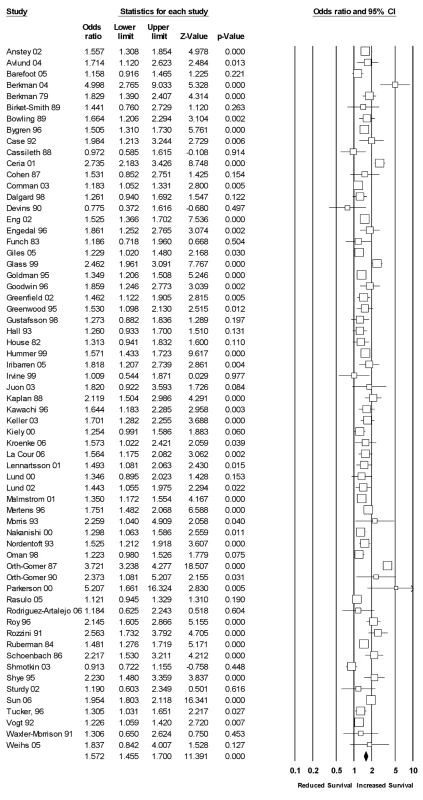
Metaregression is an analogue to multiple regression analysis for effect sizes. Its primary purpose is to ascertain which continuous and categorical (dummy coded) variables predict variation in effect size estimates. Using random effects weighted metaregression, we examined the simultaneous association (with all variables entered into the model) between effect sizes and prespecified participant and study characteristics (Table 3). To examine the most precise effect size estimates available and to increase the statistical power associated with this analysis, we shifted the unit of analysis [24] and extracted effect sizes within studies that were specific to measures of structural aspects of social relationships. That is, if a study contained effect sizes from both structural and functional types of social relationships, we extracted the structural types for this analysis (with identical subtypes aggregated), which resulted in a total of 230 unique effect sizes across 116 studies. A total of 18% of the variance in these effect sizes was explained in the metaregression (p<0.001). As can be seen in Table 3, effect sizes based on data controlling for other variables were lower in magnitude than those based on raw data. Moreover, effect sizes differed in magnitude across the subtype of structural social relationships measured. Complex measures of social integration were associated with larger effect size values than measures of social participation. Binary measures of whether participants lived alone (yes/no) were associated with smaller effect size values. Average random effects weighted odds ratios for the various subtypes of social relationships are reported in Table 4.
Tab. 3. Random effects metaregression for effect size estimates of structural social relationships. 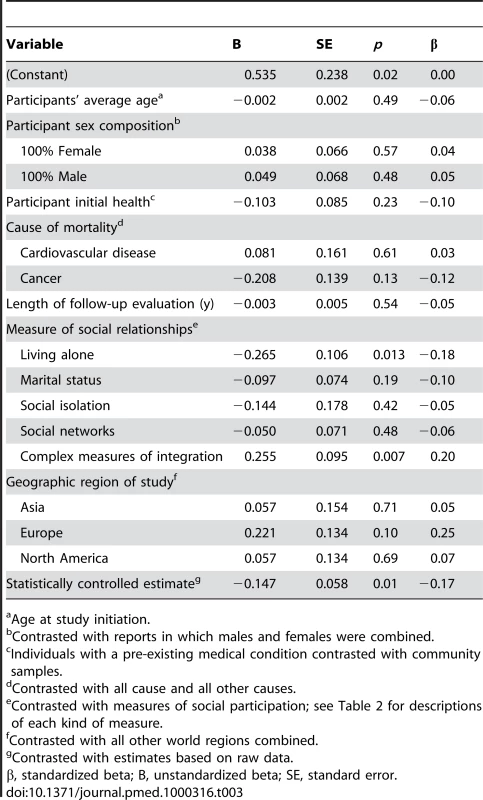
Age at study initiation. Tab. 4. Weighted average effect sizes across different measures of social relationships. 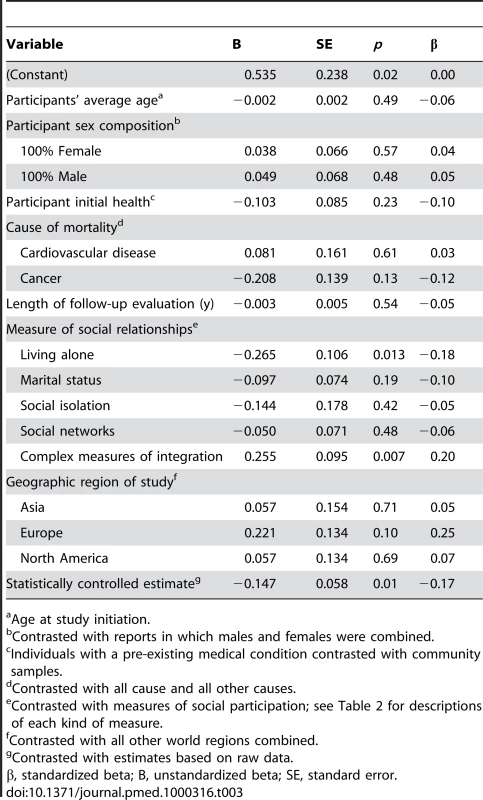
These analyses shifted the units of analysis, with distinct effect size estimates within studies used within different categories of measurement, such that many studies contributed more than one effect size but not more than one per category of measurement. Functional aspects of social relationships
Twenty-four studies had data exclusive to functional measures of social relationships (see Figure 4). Across these studies, the random effects weighted average effect size was OR = 1.46 (95% CI = 1.28 to 1.66), which value fell within the CI of the omnibus results reported previously. There was moderate heterogeneity across studies (I2 = 47% [95% CI = 16% to 68%]; Q(23) = 44, p<0.01; τ2 = 0.04), so we conducted a random effects metaregression using the same variables and analytic procedures described previously. We extracted 87 unique effect sizes that were specific to measures of functional social relationships within 72 studies. A total of 16.5% of the variance in these effect sizes was explained in the metaregression, but the model did not reach statistical significance (p = 0.46). The results were not moderated by any of the specified participant characteristics (age, sex, initial health status, cause of mortality) or study characteristics (length of follow-up, geographic region, statistical controls).
Fig. 4. Forest plot of functional measures. 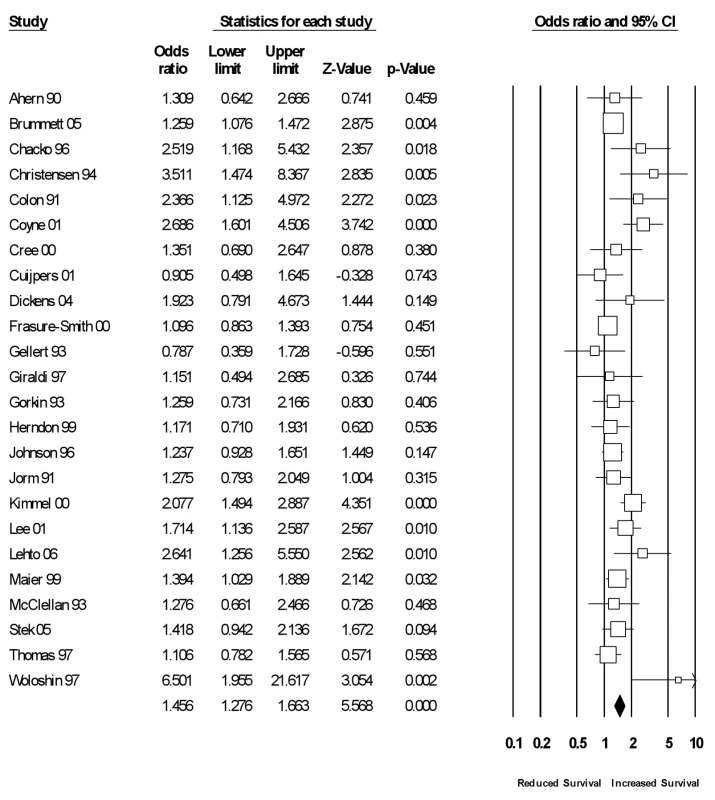
Combined assessments of social relationships
Sixty-one studies had combined data of both structural and functional measures of social relationships (see Figure 5). Across these studies, the random effects weighted average effect size was OR = 1.44 (95% CI = 1.32 to 1.58). A large degree of heterogeneity characterized studies (I2 = 82% [95% CI = 78% to 86%]; Q(60) = 337, p<0.001; τ2 = 0.09), and we conducted a random effects metaregression using the same variables and analytic procedures described previously. We extracted 64 unique effect sizes that evaluated combined structural and functional measures of social relationships within 61 studies. The metaregression explained only 6.8% of the variance in these effect sizes, and the model failed to reach statistical significance (p = 0.95). None of the variables in the metaregression moderated the results.
Fig. 5. Forest plot of combined measures. 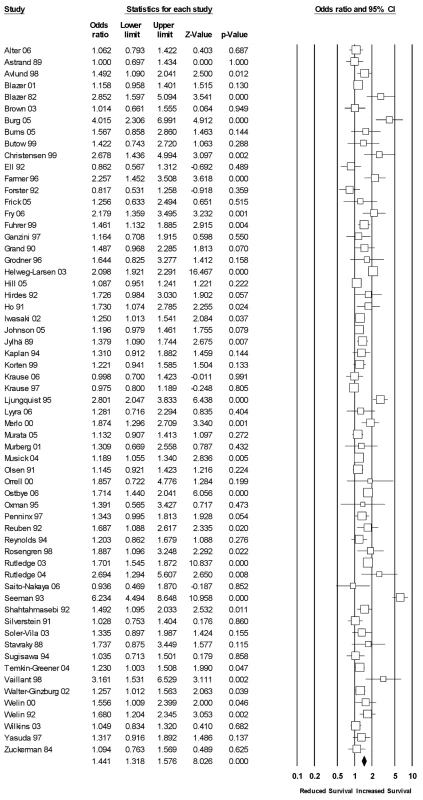
Discussion
Cumulative empirical evidence across 148 independent studies indicates that individuals' experiences within social relationships significantly predict mortality. The overall effect size corresponds with a 50% increase in odds of survival as a function of social relationships. Multidimensional assessments of social integration yielded an even stronger association: a 91% increase in odds of survival. Thus, the magnitude of these findings may be considered quite large, rivaling that of well-established risk factors (Figure 6). Results also remained consistent across a number of factors, including age, sex, initial health status, follow-up period, and cause of death, suggesting that the association between social relationships and mortality may be generalized.
Fig. 6. Comparison of odds (lnOR) of decreased mortality across several conditions associated with mortality. 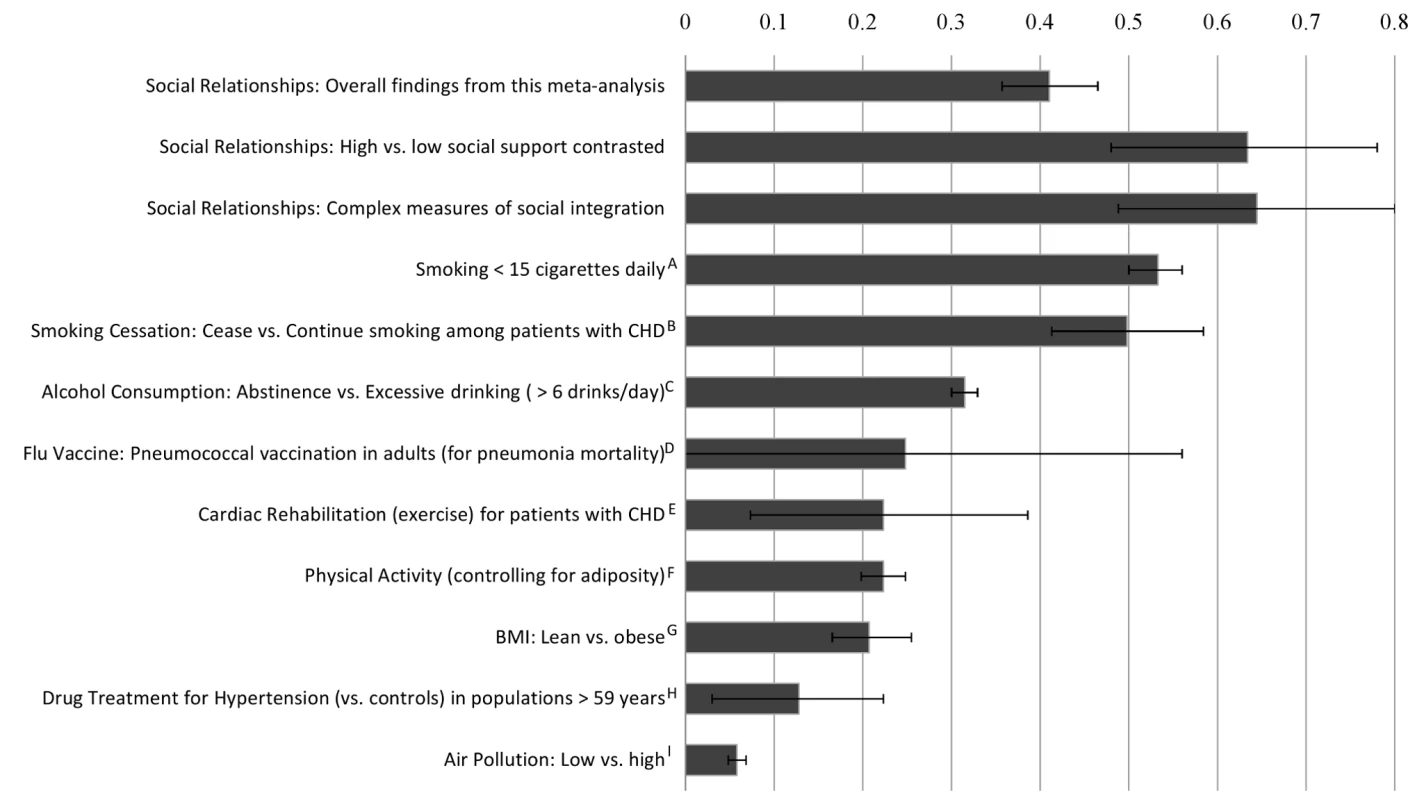
Note: Effect size of zero indicates no effect. The effect sizes were estimated from meta analyses: ; A = Shavelle, Paculdo, Strauss, and Kush, 2008 [205]; B = Critchley and Capewell, 2003 [206]; C = Holman, English, Milne, and Winter, 1996 [207]; D = Fine, Smith, Carson, Meffe, Sankey, Weissfeld, Detsky, and Kapoor, 1994 [208]; E = Taylor, Brown, Ebrahim, Jollife, Noorani, Rees et al., 2004 [209]; F, G = Katzmarzyk, Janssen, and Ardern, 2003 [210]; H = Insua, Sacks, Lau, Lau, Reitman, Pagano, and Chalmers, 1994 [211]; I = Schwartz, 1994 [212]. The magnitude of risk reduction varied depending on the type of measurement of social relationships (see Table 4). Social relationships were most highly predictive of reduced risk of mortality in studies that included multidimensional assessments of social integration. Because these studies included more than one type of social relationship measurement (e.g., network based inventories, marital status, etc.), such a measurement approach may better represent the multiple pathways (described earlier) by which social relationships influence health and mortality [182]. Conversely, binary evaluations of living alone (yes/no) were the least predictive of mortality status. The reliability and validity of measurement likely explains this finding, and researchers are encouraged to use psychometrically sound measures of social relationships (e.g., Table 2). For instance, while researchers may be tempted to use a simple single-item such as “living alone” as a proxy for social isolation, it is possible for one to live alone but have a large supportive social network and thus not adequately capture social isolation. We also found that social isolation had a similar influence on likelihood of mortality compared with other measures of social relationships. This evidence qualifies the notion of a threshold effect (lack of social relationships is the only detrimental condition); rather, the association appears robust across a variety of types of measures of social relationships.
This meta-analysis also provides evidence to support the directional influence of social relationships on mortality. Most of the studies (60%) involved community cohorts, most of whom would not be experiencing life-threatening conditions at the point of initial evaluation. Moreover, initial health status did not moderate the effect of social relationships on mortality. Although illness may result in poorer or more restricted social relationships (social isolation resulting from physical confinement), such that individuals closer to death may have decreased social support compared to healthy individuals, the findings from these studies indicate that general community samples with strong social relationships are likely to remain alive longer than similar individuals with poor social relations. However, causality is not easily established. One cannot randomly assign human participants to be socially isolated, married, or in a poor-quality relationship. A similar dilemma characterizes virtually all lifestyle risk factors for mortality: for instance, one cannot randomly assign individuals to be smokers or nonsmokers. Despite such challenges, “smoking represents the most extensively documented cause of disease ever investigated in the history of biomedical research” [183]. The link between social relationships and mortality is currently much less understood than other risk factors; nonetheless there is substantial experimental, cross-sectional, and prospective evidence linking social relationships with multiple pathways associated with mortality (see [182] for review). Existing models for reducing risk of mortality may be substantially strengthened by including social relationship factors.
Notably, the overall effect for social relationships on mortality reported here may be a conservative estimate. Many studies included in the meta-analysis utilized single item measures of social relations, yet the magnitude of the association was greatest among those studies utilizing complex assessments. Moreover, because many studies statistically adjusted for standard risk factors, the effect may be underestimated, since some of the impact of social relationships on mortality may be mediated through such factors (e.g., behavior, diet, exercise). Additionally, most measures of social relations did not take into account the quality of the social relationships, thereby assuming that all relationships are positive. However, research suggests this is not the case, with negative social relationships linked to greater risk of mortality [184],[185]. For instance, marital status is widely used as a measure of social integration; however, a growing literature documents its divergent effects based on level of marital quality [186],[187]. Thus the effect of positive social relationships on risk of mortality may actually be much larger than reported in this meta-analysis, given the failure to account for negative or detrimental social relationships within the measures utilized across studies.
Other possible limitations of this review should be acknowledged. Statistical controls (e.g., age, sex, physical condition, etc.) employed by many of the studies rule out a number of potentially confounding variables that might account for the association between social relationships and mortality. However, studies used an inconsistent variety of controlling variables, and some reports involved raw data (Table 1). Although effect size magnitude was diminished by the inclusion of statistical controls only within the data obtained by measures of structural social relationships (but not functional or combined measures), future research can better specify which variables are most likely to impact the overall association. It must also be acknowledged that existing data primarily represent research conducted in North America and Western Europe. Although we found no differences across world region, future reviews inclusive of research written in all languages (not only English) with participants better representing other world regions may yield better estimates across populations.
Approximately two decades after the review by House and colleagues [1], a generation of empirical research validates their initial premise: Social relationships exert an independent influence on risk for mortality comparable with well established risk factors for mortality (Figure 6). Although limited by the state of current investigations and possible omission of pertinent reports, this meta-analysis provides empirical evidence (nearly 30 times the number of studies previously reported) to support the criteria for considering insufficient social relationships a risk factor of mortality (i.e., strength and consistency of association across a wide range of studies, temporal ordering, and gradient of response) [188]. The magnitude of the association between social relationships and mortality has now been established, and this meta-analysis provides much-needed clarification regarding the social relationship factor(s) most predictive of mortality. Future research can shift to more nuanced questions aimed at (a) understanding the causal pathways by which social participation promotes health, (b) refining conceptual models, and (c) developing effective intervention and prevention models that explicitly account for social relations.
Some steps have already been taken identifying the psychological, behavioral, and physiological pathways linking social relationships to health [5],[182],[189]. Social relationships are linked to better health practices and to psychological processes, such as stress and depression, that influence health outcomes in their own right [190]; however, the influence of social relationships on health cannot be completely explained by these processes, as social relationships exert an independent effect. Reviews of such findings suggest that there are multiple biologic pathways involved (physiologic regulatory mechanisms, themselves intertwined) that in turn influence a number of disease endpoints [182],[191]–[193]. For instance, a number of studies indicate that social support is linked to better immune functioning [194]–[197] and to immune-mediated inflammatory processes [198]. Thus interdisciplinary work and perspective will be important in future studies given the complexity of the phenomenon.
Perhaps the most important challenge posed by these findings is how to effectively utilize social relationships to reduce mortality risk. Preliminary investigations have demonstrated some risk reduction through formalized social interventions [199]. While the evidence is mixed [2],[6], it should be noted that most social support interventions evaluated in the literature thus far are based on support provided from strangers; in contrast, evidence provided in this meta-analysis is based almost entirely on naturally occurring social relationships. Moreover, our analyses suggest that received support is less predictive of mortality than social integration (Table 4). Therefore, facilitating patient use of naturally occurring social relations and community-based interventions may be more successful than providing social support through hired personnel, except in cases in which patient social relations appear to be detrimental or absent. Multifaceted community-based interventions may have a number of advantages because such interventions are socially grounded and include a broad cross-section of the public. Public policy initiatives need not be limited to those deemed “high risk” or those who have already developed a health condition but could potentially include low - and moderate-risk individuals earlier in the risk trajectory [200]. Overall, given the significant increase in rate of survival (not to mention quality of life factors), the results of this meta-analysis are sufficiently compelling to promote further research aimed at designing and evaluating interventions that explicitly account for social relationship factors across levels of health care (prevention, evaluation, treatment compliance, rehabilitation, etc.).
Conclusion
Data across 308,849 individuals, followed for an average of 7.5 years, indicate that individuals with adequate social relationships have a 50% greater likelihood of survival compared to those with poor or insufficient social relationships. The magnitude of this effect is comparable with quitting smoking and it exceeds many well-known risk factors for mortality (e.g., obesity, physical inactivity). These findings also reveal significant variability in the predictive utility of social relationship variables, with multidimensional assessments of social integration being optimal when assessing an individual's risk for mortality and evidence that social isolation has a similar influence on mortality to other measures of social relationships. The overall effect remained consistent across a number of factors, including age, sex, initial health status, follow-up period, and cause of death, suggesting that the association between social relationships and mortality may be general, and efforts to reduce risk should not be isolated to subgroups such as the elderly.
To draw a parallel, many decades ago high mortality rates were observed among infants in custodial care (i.e., orphanages), even when controlling for pre-existing health conditions and medical treatment [201]–[204]. Lack of human contact predicted mortality. The medical profession was stunned to learn that infants would die without social interaction. This single finding, so simplistic in hindsight, was responsible for changes in practice and policy that markedly decreased mortality rates in custodial care settings. Contemporary medicine could similarly benefit from acknowledging the data: Social relationships influence the health outcomes of adults.
Physicians, health professionals, educators, and the public media take risk factors such as smoking, diet, and exercise seriously; the data presented here make a compelling case for social relationship factors to be added to that list. With such recognition, medical evaluations and screenings could routinely include variables of social well-being; medical care could recommend if not outright promote enhanced social connections; hospitals and clinics could involve patient support networks in implementing and monitoring treatment regimens and compliance, etc. Health care policies and public health initiatives could likewise benefit from explicitly accounting for social factors in efforts aimed at reducing mortality risk. Individuals do not exist in isolation; social factors influence individuals' health though cognitive, affective, and behavioral pathways. Efforts to reduce mortality via social relationship factors will require innovation, yet innovation already characterizes many medical interventions that extend life at the expense of quality of life. Social relationship–based interventions represent a major opportunity to enhance not only the quality of life but also survival.
Supporting Information
Zdroje
1. HouseJS
LandisKR
UmbersonD
1988 Social relationships and health. Science 241 540 545
2. BerkmanLF
BlumenthalJ
BurgM
2003 Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA 289 3106 3116
3. McPhersonM
Smith-LovinL
2006 Social Isolation in America: Changes in core discussion networks over two decades. Am Sociol Rev 71 353 375
4. PutnamRD
2000 Bowling Alone: The collapse and revival of American community New York, NY, US Simon & Schuster
5. CohenS
GottliebBH
UnderwoodLG
2000 Social Relationships and Health.
CohenS
UnderwoodLG
GottliebBH
Measuring and intervening in social support New York Oxford University Press 3 25
6. CohenS
GottliebBH
UnderwoodLG
2001 Social relationships and health: challenges for measurement and intervention. Adv Mind Body Med 17 129 141
7. CohenS
2004 Social relationships and health. Am Psychol 59 676 684
8. ThoitsPA
1983 Multiple identities and psychological well-being: A reformulation and test of the social isolation hypothesis. Am Sociol Rev 48 174 187
9. BrissetteI
CohenS
SeemanTE
2000 Measuring social integration and social networks.
CohenS
UnderwoodLG
GottliebBH
Social support measurement and intervention: A guide for health and social scientists New York, NY, US Oxford University Press 53 85
10. ReinhardtJP
BoernerK
HorowitzA
2006 Good to have but not to use: Differential impact of perceived and received support on well-being. J Soc Pers Relat 23 117 129
11. LakeyB
CohenS
2000 Social support theory and measurement.
CohenS
UnderwoodLG
GottliebBH
Social support measurement and intervention: A guide for health and social scientists New York, NY, US Oxford University Press 29 52
12. CohenS
GottliebBH
UnderwoodLG
2000 Social relationships and health.
CohenS
UnderwoodLG
GottliebBH
Social support measurement and intervention: A guide for health and social scientists New York, NY, US Oxford University Press 3 25
13. DiMatteoMR
2004 Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol 23 207 218 (2004)
14. MurphyBM
ElliottPC
Le GrandeMR
HigginsRO
ErnestCS
2008 Living alone predicts 30-day hospital readmission after coronary artery bypass graft surgery. Eur J Cardiovasc Prev Rehabil 15 210 215
15. LettHS
BlumenthalJA
BabyakMA
CatellierDJ
CarneyRM
2007 Social support and prognosis in patients at increased psychosocial risk recovering from myocardial infarction. Health Psychol 26 418 427
16. KnoxSS
AdelmanA
EllisonRC
ArnettDK
SiegmundK
2000 Hostility, social support, and carotid artery atherosclerosis in the National Heart, Lung, and Blood Institute Family Heart Study. Am J Cardiol 86 1086 1089
17. KopWJ
BermanDS
GransarH
WongND
Miranda-PeatsR
2005 Social network and coronary artery calcification in asymptomatic individuals. Psychosom Med 67 343 352
18. BrummettBH
BarefootJC
SieglerIC
Clapp-ChanningNE
LytleBL
2001 Characteristics of socially isolated patients with coronary artery disease who are at elevated risk for mortality. Psychosom Med 63 267 272
19. WangHX
MittlemanMA
LeineweberC
Orth-GomerK
2006 Depressive symptoms, social isolation, and progression of coronary artery atherosclerosis: the Stockholm Female Coronary Angiography Study. Psychother Psychosom 75 96 102
20. WangHX
MittlemanMA
Orth-GomerK
2005 Influence of social support on progression of coronary artery disease in women. Soc Sci Med 60 599 607
21. AngererP
SiebertU
KothnyW
MuhlbauerD
MudraH
2000 Impact of social support, cynical hostility and anger expression on progression of coronary atherosclerosis. J Am Coll Cardiol 36 1781 1788
22. KnoxSS
Uvnas-MobergK
1998 Social isolation and cardiovascular disease: an atherosclerotic pathway? Psychoneuroendocrinology 23 877 890
23. CohenS
WillsTA
1985 Stress, social support, and the buffering hypothesis. Psychol Bull 98 310 357
24. BorensteinM
HedgesL
HigginsJ
RothsteinH
2005 Comprehensive Meta-analysis Version 2, Biostat, Englewood NJ
25. CooperH
1998 Synthesizing research: A guide for literature reviews 3rd ed Thousand Oaks Sage
26. ShroutPE
FleissJL
1979 Intraclass correlations: Uses in assessing rater reliability. Psychol Bull 86 420 428
27. HedgesLV
VeveaJL
1998 Fixed - and random-effects models in meta-analysis. Psychological Methods 3 486 504
28. MostellerF
ColditzGA
1996 Understanding research synthesis (meta-analysis). Annual Review of Public Health 17 1 23
29. AhernD
GorkinL
AndersonJ
TierneyC
HallstromA
1990 Biobehavioral variables and mortality or cardiac arrest in the cardiac arrhythmia pilot study (CAPS). Am J Cardiol 66 59 62
30. AlterDA
ChongA
AustinPC
MustardC
IronK
2006 Socioeconomic status and mortality after acute myocardial infarction. Ann Intern Med 144 82 93
31. AnsteyJK
LuszczMA
2002 Mortality risk varies according to gender and change in depressive status in very old adults. Psychosom Med 64 880 888
32. AstrandNE
HansonBS
IsacssonSO
1989 Job demands, job decision latitude, job support, and social network factors as predictors of mortality in a Swedish pulp and paper company. Br J Ind Med 46 334 340
33. AvlundK
DamsgaardMT
HolsteinBE
1998 Social relations and mortality. An eleven year follow-up studey of 70 year-old men and women in Denmark. Soc Sci Med 47 635 643
34. AvlundK
LundR
HolsteinBE
DueP
Sakari-RantalaR
2004 The impact of structural and functional characteristics of social relations as determinants of functional decline. J Gerontol 59B s44 s51
35. BarefootJC
GrobaekM
JensenG
Schnohr
PrescottE
2005 Social network diversity and risks of ischemic heart disease and total mortality: Findings from the Copenhagen City Heart Study. Ame J Epidemiol 161 960 967
36. BerkmanLF
SymeSL
1979 Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. Am J Epidemiol 109 186 204
37. BerkmanLF
MelchiorM
ChastangJF
NiedhammerI
LeclercA
2004 Social integration and mortality: A prospective study of French employees of electricity of France-Gas of France: the GAZEL Cohort. Ame J Epidemiol 159 167 174
38. Birket-SmithM
KnudsenHC
NissenJ
BlegvadN
KøhlerO
1989 Life events and social support in prediction of stroke outcome. Psychother Psychosom 52 146 150
39. BlazerDG
1982 Social support and mortality in an elderly community population. Am J Epidemiol 115 684 694
40. BlazerD
HybelsC
PieperC
2001 The association of depression and mortality in elderly persons: a case for multiple, independent pathways. J Gerontol: Medical Sciences, 56A M505 M509
41. BowlingA
1989 Who dies after widow(er)hood? A discriminant analysis. Omega 19 135 153
42. BrownSL
NesseRM
VinokurAD
SmithDM
2003 Providing social support may be more beneficial than receiving it: Results from a prospective study of mortality. Psychol Sci 14 320 327
43. BrummettBH
MarkDB
SieglerIC
WilliamsRB
BabyakMA
2005 Perceived social support as a predictor of mortality of coronary patients: Effects of smoking, sedentary behavior, and depressive symptoms. Psychosom Med 67 40 45
44. BurgMM
BarefootJ
BerkmanL
CatellierDJ
CzajkowskiS
2005 ENRICHD Investigators. Low perceived social support and post-myocardial infarction prognosis in the enhancing recovery in coronary heart disease clinical trial: The effects of treatment. Psychosom Med 67 879 888
45. BurnsCM
CraftPS
RoderDM
2005 Does emotional support influence survival? Findings from a longitudinal study of patients with advanced cancer. Support Care Cancer 13 295 302
46. ButowPN
CoatesAS
DunnSM
1999 Psychosocial predictors of survival in Metastatic Melanoma. J Clin Oncol 17 2256 2263
47. BygrenLO
KonlaanBB
JohanssonS
1996 Attendance at cultural events, reading books or periodicals, and making music or singing in a choir as determinants for survival: Swedish interview survey of living conditions. BMJ 313(7072) 1577 1580
48. CaseRB
MossAJ
CaseN
McDermottM
EberlyS
1992 Living alone after myocardial infarction. JAMA 267 515 519
49. CassilethBR
WalshWP
LuskEJ
1988 Psychosocial correlates of cancer survival: A subsequent report 3 to 8 years after cancer diagnosis. J Clin Oncol 6 1753 1759
50. CeriaCD
MasakiKH
RodriguezBL
ChenR
YanoK
2001 The relationship of psychosocial factors to total mortality among older Japanese-American men: The Honolulu Heart Program. J Am Geriatr Soc 49 725 731
51. ChackoRC
HarperRG
GottoJ
1996 Young J. Psychiatric interview and psychometric predictors of cardiac transplant survival. Am J Psychiatry 153 1607 1612
52. ChristensenAJ
DorninkR
EhlersSL
SchultzSK
1999 Social Environment and Longevity in Schizophrenia. Psychosom Med 61 141 145
53. ChristensenAJ
WiebeJS
SmithTW
TurnerCW
1994 Predictors of survival among hemodialysis patients: Effect of perceived family support. Health Psychol 13 521 525
54. CohenCI
TeresiJ
HolmesD
1987 Social networks and mortality in an inner-city elderly population. Int J Aging Hum Dev 24 257 269
55. ColonEA
CalliesAL
PopkinMK
McGlavePB
1991 Depressed mood and other variables related to bone marrow transplantation survival in acute leukemia. Psychosomatics 32 420 425
56. CornmanJC
GoldmanN
GleiDA
WeinsteinM
ChangM
2003 Social ties and perceived support: Two dimensions of social relationships and health among the elderly in Taiwan. J Aging Health 15 616 644
57. CoyneJC
RohrbaughMJ
ShohamV
SonnegaJS
NichlasJM
2001 Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol 88 526 529
58. CreeM
SoskloneCL
BelseckE
HornigJ
McElhaneyJE
2000 Mortality and institutionalization following hip fracture. J Am Geriatr Soc 48 283 288
59. CuijpersP
2000 Mortality and depressive symptoms in inhabitants of residential homes. Int J Geriatr Psychiatry 16 131 138
60. DalgardOS
HaheimLL
1998 Psychosocial risk factors and mortality: A prospective study with special focus on social support, social participation, and locus of control in Norway. J Epidemiol Community Health 52 476 481
61. DevinsGM
MannJ
MandinH
PaulLC
HonsRB
1990 Psychological predictors of survival in end-stage renal disease. J Nerv Ment Dis 178 127 133
62. DickensCM
McGowanL
PervicalC
DouglasJ
TomensonB
2004 Lack of close confidant, but not depression, predicts further cardiac events after myocardial infarction. Heart 90 518 522
63. EllK
NishimotoR
MedianskyL
MantellJ
HamovitchM
1992 Social relations, social support, and survival among patients with cancer. J Psychosom Res 36 531 541
64. EngPM
RimmEB
FitzmauriceG
KawachiI
2002 Social ties and change in social ties in relation to subsequent total and cause-specific mortality and coronary heart disease incidence in men. Ame J Epidemiol 155 700 709
65. EngedalK
1996 Mortality in the elderly–A 3-year follow-up of an elderly community sample. Int J Geriatr Psychiatry 11 467 471
66. FarmerIP
MeyerPS
RamseyDJ
GoffDC
WearML
1996 Higher levels of social support predict greater survival following acute myocardial infarction: The Corpus Christi heart project. Behav Med 22 59 66
67. ForsterLE
StollerEP
1992 The impact of social support on mortality: A seven-year follow-up of older men and women. J App Gerontol 11 173 186
68. Frasure-SmithN
LesperanceF
GravelG
MassonA
JuneauM
2000 Social support, depression, and mortality during the first year after myocardial infarction. Circulation 101 1919 1924
69. FrickE
MotzkeC
FischerN
BuschR
BumederI
2005 Is perceived social support a predictor of survival from patients undergoing autologous peripheral blood stem cell transplantation? Psychooncology 14 759 770
70. FryPS
DebatsDL
2006 Sources of life strengths as predictors of late-life mortality and survivorship. Int J Aging Hum Dev 62 303 334
71. FuhrerR
DufouilC
AntonucciTC
ShipleyJM
HeimerC
1999 Psychological disorder and mortality in French older adults: do social relations modify the association? Am J Epidemiol 149 116 126
72. FunchDP
MarshallJ
1983 The role of stress, social support and age in survival from breast cancer. J Psychosom Res 27 77 83
73. GanziniL
SmithDM
FennDS
LeeMA
1997 Depression and mortality in medically ill older adults. J Am Geriatr Soc 45 307 312
74. GellertGA
MaxwellRM
SiegelBS
1993 Survival of breast cancer patients receiving adjunctive psychosocial support therapy: A 10-year follow-up study. J Clin Oncol 11 66 69
75. GilesLC
GlonekGFV
LuszczMA
AndrewsGR
2004 Effects of social networks on 10 year survival in very old Australians: The Australian longitudinal study of aging. J Epidemiol Community Health 59 547 579
76. GiraldiT
RodaniMG
CartelG
GrassiL
1997 Psychosocial factors and breast cancer: A 6-year Italian follow-up study. Psychother Psychosom 66 229 236
77. GlassTA
Mendes de LeonC
MarottoliRA
BerkmanLF
1999 Population based study of social and productive activities as predictors of survival among elderly Americans. BM J 319 478 483
78. GoldmanN
KorenmanS
WeinsteinR
1995 Marital status and health among the elderly. Soc Sci Med 40 1717 1730
79. GoodwinJS
SametJM
HuntWC
1996 Determinants of Survival in Older Cancer Patients. J Natl Cancer Inst 88 1031 1038
80. GorkinL
SchronEB
BrooksMM
WiklundI
KellenJ
1993 Psychosocial predictors of mortality in the cardiac arrhythmia suppression trial-1 (CAST-1). Am J Cardiol 71 263 267
81. GrandA
GrosclaudeP
BocquetH
PousJ
AlbaredeJL
1990 Disability, psychosocial factors, and mortality among the elderly in a rural French population. J Clin Epidemiol 43 773 783
82. GreenfieldTK
RehmJ
RogersJD
2002 Effects of depression and social integration on the relationship between alcohol consumption and all-cause mortality. Addiction 97 29 38
83. GreenwoodD
PackhamC
MuirK
MadeleyR
1995 How do economic status and social support influence survival after initial recovery from acute myocardial infarction? Soc Sci Med 40 639 647
84. GrodnerS
PrewittLM
JaworskiBA
MyersR
KaplanR
1996 The impact of social support in pulmonary rehabilitation of patients with chronic obstructive pulmonary disease. Ann Behav Med 18 139 145
85. GustafssonTM
IsacsonDGL
ThorslundM
1998 Mortality in elderly men and women in a Swedish municipality. Age Ageing 27 584 593
86. HallEM
JohnsonJV
TsouTS
1993 Women, occupation, and risk of cardiovascular morbidity and mortality. Occup Med 8 709 718
87. Helweg-LarsenM
KjollerM
ThonigH
2003 Do age and social relations moderate the relationship between self-rated health and mortality among adult Danes. Soc Sci Med 57 1237 1247
88. HerndonJE
FleishmanS
KornblithAB
KostyM
GreenMR
1999 Is quality of life predictive of the survival of patients with advanced nonsmall cell lung carcinoma. Cancer 85 333 340
89. HillTD
AngelJL
EllisonCG
AngelRJ
2005 Religious attendance and mortality: An 8-year follow-up of older Mexican Americans. J Gerontol 60B S102 S109
90. HirdesJP
ForbesWF
1992 The importance of social relationships, socioeconomic status, and health practices with respect to mortality among healthy Ontario males. J Clin Epidemiol 45 175 182
91. HoSC
1991 Health and social predictors of mortality in an elderly Chinese cohort. Ame J Epidemiol 133 907 921
92. HouseJS
RobbinsC
MetznerHL
1982 The association of social relationships and activities with mortality: Prospective evidence from the Tecumseh community health study. Ame J Epidemiol 116 123 140
93. HummerRA
RogersRG
NamCB
EllisonCG
1999 Religious involvement and U.S. adult mortality. Demography 36 273 285
94. IribarrenC
JacobsDR
KiefeCI
LewisCE
MatthewsKA
2005 Causes and demographic, medical, lifestyle and psychosocial predictors of premature mortality: The CARDIA study. Soc Sci Med 60 471 482
95. IrvineJ
BasinskiA
BakerB
JandciuS
PaquetteM
1999 Depression and risk of sudden cardiac death after acute myocardial infarction: testing for the confounding effects of fatigue. Psychosom Med 61 729 737
96. IwasakiM
OtaniT
SunagaR
MiyazakiH
XiaoL
2002 Social networks and mortality base on the Komo-ise cohort study in Japan. Int J Epidemiol 31 1208 1218
97. JohnsonJE
FinneyJW
MoosRH
2005 Predictors of 5-year mortality following inpatients/residential group treatment of substance use disorders. Addict Behav 30 1300 1316
98. JohnsonJV
StewartW
HallEM
FredlundP
TheorellT
1996 Long-term psychosocial work environment and cardiovascular mortality among Swedish men. Am J Public Health 86 324 331
99. JormAF
HendersonAS
KayDWK
JacombPA
1991 Mortality in relation to dementia, depression, and social integration in an elderly community sample. Int J Geriatr Psychiatry 6 5 11
100. JuonH
EnsmingerME
FeehanM
1989 Childhood adversity and later mortality in an urban African American cohort. Am J Public Health 93 2044 2046
101. JylhäM
AroS
1989 Social ties and survival among the elderly in Tampere, Finland. Int J Epidemiol 18 158 173
102. KaplanGA
SalonenJT
CohenRD
BrandRJ
SymeSL
1988 Social connections and mortality from all causes and from cardiovascular disease: Prospective evidence from eastern Finland. Ame J Epidemiol 28 370 380
103. KaplanGA
WilsonTW
CohenRD
KauhanenJ
WuM
1994 Social functioning and overall mortality: Prospective evidence from the Kuipio ischemic heart disease risk factor study. Epidemiology 5(5) 495 500
104. KawachiI
ColditzGA
AscherioA
RimmEB
GiovannucciE
1996 A prospective study of social networks in relation to total mortality and cardiovascular disease in men in the USA. J Epidemiol Community Health 50 245 251
105. KellerBK
MagnusonTM
CerninPA
StonerJA
PotterJF
2003 The significance of social network in a geriatric assessment population. Aging Clin Exp Res 15 512 517
106. KielyDK
SimonSE
JonesRN
MorrisJN
2000 The protective effect of social engagement on mortality in long-term care. J Am Geriatr Soc 48 1367 1372
107. KimmelPL
PetersonRA
WeihsKL
ShidlerN
SimmensSJ
2000 Dyadic relationship conflict, gender, and mortality in Urban hemodialysis patients. J Am Soc Nephrol 11(8) 1518 1525
108. KortenAE
JormAF
JaioZ
LetenneurL
JacombPA
1999 Health, cognitive, and psychosocial factors as predictors of mortality in an elderly community sample. J Epidemiol Community Health 53 83 88
109. KrauseN
1997 Received support, anticipated support, social class, and mortality. Res Aging 19 387 422
110. KrauseN
2006 Church-based social support and mortality. J Gerontol 61B(3) S140 S146
111. KroenkeCH
KubzanskyLD
SchernhammerES
HolmesMD
KawachiI
2006 Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol 24 1105 1111
112. La CourP
AvlundK
Schultz-LarsenK
2005 Religion and survival in a secular region. A twenty year follow-up of 734 Danish adults born in 1914. Soc Sci Med 62 157 164
113. LeeM
Rotheram-BorusMJ
2001 Challenges associated with increased survival among parents living with HIV. Am J Public Health 91 1303 1309
114. LehtoUS
OjanenM
DybaT
AromaaA
Kellokumpu-LehtinenP
2006 Baseline psychosocial predictors of survival in localized breast cancer. Br J Cancer 94 1245 1252
115. LennartssonC
SilversteinM
2001 Does engagement with life enhance survival of elderly people in Sweden? The role of social and leisure activities. J Gerentol 56B S335 S342
116. LjungquistB
BergS
SteenB
1995 Prediction of survival in 70-year olds. Arch Gerontol Geriatr 20 295 307
117. LundR
DueP
ModvigJ
HolsteinBE
DamsgaardMT
2002 Cohabitation and marital status as predictors of mortality–an eight year follow-up study. Soc Sci Med 55 673 679
118. LundR
ModvigJ
DueP
HolsteinBE
2000 Stability and change in structural social relations as predictor or mortality among elderly women and men. Eur J Epidemiol 16 1087 1097
119. LyyraT
HeikkinenR
2006 Perceived social support and mortality in older people. J Gerontol 61B S147 S152
120. MaierD
SmithJ
1999 Psychological predictors of mortality in old age. J Gerontol: Series B: Psychol Scis & Social Sciences 54B 44 54
121. MalmstromM
JohanssonS
SundquistJ
2001 A hierarchical analysis of long-term illness and mortality in socially deprived areas. Soc Sci Med 3 265 275
122. McClellanWM
StanwyckDJ
AnsonCA
1993 Social support and subsequent mortality among patients with end-stage renal disease. J Am Soc Nephrol 4 1028 1034
123. MerloJ
OstergrenP
ManssonN
HansonBS
RanstamJ
2000 Mortality in elderly men with low psychosocial coping resources using anxiolytic-hypnotic drugs. 1403–4948 28 294 297
124. MertensJR
MoosRH
BrennanPL
1996 Alcohol consumption, life context, and coping predict mortality among late-middle-aged drinkers and former drinkers. Alcohol Clin Exp Res 20 313 319
125. MorrisPLP
RobinsonRG
AndrzejewskiP
SamuelsJ
PriceTR
1993 Association of depression with 10-year post stroke mortality. Am J Psychiatry 150 124 129
126. MurataC
KondoT
HoriY
MiyaoD
TamakoshiK
2005 Effects of social relationships on mortality among the elderly in a Japanese rural area: An 88-month follow-up study. J Epidemiol 15 78 84
127. MurbergTA
BruE
2001 Social relationships and mortality in patients with congestive heart failure. J Psychosom Res 51 521 527
128. MusickMA
HouseJS
WilliamsDR
2004 Attendance at religious services and mortality in a national sample. J Health Soc Behav 45 198 213
129. NakanishiN
TataraK
2000 Correlates and prognosis in relation to participation in social activities among older people living in a community in Osaka, Japan. Journal of Clinical Geropsychology 6 299 307
130. NordentoftM
BreumL
MunckLK
NordestgaardAG
HundingA
BjaeldagerPAL
1993 High mortality by natural and unnatural causes: A 10 year follow up study of patients admitted to a poisoning treatment centre after suicide attempts. Br Med J 306(6893) 1637 1641
131. OlsenRB
OlsenJ
Gunner-SvenssonF
WaldstromB
1991 Social networks and longevity: A 14 year follow-up study among elderly in Denmark. Soc Sci Med 33 1189 1195
132. OmanD
ReedD
1998 Religion and mortality among the community-dwelling elderly. Am J Public Health 88 1469 1475
133. OrrellM
ButlerR
BebbingtonP
2000 Social factors and the outcome of dementia. Int J Geriatr Psychiatry 15 515 520
134. Orth-GomerK
JohnsonJV
1987 Social network interaction and mortality. J Chronic Dis 40 949 957
135. Orth-GomerK
UndenAL
1990 Type A behavior, social support, and coronary risk: Interaction and significance for mortality in cardiac patients. Psychosom Med 52 59 72
136. OstbyeT
KrauseKM
NortonMC
TschanzJ
SandersL
2006 Cache County Investigators, Ten dimensions of health and their relationships with overall self-reported health and survival in a predominately religiously active elderly population: The Cache County memory study. J Am Geriatr Soc 54 199 209
137. OxmanTE
FreemanDH
ManheimerED
1995 Lack of social participation or religious strength and comfort as risk factors for death after cardiac surgery in the elderly. Psychosom Med 57 5 15
138. ParkersonGR
GutmanRA
2000 Health-related quality of life predictors of survival and hospital utilization. Health Care Financ Rev 21 171 184
139. PennixBWJH
TilburgT
KriegsmanDMW
DeegDJH
1997 Effects of social support and personal coping resources on mortality in older age: The longitudinal aging study Amsterdam. Am J Epidemiol 146 510 519
140. RasuloD
ChristensenK
TomassiniC
2005 The influence of social relations on mortality in later life: A study on elderly Danish twins. Gerontologist 45 601 609
141. ReubenDB
RubensteinLV
HirschSH
HaysRD
1992 Value of functional status as a predictor of mortality: Results of a prospective study. Am J Med 93 663 669
142. ReynoldsP
BoydPT
BlacklowRS
JacksonJS
GreenbergRS
1994 The relationship between social ties and survival among Black and White breast cancer patients. Cancer Epidemiol Biomarkers Prev 1055–9965 3 252 259
143. Rodriguez-ArtalejoF
Guallar-CastillonP
HerreraMC
OteroCM
ChivaMO
2006 Social network as a predictor of hospital readmission and mortality among older patients with heart failure. J Card Fail 12 621 627
144. RosengrenA
Orth-GomerK
WilhelmsenL
1998 Socioeconomic differences in health indices, social networks and mortality among Swedish men: A study of men born in 1933. Scand J Soc Med 26 272 280
145. RoyAW
FitzGibbonPA
HaugMM
1996 Social support, household composition, and health behaviors as risk factors for four-year mortality in an urban elderly cohort. J App Gerontol 15 73 86
146. RozziniR
BianchettiA
FranzoniS
ZanettieO
TrabucchiM
1991 Social, functional, and health status influences on mortality: Consideration of a multidimensional inquiry in a large elderly population. J Cross Cult Gerontol 6 83 90
147. RubermanW
WeinblattE
GoldbergJD
ChaudharyBS
1984 Psychosocial influences on mortality after myocardial infarction. N Engl J Med 9 552 559
148. RutledgeT
MatthewsK
LuiL
StoneKL
CauleyJA
2003 Social networks and marital status predict mortality in older women: Prospective evidence from the Study of Osteoporotic Fractures (SOF). Psychosom Med 65 688 694
149. RutledgeT
ReisSE
OlsonM
OwensJ
KelseySF
2004 National Heart, Lung, and Blood Institute, Social networks are associated with lower mortality rates among women with suspected coronary disease: the National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation Study. Psychosom Med 66 882 888
150. Saito-NakayaK
NakayaN
FujimoriM
AkizukiN
YoshikawaE
KobayakawaM
NagaiK
NishiwakiN
TsubonoY
UchitomiY
2006 Marital status, social support and survival after curative resection in non-small-cell lung cancer. Cancer Sci 97 206 213
151. SchoenbachVJ
KaplanBH
FredmanL
KleinbaumDG
1986 Social ties and mortality in Evans County, Georgia. Am J Epidemiol 123 577 591
152. SeemanT
BerkmanL
KohoutF
LacroixA
GlynnR
1993 Intercommunity variations in the association between social ties and mortality in the elderly: A comparative analysis of three communities. Eur Psychiatry 4 325 335
153. ShahatahmasebiS
DaviesR
WengerGC
1992 A longitudinal analysis of factors related to survival in old age. Gerontologist 32 404 413
154. ShmotkinD
BlumsteinT
ModanB
2003 Beyond keeping active: Concomitants of being a volunteer in old-old age. Psychol Aging 18 602 607
155. ShyeD
MulloolyJP
FreebornDK
PopeCR
1995 Gender differences in the relationship between social network support and mortality: A longitudinal study of an elderly cohort. Soc Sci Med 41 935 947
156. SilversteinM
BengtsonVL
1991 Do close parent-child relations reduce the mortality risk of older parents? J Health Soc Behav 32 382 395
157. Soler-VilaH
KaslSV
JonesBA
2003 Prognostic significance of psychosocial factors in African-American and White breast cancer patients: A population based study. Cancer 98 1299 1308
158. StavrakyKM
DonnerAP
KincadeJE
StewartMA
1988 The effect of psychosocial factors on lung cancer mortality at one year. J Clin Epidemiol 41 75 82
159. StekML
VinkersDJ
GusseklooJ
BeekmanATF
Van der MastRC
2005 Is depression in old age fatal only when people feel lonely? The Am J Psychiatry 162 178 180
160. SturdyPM
VictorCR
AndersonHR
BlandJM
ButlandBK
2002 Psychological, social and health behavior risk factors for deaths certified as asthma: A national case-control study. Thorax 57 1034 1039
161. SugisawaH
LiangJ
LiuX
1994 Social networks, social support, and mortality among older people in Japan. J Gerontol 49 S3 S13
162. SunR
LiuY
2006 Mortality of the oldest old in China: The role of social and solitary customary activities. J Aging Health 18 37 55
163. Temkin-GreenerH
BajorskaA
PetersonDR
KunitzSJ
GrossD
2004 Social support and risk-adjusted mortality in a frail, older population. Med Care 42 779 788
164. ThomasSA
FriedmannE
WimbushF
SchronE
1997 Psychosocial factors and survival in the Cardiac Arrhythmia Suppression Trial (CAST): A reexamination. Am J Crit Care 6 116 126
165. TuckerJS
FriedmanHS
WingardDL
SchwartzJE
1996 Marital history at midlife as a predictor of longevity: alternative explanations to the protective effects of marriage. Health Psychol 15 94 101
166. VaillantGE
MeyerSE
MukaamalK
SoldzS
1998 Are social supports in late midlife a cause or a result of successful physical ageing? Psychol Med 28 1159 1168
167. VogtTM
MulloollyDE
ErnstE
PopeCR
HollisJF
1992 Social networks as predictors of ischemic heart disease, cancer, stroke, and hypertension: incidence, survival, and mortality. J Clin Epidemiol 45 659 666
168. Walter-GinzburgA
BlumsteinT
ChetritA
ModanB
2002 Social factors and mortality in old-old in Israel: The CALAS study. J Gerontol 57b S308 S318
169. Waxler-MorrisonN
HislopG
MearsB
KanL
1991 Effects of social relationships on survival for women with breast cancer: A prospective study. Soc Sci Med 33 177 183
170. WeihsKL
SimmensSJ
MizrahiJ
EnrightTM
HuntME
2005 Dependable social relationships predict overall survival in stages II and III breast carcinoma patients. J Psychosom Res 59 299 306
171. WelinC
LappasG
WilhelmsenL
2000 Independent importance of psychosocial factors for prognosis after myocardial infarction. J Intern Med 247 629 639
172. WelinL
LarssonB
SvardsuddK
TibblinB
TibblinG
1992 Social network and activities in relation to mortality from cardiovascular diseases, cancer, and other causes: A 12 year follow up of the Study of Men Born in 1913 and 1923. Journal of Epidemiology and Community Health 46 127 132
173. WilkinsK
2003 Social support and mortality in seniors. Health Rep 14 21 34
174. WoloshinS
SchwartzLM
TostesonANA
ChangCH
WrightB
1997 Perceived adequacy of tangible social support and health outcomes in patients with coronary artery disease. J Gen Intern Med 12 613 618
175. YasudaN
ZimmermanSI
HawkesW
FredmanL
HebelJR
1997 Relation of social network characteristics to 5-year mortality among young-old versus old-old White women in an urban community. Am J Epidemiol 145 516 523
176. ZuckermanDM
KaslSV
OstfeldAM
1984 Psychosocial predictors of mortality among the elderly poor. Am J Epidemiol 19 410 423
177. Rosenthal, The file drawer problem and tolerance for null results. Psychol Bull 86 638 641
178. DuvalS
TweedieR
2000 A non-parametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc 95 89 98
179. DuvalS
TweedieR
2000 Trim and fill: A simple funnel-plot based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56 455 463
180. PetersJL
SuttonAJ
JonesDR
AbramsKR
RushtonL
2006 Comparison of two methods to detect publication bias in meta-analysis. JAMA 295 676 680
181. PetersJ
SuttonA
JonesD
AbramsK
RushtonL
Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. Journal Of Clinical Epidemiology October 2008;61 991 996
182. UchinoBN
2006 Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med 29 377 387
183. SametJM
1990 The 1990 Report of the Surgeon General: The Health Benefits of Smoking Cessation. Am Rev Respir Dis 142 993 994
184. FriedmanHS
TuckerJS
SchwartzJE
Tomlinson-KeaseyC
MartinLR
1995 Psychosocial and behavioral predictors of longevity: The aging and death of the ‘Termites’. Am Psychol 50 69 78
185. TuckerJS
FriedmanHS
WingardDL
SchwartzJE
1996 Marital history at midlife as a predictor of longevity: Alternative explanations to the protective effect of marriage. Health Psychol 15 94 101
186. CoyneJC
RohrbaughMJ
ShohamV
SonnegaJS
NicklasJM
2001 Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol 88 526 529
187. EakerED
SullivanLM
Kelly-HayesM
D'AgostinoRBSr
BenjaminEJ
2007 Marital status, marital strain, and risk of coronary heart disease or total mortality: the Framingham Offspring Study. Psychosom Med 69 509 513
188. RothmanKJ
GreenlandS
LashTL
2008 Modern Epidemiology Philadelphia Lippincott Williams & Wilkins
189. UchinoBN
CacioppoJT
Kiecolt-GlaserJK
1996 The relationship between social support and physiological processes: A review with emphasis on underlying mechanisms and implications for health. Psychol Bull 119 488 531
190. RozanskiA
BlumenthalJA
KaplanJ
1999 Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 99 2192 2217
191. CohenS
1988 Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol 7 269 297
192. UchinoBN
Holt-LunstadJ
UnoD
CampoR
ReblinM
2007 The Social Neuroscience of Relationships: An Examination of Health-Relevant Pathways. Social neuroscience: Integrating biological and psychological explanations of social behavior New York, NY, US Guilford Press 474 492
193. UchinoBN
UnoD
Holt-LunstadJ
1999 Social support, physiological processes, and health. Curr Dir Psychol Sci 8 145 148
194. LutgendorfSK
SoodAK
AndersonB
McGinnS
MaiseriH
2005 Social support, psychological distress, and natural killer cell activity in ovarian cancer. J Clin Oncol 23 7105 7113
195. MiyazakiT
IshikawaT
NakataA
SakuraiT
MikiA
2005 Association between perceived social support and Th1 dominance. Biol Psychol 70 30 37 (2005)
196. MoynihanJA
LarsonMR
TreanorJ
DubersteinPR
PowerA
2004 Psychosocial factors and the response to influenza vaccination in older adults. Psychosom Med 66 950 953
197. CohenS
DoyleWJ
SkonerDP
RabinBS
GwaltneyJMJr
1997 Social ties and susceptibility to the common cold. JAMA 277 1940 1944
198. Kiecolt-GlaserJK
LovingTJ
StowellJR
MalarkeyWB
LemeshowS
2005 Hostile marital interactions, proinflammatory cytokine production, and wound healing. Arch Gen Psychiatry 62 1377 1384
199. SpiegelD
BloomJR
KraemerH
GottheilE
1989 Psychological support for cancer patients. Lancet 2(8677) 1447
200. AltmanDG
1995 Sustaining interventions in community systems: On the relationship between researchers and communities. Health Psychology 14 526 536
201. SpitzRA
1945 Hospitalism: An inquiry into the genesis of psychiatric conditions in early childhood. Psychoanalytic Study of the Child 1 53 74
202. BowlbyJ
1951 Maternal care and mental health Geneva WHO
203. ProvenceSA
LiptonRC
1962 Infants in institutions New York International Universities Press
204. UNICEF 1997 Children at risk in Central and Eastern Europe: Perils and promises Florence, Italy United Nations Children's Fund, International Child Development Centre
205. ShavelleRM
PaculdoDR
StraussDJ
KushSJ
2008 Smoking habit and mortality: a meta-analysis. J Insur Med 40 170 178
206. CritchleyJA
CapewellS
2003 Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic review. JAMA 290 86 97
207. HolmanCD
EnglishDR
MilneE
WinterMG
1996 Meta-analysis of alcohol and all-cause mortality: a validation of NHMRC recommendations. Med J Aust 164 141 145
208. FineMJ
SmithMA
CarsonCA
MeffeF
SankeySS
1994 Efficacy of pneumococcal vaccination in adults. A meta-analysis of randomized controlled trials. Arch Intern Med 154 2666 2677
209. TaylorRS
BrownA
EbrahimS
JolliffeJ
NooraniH
2004 Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med 116 682 692
210. KatzmarzykPT
JanssenI
ArdernCI
2003 Physical inactivity, excess adiposity and premature mortality. Obes Rev 4 257 290
211. InsuaJT
SacksHS
LauTS
LauJ
ReitmanD
1994 Drug treatment of hypertension in the elderly: a meta-analysis. Ann Intern Med 121 355 362
212. SchwartzJ
1994 Air pollution and daily mortality: a review and meta analysis. Environ Res 64 36 52
213. BarreraM
SandlerI
RamsayT
1981 Preliminary development of a scale of social support: Studies on college students. Am J Commun Psychol 9 435 441
214. Dunkel-SchetterC
FolkmanS
LazarusR
1987 Correlates of social support receipt. J Pers Soc Psychol 53 71 80
215. Dunkel-SchetterC
FeinsteinL
CallJ
1987 UCLA Social Support Inventory. Unpublished manuscript, University of California, Los Angeles
216. VauxA
RiedelS
StewartD
1987 Models of social support: The social support behaviors (SS-B) scale. Am J Commun Psychol 15 209 237
217. SeemanTE
BerkmanLF
1988 Structural characteristics of social support networks and their relationship with social support in the elderly: Who provides support. Soc Sci Med 26 737 794
218. HansonBS
OstergrenP-O
ElmstahlS
IsacssonS-O
RanstamJ
1997 Reliability and validity assessments of measures of social networks, social support and control — results from the Malmo Shoulder and Neck Study. Scand J Soc Med 25 249 257
219. SarasonIG
LevineHM
BashamRB
SarasonBR
1983 Assessing social support: The social support questionnaire. J Pers Soc Psychol 44 217 139
220. CohenS
HobermanHM
1983 Positive events and social support as buffers of life change stress. J Appl Soc Psychol 13 99 125
221. De Jong-GierveldJ
KamphuisF
1985 The development of a Rasch-type loneliness scale. Appl Psych Meas 9 289 299
222. RussellD
PeplauLA
CutronaCE
1980 The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. J Pers Soc Psychol 39 472 480
223. KahnRL
AntonucciTC
1980 Convoys over the life course: Attachment, roles and social support.
BaltesPB
Brim0
Life span development and behavior New York, NY Academic Press 253 286
224. HirschBJ
1979 Psychological dimensions of social networks: A multi-method analysis. Am J Commun Psychol 163 277
225. HansonBS
OstergrenP-O
ElmstahlS
IsacssonS-O
RanstamJ
1997 Reliability and validity assessments of measures of social networks, social support and control — results from the Malmo Shoulder and Neck Study. Scand J Soc Med 25 249 257
226. CohenS
1991 Social supports and physical health.
GreeneAL
CummingsM
KarrakerKH
Life-Span Developmental Psychology: Perspectives on Stress and Coping Hillsdale, NJ Erlbaum Associates
227. CohenS
DoyleWJ
SkonerDP
RabinBS
GwaltneyJM
1997 Social ties and susceptibility to the common cold. JAMA 277 1940 1944
228. KahnRL
AntonucciTC
1984 Social supports of the elderly: Family, friends, professionals (Refort No. AGO 01632) Bethesda, MD National Institute on Aging
229. DonaldCA
WareJE
1984 The measurement of social support. Res Commun Mental Health 4 334 335
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2010 Číslo 7- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
-
Všechny články tohoto čísla
- Estimating the Number of Paediatric Fevers Associated with Malaria Infection Presenting to Africa's Public Health Sector in 2007
- HIV in Maternal and Child Heath: Concurrent Crises Demand Cooperation
- HIV Testing for Children in Resource-Limited Settings: What Are We Waiting For?
- Improving Implementation: Building Research Capacity in Maternal, Neonatal, and Child Health in Africa
- Evidence-Based Priority Setting for Health Care and Research: Tools to Support Policy in Maternal, Neonatal, and Child Health in Africa
- Three Adult Cases of Meningitis in Vietnam
- Integrative Genomic Analyses Identify as a Novel Lineage-Specific Oncogene in Lung Squamous Cell Carcinoma
- Association of Early Repolarization Pattern on ECG with Risk of Cardiac and All-Cause Mortality: A Population-Based Prospective Cohort Study (MONICA/KORA)
- Stable and Unstable Malaria Hotspots in Longitudinal Cohort Studies in Kenya
- A Model for the Roll-Out of Comprehensive Adult Male Circumcision Services in African Low-Income Settings of High HIV Incidence: The ANRS 12126 Bophelo Pele Project
- Left to Their Own Devices: Breakdowns in United States Medical Device Premarket Review
- A Six-Gene Signature Predicts Survival of Patients with Localized Pancreatic Ductal Adenocarcinoma
- Financing Maternal and Child Health—What Are the Limitations in Estimating Donor Flows and Resource Needs?
- Improving Prevention of Mother-to-Child Transmission of HIV Care and Related Services in Eastern Rwanda
- Social Relationships and Mortality Risk: A Meta-analytic Review
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Three Adult Cases of Meningitis in Vietnam
- Left to Their Own Devices: Breakdowns in United States Medical Device Premarket Review
- Social Relationships and Mortality Risk: A Meta-analytic Review
- Evidence-Based Priority Setting for Health Care and Research: Tools to Support Policy in Maternal, Neonatal, and Child Health in Africa
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání