-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
HIF–VEGF Pathways Are Critical for Chronic Otitis Media in and Mouse Mutants
Otitis media with effusion (OME) is the commonest cause of hearing loss in children, yet the underlying genetic pathways and mechanisms involved are incompletely understood. Ventilation of the middle ear with tympanostomy tubes is the commonest surgical procedure in children and the best treatment for chronic OME, but the mechanism by which they work remains uncertain. As hypoxia is a common feature of inflamed microenvironments, moderation of hypoxia may be a significant contributory mechanism. We have investigated the occurrence of hypoxia and hypoxia-inducible factor (HIF) mediated responses in Junbo and Jeff mouse mutant models, which develop spontaneous chronic otitis media. We found that Jeff and Junbo mice labeled in vivo with pimonidazole showed cellular hypoxia in inflammatory cells in the bulla lumen, and in Junbo the middle ear mucosa was also hypoxic. The bulla fluid inflammatory cell numbers were greater and the upregulation of inflammatory gene networks were more pronounced in Junbo than Jeff. Hif-1α gene expression was elevated in bulla fluid inflammatory cells, and there was upregulation of its target genes including Vegfa in Junbo and Jeff. We therefore investigated the effects in Junbo of small-molecule inhibitors of VEGFR signaling (PTK787, SU-11248, and BAY 43-9006) and destabilizing HIF by inhibiting its chaperone HSP90 with 17-DMAG. We found that both classes of inhibitor significantly reduced hearing loss and the occurrence of bulla fluid and that VEGFR inhibitors moderated angiogenesis and lymphangiogenesis in the inflamed middle ear mucosa. The effectiveness of HSP90 and VEGFR signaling inhibitors in suppressing OM in the Junbo model implicates HIF–mediated VEGF as playing a pivotal role in OM pathogenesis. Our analysis of the Junbo and Jeff mutants highlights the role of hypoxia and HIF–mediated pathways, and we conclude that targeting molecules in HIF–VEGF signaling pathways has therapeutic potential in the treatment of chronic OM.
Published in the journal: . PLoS Genet 7(10): e32767. doi:10.1371/journal.pgen.1002336
Category: Research Article
doi: https://doi.org/10.1371/journal.pgen.1002336Summary
Otitis media with effusion (OME) is the commonest cause of hearing loss in children, yet the underlying genetic pathways and mechanisms involved are incompletely understood. Ventilation of the middle ear with tympanostomy tubes is the commonest surgical procedure in children and the best treatment for chronic OME, but the mechanism by which they work remains uncertain. As hypoxia is a common feature of inflamed microenvironments, moderation of hypoxia may be a significant contributory mechanism. We have investigated the occurrence of hypoxia and hypoxia-inducible factor (HIF) mediated responses in Junbo and Jeff mouse mutant models, which develop spontaneous chronic otitis media. We found that Jeff and Junbo mice labeled in vivo with pimonidazole showed cellular hypoxia in inflammatory cells in the bulla lumen, and in Junbo the middle ear mucosa was also hypoxic. The bulla fluid inflammatory cell numbers were greater and the upregulation of inflammatory gene networks were more pronounced in Junbo than Jeff. Hif-1α gene expression was elevated in bulla fluid inflammatory cells, and there was upregulation of its target genes including Vegfa in Junbo and Jeff. We therefore investigated the effects in Junbo of small-molecule inhibitors of VEGFR signaling (PTK787, SU-11248, and BAY 43-9006) and destabilizing HIF by inhibiting its chaperone HSP90 with 17-DMAG. We found that both classes of inhibitor significantly reduced hearing loss and the occurrence of bulla fluid and that VEGFR inhibitors moderated angiogenesis and lymphangiogenesis in the inflamed middle ear mucosa. The effectiveness of HSP90 and VEGFR signaling inhibitors in suppressing OM in the Junbo model implicates HIF–mediated VEGF as playing a pivotal role in OM pathogenesis. Our analysis of the Junbo and Jeff mutants highlights the role of hypoxia and HIF–mediated pathways, and we conclude that targeting molecules in HIF–VEGF signaling pathways has therapeutic potential in the treatment of chronic OM.
Introduction
Chronic middle ear effusion without the symptoms of acute infection is termed otitis media (OM) with effusion and can be sequel to acute bacterial otitis media. Otitis media with effusion (OME) is the most common cause of hearing impairment in children potentially causing language delays, learning and behavioral problems [1], [2]. About 2.2 million episodes of OME occur annually in the US with an annual cost estimate of $4.0 billion [3].The prolonged ventilation of the middle ear with tympanostomy tubes, also known as grommets, remains the best treatment for OME [4]. Placement of tympanostomy tubes is the most common operation in the UK (30,000 procedures per annum) however the mechanism by which they work remains uncertain. As hypoxia is a common feature of inflamed microenvironments [5], [6] the therapeutic benefits of ventilating the middle ear may conceivably include the moderation of hypoxia as well as relieving negative pressure and fluid drainage.
Responses to hypoxia are mediated by Hypoxia Inducible Factor (HIF) protein a transcription factor that induces genes whose products restore blood supply, nutrients and energy production to maintain tissue homeostasis. Constitutively expressed HIF-1α is modified by prolyl hydroxylase domain (PHD) enzymes under normoxic conditions and targeted for proteasomal degradation. Under hypoxic conditions PHD activity is limited and HIF-1α is stabilized and forms a heterodimer with HIF-1β before translocation to the nucleus where it binds to hypoxic response elements [7]. HIF signaling is also regulated by inflammation at the transcriptional level via HIF-1α interactions with the master regulator of inflammation NF-κB [8]–[10] and at the translational level by cytokines such as IL-1β and TNF-α [5], [6]. HIF responses are adaptive and help overcome localized ischemia as well as regulating innate immune responses to microbial infections [11] but chronic hypoxic inflammation may result in dysregulated HIF signaling and lead to pathological outcomes. Examples include fibrosis via immune cell activation [6] and the progression of rheumatoid arthritis [12] via angiogenesis caused by HIF-induced vascular endothelial growth factor (VEGF). Indeed, treatment using VEGF receptor (VEGFR) signaling inhibitors moderates experimentally-induced arthritis [13].
Although hypoxia might be expected in the inflammatory conditions of chronic OM the evidence is inconsistent. Some studies have found that OME fluids in the middle ear cavity (bulla) have oxygen tensions similar to venous blood, of ∼40 Torr [14], [15]. Another study reported pO2 in mucoid and serous OME fluids were lower ∼29–32 Torr. However, these values were not significantly different than pO2 values in barotrauma bulla fluids [16]. Nevertheless, there are a few studies to suggest that the downstream HIF signaling protein VEGF plays a role in experimental and clinical OME. Injection of recombinant VEGF into the rat bulla causes fluid effusion, mucosal inflammation and an increase in vascular permeability [17]. Vegf, Vegfr1 (also known as Flt1) and Vegfr2 (also known as Kdr) gene and protein expression are upregulated in the endotoxin-induced rat model of OME [18], [19] and Vegf protein is elevated in mouse middle and inner ear tissue after challenge with Haemophilus influenzae [20]. Moreover VEGF mRNA and protein are detectable in bulla fluids of patients with OME [18], [21]. However, these studies have not investigated the role of hypoxia and HIF signaling in the inflamed middle ear.
There is a significant genetic component predisposing to recurrent or chronic OM in human populations [22]–[26]. However, while a number of association studies have been carried out, sample sizes are relatively small and confirmation will be required through larger scale analyses and replication. A number of underlying OM susceptibility genes have been discovered in the mouse which represents a powerful model for dissecting the underlying pathways. These genes apppear to fall into three categories; those which are involved in craniofacial development and thereby Eustachian tube morphology and function, TLR4/MyD88 pathway genes that regulate innate immune function, and TGF-β pathway genes that modulate pro-inflammatory responses [27]. The two OM mouse mutants Junbo and Jeff, generated by N′-ethyl-N′-nitrosourea mutagenesis, represent powerful models for human OM as unlike many other mouse mutants they are non-syndromic and do not show the wide-ranging pleiotropic effects often associated with middle ear inflammatory disease in other models [27]. Jeff encodes a mutation in the Fbxo11 protein [28] and Junbo encodes a mutation in the transcription factor Evi1 [29]. Heterozygote Junbo (Jbo/+) and Jeff (Jf/+) mice develop OM spontaneously in the absence of other organ pathology or overt immune deficiency [28], [29]. There is an association between polymorphisms in FBXO11, the human homologue of the Jeff mutant protein, in OME and recurrent OM [24] and severe OM [25], but there is no such association with EVI1 polymorphisms.
In this work we have analyzed the two OM mouse models Junbo and Jeff by hypoxia labeling, transcriptional profiling and, in Junbo, using small-molecule inhibitors. We have discovered that the response to chronic inflammatory hypoxia via Hif-1α signaling and VEGF pathways is critical for chronic OM. Our analysis of the two mutants provides insight into the molecular and genetic mechanisms of OM and identifies potential new therapeutic targets for OM.
Results
Hypoxia in the middle ear
We surmised that the inflamed microenvironment in chronic OM is hypoxic and proceeded to test this hypothesis by the analysis of the Junbo and Jeff mutants. To test whether the inflammatory cells that accumulate within the middle ear were hypoxic we injected mice in vivo with pimonidazole (PIMO), a marker that labels cells and tissues with a pO2<10 Torr (∼1.5% O2). FACS analysis revealed hypoxia in viable and apoptotic polymorphonuclear cell (PMN) populations in the purulent bulla fluids of Jbo/+ (7.1±1.7×106 cells per µl, n = 10) and serous effusions of Jf/+ mice (55±25×103 cells per µl, n = 5) (Figure 1H and Table 1). In addition, immunohistochemistry showed hypoxia in F4/80-positive foamy macrophages (mΦ) within the bulla, the epithelium and in the connective tissues of the thickened, inflamed middle ear mucosa of Jbo/+ mice (Figure 1A, 1C, 1D, 1G) but not in the normal thin mucosa of wild type (+/+) mice (Figure 1B). Hypoxia was evident at 4 wk, increased at 7–8 wk and remained chronically elevated for >30 wk (Figure 1E). The only part of the tubotympanum that appeared hypoxic under normal physiological conditions was the Eustachian tube (Figure 1F). In Jf/+ mice PIMO labeling was restricted to inflammatory cells in the bulla fluids and there was no detectable mucosal labeling (Figure 1I, 1J).
Fig. 1. The inflamed middle ear of the Jbo/+ and Jf/+ mice is hypoxic. 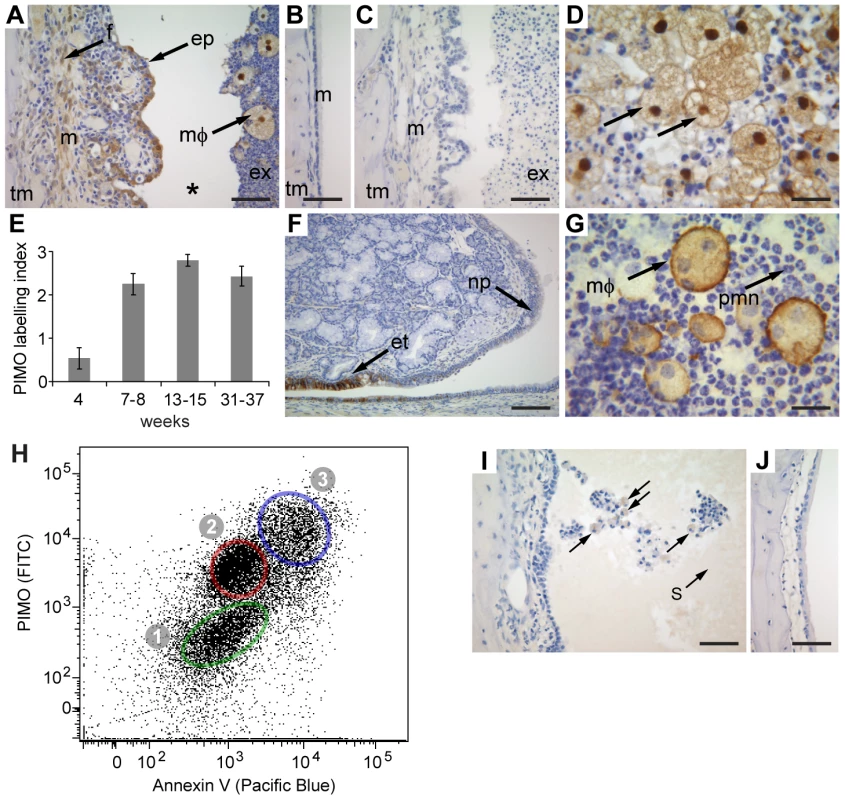
(A) Jbo/+ mouse labeled with pimonidazole (PIMO), arrows indicate hypoxia in [ep] epithelium, [f] connective tissue fibrocyte, [mΦ] foamy macrophage; [tm] temporomandibular bone, [m] thickened inflamed mucosa, [ex] exudate. Note * the cleft is an artifact produced by tissue processing. (B) The normal thin mucosa [m] is not labeled in Junbo wild type (+/+) mice. (C) An unlabeled Jbo/+ mouse is a negative control for anti-PIMO antibody. (D) Hypoxia in foamy mΦ. (E) The middle ear in Jbo/+ mice is chronically hypoxic. The labeling index scores one point each for PIMO-positive staining in inflammatory cells in the bulla; mucosal epithelium; and mucosal connective tissues. Histogram bars are mean ± SEM. 4 wk group size n = 8, 7–8 wk n = 10, 13–15 wk n = 5, 31–37 wk n = 7. (F) The Eustachian tube epithelium [et] is hypoxic in a +/+ mouse but the adjacent nasopharynx epithelium [np] is normoxic. (G) Bulla fluid cytology from a Jbo/+ mouse shows F4/80 foamy mΦ and polymorphonuclear cells (PMN). (H) FACS analysis of PIMO-labeled Jbo/+ bulla fluids stained with Ly6G and Ly6C (PMN marker), for PIMO (hypoxia), and Annexin V (apoptosis marker). The PMN population was gated on the Ly6G and Ly6C signal. Population (1) normoxic viable PMN, (2) hypoxic viable PMN, (3) hypoxic apoptotic PMN. (I) Jf/+ mouse PIMO labeling was restricted to inflammatory cells in the bulla fluids and there was no detectable mucosal labeling, (J) Jeff +/+ mouse does not show PIMO labeling. Scale bars: A,B,C,I,J = 50 µm; D,G = 20 µm; F = 100 µm. Tab. 1. Viable and apoptotic PMN populations in bulla fluids of Jbo/+ and Jf/+ mice are hypoxic. 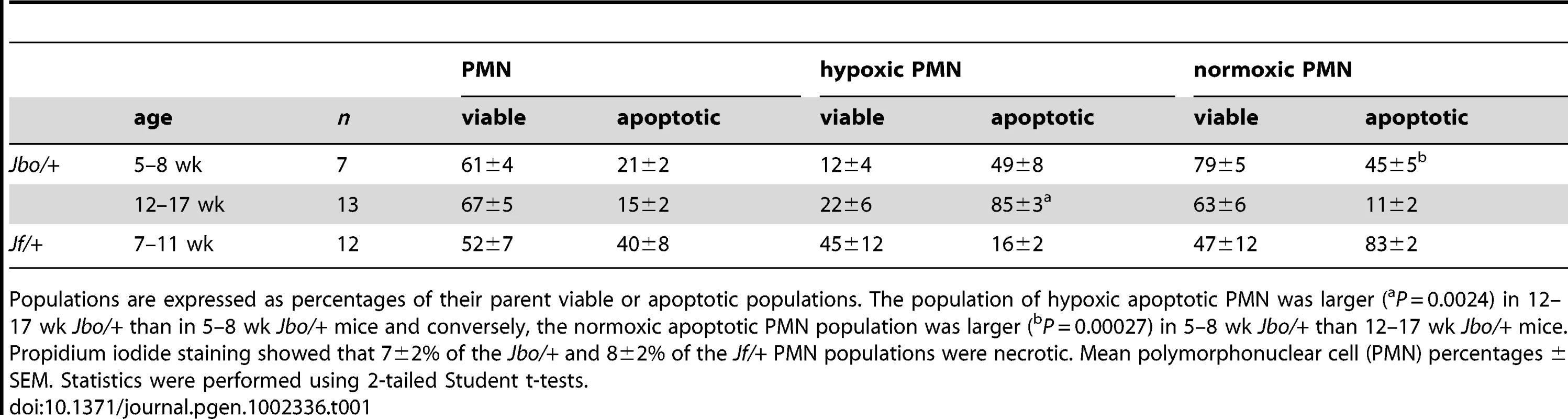
Populations are expressed as percentages of their parent viable or apoptotic populations. The population of hypoxic apoptotic PMN was larger (aP = 0.0024) in 12–17 wk Jbo/+ than in 5–8 wk Jbo/+ mice and conversely, the normoxic apoptotic PMN population was larger (bP = 0.00027) in 5–8 wk Jbo/+ than 12–17 wk Jbo/+ mice. Propidium iodide staining showed that 7±2% of the Jbo/+ and 8±2% of the Jf/+ PMN populations were necrotic. Mean polymorphonuclear cell (PMN) percentages ± SEM. Statistics were performed using 2-tailed Student t-tests. Chronic inflammatory hypoxia and upregulation of HIF and VEGF pathways
Evi1 and Fbxo11 were expressed in the inflammatory cells that accumulate within the bulla fluids of Jbo/+ and Jf/+ mice, but only Evi1 (23–37 fold) was expressed at higher levels relative to a normoxic baseline control of Jbo/+ or Jf/+ venous blood white blood cells (WBC). The Evi1 target genes Jun (28–50 fold) and Fos (5–10 fold) were also elevated in Jbo/+ and Jf/+ bulla fluid inflammatory cells relative to blood WBC (Figure S1).
We found elevated expression of Hif-1α (6–12 fold) and HIF responsive genes Vegfa (41–122 fold) and Slc2a1 (also known as Glut1) (8 fold) in Jbo/+ and Jf/+ bulla fluid WBC relative to blood WBC (Figure S1) and Vegf signaling arrays showed elevated expression in a wide spectrum of Vegf pathway genes (Table S1). In Jbo/+ and Jf/+ mice we obtained data for 84 and 77 genes respectively and there was a strong similarity in pattern of upregulation of genes belonging to functional groups such as Vegf/growth factors and their receptors, Akt and Pi-3-Kinases, phospholipases A2, heat shock proteins, Hif-1α and Arnt (Hif-1β). 44% of the genes were significantly elevated (>2-fold, P<0.05) in both mutants; 18% genes were elevated in both mutants with levels in either Jf/+ or Jbo/+ achieving statistical significance; 4% of genes were elevated in both mutants but P>0.05, and 8% of genes were up-regulated in Jbo/+ mice but beneath detection limits for Jf/+. 11% of genes were unaltered in one or other mutant; 14% unaltered in both mutants and only 1 gene was significantly lower in both mutants (Table S1, Figure S2).
In 8 wk old mice, Vegfa protein was elevated ∼74-fold in Jf/+ bulla fluids compared with Jf/+ sera (median values of 5,793 pg/ml versus 78 pg/ml; P<0.001) and ∼335-fold in Jbo/+ bulla fluids compared with Jbo/+ sera (median values of 28,123 pg/ml versus 84 pg/ml; P<0.001) (Figure 2). The difference between Vegfa titers in Jf/+ and Jbo/+ bulla fluids did not achieve statistical significance, nor did titer differences between Jeff and Junbo mutant and wild type (+/+) sera (Kruskall Wallis ANOVA and Dunn's multiple comparison post hoc tests).
Fig. 2. Vegfa titers are elevated in bulla fluids of 8-week-old Jbo/+ and Jf/+ mice compared to serum. 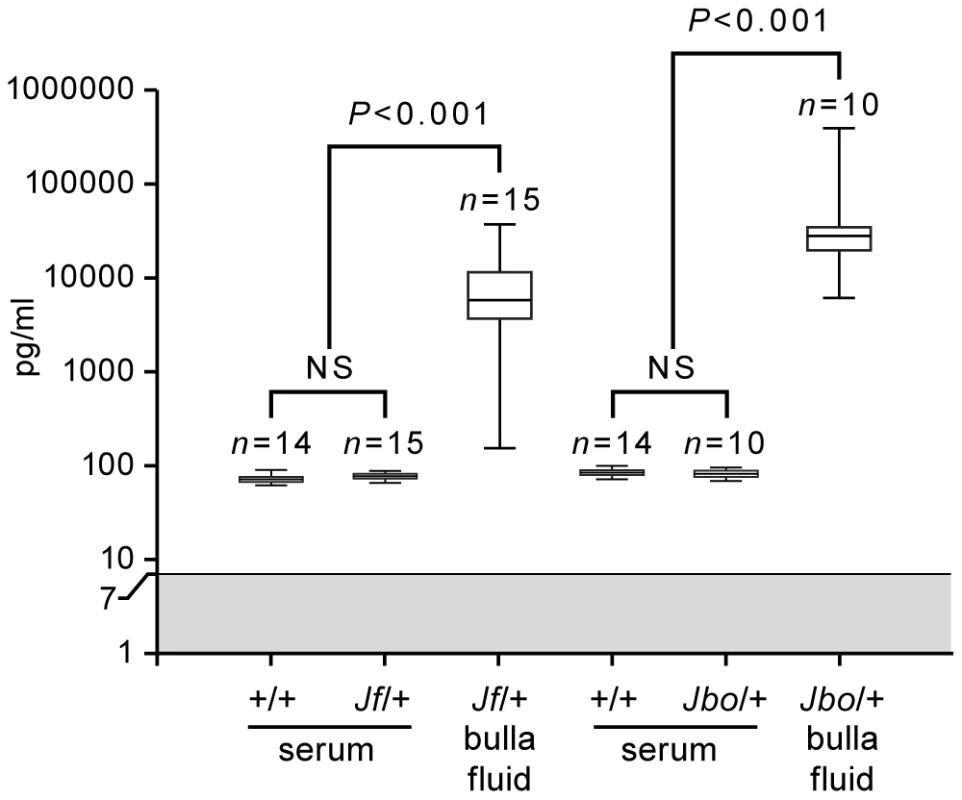
Protein titers of Vegfa in serum and bulla fluids of 8 wk Junbo (+/+ and Jbo/+) and Jeff (+/+ and Jf/+) mice. The gray zone represents the lowest assay standard (7 pg/ml). Each box represents the median with 25 and 75% inter-quartile ranges, with whiskers representing the data range (minimum and maximum). A Kruskall-Wallis test was performed followed by Dunn's multiple comparison tests for post hoc testing. Using inflammation arrays we obtained data for 84 genes in Jbo/+ and 79 genes in Jf/+ mice. Again there was a strong similarity in the pattern of upregulation of gene expression for chemokines, cytokines, their receptors and acute phase response mediators. 35% of genes were significantly elevated (>2-fold, P<0.05) in both mutants; 31% genes were elevated in both mutants with either Jf/+ or Jbo/+ achieving statistical significance; 11% of genes were elevated in both mutants but did not achieve statistical significance (P>0.05); 6% of genes were up-regulated in Jbo/+ mice but beneath detection limits for Jf/+. 10% of genes were unaltered in one or other mutant, 5% unaltered in both and only 2 genes were significantly lower (>2-fold, P<0.05) in one or both mutants (Table S2, Figure S3).
Il-1β and Tnf-α are known modulators of Hif-1α translation and array data indicated that they were significantly elevated (P<0.05) in Jbo/+ (Il-1β 26-fold; Tnf-α 78-fold) but elevations in Jf/+ expression (Il-1β 3-fold; Tnf-α 50-fold) were not statistically significant (Table S2). We therefore went on to determine their protein titers. Il-1β and Tnf-α were elevated in Jbo/+ bulla fluid but not consistently so in Jf/+ mice (Figure 3). Two of 22 Jf/+ mice had Tnf-α bulla fluid titers of 571 and 7,352 pg/ml respectively whereas 20/29 Jbo/+ mice had a median bulla fluid titer of 4,598 pg/ml (range 2,156 to 15,293 pg/ml). The Tnf-α serum titers for mutant and +/+ mice were comparable and ranged from 24 to 107 pg/ml. One of 22 Jf/+ mice had an Il-1β bulla fluid titer of 1920 pg/ml whereas 28/29 Jbo/+ mice had a median bulla fluid titer of 2,862 pg/ml (range 1,319 to 5,819 pg/ml). The Il-1β serum titers for mutant and +/+ mice were comparable and ranged from 15 to 27 pg/ml Figure 3).
Fig. 3. Il-1β and Tnf-α titers in bulla fluids are elevated in Jbo/+ but not Jf/+ mice. 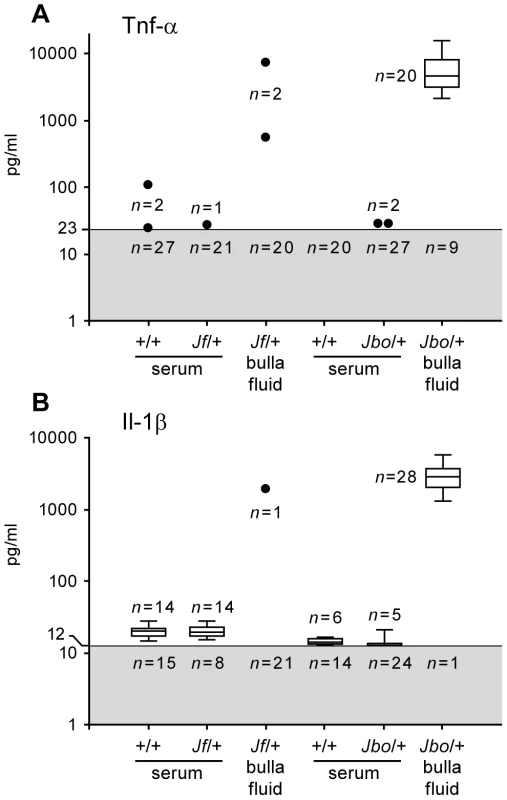
Protein titers of (A) Tnf-α and (B) Il-1β in serum and bulla fluids of 8 wk Junbo (+/+ and Jbo/+) and Jeff (+/+ and Jf/+) mice. Figures in the gray zone represent the numbers of samples with values beneath the lowest assay standard (23 pg/ml for Tnf-α and 12 pg/ml for Il-1β. Each box and whisker symbol represents the minimum, 25% quartile, median, 75% quartile and maximum for reportable measurements while single values are represented by dots. Since the level of Tnf-α and Il-1β in many Jf/+ and Jbo/+ sera and Jf/+ bulla fluid samples was beneath detection limits, a statistical analysis was not performed. Inhibitors of VEGFR signaling and HSP90 moderate hearing loss, angiogenesis, and lymphangiogenesis in Junbo mice
To investigate whether Vegf has a pro-inflammatory role in OM we employed a variety of small-molecule inhibitors of VEGFR and assessed their effects on OM when delivered systemically to the Junbo mouse mutant. The rationale for using the Junbo model and not Jeff was that the OM phenotype was more penetrant. The percentage of Jbo/+ mice with bilateral OM was higher at 78% versus 46% in Jf/+ (Figure S4) making auditory brainstem response (ABR) measurements more robust (see below). Moreover, hearing loss over the standard test period from day 28 to day 56 was greater in Jbo/+ (averaging 7–14 dB in independent experiments) than in Jf/+ (∼4 dB) (Figure 4 and Figure S5). When Jbo/+ mice were treated with VEGFR signaling inhibitors BAY 43-9006 (30 mg/kg), SU-11248 (20 mg/kg) and PTK787/ZK 222584 (50 mg/kg or 75 mg/kg) (hereafter referred to as PTK787) there was a significant moderation of hearing loss (Figure 4). The trial with BAY 43-9006 was terminated after 2 wk when mice suddenly became piloerect. Although BAY 43-9006 was not as well tolerated as PTK787 and SU-11248, the positive therapeutic response to three separate VEGFR signaling inhibitors confirms our data, indicating that HIF mediated VEGF is a critical pathway in OM pathogenesis. We also proceeded to target HIF signaling directly using a HSP90 inhibitor, 17-DMAG. HSP90 is a chaperone of HIF-1α. We found that its use also moderated hearing loss (Figure 4).
Fig. 4. Treatment of Jbo/+ mice with VEGF receptor inhibitors and the HSP90 inhibitor 17-DMAG moderates hearing loss. 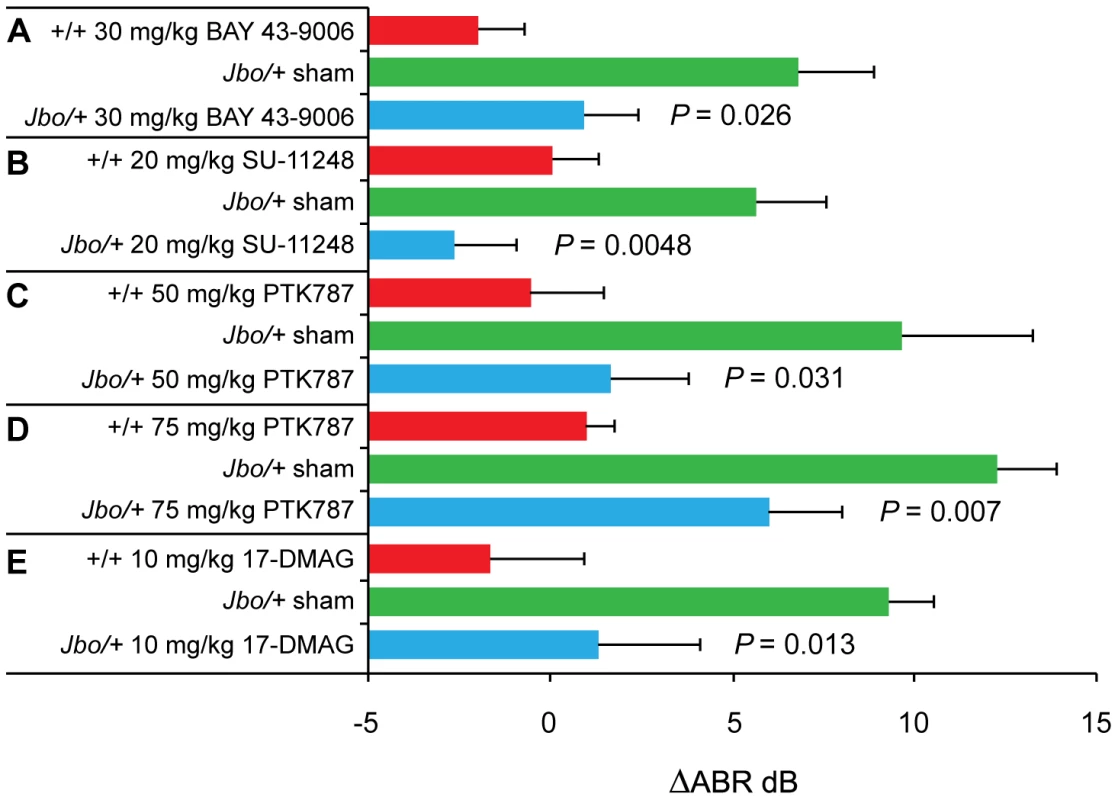
(A) Change in Auditory Brain Stem response (ΔABR) in decibels (dB) in 15 d treatment with BAY 43-9006 (+/+, sham Jbo/+, drug Jbo/+ n = 5, 11, 11 respectively); (B) ΔABR in 28 d treatment with SU-11248 (+/+, sham Jbo/+, drug Jbo/+ n = 10, 15, 15 respectively); (C) ΔABR in 21 d treatment with 50 mg/kg PTK787 (+/+, sham Jbo/+, drug Jbo/+ n = 9, 13, 15 respectively); (D) ΔABR in 28 d treatment with 75 mg/kg PTK787 (+/+, sham Jbo/+, drug Jbo/+ n = 40, 60, 40 respectively); (E) ΔABR in 28 d treatment with 17-DMAG (+/+, sham Jbo/+, drug Jbo/+ n = 9, 15, 15 respectively). In each experiment, the response to drug treatment was compared to the sham control. Histogram bars are mean ± SEM. Statistics were conducted using 1-tailed Mann Whitney U tests. We went on to examine the middle ear mucosal changes in mice treated with VEGFR inhibitors. Morphometric analysis of the mucosal histology was performed on 50 mg/kg and 75 mg/kg PTK787 treatment groups (Figure 5). ANOVA analyses revealed significant reductions in blood vessel number at the higher 75 mg/kg dose; lymphatic vessel number was reduced at both dosages; but neither the mucosal thickness nor lymphatic vessel diameter was reduced by PTK787 treatment (Figure 5). In the BAY 43-9006 trial, treated Jbo/+ mice had reduced lymphatic vessel number (10.8±1.1 n = 11 mice versus 16.4±1.0 n = 11, P = 0.0012) and lymphatic vessel dilation (9.9±1.0 µm n = 11 versus 14.2±0.9 µm n = 11, P = 0.0072) compared with sham treated controls but mucosal thickness and blood vessel number were not altered.
Fig. 5. Treatment of Jbo/+ mice with PTK787 reduces angiogenesis and lymphangiogenesis in the inflamed middle ear mucosa. 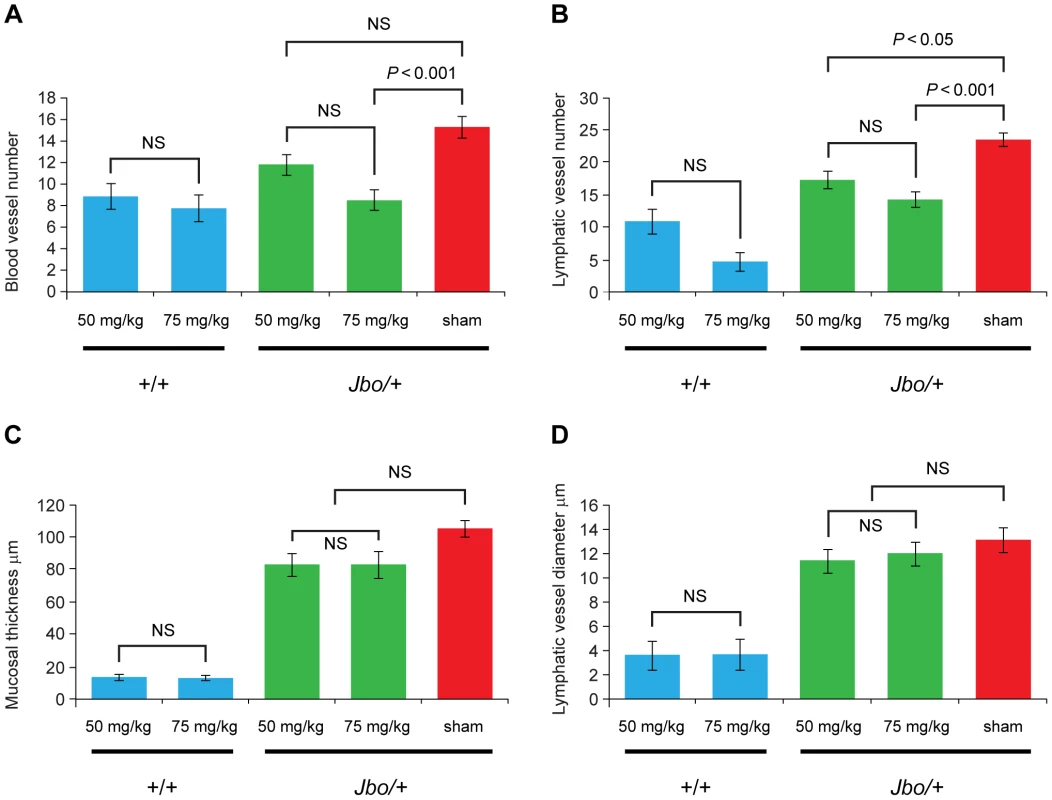
Junbo (+/+ and Jbo/+) mice were treated with either 50 mg/kg or 75 mg/kg of PTK787 for 4 wk, the sham control Jbo/+ groups received vehicle alone. The middle ear mucosa in treated Jbo/+ mice had (A) fewer blood vessels in the 75 mg/kg treatment group and (B) fewer lymphatic vessels in the 50 mg/kg or 75 mg/kg treatment groups. (C) The mucosa thickness and (D) mucosal lymphatic vessel diameter did not differ significantly from sham treated controls. The +/+ group sizes were n = 8; Jbo/+ drug treatment groups n = 15; Jbo/+ sham group n = 28. Histogram bars represent mean ± SEM. Data in panels A, B and C were analyzed by one-way ANOVAs and Bonferroni's multiple comparison tests for post hoc testing. Lymphatic vessel number (panel B) was not normally distributed and a Kruskall-Wallis test was performed followed by Dunn's multiple comparison tests for post hoc testing. To qualitatively assess the effect of drug treatment on bulla fluid accumulation, the middle ears were sampled in the 75 mg/kg PTK787, SU-11248 and 17-DMAG treated and sham treated Jbo/+ mice. In each trial, a significantly lower (P<0.05) proportion of treated Jbo/+ mice yielded bulla fluid samples than sham treated Jbo/+ controls (Figure S6).
Discussion
Single gene mutations in mouse Eya4, Tlr4, p73, MyD88, Fas, E2f4, Plg, Fbxo11 and Evi1 give rise to chronic spontaneous OM phenotypes, in several cases as part of a spectrum of pleiotropic effects, and are candidate susceptibility genes for human OM. In human populations there are significant associations between OM and polymorphisms in FBXO11, TLR4 and PAI1. However, the mechanisms and pathways by which these mutations result in chronic middle ear inflammatory disease are poorly understood. It has been proposed that they may act by a variety of different mechanisms including altered Eustachian tube function and reduced clearance of middle ear pathogens, dysregulation of innate immunity via TLR4/MyD88 pathways and dysregulation of anti-inflammatory mechanisms via TGF-β pathways [27]. We have analyzed the Junbo and Jeff mutants using a number of approaches, including transcriptional profiling and, in Junbo mice, small-molecule inhibitors to dissect the genetic pathways and pathophysiological processes leading to chronic OM.
The characteristic lesion of OM is the accumulation of fluid and inflammatory cells in the bulla and mucosal inflammation. At other sites of inflammation, hypoxia is likely to occur as a result of the uptake of oxygen by inflammatory cells coupled with their physical separation from an underlying vascular bed [30]. Using PIMO labeling we have identified cellular hypoxia in inflammatory cells in the purulent Jbo/+ and serous Jf/+ fluids that accumulate within the 5–6 µl bulla [31]. However mucosal hypoxia was only detectable in Jbo/+ mice. The driver of mucosal hypoxia may be the unmet oxygen demand of inflammatory cells in bulla fluids which in turn is presumably a function of their numbers and viability. The cellularity of Jbo/+ bulla fluids is certainly >100-fold higher than in Jf/+ mice but there are substantial apoptotic PMN cell populations (ranging from 20–40%) and a necrotic cell population (7–8%) which may affect overall oxygen requirements (Table 1). Apoptosis/cell death pathways and oxidative stress pathways would be expected to be upregulated as part of the inflammatory process. Human chronic OME effusions (with or without bacterial infection) range from purulent to serous and mucoid and contain viable and degenerative inflammatory cells [32], [33] and VEGF protein [21] which is a critical downstream mediator of hypoxia signaling. Our results provide direct evidence of cellular hypoxia in bulla fluid inflammatory cells whereas the data for pO2 in human OME bulla fluids is inconsistent [14]–[16]. Mucosal gas exchange is the main method of ventilation of the normal tubotympanum and the resting oxygen tension of the middle ear is comparable to that of venous blood [34]. Surgical ventilation causes relative hyperoxia of the middle ear [35] and a change in oxygen tension might also be an important mechanism in the down-regulation of HIF signaling. One therapeutic benefit may be reduced mucin secretion as conserved promoter regions of respiratory mucin genes expressed in human middle ear bind to HIF-1α [36], [37].
While the influx of inflammatory cells into the bulla lumen may be a key event in the development of hypoxia and activation of HIF signaling via stabilization of HIF-1α protein the activation of inflammatory cells and upregulation of Il-1β, Tnf-α and Nfκb in particular may further modulate HIF signaling [5], [6]. Transcriptional profiling showed upregulation of inflammatory gene networks in the bulla fluids of Jbo/+ and Jf/+ mice relative to blood WBC. Il-1β and Tnf-α serum titers are comparable in mutant and +/+ mice suggesting that OM is not a cause of systemic inflammation, nor is it part of an ongoing systemic inflammatory condition in Junbo and Jeff models. A number of inflammatory genes associated with OM have been published; for a review, see [38] and [39]–[63] and our array data adds another 20 genes to this list (Table S2). However, middle ear inflammation appeared less pronounced in Jf/+ mice. In line with Jf/+ serous bulla fluids containing fewer inflammatory cells, protein titers for the key cytokines Il-1β and Tnf-α were only elevated in a minority of mice. This degree of biological variation between individual Jf/+ mice may explain the variability between pooled samples in which elevated expression levels for genes such as Il-1β and Tnf-α failed to achieve statistical significance. The relative contributions of Il-1β and Tnf-α to hypoxic modulation of Hif-1α and Vegf signaling in the middle ear may be greater in Jbo/+ mice. Nevertheless in both mutants upregulation of HIF signaling was evident from the elevated expression of multiple Vegf signaling pathway genes (Figure S1 and Table S1) including Vegfa and in Jbo/+ its principle receptor Kdr (Vegfr2). Elevated Vegfa gene expression was accompanied by elevated Vegfa protein in Jbo/+ and Jf/+ mice (Figure 2).
VEGF acts to induce angiogenesis, increases vascular permeability and recruitment of neutrophils and macrophages [64], [65] and may therefore contribute to OM by the accumulation of fluid and inflammatory cells within the bulla causing conductive hearing loss and secondary cochlear dysfunction via diffusion of cytokines through the round window [66], [67]. We tested the hypothesis that VEGF signaling contributes to OM pathogenesis by treating Junbo mice, which have highly penetrant OM, with the VEGFR signaling inhibitors PTK787, SU-11248, and BAY 43-9006 and the HSP90 inhibitor 17-DMAG. Their use reduced hearing loss (Figure 4). Histological analysis of the middle ear mucosa in PTK787 treated Jbo/+ mice revealed reduced blood vessel formation (at the higher 75 mg/kg dose) and lymphatic vessel formation (at 50 mg/kg and 75 mg/kg dosages) consistent with the anti-angiogenic effects of VEGFR signaling inhibitors (Figure 5). Only lymphatic vessel number and diameter were significantly moderated by BAY 43-9006 but this may be a reflection of the initial acute inflammatory change taking place in the first 2 wk which was the end point of this trial. SU-11248 treated mice were not examined by histology.
Another effect of treatment with PTK787, SU-11248 and 17-DMAG was to reduce the proportion of Jbo/+ mice that yielded bulla fluid samples (Figure S6). This may reflect moderation of VEGF induced vascular permeability in treated mice. The implication is that bulla fluids recoverable from treated Jbo/+ mice come from those which are less responsive to treatment, and this would confound comparisons of inflammatory cell numbers and gene expression between treated and control mice.
The range of molecular targets for VEGFR and HSP90 inhibitors will require further clarification. VEGF receptors are members of the Receptor Tyrosine Kinase (RTK) superfamily and small-molecule VEGFR inhibitors have multi-kinase inhibitor profiles against different VEGF receptors as well as other RTK families. PTK787 is an inhibitor of VEGFR1, VEGFR2, VEGFR3, PDGFR-β and c-Kit; SU-11248 acts as a VEGFR2, PDGFR-β, FLT3 and c-Kit inhibitor; and BAY 43-9006 acts as a VEGFR2, FLT3, PDGFR-β, c-Kit and Raf1 inhibitor [68]. VEGFR inhibitors therefore have the potential to disrupt additional pathways [69] that might contribute to OM pathogenesis. We therefore also targeted HIF-VEGF signaling pathways using 17-DMAG treatment to inhibit HSP90. HSP90 chaperones a number of proteins involved in HIF-VEGF signaling including HIF-1α itself, the mitogenic signaling protein AKT, and RAF-1 in the RAS/RAF/MEK/ERK MAPK pathway [70]–[72]. In addition, phosphorylation of HSP90 by its client protein VEGFR2 is required for receptor signaling to endothelial NO synthase [73]. However, 17-DMAG can also attenuate inflammatory pathways [74] and may also contribute to the amelioration of OM observed in Junbo mice.
The expression of mutant Evi1 and Fbxo11 proteins in inflammatory cells in bulla fluids has the potential to perturb a variety of signaling pathways that may affect the response to hypoxia and contribute to OM pathogenesis. The Fbxo11 gene is a member of the large F-box family which are specificity factors for the SCF E3 ubiquitin ligase complex, and in homozygote Jeff mutants there are developmental defects in palate, eyelid and lung airway as a result of perturbed Tgf-β signaling [75]. EVI1 is a co-transcriptional repressor of SMAD3 and the mutation in Evi1 in Junbo mice may also exert effects via TGF-β signaling. EVI1 has two zinc-finger domains and a central transcription repression domain. Repressor activities via the proximal N-terminal zinc-finger domain include c-Jun N-terminal kinases (JNK) and TGF-β signaling via direct binding of SMAD3. SMAD3 activity is also reduced by recruitment of the co-repressor CtBP by the central repressor domain [76]. There is considerable cross-talk between TGF-β and HIF-1α pathways. For example, SMAD3 and HIF-1α are co-activators of VEGF expression [77], [78] and mutations affecting TGF-β signaling might be expected to perturb hypoxia responses.
The distal zinc-finger domain of EVI1 has three zinc-finger motifs [79] and the Junbo mutation is a non-conservative Asn763Ile change located within three amino acids of a contact residue in the second zinc-finger motif. Interactions with the distal zinc finger domain raise AP-1 activity by increased expression of Jun and Fos [80]. AP-1 and Jun also interact with HIF pathways [81], [82] and play a role in the pathogenesis of inflammatory bone and skin disease [83]. We found Evi1, and its target genes Jun and Fos were relatively upregulated in the bulla of both Jbo/+ and Jf/+ mice. However we cannot usefully speculate on the possibility of differential expression of Jun and Fos by mutant Evi1Jbo/+ and wild type Evi1+/+ protein. Interpretation is problematic because bulla gene expression levels were normalized to their respective blood baselines, and we have no Evi1 protein data.
Our studies on the mutants Junbo and Jeff, highlights chronic inflammatory hypoxia as a key mechanism of OM pathogenesis and underlines the role of Hif-1α signaling in the underlying genetic and pathophysiological mechanisms that predispose to chronic OM. Jeff has a less pronounced inflammatory OM phenotype, nevertheless the underlying hypoxic signaling mechanism acting via VEGF appears similar to the Junbo model. As a consequence we have identified potential new therapeutic targets for OM. The practical clinical implications for using small-molecule VEGFR signaling inhibitors or other anti-VEGF agents and HSP90 inhibitors are limited in pediatric applications as they are used principally for the treatment of cancer [68], [69], [84]. Ototopical delivery appears to be the most likely way forwards to achieve therapeutic levels of small-molecule inhibitors in the bulla fluids whilst reducing any adverse effects caused by systemic administration. In summary, our findings on the genetic bases for OM in the Junbo and Jeff mutants have underlined the importance of hypoxia mechanisms in the development of chronic OM and as a consequence have revealed potential new therapeutic strategies that merit further exploration.
Materials and Methods
Ethics statement
The humane care and use of mice in this study was under the appropriate UK Home Office license.
Mice
Junbo mice were congenic on a C3H/HeH background [29] and Jeff mice were on a mixed C3H/HeH and C57BL/6J genetic background [28]. The mice were specific pathogen free and had normal commensal nasopharyngeal flora [29].
Blood and bulla fluid collection
Blood was collected from the retro-orbital sinus of mice under terminal anesthesia induced by an i.p. overdose of sodium pentobarbital. After removal of any adherent material on the external surface of the tympanic membrane, a hole in the membrane was made by removing the malleus with a clean pair of forceps and collecting the bulla fluid with a pipette. Bulla fluid volume was measured by collecting 0.5 µl aliquots and the total pooled samples from both ears generally ranged between 0.5–2.0 µl. Bulla fluid was collected into 100 µl aliquots of the appropriate buffer for each analysis (see below) or into 20 µl of RNase free water for RNA isolation. Whole blood for RNA isolation was collected in RNAlater (Qiagen).
Hematology and bulla fluid analysis
Samples of bulla fluids from 8 wk old Jbo/+ and Jf/+ mice were analyzed for total WBC counts on an Advia 120 hematology analyzer (Bayer). Cytology preparations of bulla fluids were made on electrostatically charged slides (Superfrost Plus, Menzel Glaser), methanol fixed then stained with rat anti-mouse F4/80 Mab (MCA497) (AbD Serotech) and counterstained with haematoxylin.
Pimonidazole labeling for hypoxia
Jbo/+, Jf/+ and their respective wild type (+/+) controls were labeled 3 h in vivo by i.p. injection with 60 mg/kg pimonidazole (PIMO) (Hypoxyprobe, HPI Inc) dissolved in 100 µl of sterile PBS. For FACS, bulla fluid samples were collected into 100 µl aliquots of ice cold FACS buffer then stained with anti-PIMO FITC, anti-mouse Ly6G and Ly6C PerCP-Cy5.5 (BD Pharminogen) and anti-Annexin V Biotin (BD Pharminogen)/Streptavidin Pacific Blue (Invitrogen). Propidium iodide (BD Pharminogen) was used to assess necrotic cells. 50 µl EDTA blood samples were diluted in 100 µl FACS buffer then treated with RBC lysis buffer (BD Pharminogen). Unlabeled bulla fluid PMN and non-staining peripheral (normoxic) PMN from PIMO-labeled mice served as negative controls. For histology, the head with the tympanic membranes left intact was fixed for 48 h in 10% neutral buffered formalin then decalcified with Formical (Decal Corp) for 72 h. Wax embedded 3 µm dorsal plane sections of the middle ear were immunostained for PIMO or stained with haematoxylin and eosin.
Real-time quantitative PCR (RT-qPCR) using Applied Biosystems' TaqMan assays
Total RNA from 4 independent pooled samples of Jbo/+ and Jf/+ bulla fluids was isolated using Nucleospin RNA/protein isolation kits (Macherey-Nagel). Individual blood samples from Jbo/+ and Jf/+ mice were extracted using Mouse RiboPure kits (Ambion) then the RNA was made into 3 separate sample pools. Each sample pool comprised 10–15 Jbo/+ mice or 5–9 Jf/+ mice. RNA quantity was measured on a Nanodrop 8000 (Thermo Fisher Scientific) and the integrity assessed by gel electrophoresis. 1 µg of RNA from each pool was used to synthesize double stranded cDNA with a High Capacity cDNA archive kit (AB).
RT-qPCR was performed using TaqMan gene expression assays using Fast Universal PCR Master Mix on a 7500 Fast Real-Time PCR System (AB). Three technical replicates were performed for each TaqMan assay. Data was normalized using Ppia as the endogenous control and fold changes of expression (ddCts) of bulla fluid WBC over blood WBC were calculated using AB 7500 software v2.0.1. This software allowed us to average the technical replicates for each pool and then average the biological replicates for the n = 4 bulla fluid sample pools and n = 3 blood sample pools. The fold change data is shown by mean relative quantification (RQ) ± min/max error bars representing 95% Confidence Limits (CL).
Real-time quantitative PCR (RT-qPCR) using SABiosciences' RT2 Profiler PCR array system
Using the biological replicate pools of bulla fluids and bloods described above, Vegf signaling (PAMM-091c) and Inflammation Response and Autoimmunity (PAMM-077c) arrays (RT2-qPCT™, SA Biosciences) were performed. For each plate, 0.5 µg of RNA was converted to double stranded cDNA using the RT2 first strand synthesis kit. After mixing with the SABiosciences RT2 qPCR mastermix, the cDNA was pipetted into the 96 well profile plate and run on a 7500 Fast Real-Time PCR System (AB). Data was normalized using β-actin as an endogenous control and fold changes of expression of bulla fluid WBC over blood WBC were calculated using SA Biosciences online software (http://pcrdataanalysis.sabiosciences.com/pcr/arrayanalysis.php). The significance of the fold change is shown as a P value based on a Student's t-test of the replicate 2∧(−dCt) values for each gene in the n = 3 control blood and n = 4 bulla fluid sample pools.
Vegfa, Il-1β, and Tnf-α protein assays
Blood was collected into serum-gel clotting activator tubes (Sarstedt). Measured volumes of bulla fluid were added to 100 µl of ice cold PBS, then vortexed and centrifuged at 500×g for 5 min at 4°C. Bulla fluid supernatants and serum samples were stored at −80°C until assay using Quantikine mouse Vegfa, Il-1β and Tnf-α ELISA kits (R&D Systems). Some serum and bulla fluid samples had cytokine titers beneath the lowest assay standard (23 pg/ml for Tnf-α and 12 pg/ml for Il-1β) and according to the manufacturer's instructions these results are not reportable.
Drug treatment and auditory brain-stem response (ABR)
27–29 d old +/+ and Jbo/+ mice were dosed by oral gavage once a day with 30 mg/kg BAY 43-9006, 20 mg/kg SU-11248, 50 or 75 mg/kg PTK787, or 10 mg/kg 17-dimethylaminoethylamino-17-demethoxy-geldanamycin (17-DMAG). +/+ mice were treated with drug as a control for unforeseen ototoxicity. DMSO stock solutions of BAY 43-9006 and SU-11248 (LC Laboratories) or aqueous solutions of PTK787 and 17-DMAG were frozen at −20°C then diluted 10-fold in 2% methyl cellulose for administration. Drug and sham Jbo/+ groups were matched for age, gender and pre-trial ABR threshold (range 30–60 dB) and the sham group received vehicle alone. The anesthetized mouse was placed in right lateral recumbency with the speaker positioned 1.5 cm from the right ear, and a click-evoked ABR performed [85]. ABR measurements were made one day before the first treatment and one day after the last treatment. For ABR with recovery, anesthesia was induced by i.p. injection with a mixture of 10 mg/kg xylazine and 100 mg/kg ketamine and was reversed by 5 mg/kg atipamezole hydrochloride.
To assess whether treatment with SU-11248, 75 mg/kg PTK787, or 17-DMAG treatment altered bulla fluid accumulation a note was made whether fluids were recoverable.
Histology
Middle ear histology was assessed in the BAY 43-9006, and the 50 or 75 mg/kg PTK787 trial mice. Morphometric evaluation was by blinded assessment of a standard 1000 µm length of middle ear mucosa (avoiding the cochlea and the region close to the Eustachian tube), the mucosal thickness was averaged from 5 measurements, and the numbers of capillaries and lymphatic vessels (and their diameter) were recorded.
Statistics
D'Agostino & Pearson omnibus normality tests were performed on PTK787 histology data and Vegfa titer data. Blood vessel number, lymphatic vessel diameter and mucosal thickness were normally distributed and this data was subsequently analyzed using one-way ANOVAs and Bonferroni's multiple comparison tests for post hoc testing. Lymphatic vessel number and Vegfa titers were not normally distributed and a Kruskall-Wallis test was performed followed by Dunn's multiple comparison tests for post hoc testing. Arcsine transformed proportion data from FACS was analyzed using Student t-tests. Chi-squared tests were used to analyze tympanic membrane appearance (cloudy or clear) and the presence or absence of bulla fluids. All other data including ABR measurements (where interval data was in 5 dB increments) was analyzed using Mann Whitney U tests. In the drug trials, 1-tailed tests were used to test positive response to therapy, otherwise 2-tailed tests were used and values P<0.05 were considered significant. Data are presented as mean ± SEM (n) or in the case of Vegfa, Tnf-α and Il-1β protein titers with box and whisker plots.
Supporting Information
Zdroje
1. DavidsonJHydeMLAlbertiPW 1989 Epidemiologic patterns in childhood hearing loss: a review. Int J Ped Otorhinolaryngol 17 239 266
2. KubbaHPearsonJPBirchallJP 2000 The aetiology of otitis media with effusion: a review. Clin Otolaryngol Allied Sci 25 181 194
3. RosenfeldRMCulpepperLDoyleKJGrundfastKMHobermanA 2004 Clinical practice guideline: otitis media with effusion. Otolaryngol Head Neck Surg 130 S95 S118
4. LousJBurtonMJFeldingJUOvesenTRoversMM 2005 Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst Rev CD001801
5. FredeSBerchner-PfannschmidtUFandreyJ 2007 Regulation of hypoxia-inducible factors during inflammation. Meth Enzymol 435 405 419
6. DehneNBrüneB 2009 HIF-1 in the inflammatory microenvironment. Exp Cell Res 315 1791 1797
7. DoedensAJohnsonRS 2007 Transgenic models to understand hypoxia-inducible factor function. Meth Enzymol 435 87 105
8. WalmsleySRPrintCFarahiNPeyssonnauxCJohnsonRS 2005 Hypoxia-induced neutrophil survival is mediated by HIF-1alpha-dependent NF-kappaB activity. J Exp Med 201 105 115
9. RiusJGumaMSchachtrupCAkassoglouKZinkernagelAS 2008 NF-κB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1α. Nature 453 807 811
10. TaylorCT 2008 Interdependent roles for hypoxia inducible factor and nuclear factor-kappaB in hypoxic inflammation. J Physiol 586 4055 4059
11. ZinkernagelAJohnsonRNizetV 2007 Hypoxia inducible factor (HIF) function in innate immunity and infection. J Mol Med 85 1339 1346
12. OliverKTaylorCCumminsE 2009 Hypoxia. Regulation of NFκB signalling during inflammation: the role of hydroxylases. Arthritis Res Ther 11 215
13. GrosiosKWoodJEsserRRaychaudhuriADawsonJ 2004 Angiogenesis inhibition by the novel VEGF receptor tyrosine kinase inhibitor, PTK787/ZK222584, causes significant anti-arthritic effects in models of rheumatoid arthritis. Inflamm Res 53 133 142
14. IngelstedtSJonsonBRundcrantzH 1975 Gas tension and pH in middle ear effusion. Otol Rhinol Laryngol 84 198 202
15. HergilsLMagnusonB 1997 Middle ear gas composition in pathologic conditions: mass spectrometry in otitis media with effusion and atelectasis. Ann Otol Rhinol Laryngol 106 743 745
16. TakahashiMNiwaHYanagitaN 1990 PO2 levels in middle ear effusions and middle ear mucosa. Acta Otolaryngol Suppl 471 39 42
17. KimTHChaeSWKimHJJungHH 2005 Effect of recombinant vascular endothelial growth factor on experimental otitis media with effusion. Acta Otolaryngol 125 256 259
18. JungHHKimMWLeeJHKimYTKimNH 1999 Expression of vascular endothelial growth factor in otitis media. Acta Otolaryngol 119 801 808
19. ChaeSWKimSJKimJLJungHH 2003 Expression of vascular endothelial growth factor receptors in experimental otitis media in the rat. Acta Otolaryngol 123 559 563
20. TruneDRLarrainBEHausmanFAKemptonJBMacArthurCJ 2010 Simultaneous measurement of multiple ear proteins with multiplex ELISA assays. Hear Res 2010 Dec 7 doi:10.1016/j.heares.2010.11.009
21. SekiyamaKOhoriJMatsuneSKuronoY 2011 The role of vascular endothelial growth factor in pediatric otitis media with effusion. Auris Nasus Larynx 3 319 24 Epub 2011 Jan 11
22. CasselbrantMLMandelEMRocketteHEKurs-LaskyMFallPA 2004 The genetic component of middle ear disease in the first 5 years of life. Arch Otolaryngol Head Neck Surg 130 273 278
23. DalyKABrownWMSegadeFBowdenDWKeatsBJ 2004 Chronic and recurrent otitis media: a genome scan for susceptibility loci. Am J Hum Genet 75 988 997
24. SegadeFDalyKAAllredDHicksPJCoxM 2006 Association of the FBXO11 gene with chronic otitis media with effusion and recurrent otitis media: The Minnesota COME/ROM family study. Arch Otolaryngol Head Neck Surg 132 729 733
25. RyeMSWiertsemaSPScamanESHOommenJSunW 2011 FBXO11, a regulator of the TGFβ pathway, is associated with severe otitis media in Western Australian children. Genes Immun 2011 Feb 3. Epub ahead of print doi:10.1038/gene.2011.2
26. DalyKAHoffmanHJKvaernerKJKvestadECasselbrantML 2010 Epidemiology, natural history, and risk factors: panel report from the ninth international research conference on otitis media. Int J Ped Otorhinolaryngol 74 231 240
27. RyeMSBhuttaMFCheesemanMTBurgnerDBlackwellJM 2010 Unraveling the genetics of otitis media - from mouse to human and back again. Mammalian Genome 22 66 82
28. Hardisty-HughesRETateossianHMorseSARomeroMRMiddletonA 2006 A mutation in the F-box gene, Fbxo11, causes otitis media in the Jeff mouse. Hum Mol Genet 15 3273 3279
29. ParkinsonNHardisty-HughesRETateossianHTsaiHTBrookerD 2006 Mutation at the Evi1 Locus in Junbo mice causes susceptibility to otitis media. PLoS Genet 2 e149 doi:10.1371/journal.pgen.0020149
30. WalmsleySRCadwalladerKAChilversER 2005 The role of HIF-1alpha in myeloid cell inflammation. Trends Immunol 26 434 439
31. HuangfuMSaundersJ 1983 Auditory development in the mouse: structural maturation of the middle ear. J Morphol 176 249 259
32. GiebinkGSJuhnSKWeberMLLeCT 1982 The bacteriology and cytology of chronic otitis media with effusion. Ped Infect Dis 1 98 103
33. SipiläPKarmaP 1982 Inflammatory cells in mucoid effusion of secretory otitis media. Acta Otolaryngol 94 467 472
34. SadéJArA 1997 Middle ear and auditory tube: middle ear clearance, gas exchange, and pressure regulation. Otolaryngol Head Neck Surg 116 499 524
35. FeldingJURasmussenJBLildholdtT 1987 Gas composition of the normal and the ventilated middle ear cavity. Scand J Clin Lab Invest Suppl 186 31 41
36. KerschnerJE 2007 Mucin gene expression in human middle ear epithelium. Laryngoscope 117 1666 1676
37. YoungHWWilliamsOWChandraDBellinghausenLKPérezG 2007 Central role of Muc5ac expression in mucous metaplasia and its regulation by conserved 5′ elements. Am J Respir Cell Mol Biol 37 273 290
38. JuhnSKJungMKHoffmanMDDrewBRPreciadoDA 2008 The role of inflammatory mediators in the pathogenesis of otitis media and sequelae. Clin Exp Otorhinolaryngol 1 117 138
39. IinoYKakizakiKKatanoHSaigusaHKanegasakiS 2005 Eosinophil chemoattractants in the middle ear of patients with eosinophilic otitis media. Clin Exp Allergy 35 1370 1376
40. NonakaMOgiharaNFukumotoASakanushiAPawankarR 2009 Poly(I∶C) synergizes with Th2 cytokines to induce TARC/CCL17 in middle ear fibroblasts established from mucosa of otitis media with effusion. Acta Otolaryngol Suppl 562 57 62
41. MoonSKWooJILeeHYParkRShimadaJ 2007 Toll-like receptor 2-dependent NF-kappaB activation is involved in nontypeable Haemophilus influenzae-induced monocyte chemotactic protein 1 up-regulation in the spiral ligament fibrocytes of the inner ear. Infect Immun 75 3361 3372
42. LeichtleAHernandezMEbmeyerJYamasakiKLaiY 2010 CC chemokine ligand 3 overcomes the bacteriocidal and phagocytic defect of macrophages and hastens recovery from experimental otitis media in TNF−/ − mice. J Immunol 184 3087 3097
43. TongHHLongJPShannonPADeMariaTF 2003 Expression of cytokine and chemokine genes by human middle ear epithelial cells induced by influenza A virus and Streptococcus pneumoniae opacity variants. Infect Immun 71 4289 4296
44. KitaHHimiT 1999 Cytokine and chemokine induction using cell wall component and toxin derived from gram-positive bacteria in the rat middle ear. Acta Otolaryngol 119 446 452
45. HarimayaAFujiiNHimiT 2009 Preliminary study of proinflammatory cytokines and chemokines in the middle ear of acute otitis media due to Alloiococcus otitidis. Int J Pediatr Otorhinolaryngol 73 677 680
46. KariyaSOkanoMFukushimaKNomiyaSKataokaY 2008 Expression of inflammatory mediators in the otitis media induced by Helicobacter pylori antigen in mice. Clin Exp Immunol 154 134 140
47. SkovbjergSRoosKNowrouzianFLindhMHolmSE 2010 High cytokine levels in perforated acute otitis media exudates containing live bacteria. Clin Microbiol Infect 16 1382 1388
48. ZhaoSQLiJLiuHZhangQGWangY 2009 Role of interleukin-10 and transforming growth factor beta 1 in otitis media with effusion. Chin Med J (Engl) 122 2149 2154
49. LongJPTongHHShannonPADeMariaTF 2003 Differential expression of cytokine genes and inducible nitric oxide synthase induced by opacity phenotype variants of Streptococcus pneumoniae during acute otitis media in the rat. Infect Immun 71 5531 5540
50. EmontsMVeenhovenRHWiertsemaSPHouwing-DuistermaatJJWalravenV 2007 Genetic polymorphisms in immunoresponse genes TNFA, IL6, IL10, and TLR4 are associated with recurrent acute otitis media. Pediatrics 120 814 823
51. MatkovićSVojvodićDBaljosevicI 2007 Cytokine levels in groups of patients with different duration of chronic secretory otitis. Eur Arch Otorhinolaryngol 264 1283 1287
52. MattilaPSNykänenAElorantaMTarkkanenJ 2002 Adenoids provide a microenvironment for the generation of CD4(+), CD45RO(+), L-selectin(−), CXCR4(+), CCR5(+) T lymphocytes, a lymphocyte phenotype found in the middle ear effusion. Int Immunol 12 1235 1243
53. LeichtleAHernandezMPakKYamasakiKChengCF 2009 TLR4-mediated induction of TLR2 signaling is critical in the pathogenesis and resolution of otitis media. Innate Immun 15 205 215
54. KingPNguiJOppedisanoFRobins-BrowneRHolmesP 2008 Effect of interferon gamma and CD40 ligation on intracellular monocyte survival of nontypeable Haemophilus influenzae. APMIS 116 1043 1049
55. RezesSKésmárkiKSipkaSSziklaiI 2007 Characterization of otitis media with effusion based on the ratio of albumin and immunoglobulin G concentrations in the effusion. Otol Neurotol 28 663 667
56. HongCKParkDCKimSWChaCIChaSH 2008 Effect of paranasal sinusitis on the development of otitis media with effusion: influence of Eustachian tube function and adenoid immunity. Int J Pediatr Otorhinolaryngol 72 1609 1618
57. SabharwalVRamSFigueiraMParkIHPeltonSI 2009 Role of complement in host defense against pneumococcal otitis media. Infect Immun 77 1121 1127
58. JaatinenTRuuskanenOTruedssonLLokkiML 1999 Homozygous deletion of the CYP21A-TNXA-RP2-C4B gene region conferring C4B deficiency associated with recurrent respiratory infections. Hum Immunol 60 707 714
59. ChenALiHSHebdaPAZeeviASwartsJD 2005 Gene expression profiles of early pneumococcal otitis media in the rat. Int J Pediatr Otorhinolaryngol 69 1383 1393
60. HernandezMLeichtleAPakKEbmeyerJEuteneuerS 2008 Myeloid differentiation primary response gene 88 is required for the resolution of otitis media. J Infect Dis 198 1862 1869
61. LiHSDoyleWJSwartsJDLoCYHebdaPA 2003 Mucosal expression of genes encoding possible upstream regulators of Na+ transport during pneumococcal otitis media. Acta Otolaryngol 123 575 582
62. GranathAUddmanRCardellLO 2010 Increased TLR7 expression in the adenoids among children with otitis media with effusion. Acta Otolaryngol 130 57 61
63. KamimuraMHimiTKatauraA 1996 Cell adhesion molecules of experimental otitis media in the rat. Acta Otolaryngol 116 857 862
64. AngeloLSKurzrockR 2007 Vascular endothelial growth factor and its relationship to inflammatory mediators. Clin Cancer Res 13 2825 2830
65. NagyJBenjaminLZengHDvorakADvorakH 2008 Vascular permeability, vascular hyperpermeability and angiogenesis. Angiogenesis 11 109 119
66. PenhaREscadaP 2007 Interrelations between the middle and inner ear in otitis media. Int Tinnitis J 9 87 91
67. JuhnSKHamaguchiYGoycooleaM 2009 Review of round window membrane permeability. Acta Otolaryngol 105 s457 43 48
68. OlssonAKDimbergAKreugerJClaesson-WelshL 2006 VEGF receptor signalling - in control of vascular function. Nat Rev Mol Cell Biol 7 359 371
69. KiselyovABalakinKVTkachenkoSE 2006 VEGF/VEGFR signalling as a target for inhibiting angiogenesis. Expert Opin Investig Drugs 16 83 107
70. van der BiltJDSoetersMEDuyvermanAMNijkampMWWitteveenPO 2007 Perinecrotic hypoxia contributes to ischemia/reperfusion-accelerated outgrowth of colorectal micrometastases. Am J Pathol 170 1379 1388
71. MilkiewiczMDoyleJLFudalewskiTIspanovicEAghasiM 2007 HIF-1α and HIF-2α play a central role in stretch-induced but not shear-stress-induced angiogenesis in rat skeletal muscle. J Physiol 583 753 766
72. FukuyoYHuntCRHorikoshiN 2010 Geldanamycin and its anti-cancer activities. Cancer Lett 290 24 35
73. DuvalMLe BoeufFHuotJGrattonJP 2007 Src-mediated phosphorylation of Hsp90 in response to vascular endothelial growth factor (VEGF) is required for VEGF receptor-2 signaling to endothelial NO synthase. Mol Biol Cell 18 4659 4668
74. Madrigal-MatuteJLópez-FrancoOBlanco-ColioLMMuñoz-GarcíaBRamos-MozoP 2010 Heat shock protein 90 inhibitors attenuate inflammatory responses in atherosclerosis. Cardiovasc Res 86 330 337
75. TateossianHHardisty-HughesREMorseSRomeroMRHiltonH 2009 Regulation of TGF-β signalling by Fbxo11, the gene mutated in the Jeff otitis media mouse mutant. PathoGenet Published online 2009 July 6. doi: 10.1186/1755-8417-2-5
76. GoyamaSKurokawaM 2009 Pathogenetic significance of ecotropic viral integration site-1 in hematological malignancies. Cancer Sci 100 990 995
77. JeonSHChaeBCKimHASeoGYSeoDW 2007 Mechanisms underlying TGF-beta1-induced expression of VEGF and Flk-1 in mouse macrophages and their implications for angiogenesis. J Leukoc Biol 81 557 566
78. Sánchez-ElsnerTBotellaLMVelascoBCorbíAAttisanoL 2001 Synergistic cooperation between hypoxia and transforming growth factor-beta pathways on human vascular endothelial growth factor gene expression. J Biol Chem 276 38527 38535
79. MorishitaKParkerDSMucenskiMLJenkinsNACopelandNG 1988 Retroviral activation of a novel gene encoding a zinc finger protein in IL-3-dependent myeloid leukemia cell lines. Cell 54 831 840
80. TanakaTNishidaJMitaniKOgawaSYazakiY 1994 Evi-1 raises AP-1 activity and stimulates c-fos promoter transactivation with dependence on the second zinc finger domain. J Biol Chem 269 24020 24026
81. LaderouteKR 2005 The interaction between HIF-1 and AP-1 transcription factors in response to low oxygen. Semin Cell Dev Biol 16 502 513
82. YuBMiaoZHJiangYLiMHYangN 2009 c-Jun protects hypoxia-inducible factor-1alpha from degradation via its oxygen-dependent degradation domain in a nontranscriptional manner. Cancer Res 69 7704 7712
83. ZenzREferlRScheineckerCRedlichKSmolenJ 2008 Activator protein 1 (Fos/Jun) functions in inflammatory bone and skin disease. Arthritis Res Ther 2008;10 1 201 Epub 2008 Jan 18
84. TrepelJMollapourMGiacconeGNeckersL 2010 Targeting the dynamic HSP90 complex in cancer. Nat Rev Cancer 10 537 549
85. ZhengQYJohnsonKRErwayLC 1999 Assessment of hearing in 80 inbred strains of mice by ABR threshold analyses. Hearing Res 130 94 107
Štítky
Genetika Reprodukční medicína
Článek Macroautophagy Is Regulated by the UPR–Mediator CHOP and Accentuates the Phenotype of SBMA MiceČlánek Dynamic Replacement of Histone H3 Variants Reprograms Epigenetic Marks in Early Mouse EmbryosČlánek Mutations in a Guanylate Cyclase GCY-35/GCY-36 Modify Bardet-Biedl Syndrome–Associated Phenotypes in
Článek vyšel v časopisePLOS Genetics
Nejčtenější tento týden
2011 Číslo 10- Akutní intermitentní porfyrie
- Farmakogenetické testování pomáhá předcházet nežádoucím efektům léčiv
- Růst a vývoj dětí narozených pomocí IVF
- Pilotní studie: stres a úzkost v průběhu IVF cyklu
- Vliv melatoninu a cirkadiálního rytmu na ženskou reprodukci
-
Všechny články tohoto čísla
- Transcriptional Robustness Complements Nonsense-Mediated Decay in Humans
- Identification, Replication, and Fine-Mapping of Loci Associated with Adult Height in Individuals of African Ancestry
- Genetic Determinants of Serum Testosterone Concentrations in Men
- A One Base Pair Deletion in the Canine Gene Causes Exon Skipping and Late-Onset Neuronal Ceroid Lipofuscinosis in the Tibetan Terrier
- Three Structure-Selective Endonucleases Are Essential in the Absence of BLM Helicase in
- Identification of Widespread Ultra-Edited Human RNAs
- Multiple Wnts Redundantly Control Polarity Orientation in Epithelial Stem Cells
- The Bicoid Stability Factor Controls Polyadenylation and Expression of Specific Mitochondrial mRNAs in
- Transcriptome-Wide Binding Sites for Components of the Non-Poly(A) Termination Pathway: Nrd1, Nab3, and Sen1
- Macroautophagy Is Regulated by the UPR–Mediator CHOP and Accentuates the Phenotype of SBMA Mice
- Genetic Rearrangements Can Modify Chromatin Features at Epialleles
- Novel Function of as a Gap Gene during Spider Segmentation
- A Genome-Wide Screen for Interactions Reveals a New Locus on 4p15 Modifying the Effect of Waist-to-Hip Ratio on Total Cholesterol
- Comparative Genomic Analysis of Human Fungal Pathogens Causing Paracoccidioidomycosis
- Genetic Diversity in Cytokines Associated with Immune Variation and Resistance to Multiple Pathogens in a Natural Rodent Population
- Mutator Suppression and Escape from Replication Error–Induced Extinction in Yeast
- Dynamic Replacement of Histone H3 Variants Reprograms Epigenetic Marks in Early Mouse Embryos
- A Barcode Screen for Epigenetic Regulators Reveals a Role for the NuB4/HAT-B Histone Acetyltransferase Complex in Histone Turnover
- HIF–VEGF Pathways Are Critical for Chronic Otitis Media in and Mouse Mutants
- A Conserved Developmental Patterning Network Produces Quantitatively Different Output in Multiple Species of Drosophila
- Role of Exonic Variation in Chemokine Receptor Genes on AIDS: Association with Pneumocystis Pneumonia
- Whole-Exome Sequencing Identifies Homozygous Mutations in a Spastic Ataxia-Neuropathy Syndrome Linked to Mitochondrial -AAA Proteases
- Von Hippel-Lindau () Inactivation in Sporadic Clear Cell Renal Cancer: Associations with Germline Polymorphisms and Etiologic Risk Factors
- A Systems Biology Approach Reveals the Role of a Novel Methyltransferase in Response to Chemical Stress and Lipid Homeostasis
- Identification of Genomic Regions Associated with Phenotypic Variation between Dog Breeds using Selection Mapping
- Global Mapping of Cell Type–Specific Open Chromatin by FAIRE-seq Reveals the Regulatory Role of the NFI Family in Adipocyte Differentiation
- Natural Selection Affects Multiple Aspects of Genetic Variation at Putatively Neutral Sites across the Human Genome
- MicroRNA Expression and Regulation in Human, Chimpanzee, and Macaque Brains
- An Adaptive Allelic Series Featuring Complex Gene Rearrangements
- Feed-Forward Microprocessing and Splicing Activities at a MicroRNA–Containing Intron
- Developmental Stability: A Major Role for in
- A Phenomics-Based Strategy Identifies Loci on , , and Associated with Metabolic Syndrome Phenotype Domains
- Association of , , , , and with Systemic Lupus Erythematosus
- Small RNAs Prevent Transcription-Coupled Loss of Histone H3 Lysine 9 Methylation in
- Successive Increases in the Resistance of to Viral Infection through a Transposon Insertion Followed by a Duplication
- Mutations in a Guanylate Cyclase GCY-35/GCY-36 Modify Bardet-Biedl Syndrome–Associated Phenotypes in
- The Glycobiome Reveals Mechanisms of Pentose and Hexose Co-Utilization in Bacteria
- Insights into Hox Protein Function from a Large Scale Combinatorial Analysis of Protein Domains
- Mutations Cause Seckel and Jawad Syndromes
- Zelda Binding in the Early Embryo Marks Regions Subsequently Activated at the Maternal-to-Zygotic Transition
- Temporal Coordination of Gene Networks by Zelda in the Early Embryo
- Genetic Interaction between MTMR2 and FIG4 Phospholipid Phosphatases Involved in Charcot-Marie-Tooth Neuropathies
- Oxr1 Is Essential for Protection against Oxidative Stress-Induced Neurodegeneration
- Transforming Growth Factor β Receptor Type 1 Is Essential for Female Reproductive Tract Integrity and Function
- Positional Cloning of a Type 2 Diabetes Quantitative Trait Locus; , a Negative Regulator of Insulin Secretion
- PLOS Genetics
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- The Glycobiome Reveals Mechanisms of Pentose and Hexose Co-Utilization in Bacteria
- Global Mapping of Cell Type–Specific Open Chromatin by FAIRE-seq Reveals the Regulatory Role of the NFI Family in Adipocyte Differentiation
- Genetic Determinants of Serum Testosterone Concentrations in Men
- MicroRNA Expression and Regulation in Human, Chimpanzee, and Macaque Brains
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



