-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Rare Case of Pathological Biomineralization of Eye Tissue
Vzácný případ patologické mineralizace oční tkáně
Autor popisuje případ patologické mineralizace zadní komory oka. Histologické vyšetření obalů postiženého oka odhalilo zánět, otok, poruchy cirkulace a známky dystrofické kalcifikace. Strukturálně fázové vyšetření a chemická analýza kalcifikace stanovily, že biominerál je tvořen hydroxyapatitem z relativně malých krystalů s poruchou krystalické mřížky.
V popisovaném případě byla tvorba patologického biominerálu ve zrakovém orgánu vyvolána penetrujícím poraněním. Oční úraz mohl způsobit hemoftalmus a chronickou zánětlivou reakci v obalech oka. Tyto procesy mohly způsobit částečnou atrofii oka a vývoj dystrofických a nekrobiotických změn v tkáních. Patologická biomineralizace v postiženém oku se vznikla jako druh dystrofické kalcifikace.
Klíčová slova:
oko, patologická biomineralizace, hydroxyapatit
Do redakce doručeno dne 23. 4. 2014
Do tisku přijato dne 18. 7. 2014
Authors: R. A. Moskalenko 1; A. N. Romanyuk 1; S. N. Danilchenko 2; N. I. Kozinets 3; E. V. Smeyanov 1; T. G. Kalinichenko 2; V. N. Kuznetsov 2
Authors place of work: Sumy State University, Medical institute, Department of Pathological Anatomy, Rimsky-Korsakov st. , 40007, Sumy, Ukraine 1; IAP NASU, Institute for Applied Physics, National Academy of Sciences of Ukraine, Petropavlovskaya st. 58, 40000, Sumy, Ukraine. 2; PI “SCCH number 5”, Public Institution “Sumy City Clinical Hospital № 5”, branch of Eye Microsurgery, Marco Vovchok st., 2, 40007 Sumy, Ukraine. 3
Published in the journal: Čes. a slov. Oftal., 70, 2014, No. 4, p. 160-163
Category: Kazuistika
Summary
The authors have described the case of pathological biomineralization of ocular posterior chamber. Histological examination of affected eye shells revealed inflammation, oedema, dyscirculatory violations, and signs of dystrophic calcification. Structural-phase and chemical analyses of calcification have revealed that the biomineral consists of hydroxyapatite with relatively small crystallite size and defective crystal lattice.
In the described case the formation of pathological biomineral in the vision organ was initiated by penetrating wound. Eye injury might have caused a hemophthalmus and chronic inflammatory reaction in the shells, these processes eventually led to the organ subatrophy and to the development of dystrophic and necrobiotic changes in the tissues. Pathological biomineralization in the affected organ developed as a type of dystrophic calcification.
Key words:
eye, pathological biomineralization, hydroxyapatite
Biominerals formation in the vision organ is a fairly rare pathology. The literature in connection with the processes of biomineralization and calcification described choroidal osteoma, idiopathic choroidal sclerosis, focal tofus-like calcification of the sclera and intraocular osseous metaplasia [1, 2, 3, 4, 5]. Choroidal osteoma is a benign tumor that replaces a choroidal shell by a mature bone. This tumor was first described in 1975. It is more often one-sided, but sometimes there is a later affection of the second eye (20%). Etiology of choroidal osteoma is unknown; it is believed that this pathology relates to choristoma [3]. Intraocular osseous metaplasia, according to Vemuganti GK et al (2002), is found in 5.2% of patients who were performed ocular enucleation owing to tuberculosis of eyeball, staphyloma, absolute glaucoma or microphthalmos [5]. The processes of dakrioliths formation in the lacrimal sac were also studied [6].
The reason of the development of pathological mineral formation processes in the vision organ and in the accessory glands has not been determined [1, 2, 6].
The aim of this work is to study the pathological processes of biomineralization in the eye tissues, using pathomorphological methods and applied materials science.
Materials and Methods
Surgical material was fixed in 10% neutral formalin for further fixation in alcohols at carousel device AT-4M and filling in paraffin blocks, from which 4-6 microns thick sections were manufactured by a rotary microtome “Shandon Finesse 325”. Histological sections were stained with hematoxylin-eosin and examined with the use of a light microscope of the company “Carl Zeiss Primo Star”. Micrographs were obtained with the help of a digital image output system “SEO Scan ICX 285 AK-F IEE-1394”.
Mineral component was isolated by heat treatment at 200 ° C for 1 hour. X-ray diffraction investigations were performed on a diffractometer DRON4 -07 (“Petrel”). Radiation CuK (wavelength 0,154 nm) was used under conditions of Bragg-Brentano focusing (J-2J) (2J – Bragg angle) [7]. The current and the voltage at the X-ray tube were 20 mA and 30 kV, respectively. Samples were shot with the continuous registration (speed 2 °/ min) in the angular range 2J from 10 to 60°. All procedures of the experimental data processing were performed by licensed software support package and processing of the results (DIFWIN-1, TOO “Etalon PTC”). Identification of the crystalline phases was carried out by automatic comparison of the obtained results with the database cards Powder Diffraction File 2 without imposing restrictions on the elemental composition of samples; the software package Crystallographica Search-Match (Oxford Cryosystems) was used in this work.
Scanning electron microscopy with X-ray microanalysis was performed by the instrument REMMA102 (SELMI). In the energy-dispersive microanalysis (EDX) conditions analytical signal accumulated from three fragments of calcifications for 200 seconds at an accelerating voltage of 20 keV and a current probe 3 nA. The sample particles, deposited on a special conductive carbon tape, were coated with a thin conductive film of gold in a vacuum system VUP -5M (SELMI) to prevent the accumulation of electrostatic charge during the investigation of the elemental composition.
Clinical case
A 61-year-old man was taken to the ophthalmology department of Sumy Regional Hospital in November 2011. The patient complained of cramps, redness, and blindness of the right eye. The pain was observed for 10 days, but he didn’t apply for medical aid. The history tells about a penetrating wound of the right eye in 1965. An ophthalmic status of the right eye: the right eyeball reduced in size, mobility is not limited, visual acuity of 0 (zero), blepharospasmus, lacrimal path is passable. Conjunctiva is hyperemic, there is a mixed injection of the eyeball, and the cornea is edematous and lumpy. The anterior chamber is filled with pus, deeply lying structures aren’t visualized. The left eye examination revealed: visual acuity is 0.9, the intraocular pressure is 20 mm, the eyelids are not changed, the lacrimal path is passable, the conjunctiva is pale pink, the cornea is clear, the anterior chamber is depth average, the iris pattern is not changed, the lens has starting opacities in the cortical layers, the vitreous and optic disc are unremarkable. After examination the diagnosis was determined as a penetrating wound exodus (1965), subatrophy, and endophthalmitis of the right eye. The patient had incipient senile cataract of the left eye. Enucleation of the right eye with the formation of the stump was performed.
Pathologic study of surgical material revealed that the eyeball reduced in size to 1,3x0,9 cm, the tone also dramatically reduced. Dirty yellowish color clots were revealed in the anterior chamber. Hardening of the inner lining of the eye, which was almost total, was detected in the posterior chamber. The formation was of a gray-brown color, the size was 1,2 x0, 7 cm, had the form of a funnel with a hole of 0.2-0.3 cm diameter at the tapered end, weighing 0,815 g (Fig. 1A). After scorching in a muffle furnace at 200°C for 60 minutes, the formation retained the structure of a funnel and acquired gray-whitish color, the weight was 0.17 g (Fig. 1B).
Fig. 1. Eye macropreparations after fixation in formalin (Fig. 1A). Biomineral component after heat treatment of the material (Fig. 1B). 
Histological examination of the sclera revealed the signs of swelling (Fig. 2A), there were signs of intense inflammatory infiltration, congestion of vessels, foci of hemorrhage in choroid (Fig. 2B). Deposits of calcifications, most likely of degenerative genesis, were revealed in the tissue of posterior chamber membranes.
Fig. 2. Histological examination of the affected eye. A – the sclera with symptoms of oedema. B – inflammatory infiltration (1), hemorrhage (2) in the choroid . C – calcification in the shells of eye posterior chamber (1). Hematoxylin-eosin. Increase is shown in the lower left corner of each image. Asterisk* points artifact crack, which was formed in the manufacture of sections of mineralized tissue. 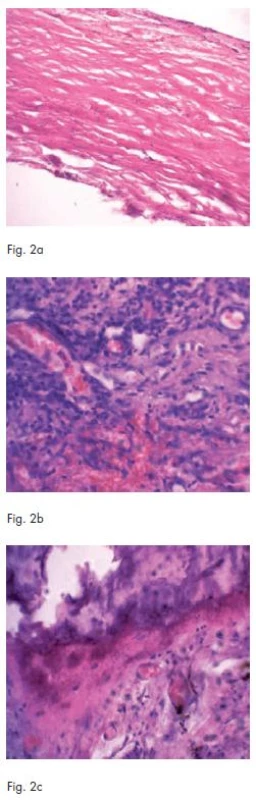
Research of biomineralith using the methods of applied materials science
The decoding of a ray diffraction pattern of the sample of pathological mineral formation of the eye showed a good accordance to the structural data of hydroxyapatite (Ca10(PO4)6(OH)2, JCPDS 9-0432).
Considerable broadening and overlap of the diffraction peaks shows a low degree of crystallinity of the investigated material, namely the small size of the areas with a regular periodic structure (crystallites or mosaic blocks) and a large proportion of defects, which lead to lattice microstrain. Scherrer’s [3] estimating of the crystallites size in the perpendicular direction to the crystallographic plane (002) gave meanings very close to the typical size of bone tissue crystallites (L002=18,2 nm). It should be noted that the line of the longitudinal size of apatite crystals (e.g., 002) are broadened much less than the lines of the transverse size (e.g., 310). It means that the crystals along the hexagonal axis are elongated and have small sizes in their transverse direction. This morphology of biological apatite crystals (like a plate, needle or bar) is typical for bone tissue and similar synthetic biomaterials.
Data of EDX microanalysis showed that the main elements of deposit were calcium and phosphorus in the typical ratio of apatite (Fig. 4, Table 1). Some excess of Ca in the stoichiometric apatite indicates the presence of calcium-fortified non-apatite mineral constituents, which are the source of biocrystal growth, and it is typical for many cases of investigated pathological deposits [8, 9].
Fig. 3. Original diffraction of mineral material of pathological eye formation, vertical lines indicate the position and intensity of the peaks of hydroxyapatite Ca<sub>10</sub>(PO<sub>4</sub>)<sub>6</sub>(OH)<sub>2</sub> according to the reference data JCPDS 9-0432. 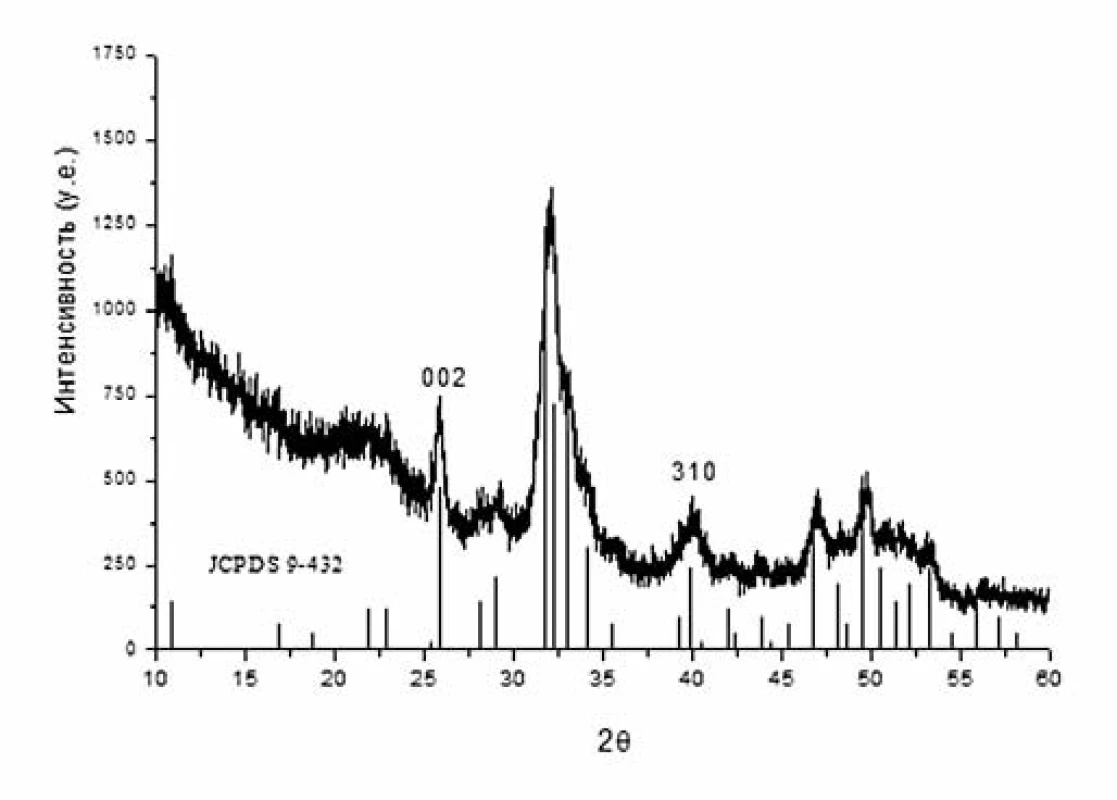
Fig. 4. EDX spectrum of pathological mineral eye formation. 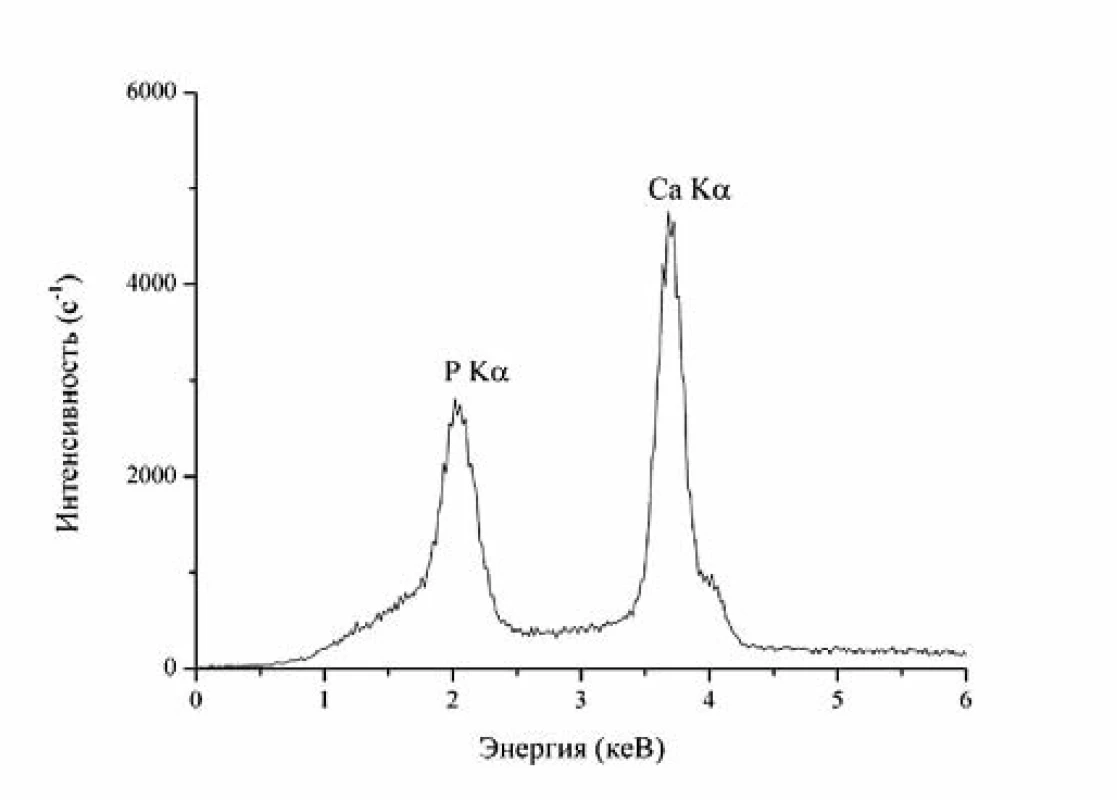
Tab. 1. The concentrations of Ca and P in three areas of the investigated calcifications according to EDX analysis (wt.%). 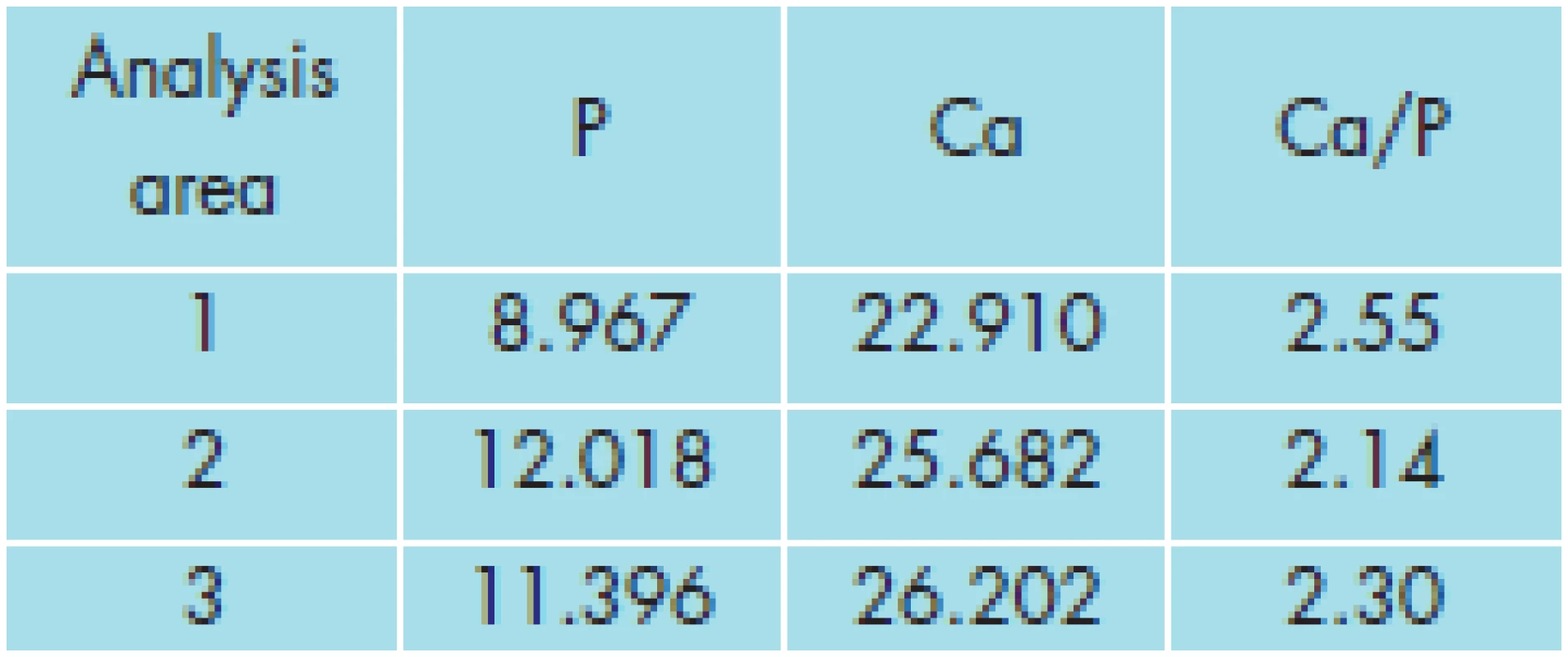
Disscusion
Chronic inflammation cells, bone morphogenetic proteins, growth factors and stem mesenchymal cells play possible role in the pathogenesis of intraocular biomineralization. Under the influence of bone morphogenetic proteins and growth factors mesenchymal stem cells differentiate into osteoblasts. They secrete bone matrix (osteoid), whose regeneration and remodeling lead to the formation of bone-like tissue [10]. In the paper of Rohrbach J. M. et al (1990) it is indicated that intraocular osseous metaplasia is triggered by chronic changes of the Retinal Pigment Epithelium (RPE). The primary lesion (e.g. trauma, inflammation or tumor) plays a minor or no role [11].
The peculiarity of the investigated case is a significant size of ocular lesion and a long period of the process development (46 years). Of course, the process of biomineralization in the tissues grows slowly, but this long period of development inclines us to believe that a key element in the development of ocular calcification is the Retinal Pigment Epithelium (RPE). We believe that the biomineralization processes in the investigated case should not be called intraocular ossification or bone formation, but dystrophic calcification. Firstly, structures characteristic of bone (formation of bone marrow, Havers tubules) have not been observed in the ocular tissues. Secondly, the data about a small size of the crystals of hydroxyapatite and defective crystal lattice, which were received using the methods of applied material science, indicate the development of dystrophic biomineralization, but not bone tissue, in the ocular tissues.
Conclusion
Detection of pathological biomineralization in the vision organs of patients is a rare event, thus being of great interest. In this case the treatment of the patient in a conservative manner was futile and posed a threat to the healthy eye. Histological examination of the affected eye shells revealed inflammation, oedema, dyscirculatory violations, and signs of dystrophic calcification.
Structure-phase and chemical compositions of biomineral were established using the methods of applied materials science. Presence of apatite crystal phase with relatively small crystallite size and defective lattice in pathological formation is quite typical for many cases of ectopic biomineralization, but in our opinion, for the first time it was described for ocular calcifications and using the methods of applied materials science.
In the described case the pathological biomineral formation in the vision organ was initiated by penetrating wound. Eye injury probably led to hemophthalmus and chronic inflammatory reaction in the shells, these processes eventually led to organ subatrophy, development of dystrophic and necrobiotic changes in the tissues. Pathological biomineralization in the affected vision organ developed as a type of dystrophic calcification.
The value of presented work is not only a rare case, but also the opportunity to raise the ophthalmologists’ knowledge of morphogenesis of pathological biomineralization in the diseases of vision organ.
R. A. Moskalenko
Sumy State University,
Medical institute, Department of Pathological Anatomy,
Rimsky-Korsakov st. 2,
40007, Sumy,
Ukraine
eriugen@ukr.net
Zdroje
1. Daicker B.: Tophus-like, conglomerated, crystalline calcification of the sclera. Ophthalmologica, 1996; 210(4): 223–8.
2. Chen KH, Li MJ, Cheng WT. et al.: Identification of monoclinic calcium pyrophosphate dihydrate and hydroxyapatite in human sclera using Raman microspectroscopy. Int J Exp Pathol, 2009; Feb;90(1):74–8.
3. Pandey N., Guruprasad A. Choroidal osteoma with choroidal neovascular membrane successful treatment with intravitreal bevacizumab. Clinical Ophtalmology, 2010; 4, :1081–84.
4. Bourcier T, Blain P, Massin P. et al.: Sclerochoroidal calcification associated with Gitelman syndrome. Am J Ophthalmol, 1999; Dec;128(6): 767–8.
5. Vemuganti G.K, Honavar S.G, Jalali S.: Intraocular osseous metaplasia. A clinico-pathological study. Indian J Ophthalmol, 2002 Sep; 50(3): 183–8.
6. Karakeshinian . [Dacrolithiasis]. Noviy armianskiy meditsinskiy jurnal [New Armenian Medical Journal]. 2011; 5 (3):71–72. (In Russ).
7. Klug H.P., Alexander L.E. X-Ray diffraction procedures for polycrystallite and amorphous materials.-New York: JohnWiley and Sons, 1974.-965p.
8. Moskalenko R., Romanyuk A., Danilchenko S. et al.: Morphogenetic aspects of biomineralization on the background of benign prostatic hyperplasia. Georgian medical news, 2013; 214 (1): 54–61.
9. Danilchenko S.N., Kuznetsov V.N., Stanislavov A.S. et al.: The mineral component of human cardiovascular deposits: morphological, structural and crystal-chemical characterization. Crystal research and technology, 2013, 48 (3): 153–62.
10. Munteanu M, Munteanu G, Giuri S, Zolog I, Motoc A.G.: Ossification of the choroid: three clinical cases and literature review of the pathogenesis of intraocular ossification. Rom J Morphol Embryol, 2013;54(3 Suppl): 871–7.
11. Rohrbach J.M, Liesenhoff E, Steuhl K.P.: [Principles of intraocular ossification exemplified by secondary choroid ossification]. Klin Monbl Augenheilkd, 1990 Nov;197(5): 397–403.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2014 Číslo 4- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Léčba chronické blefaritidy vyžaduje dlouhodobou péči
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Selektivní laserová trabekuloplastika nesnižuje nitroční tlak více než argonová laserová trabekuloplastika
-
Všechny články tohoto čísla
- Contrast Sensitivity and Optic Coherence Tomography Examinations in Adolescent Patients with Diabetes Type I Preretinopathy (A Pilot Study)
- Cytomegalovirus Infection (CMV) in Patients with Acquired Immunodeficiency Syndrome
- Clinical Findings in Family with Aniridia due the PAX6 Mutation
- Supracor, Laser Correction of Presbyopia: One-year Follow-up Outcomes
- Lymphangioma of the Orbitopalpebral Area
- Rare Case of Pathological Biomineralization of Eye Tissue
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Lymphangioma of the Orbitopalpebral Area
- Cytomegalovirus Infection (CMV) in Patients with Acquired Immunodeficiency Syndrome
- Supracor, Laser Correction of Presbyopia: One-year Follow-up Outcomes
- Clinical Findings in Family with Aniridia due the PAX6 Mutation
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



