-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Respiratory problems in full term newborns, which parameters are related to the length of in-patient stay?
Respirační potíže u donošených novorozenců, které parametry souvisí s délkou hospitalizace?
Cíl: Analyzovat respirační problémy donošených novorozenců během prvních hodin jejich života, porovnat parametry související s délkou pobytu na novorozenecké jednotce intenzivní péče (JIP) a prodiskutovat postupy perinatální péče, které by mohly zabránit následkům a/nebo snížit související náklady hospitalizace na JIP. Materiál a metody: Retrospektivní revize grafu mezi 31. červencem 2017 a 2. březnem 2018 v terciární porodnici. Chí-kvadrátové testování analyzovalo kvalitativní data. Pro kvantitativní proměnné byl použit Mann-Whitney test. Vícenásobné lineární regresní modely určovaly poměry šancí pro asociace, které byly v jednorozměrných analýzách významné. Výsledky: Bylo studováno 86 dětí s dýchacími problémy. Způsob porodu byl vaginální u 11,6 % a císařský řez u 88,4 % novorozenců. 52,3 % přijatých novorozenců mělo přechodnou tachypnoii a relativně rychle se zlepšila. Novorozenci resuscitovaní (p = 0,004) nebo přijatí na JIP z porodního sálu (p = 0,000) vykazovali větší potřebu podávání O2. Dvacet novorozenců bylo intubováno, 16 z nich byl podán surfaktant. Infekce (p < 0,05), abnormální rentgenové vyšetření hrudníku (p = 0,022) a závažnost nemocnosti dýchacího systému (p < 0,05) prodloužily neonatální hospitalizaci. Respirační problémy (p = 0,003) a intubace (p = 0,032) přinesly vyšší náklady na hospitalizaci. Zahájení kojení před 3. dnem života (p = 0,031) a podávání O2 déle než 72 hod (p = 0,036) byly v multivariační regresní analýze významně spojeny s délkou hospitalizace. Závěr: Povinná přítomnost dětského lékaře na porodním sále by optimalizovala oprávněné přímé přijetí na JIP a snížila možnost opožděné diagnózy dechové tísně během rooming-in. Pobyt na jednotce intenzivní péče u novorozenců v termínu by měl být založen na kombinaci diagnostických markerů sepse, jako je prokalcitonin nebo interleukin-6. Je také nutný specifický protokol týkající se podávání surfaktantu u intubovaných donošených dětí. Závažnost nemocnosti dýchacího systému není klíčovým určujícím faktorem výživy kojenců. Informace matek týkající se zdraví kojence a schopností kojení mohou zvýšit míru kojení.
Klíčová slova:
novorozenec – dýchání – tíseň – tachypnoe – JIP
Authors: A. Fotiou 1
; P. V. Vlastarakos 2
; A. E. Sfetsiori 3; E. F. Tavoulari 4
; M. Liaska 3; I. Salvanos 1
Authors place of work: Department of Neonatology, Helena Venizelou General & Maternity Hospital, Athens, Greece 1; 2nd ENT Department, University of Athens, ATTIKON University Hospital, Athens, Greece 2; 2nd Department of Pediatrics University of Athens, P. & A. Kyriakou Children's Hospital, Athens, Greece 3; Department of Neonatology, Agios Panteleimon General Hospital, Nikaia, Greece 4
Published in the journal: Ceska Gynekol 2023; 88(4): 264-272
Category: Původní práce
doi: https://doi.org/10.48095/cccg2023264Summary
Objective: To analyze respiratory problems of full term newborn babies during their first hours of life, compare parameters related to the length of neonatal intensive care unit (NICU) in-patient stay, and discuss perinatal care practices, which could prevent consequences, and/or reduce associated costs of NICU hospitalization. Material and methods: Retrospective chart review between July 31st 2017 and March 2nd 2018 in a tertiary maternity hospital. Chi-square testing analyzed qualitative data. Mann-Whitney test was used for quantitative variables. Multiple linear regression models determined odds ratios for associations were found to be significant in univariate analyses. Results: 86 babies with respiratory problems were studied. Delivery mode was vaginal in 11.6% and caesarean section in 88.4% of newborns. About 52.3% of admitted newborns had transient tachypnea and improved relatively quickly. Newborns resuscitated in (P = 0.004) or admitted to the NICU from the delivery room (P = 0.000) displayed greater need for O2 administration. Twenty neonates were intubated; 16 of them were administered surfactant. Infection (P < 0.05), abnormal chest x-ray (P = 0.022), and the severity of respiratory system morbidity (P < 0.05) prolonged neonatal in-patient stay. Respiratory problems (P = 0.003) and intubation (P = 0.032) incurred greater hospitalization costs. Breastfeeding initiation before the 3rd day of life (P = 0.031), and O2 administration for more than 72 h (P = 0.036) were significantly associated with the length of in-patient stay in the multivariate regression analysis. Conclusion: Mandating the presence of a pediatrician in the delivery room would optimize justified direct NICU admissions and reduce the possibility of delayed diagnosis of respiratory distress during rooming-in. NICU in-patient stay in full term neonates should be based on combining diagnostic markers of sepsis, such as procalcitonin or interleukin-6. A specific protocol regarding surfactant administration in intubated full term infants is also necessary. The severity of respiratory system morbidity is not the key determinant of infant feeding. Maternal information regarding infant health and breastfeeding abilities may improve breastfeeding rates.
Keywords:
newborn – respiratory – distress – tachypnea – NICU
Introduction
Respiratory distress represents a rather routine cause of hospital admission in the neonatal intensive care unit (NICU) during the early neonatal period, ranging between 7% and 15% for full-term neonates, 29% for late pre-terms (between the 34th and 37th week of gestation), and even a higher percentage in premature newborns less than 34 weeks of gestation. Neonatal respiratory distress is recognized through various symptoms of breathing difficulty (i.e. grunting, tachypnea, nasal flaring and chest retractions) with or without cyanosis [1–3].
Among term neonates, those between the 37th and 38th week of gestation (early terms) are more prone to develop respiratory distress and demonstrate increased morbidity in terms of the duration of mechanical ventilation, need for surfactant administration and prolonged hospitalization, compared to those who were born after the 38th week [4]. Specific risk factors increase the likelihood of breathing problems among full term newborns, including meconium or amniotic fluid aspiration, caesarean section (CS), gestational diabetes mellitus, chorioamnionitis, as well as oligohydramnios or structural lung anomalies. Nevertheless, identifying newborns who will develop respiratory problems is not always possible [2].
Irrespective of the cause of breathing difficulty, early identification and adequate management may prevent the development of respiratory failure and cardio-respiratory arrest. Hence, differential diagnosis is central to the therapeutic approach of respiratory distress, since the latter may stem from either the respiratory tract system (i.e. transient tachypnea, pneumothorax, pneumonia, meconium aspiration, etc.), or the cardiovascular system (i.e. pulmonary hypertension, congenital heart disease), or other hematologic, neurologic, musculoskeletal, and metabolic disorders, congenital anomalies, injuries and infections [5]. Among the aforementioned causes of respiratory distress in full term newborns, transient tachypnea (TTN) is most commonly encountered, and is usually associated with elective CS [6].
Hence, although full term babies with breathing difficulties seem to represent the majority of NICU admissions in Greece at a nationwide level, no study has attempted to assess the respective percentages so far. The aim of the present study was threefold:
a) to assess and analyze the respiratory problems of full term newborn babies during their first hours of life in Greece;
b) to compare parameters related to the length of NICU in-patient stay, taking into account potential requirements for O2 administration;
c) to discuss perinatal care practices, which could reduce the morbidity, and associated costs of NICU hospitalization, and restrict the premature and involuntary separation of the maternal-newborn duo during the first post-natal days [7,8].
Materials and methods
Data collection
A retrospective chart review was conducted between July 31st 2017 and March 2nd 2018 in a tertiary maternity hospital. The hospital provides gynecological and maternity services to women belonging to the Prefecture of Attica, and monitoring of high-risk pregnancies at a nationwide level. All births along with the mode of delivery were initially recorded. NICU admissions were subsequently searched and recorded, and the notes involving newborns with respiratory problems were retrieved. Related demographic data, along with birth conditions and morbidity during NICU hospitalization, were subsequently recorded.
Univariate analyses were performed using chi-square testing for qualitative data, whilst potential associations between quantitative variables were explored using the non-parametric Mann--Whitney test. Multiple linear regression models were used to determine the respective odds ratio (along with the 95% CI) for the associations, which were found to be significant in the univariate analyses. All analyses were performed using SPSS version 25.0. Statistical significance was accepted at the level of 0.05.
Criteria for NICU admission and in-patient stay
Full-term newborns typically remained in the delivery room with their mothers for the first two hours of their life for monitoring and stabilization. During this acclimatization period the dyad also familiarized themselves with the practice of skin-to-skin contact and breast-feeding.
NICU admission directly from the delivery room depended on the respective clinical presentation and vital signs (i.e. Apgar score < 8 in the first 10 min after birth, SatO2< 95%, grunting, increased respiratory workload, which persisted after newborn resuscitation). Umbilical cord blood gas values represented an additional criterion in high-risk pregnancies (i.e. gestational diabetes mellitus, intra-uterine growth retardation, congenital anomalies, etc.), or when unexpected complications occur during delivery (i.e. uterine rupture, placental abruption, umbilical cord prolapse, meconium-stained amniotic fluid, induced labor, administration of analgesics/sedatives, irregular fetal heart rate, or malpresentation) [9].
The mode of respiratory support (invasive, non-invasive) and percentage of supplemental O2 administration (FiO2< 0.30, or FiO2> 0.30) during NICU in-patient stay was decided under continuous monitoring of the newborn’s vital signs (heart rate, blood pressure, O2 saturation) [10]. Newborns were intubated when FiO2 was greater than 35% and/or pH value was less than 7.2, despite own respiratory efforts [11].
Results
About 2,303 live term births were recorded, among which 1,939 newborns were delivered by CS (84.2%). NICU admissions represented 34.6% of live births (N = 797), whereas 59 newborns were readmitted for several reasons (7.4%). From the total number of new admissions to the NICU, 120 presented with respiratory difficulty (18.8%). Thirty-four of these babies (4.2%) were transported to another unit, primarily due to capacity restrictions or need for highly specialized treatment (Tab. 1). Hence, 86 babies with respiratory problems were finally studied. The majority of these newborns (43%) represented early term neonates (37th week of gestation), whereas 31.4% were born between the 38th and 39th week, and 13.9% between the 39th and the 42nd week of gestation. The mean birth weight was 3,049 g; four newborns weighed less than 2,500 g, and one more than 4,000 g. Approximately 88% of the studied babies were appropriate for their gestational age, whereas 6.9% were small, and 4.6% were large for their gestational age.
Tab. 1. Reasons for term newborn admission in NICU or Special Care Units.
Tab. 1. Důvody pro přijetí novorozence v termínu na novorozenecké JIP nebo na jednotky speciální péče.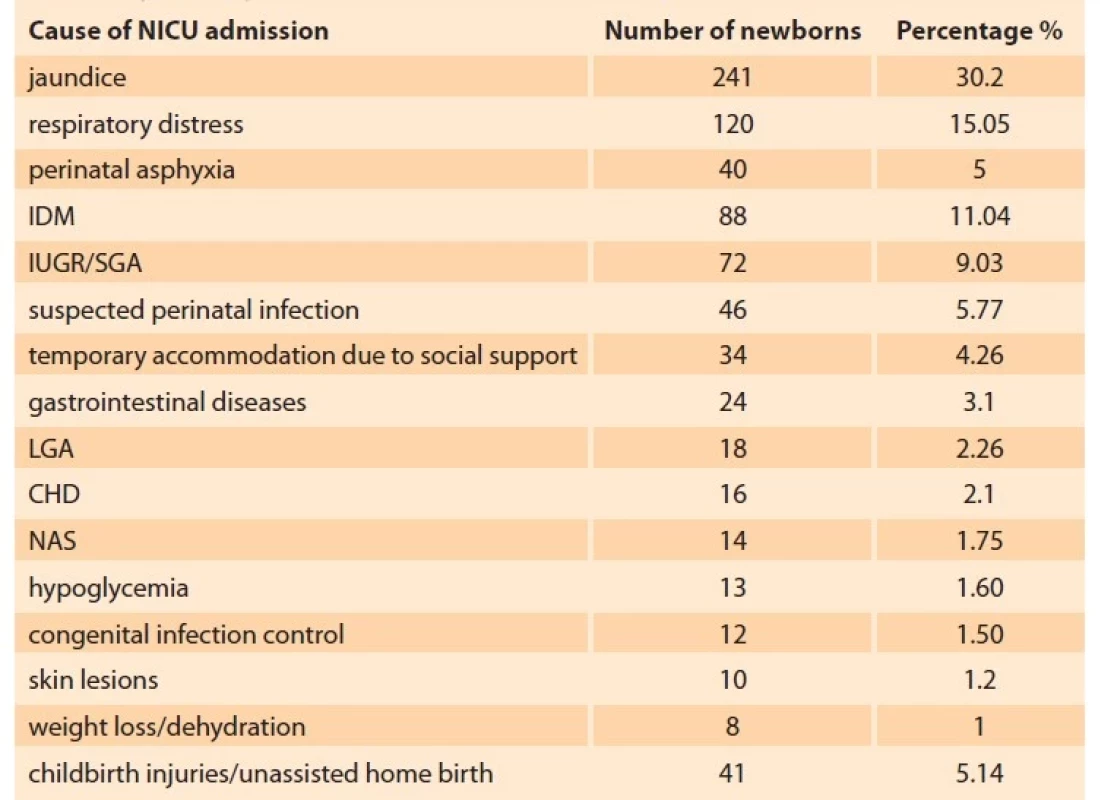
CHD – congenital heart disease, IDM – infants of diabetic mother, IUGR/SGA – intra-uterine growth retardation/small for gestational age, LGA – large for gestational age, NAS – neonatal abstinence syndrome, NICU – neonatal intensive care unit The mode of delivery was vaginal in 11.6% of the studied newborns (N = 10), and CS in the remaining 88.4% (N = 76). Then, 57.8% of the latter were performed due to a previous CS (N = 44), 2.6% due to twin pregnancy (N = 2), 6.5% due to breech presentation (N = 5), 2.6% due to post-term pregnancy (N = 2), and 1.3% due to maternal HPV infection (N = 1). CS performed due to fetal distress, hydramnios, or obstetric cholestasis was considered as an emergency and represented 6.6% of cases. Semi-elective CS was performed due to cephalo-pelvic disproportion in 15.8% of cases (N = 12), intra-uterine growth retardation (IUGR) in 2.6% (N = 2), and premature rupture of the membranes (PROM) in 3.9% (N = 3).
The causes of respiratory problems among newborns admitted to the NICU are summarized in Fig. 1. About 79.1% of newborns who were admitted due to respiratory distress did not require resuscitation in the delivery room (N = 68), whilst 20.9% (N = 18) were resuscitated. Newborn resuscitation was performed according to the respective European guidelines [12–17]. A decision regarding the necessity to intubate the newborn was based either on special circumstances (i.e. hiatus hernia, meconium aspiration, congenital anomalies, etc.), or on the presumed ineffectiveness of non-invasive positive pressure ventilation (NIV) [18,19].
Fig. 1. Causes of respiratory problems among full term newborns admitted in the NICU (absolute numbers).
Obr. 1. Příčiny respiračních problémů u donošených novorozenců přijatých na novorozenecké JIP (absolutní počty).
CE – cyanotic episode, CHD – congenital heart disease, Met Pro – metabolic problems, NAS – neonatal abstinence syndrome, Neo Polycyt – neonatal polycythemia, NICU – neonatal intensive care unit, PA – perinatal asphyxia, PH – pulmonary hypertension, RDS – respiratory distress syndrome, TTN – transient tachypnea of the newborn About 46.5% of newborns (N = 40) were either not administered O2 (N = 33) or O2 administration did not exceed 24 hours (N = 7) during their in-patient stay, compared to 53.4% (N = 46) who required longer O2 administration; this finding was not affected by previous resuscitation. Chest radiography in the former patient category was either normal or depicted signs of transient tachypnea. The mode of respiratory support in the latter patient category was decided according to the respective clinical signs and O2 saturation [10], and is shown in Fig. 2. Supplemental O2 in the incubator or a head-box was administered in 12 neonates, all of which required FiO2 < 0.30. About 16.3% of neonates (N = 14) received n-CPAP; FiO2 < 0.30 was necessary in nine and > 0.30 in five of these neonates. Twenty neonates (23.2%) received mechanical ventilation with FiO2 > 0.30, apart from a case with pneumothorax, in whom the respective FiO2 was less than 0.30 (Fig. 2). The vast majority of intubated newborns (N = 16) were administered surfactant. Among the four intubated newborns without surfactant administration, two had signs of TTN and a normal chest x-ray, one had perinatal asphyxia, and one was diagnosed with persistent pulmonary hypertension (PPHN) based on cardiac triplex findings. Surfactant was also administered in two n-CPAP neonates (following the MIST and INSURE modes of administration, respectively) with FiO2 > 0.30.
Fig. 2. Mode of respiratory support in full term newborns with respiratory distress.
Obr. 2. Způsob podpory dýchání u donošených novorozenců s respirační tísní.
CMV – conventional mechanical ventilation, nCPAP – nasal Continuous Positive Airway Pressure With regard to infection markers, newborns not requiring O2 administration did not have positive blood cultures. Only 12.5% (N = 5) had increased CRP, which gradually normalized, and 20% (N = 8) received first-line antibiotic treatment. The mean in-patient stay was 5.6 days. Newborn feeding in the first day of life was initiated in 62.5% (N = 25), yet only 37.5% (N = 15) achieved full enteral nutrition on the first day. About 17.5% (N = 7) of these newborns experienced exclusive breastfeeding, 75% (N = 30) any breastfeeding, and 7.5% (N = 3) received formula feeding.
In contrast, among the 46 newborns who were administered O2 for longer than 24 hours, 28.2% (N = 13) had increased CRP, and 8.7% (N = 4) had positive blood cultures (Enterobacter cloaca in one, and Staphylococcus epidermidis in three cases). First-line double antibiotic regimen consisting of ampicillin and aminoglycoside was administered in 53.5% (N = 25) of newborns, based on strong suspicion of infection from the clinical signs of the respiratory system. Third-generation cephalosporin on the basis of the antibiogram susceptibility was subsequently given to two of these newborns (4.4%), and a second-line double antibiotic regimen consisting of vancomycin and aminoglycoside in seven (15.2%). The mean in-patient stay was 8.58 days. Newborn feeding in the first day of life was initiated in 26% (N = 12), in the second in 52.1% (N = 24), in the third in 10.8% (N = 5), and after the third day in the remaining 10.8% (N = 5). However, only one newborn achieved full enteral nutrition by the second day (2.2%), and almost all (N = 45) after the third day of life. About 15.2% (N = 7) of these newborns experienced exclusive breastfeeding, 76.1% (N = 35) had any breastfeeding, and 8.7% (N = 4) received formula feeding.
Comparison of parameters related to the length of NICU in-patient stay and O2 administration (univariate analysis)
O2 administration
Newborns, who were admitted to the NICU due to respiratory distress, but did not require O2 administration, did not differ from those who were administered O2 in gender (P = 0.449), median birth weight (P = 0.221), gestational age (P = 0.694), parity (P = 0.637), mode of delivery (P = 0.363), or reason for performing CS (P = 0.104). The same applied with regard to positive infection markers, i.e. elevated CRP or positive blood culture (P= 0.073, and P = 0.056 respectively). However, newborns who were resuscitated in the delivery room, displayed greater need for O2 administration (P = 0.004). In addition, newborns who were admitted to the NICU due to respiratory distress immediately from the delivery room, displayed greater need for O2 administration compared to their counterparts, who were transported from the maternity ward after the first hours of rooming-in with their mothers (P = 0.000).
Length of NICU in-patient stay
The length of NICU in-patient stay for neonates who were admitted due to respiratory problems did not seem to be affected by gender (P = 0.262), parity (P = 0.954), labor anesthesia or analgesia (PGA = 0.262, Pepidural = 0.632), resuscitation (P =0.519), umbilical cord gas values (P = 0.350), or performing intubation (P = 0.147). In addition, paraclinical tests, such as cranial ultrasound (P = 0.292) and echocardiogram (P = 0.096), along with phototherapy (P = 0.057) and cesarean section (P = 0.854) were also not significant regarding the length of in-patient stay.
In contrast, the presence of infection (i.e. elevated CRP [P = 0.000], positive blood culture [P = 0.003], or antibiotic administration [P = 0.000]), the identification of an abnormal chest x-ray (P = 0.022), and the severity of respiratory system morbidity, as depicted by surfactant administration (P = 0.004), O2 requirement of more than 30% (P = 0.045), or for more than 72 hours (P = 0.002) appeared to prolong the neonatal in-patient stay.
Neonatal feeding
The respective feeding mode (exclusive breastfeeding, formula feeding, or mixed feeding – henceforth termed any breastfeeding) was not affected by O2 administration (P = 0.770, P = 0.720, and P = 0.850, respectively) (Tab. 2). Although newborns not requiring O2 administration initiated feeding in the first 24 hours, achieved full enteral nutrition before the third day of life, and were also breastfed before the third day of life, compared to their counterparts, who were administered O2 (P = 0.001, P = 0.000, and P = 0.000, respectively), the total length of in-patient stay did not differ between the two groups (P = 0.270) (Tab. 2). Full enteral nutrition was also delayed in newborns, who required surfactant administration (P = 0.000), whereas all intubated newborns achieved full enteral nutrition after the third day of life, compared to 65.4% of their non-intubated counterparts (P = 0.003).
Tab. 2. Medical and socio-economic parameters of full term babies admitted in the NICU in relation with O2 requirement.
Tab. 2. Zdravotní a socioekonomické parametry donošených dětí přijatých na novorozenecké JIP v souvislosti s požadavkem O2.
* no O2 requirement included, ** combined breast and formula feeding
CRP – C-reactive protein, NICU – neonatal intensive care unitCost of NICU in-patient stay
The mean cost of infant in–patient stay in the NICU due to respiratory distress between infants who required O2 administration for longer than 24 h, and those requiring less than 24 h (or not at all) did not differ (P = 0.270). However, there was a difference in hospitalization costs between NICU-admitted term infants with respiratory problems, in comparison with those who were admitted for other reasons (P = 0.003). Furthermore, intubated neonates incurred greater median cost of in-patient stay compared to their non-intubated counterparts (P = 0.032), whereas surfactant administration proved to be borderline significant regarding its impact on the median cost of infant in-patient stay (P = 0.059).
Multivariate regression analysis
Breastfeeding initiation before the third day of life (P = 0.031) and O2 administration for more than 72 hours (P = 0.036) were significantly associated with the length of in-patient stay in the multivariate regression analysis. The former parameter was associated with shorter stay and the latter with increased in-patient stay, irrespective of the need for mechanical ventilation, FiO2, surfactant administration, abnormal chest x-ray, increased CRP, positive blood culture, time to full enteral nutrition, or final diagnosis. Furthermore, newborns in the former category were 44% less likely to remain in-patient for more than one week (OR = 0.056; 95% CI = 0.004–0.773), whilst newborns in the latter category had 7.916 more odds (95% CI = 1.149–54.539) for more than one week of in-patient stay.
Discussion
The results of the present study show that the majority of full term newborns admitted in the NICU due to respiratory problems were born by elective CS. This finding indicates the detrimental impact of this mode of delivery in relation to the morbidity of the respiratory system [20]. However, not all researchers accept this reservation, but may instead remain skeptical, as to whether this mode of delivery actually affects perinatal mortality in a negative manner [21]. Part of the problem is that more specific data regarding the impact of selective CS in perinatal mortality and morbidity in uncomplicated pregnancies still remain controversial [6,7,22–25].
Having said that and taking into account that elective CS is commonly practiced in some countries, establishing a protocol regarding the presence of a pediatrician in the delivery room is necessary if not imperative, since the possibility of resuscitation is increased [26] resulting in increased likelihood for subsequent O2 administration. This may come in stark contrast with everyday clinical practice in many maternity hospitals, including our own, where a pediatrician is present in the delivery room on a per required basis, depending on the presumed condition of the fetus and the expectant mother during or shortly before delivery, as well as a potentially adverse gestational history of the mother. However, neonatal assessment in the delivery room in the first hour of life reduces the possibility of delayed diagnosis of respiratory distress during the subsequent rooming-in stay with his/her mother in the maternity ward, and a potentially traumatic separation of the mother-newborn duo. Nonetheless, potential predisposing factors for resuscitation of full term newborns requiring pediatric attendance in the delivery room during elective CS are summarized in Tab. 3 [27].
Tab. 3. Reasons for pediatric attendance and potential resuscitation of full-term infants in cases of elective caesarean section.
Tab. 3. Důvody pro přítomnost pediatra a potenciální resuscitace donošených dětí v případech elektivního císařského řezu.
BMI – body mass index Full term infants who were intubated due to FiO2 > 0.35, blood gas acidosis, increased respiratory workload, and abnormal chest x-ray were also administered surfactant as a rescue therapy to avoid complications stemming from significant respiratory distress, and reduce the ensuing infant morbidity and mortality [28]. This practice was not followed in a case with pre-existing PPHN, two cases of TTN with a normal chest x-ray, and a case of perinatal asphyxia. Taking into account that the administration of surfactant in everyday clinical practice may depend on the attending physician and neonate on an individual basis as the indications for surfactant administration in intubated term infants represent a subject not yet fully clarified in the existing literature, clinical practices similar to the ones followed in the presented newborn cohort could serve as a basis of forming a respective protocol.
A significant percentage of neonates admitted in the NICU due to respiratory distress improved relatively quickly, having TTN, as the working diag-nosis [12,29,30]. The primary mech-anism behind TTN appears to be the delayed clearance of pulmonary fluid either due to immaturity or the lack of fetal thorax compression that occurs during labor when elective CS is performed. Even though this condition is thought to be benign and self-resolving, it seems to be associated with NICU admission, separation from the mother, and unnecessary exposure to antibiotics. Different strategies and antenatal interventions for TTΝ management should be more systematically assessed in future studies [31], potentially including keeping the mother-infant pair in the delivery area for the first 2 h of life as a standard practice in order to assess whether the respiratory distress of the infant demonstrates signs of stabilization.
Although the majority of neonates in the present study displayed quick recovery from their respiratory problems, they appeared to have prolonged their stay in the NICU. This finding could be interpreted either as a proof of timely intervention or an indication of unnecessary initial intervention. Indeed, the multivariate regression analysis revealed that the full term infants in the present study remained in-patient irrespective of the mode of respiratory support (i.e. need for mechanical ventilation, surfactant administration), laboratory findings (i.e. abnormal chest x-ray, increased CRP, positive blood culture), time to full enteral nutrition, or final diagnosis. Delayed respiratory stabilization (i.e. O2 administration for more than 72 hours (OR = 0.056) and breastfeeding initiation before the third day of life (OR 7.916) were the only parameters significantly associated with the length of in-patient stay. These findings indicate that basing the clinical decision of keeping this category of neonates in-patient, mainly on borderline non-specific positive inflammation markers (i.e. CRP), or antibiotic treatment initiation (with the view of prolonging their administration), may result in unnecessary increase to the respective length of in-patient stay, which in turn results in increased costs in hospitalization. Reducing a potentially unnecessary stay in NICU represents a case in point for medical practitioners in National Health Systems, having as an end--point to propose and organize monitoring programs for both a safe and cost-effective in-patient stay [9,32–35]. The standard use of a combination of more than one early diagnostic marker of sepsis, such as procalcitonin or interleukin-6, may further improve the effectiveness of sepsis risk assessment in in-patient neonates [36].
The median in-patient stay for newborns who were admitted to NICU due to respiratory distress, but did not require O2 administration was 2 days shorter compared to their counterparts who were administered O2 (data not shown). Nevertheless, mildly tachypneic newborns with SatO2 greater than 94% and a normal chest x-ray could remain with their mothers in the maternity ward provided that other morbidity parameters have been excluded. Upon discharge, these babies should be monitored at home for a time period of four weeks. That is because respiratory distress could result from other co-morbidities, which should be excluded, if the clinical condition of the newborn does not coincide with the results of imaging or laboratory testing [37].
As far as infant feeding is concerned, although neonates not requiring O2 administration initiated breastfeeding earlier than their counterparts, who did require the final percentage of exclusively breastfed newborns did not differ. This finding suggests that the severity of respiratory system morbidity is not the key determinant of infant feeding. The stress of early separation between mother and infant, parental anxiety regarding the health status of the newborn, along with moving and self-caring difficulties of the mother following a CS seem to hinder breastfeeding initiation [38,39]. Hence, maternal information and encouragement with regard to infant health and breastfeeding abilities by the ward personnel may improve breastfeeding rates [40–42].
Conclusion
The present study analyzed respiratory problems of full term newborn babies during the first hours of life, and compared parameters related to the length of NICU in-patient stay.
The results show that the majority of full term newborns admitted in the NICU due to respiratory problems were born by elective CS indicating the detrimental impact of this mode of delivery in relation to the morbidity of the respiratory system. Although everyday clinical practice in many maternity hospitals requires the optional presence of a pediatrician in the delivery room, mandating such presence would not only optimize justified direct NICU admissions of full-term neonates following resuscitation, but also reduce the possibility of delayed diagnosis of respiratory distress during the mother-newborn rooming-in.
The vast majority of intubated full term infants were also administered surfactant as a rescue therapy. Although this represents a mainstay treatment practice, the respective indications are not yet fully clarified in the existing literature. Hence, such administration in everyday clinical practice may depend on the respective momentum of the physician and/or neonate rather than result from adherence to a specific protocol, thus necessitating the formation of a respective algorithm.
A significant percentage of neonates admitted in the NICU due to respiratory distress improved relatively quickly, having TTN as the working diagnosis. Although this condition is thought to be benign and self-resolving, it seems to be associated with NICU admission, separation from the mother, and unnecessary exposure to antibiotics.
Breastfeeding initiation before the third day of life (P = 0.031) and O2 administration for more than 72 hours (P = 0.036) were significantly associated with the length of in-patient stay in the multivariate regression analysis. The former parameter was associated with shorter stay and the latter with increased in-patient stay, irrespective of the need for mechanical ventilation, FiO2, surfactant administration, abnormal chest x-ray, increased CRP, positive blood culture, time to full enteral nutrition, or final diagnosis. Hence, NICU in-patient stay in full term neonates should not be based on borderline non-specific positive inflammation markers or antibiotic treatment initiation, but rather on clinical improvement, taking also into account the combination of more than one diagnostic markers of sepsis, such as procalcitonin or interleukin-6.
The severity of respiratory system morbidity is not the key determinant of infant feeding. Hence, maternal information and encouragement with regard to infant health and breastfeeding abilities by the ward personnel may improve breastfeeding rates.
ORCID authors
A. Fotiou 0000-0003-1011-096X
P. V. Vlastarakos 0000-0002-2803-1971
E. F. Tavoulari 0000-0002-4231-2307
Submitted/Doručeno: 4. 3. 2023
Accepted/Přijato: 3. 5. 2023
Prof. Petros V. Vlastarakos, MD, MSc, PhD, IDO-HNS
2nd ENT Department
University of Athens
ATTIKON University Hospital
1 Rimini Rd
124 62 Athnes
Greece
Zdroje
1. Chowdhury N, Giles BL, Dell SD. Full-term neonatal respiratory distress and chronic lung disease. Pediatr Ann 2019; 48 (4): e175–e181. doi: 10.3928/19382359-20190328-01.
2. Reuter S, Moser C, Baack M. Respiratory distress in the newborn. Pediatr Rev 2014; 35 (10): 417–429. doi: 10.1542/pir.35-10-417.
3. Kumar A, Bhat BV. Epidemiology of respiratory distress of newborns. Indian J Pediatr 1996; 63 (1): 93–98. doi: 10.1007/BF02823875.
4. Razak A, Nagesh KN, Karthik G et al. Morbidities in neonates delivered electively at early term. J Obstet Gynaecol India 2016; 66 (4): 248–251. doi: 10.1007/s13224-015-0739-0.
5. Sivanandan S, Agarwal R, Sethi A. Respiratory distress in term neonates in low-resource settings. Semin Fetal Neonat Med 2017; 22 (4): 260–266. doi: 10.1016/j.siny.2017.04.004.
6. Ahimbisibwe A, Coughlin K, Eastabrook G. Respiratory morbidity in late preterm and term babies born by elective caesarean section. J Obstet Gynaecol Can 2019; 41 (8): 1144–1149. doi: 10.1016/j.jogc.2018.11.002.
7. Signore C, Klebanoff M. Neonatal morbidity and mortality after elective cesarean delivery. Clin Perinatol 2008; 35 (2): 361–371. doi: 10.1016/j.clp.2008.03.009.
8. Rowe-Murray HJ, Fisher JR. Baby friendly hospital practices: cesarean section is a persistent barrier to early initiation of breastfeeding. Birth 2002; 29 (2): 124–131. doi: 10.1046/j.1523-536x.2002.00172.x.
9. Al-Wassia H, Saber M. Admission of term infants to the neonatal intensive care unit in a Saudi tertiary teaching hospital: cumulative incidence and risk factors. Ann Saudi Μed 2017; 37 (6): 420–424. doi: 10.5144/0256-7947.2017.420.
10. Foster JP, Buckmaster A, Sinclair L et al. Nasal continuous positive airway pressure (nCPAP) for term neonates with respiratory distress. Cochrane Database Syst Rev 2015; 11: CD011962. doi: 10.1002/14651858.CD011962.
11. Atasay B, Mungan Akın İ, Alan S. Respiratory distress and management strategies in the newborn. In: Aly H, Abdel-Hady H (eds). Respiratory management of newborns. London: IntechOpen 2016.
12. Madar J, Roehr CC, Ainsworth S et al. European resuscitation council guidelines 2021: newborn resuscitation and support of transition of infants at birth. Resuscitation 2021; 161 : 291–326. doi: 10.1016/j.resuscitation.2021.02. 014.
13. Soar J, Perkins GD, Maconochie I et al. European resuscitation council guidelines for resuscitation: 2018 update – antiarrhythmic drugs for cardiac arrest. Resuscitation 2019; 134 : 99–103. doi: 10.1016/j.resuscitation.2018.11.018.
14. Perkins GD, Olasveengen TM, Maconochie I et al. European resuscitation council guidelines for resuscitation: 2017 update. Resuscitation 2018; 123 : 43–50. doi: 10.1016/j.resuscitation.2017.12.007.
15. Soar J, Donnino MW, Maconochie I et al. 2018 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations summary. Resuscitation 2018; 133 : 194–206. doi: 10.1016/j.resuscitation.2018.10.017.
16. Olasveengen TM, de Caen AR, Mancini ME et al. 2017 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations summary. Circulation 2017; 136 (23): e424–e440. doi: 10.1161/CIR.0000000 000000541.
17. Monsieurs KG, Nolan JP, Bossaert LL et al. European resuscitation council guidelines for resuscitation 2015: section 1. Executive summary. Resuscitation 2015; 95 : 1–80. doi: 10.1016/ j.resuscitation.2015.07.038.
18. Sweet DG, Carnielli VP, Greisen G et al. European consensus guidelines on the management of respiratory distress syndrome: 2022 update. Neonatology 2023; 120 (1): 3–23. doi: 10.1159/000528914.
19. Sweet DG, Carnielli VP, Greisen G et al. European consensus guidelines on the management of respiratory distress syndrome – 2019 update. Neonatology 2019; 115 (4): 432–450. doi: 10.1159/000499361.
20. Tefera M, Assefa N, Mengistie B et al. Elective cesarean section on term pregnancies has a high risk for neonatal respiratory morbidity in developed countries: a systematic review and meta-analysis. Front Pediatr 2020; 8 : 286. doi: 10.3389/fped.2020.00286.
21. Pratilas GC, Sotiriadis A, Dinas K. Is high use of caesarean section sometimes justified? Lancet 2019; 394 (10192): 25–26. doi: 10.1016/S0140-6736 (19) 30221-1.
22. Clapp MA, James KE, Bates SV et al. Unexpected term NICU admissions: a marker of obstetrical care quality? Am J Obstet Gynecol 2019; 220 (4): 395.e1–395.e12. doi: 10.1016/j.ajog. 2019.02.001.
23. Hasan YW, Arrar SM. Neonatal and early childhood outcomes of esarean. World J Pharm Res 2019; 8 (5): 479–492. doi: 10.20959/wjpr 20195-14678.
24. Jain L, Eaton DC. Physiology of fetal lung fluid clearance and the effect of labor. Semin Perinatol 2006; 30 (1): 34–43. doi: 10.1053/ j.semperi.2006.01.006.
25. Gordon A, McKechnie EJ, Jeffery H. Pediatric presence at cesarean section: justified or not? Am J Obstet Gynecol 2005; 193 (3 Pt 1): 599–605. doi: 10.1016/j.ajog.2005.06.013.
26. Weir J, Smith S, Soper J. Neonatal resuscitation following elective caesarean section: an observational study. Pediatr Child Health 2015; 20 (5): e71. doi: 10.1093/pch/20.5.e71.
27. Zanardo V, Simbi KA, Vedovato S et al. The influence of timing of elective cesarean section on neonatal resuscitation risk. Pediatr Crit Care Med 2004; 5 (6): 566–570. doi: 10.1097/01.PCC.0000144702.16107.24.
28. Ramaswamy VV, Abiramalatha T, Bandyopadhyay T et al. Surfactant therapy in late preterm and term neonates with respiratory distress syndrome: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 2022; 107 (4): 393–397. doi: 10.1136/archdis child-2021-322890.
29. Betran AP, Ye J, Moller AB et al. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health 2021; 6 (6): e005671. doi: 10.1136/bmjgh-2021-005671.
30. Kim JH, Lee SM, Lee YH. Risk factors for respiratory distress syndrome in full-term neonates. Yeungnam Univ J Med 2018; 35 (2): 187–191. doi: 10.12701/yujm.2018.35.2. 187.
31. Buchiboyina A, Jasani B, Deshmukh M et al. Strategies for managing transient tachypnoea of the newborn – a systematic review. J Matern Fetal Neonat Med 2017; 30 (13): 1524–1532. doi: 10.1080/14767058.2016.1193143.
32. Baker EL, Parker LA, Alissa R. Decreasing admissions to the NICU: an official transition bed for neonates. Adv Neonat Care 2021; 21 (1): 87–91. doi: 10.1097/ANC.0000000000000765.
33. Davies S, Matchett M, Gouk E et al. Reducing term infant admissions into neonatal unit – quality improvement project. J Neonat Nurs 2021; 27 (Suppl 1): 82–87. doi: 10.1016/ j.jnn.2020.07.012.
34. NHS Improvement. Reducing harm leading to avoidable admission of full-term babies into neonatal units: summary. UK: NHS Improvement 2017. Publication code IG 02/17.
35. Antoniou E, Orovou E, Iliadou M. Cesarean sections in Greece. How can we stop the vicious cycle? World J Adv Res Rev 2021; 12 (1): 375–377. doi: 10.30574/wjarr.2021.12.1.0502.
36. Morad EA, Rabie RA, Almalky MA et al. Evaluation of procalcitonin, C-reactive protein, and interleukin-6 as early markers for diagnosis of neonatal sepsis. Int J Microbiol 2020; 2020 : 8889086. doi: 10.1155/2020/8889086.
37. Balfour-Lynn IM, Rigby ML. Tachypnoea in a well baby: what to do next? Arch Dis Child 2015; 100 (8): 722–727. doi: 10.1136/archdischild - 2014-306692.
38. Weir J, Smith S, Soper J. Neonatal resuscitation following caesarean section: a retrospective chart review. Pediatr Child Health 2015; 20 (5): e48. doi: 10.1093/pch/20.5.e48.
39. Ozlu F, Yapıcıoglu H, Ulu B et al. Do all deliveries with elective caesarean section need paediatrician attendance? J Matern Fetal Neonatal Med 2012; 25 (12): 2766–2768. doi: 10.3109/ 14767058.2012.703722.
40. Fan HS, Wong JY, Fong DY et al. Association between intrapartum factors and the time to breastfeeding initiation. Breastfeed Med 2020; 15 (6): 394–400. doi: 10.1089/bfm.2019.0166.
41. Serra G, Miceli V, Albano S et al. Perinatal and newborn care in a two years retrospective study in a first level peripheral hospital in Sicily (Italy). Ital J Pediatr 2019; 45 (1): 152. doi: 10.1186/s13052-019-0751-6.
42. Jaafar SH, Ho JJ, Lee KS. Rooming-in for new mother and infant versus separate care for increasing the duration of breastfeeding. Cochrane Database Syst Rev 2016; 2016 (8): CD006641. doi: 10.1002/14651858.CD006641.pub3.
Štítky
Dětská gynekologie Gynekologie a porodnictví Reprodukční medicína
Článek Editorial
Článek vyšel v časopiseČeská gynekologie
Nejčtenější tento týden
2023 Číslo 4- Alergie na antibiotika u žen s infekcemi močových cest − poznatky z průřezové studie z USA
- Horní limit denní dávky vitaminu D: Jaké množství je ještě bezpečné?
- Magnosolv a jeho využití v neurologii
- Isoprinosin je bezpečný a účinný v léčbě pacientů s akutní respirační virovou infekcí
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
-
Všechny články tohoto čísla
- Editorial
- Registration of a pregnant woman in the maternity hospital (optimally at 36th–37th weeks) at the Olomouc University Hospital in 2022
- Severe maternal morbidity requiring intensive care units admission in the Slovak Republic – a 9-year population based study
- Effect of umbilical cord drainage after spontaneous delivery in the third stage of labor
- Respiratory problems in full term newborns, which parameters are related to the length of in-patient stay?
- Direct abdominal muscle diastasis and stress urinary incontinence in postpartum women
- Use of serum copper and zinc levels in the diagnostic evaluation of endometrioma and epithelial ovarian carcinoma
- Bilateral tubal ectopic pregnancy after spontaneous conception
- Pure uterine lipoma – a paradoxical rarity
- The efficacy of human papillomavirus vaccination in the prevention of recurrence of severe cervical lesions
- Therapeutical strategies for recurrent endometrial cancer
- Uterine inversion – some procedures to prevent reinversion
- Follitropin delta – experience from clinical practice
- Česká gynekologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- The efficacy of human papillomavirus vaccination in the prevention of recurrence of severe cervical lesions
- Therapeutical strategies for recurrent endometrial cancer
- Direct abdominal muscle diastasis and stress urinary incontinence in postpartum women
- Effect of umbilical cord drainage after spontaneous delivery in the third stage of labor
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



