-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
MANAGEMENT OF INFECTED TIBIAL FRACTURES AND CHRONIC TIBIAL OSTEOMYELITIS BY MUSCLE FLAP TRANSFER: A COMPARISON OF TWO SERIES OF PATIENTS
Autoři: J. Záhorka 1; A. Nejedlý 2; M. Tvrdek 2; V. Džupa 1
Působiště autorů: Department of Orthopaedics, Third Faculty of Medicine, Charles University, Prague, and 1; Department of Plastic Surgery, Third Faculty of Medicine, Charles University, Prague, Czech Republic 2
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 51, 1, 2009, pp. 3-9
INTRODUCTION
Application of free flap or transpositional muscle and musculocutaneous flaps is considered the method of choice for the treatment of extensive soft tissue defects in the lower extremity (11, 15, 16). At the same time, treatment of tibial osteomyelitis after extensive soft tissue and bone debridement requires coverage of the defect with a muscle flap (3, 12, 13, 17, 23). Advantages of this method are: 1) good quality defect coverage after radical treatment, 2) autonomous blood supply of the flap allows distribution of the administered antibiotic into the area of defect, and 3) improvement of the long term blood supply to the area of fracture, which is important for healing (12, 17). At our workplace we started to use this method in 1985 (19, 23).
The goal of this work is to compare results of treatment of two groups of patients with infected fracture or chronic osteomyelitis in the area of the lower leg and ankle joint by the method of radical debridement of the skeleton and coverage of the defect by a free muscle flap or muscle transposition.
MATERIAL AND METHODS
Patients
The observed group comprised 52 patients, 10 females and 42 males with an average age of 44 years (aged between 10 and 67). The group was divided into two subgroups. Retrospectively we evaluated treatment results in 26 patients (6 females and 20 males) who underwent surgery between 1 January 2005 and 30 September 2007. Basic demographic data for both subgroups are listed in Table 1.
Tab. 1. Basic demographic data of both groups of patients 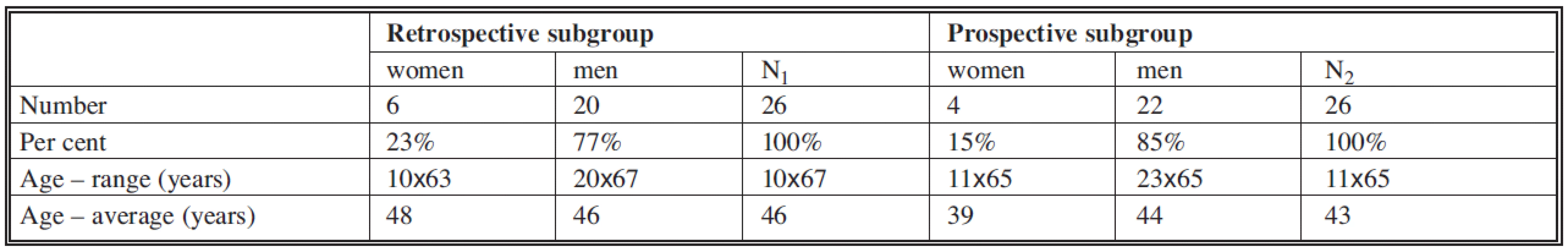
Indications
Indication for treatment: 1) Patients after ankle fractures with a non-healing infected soft tissue defect, 2) patients with tibial osteomyelitis. These were patients with indications for high lower leg amputation. Lists of subgroups of patients divided according to indications are provided in Table 2.
Tab. 2. List of patients of subgroups divided according to indication 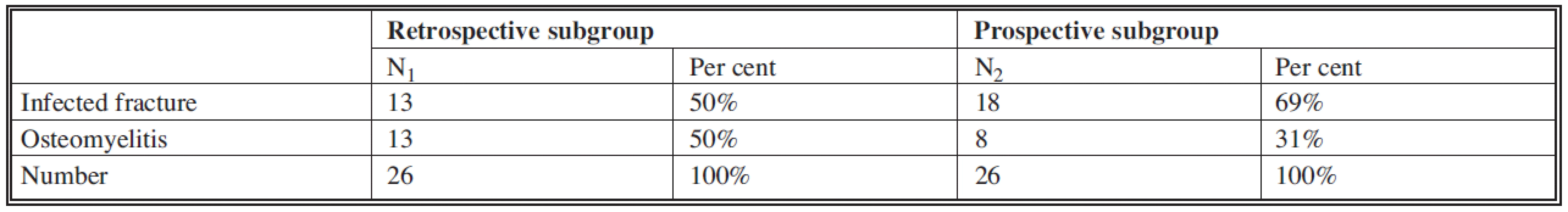
Operative technique
The debridement was completed in the first phase of the treatment. It consisted of removal of all macroscopically infected tissues and free bone fragments and sequesters. In patients with osteomyelitis completed tibial cavity trepanation by 10–12 mm wide groove within the extent of changes was confirmed by X-ray or CT scan, or in the extent of perisurgical macroscopically apparent changes. The criterion to determine the debridement border was vital bone and muscle tissue with capillary bleeding.
Another phase of treatment was to cover the defect with suitably chosen muscle or musculocutaneous flap. The flap was either in the form of muscle transposition (soleus muscle, medial gastrocnaemius) or free transferred muscle flap (gracilis muscle, rectus abdominis muscle, latissimus dorsi muscle). A list of flaps used can be found in Table 3. In free flaps the blood supply of the transferred flap was restored by microsurgical technique of anastomoses between blood vessels of the flap and recipient blood vessels in the area of defect. The most frequently used recipient blood vessels were blood vessels of the posterior tibial artery bundle.
Tab. 3. List of used free and transposition flaps in patients in both subgroups 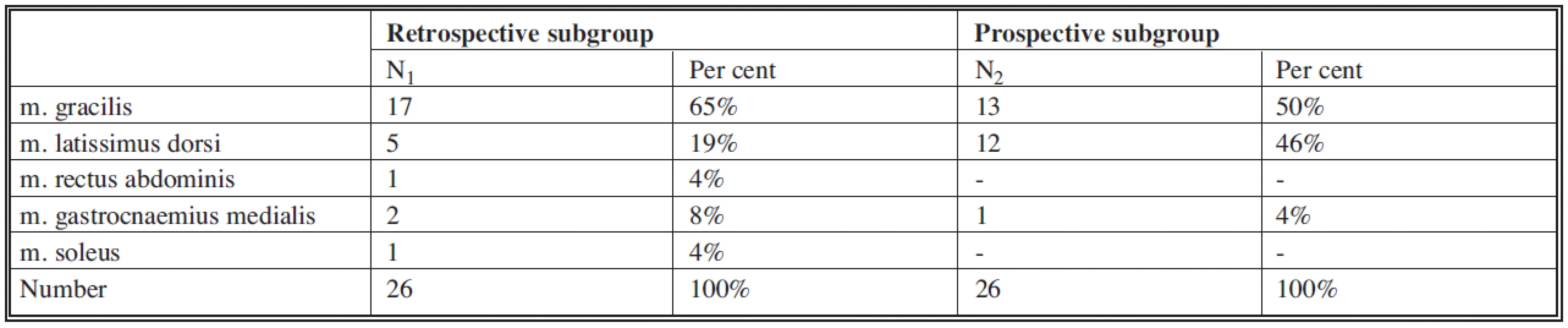
The decision to cover by a flap either in the period immediately after debridement (in 43 patients) or in the later period (in 9 patients) was influenced by: 1) diagnosis (infected fracture always immediately after debridement, osteomyelitis immediately or in later period), 2) perisurgical finding (flap immediately after debridement was completed only if it was certain that all the infected tissues were removed). Coverage of the defect by a flap in the later period was countermined by a negative cultivation of swab from the base of the defect.
In all patients we placed a drain under the flap until the drained volume was minimal (3–5 days). The end of the drain was sent to a bacteriological department for assessment after removal.
Blood supply of the flap was carefully monitored after the surgery. Covering the flap with a dermoepidermal graft harvested from the thigh was completed after permanently established good blood supply to the flap on the 3rd or 5th days after the transplant.
The difference between the retrospective and prospective parts of the study depended on how extensive the debridement and the necrectomy of soft tissues was. In the retrospective part of the study we took into consideration the size and shape of the future flap and accordingly decided how extensive the debridement should be. In the prospective part of the study we debrided and completed necrectomy into a good quality blood supplied tissue very radically, no matter what the extent of the created defect.
Perioperative management
In the perisurgical period all patients were administered intravenous antibiotics according to the sensitivity of the preoperatively cultivated microorganisms for a period of 7 to 10 days.
Next, all patients were administered a continual antithrombotic infusion for a period of 9 days (heparin, agapurin, mesocain). After that the antithrombotic prophylaxis continued until the period of management of mobilization of the patient (another 3 to 7 days) by administration of retarded heparin or low molecular heparins (in patients with DVT in anamnesis). After completion of low dose heparin administration we administered 200 mg of acetylsalicylic acid two times per day for 8 weeks.
Physiotherapy on bed rest started on the first day after surgery. Between the 9th and 12th day the patients were mobilized on crutches. Full weight bearing was allowed in patients with infected fracture after healing of the bone (6 to 14 months). Patients with osteomyelitis were partially weight-bearing until full integration of the flap (2 months after surgery).
Study design
The study is a comparison study of patients followed retrospectively and prospectively. We found the basic patient data of the followed group from documentation and X-ray documentation. Clinically, 25 patients were part of the retrospective study from February till March 2006 (one patient died due to myocardial infarction). The prospective part of study comprised 24 patients (one female and one male patient were repatriated after treatment) between February and March 2008. Comparability of both subgroups was evaluated based on:
- gender,
- age,
- indication for surgery,
- severity of the injury,
- type of fracture according to the AO classification (14),
- degree of soft tissue injury according to the Gustilo-Anderson classification,
- risk factors for occurrence of infection complication,
- number of prior surgeries in patients with infected fractures.
- Evaluation of results reached within the subgroups was compared by:
- number of postsurgical complications,
- number of necessary follow-up surgeries,
- actual weight-bearing ability of the extremity,
- satisfaction of patient with the completed treatment.
Statistical analysis
For the analysis of the results we used the statistical program EpiInfo. At the level of 5% significance we completed incidence comparison of chosen observed characteristics (age, gender, severity of injury, degree of soft tissue injury, infection risk factors, previous surgeries, postsurgical complications, follow-up surgeries, weight-bearing ability of the extremity).
RESULTS
In the retrospective part of the study the results of 25 patients (5 females and 20 males) were analyzed, and in the prospective part of the study the results of 24 patients (3 females and 21 males) were analyzed. The average period of observation in the retrospective group of patients was 27 months (between 15 to 49 months); in the prospective group of patients it was 18 months (between 7 to 37 months). Due to the shorter time of observation, two patients of the prospective part of the study were still undergoing treatment at the time of control.
Gender and age of patients
Difference in gender in both subgroups was not significant (p=0.510). Difference in ages in both subgroups (the patients in the prospective part of the study were 3 years younger) was also not significant (p=0.847).
Indication for surgery
The difference in both subgroups in the number of treated infected fractures (13 versus 18) and osteomyelitis (13 versus 8) was not significant (p=0.253).
Severity of injury, type of fracture, degree of soft tissue injury
Severity of injuries in the observed patients, type of fracture according to AO classification and soft tissue injuries according to Gustilo-Anderson are listed in Tables 4–6. Differences between both subgroups were not significant (Table 7).
Tab. 4. List of patients of subgroups divided according to severity of injury 
Tab. 5. List of patients of both subgroups according to the type of fracture (AO classification) 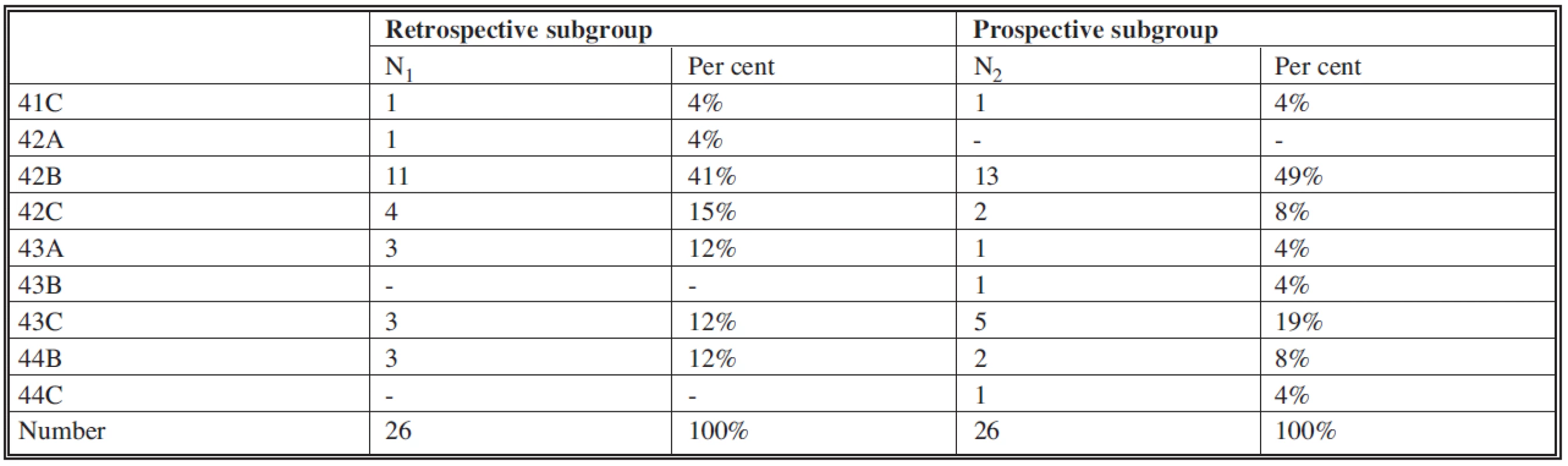
Tab. 6. List of patient of subgroups with open fracture according to Gustilo-Anderson classification 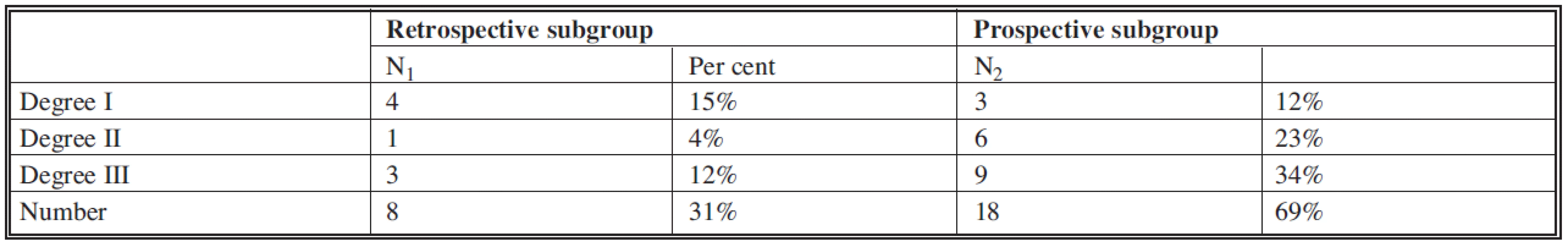
Risk factors for infection complications
In the retrospective part of the study we documented risk factors for infection complication in 11 patients (8 cases of open fracture, diabetes mellitus in 3 patients), in the prospective part we documented a total of 23 risk factors in 19 patients (19 cases of open fracture, 2 cases of nicotine abuse, one patient after lung resection due to tuberculosis and one case of obesity). The difference in risk factor occurrence was not significant (p=0.243, see Table 7).
Tab. 7. Comparison of followed parameters in both subgroups of the followed group 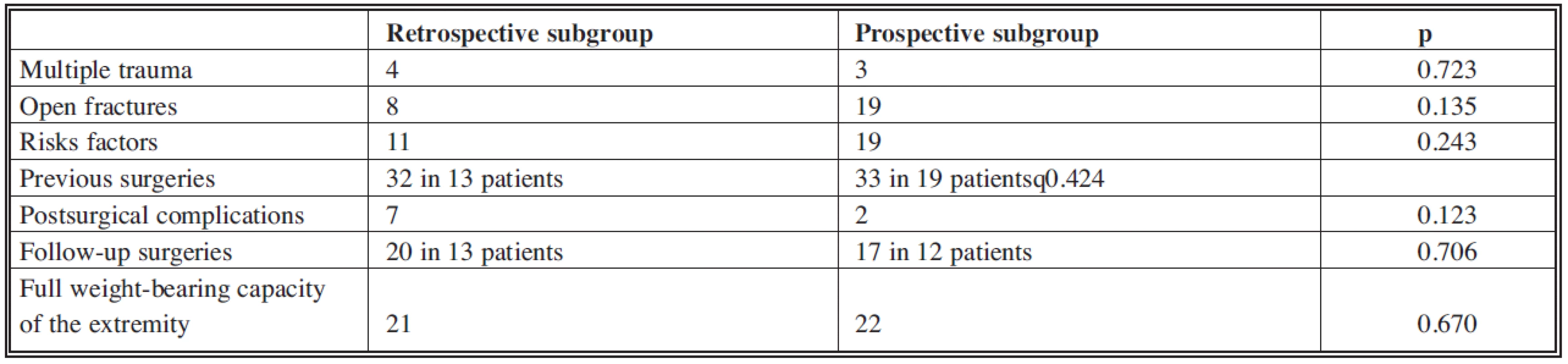
Preceding surgeries in patients with infected fracture
The number of preceding surgeries in 13 patients with infected fracture in the retrospective part of the study was 32 (between 1 and 4, average 2.5). In the prospective part of the study, in 18 patients with infected fracture, 33 preceding surgeries were completed (between 1 and 3, average 1.8). This difference was not significant (p=0.424, see Table 7).
Postoperative complications
In the retrospective part of the study postsurgical complications were documented in 7 patients (27%). Failure of blood supply to the flap early after surgery occurred in two patients (8%). This was resolved by revision and reanastomosis; in one case continuing ischemia of the flap required another flap transfer. Two patients (8%) developed purulent secretion due to residual infected tissues under the flap. In one case we completed revision and extensive redebridement (the patient was without relapse at a check-up 45 months after surgery). In the other patient the repeated secretion lead to an indication for extremity amputation. In three patients (12%) the fracture did not consolidate, and the extremity could not bear weight at the time of control. None of these patients at the time of control accepted the proposal to surgically solve the non-union.
In the retrospective part of the study postsurgical complications occurred in 2 patients (8%). In one patient (4%) failure of blood supply to the flap in the early postsurgical time was resolved by revision and reanastomosis. In one patient (4%) early secretion after surgery required extensive debridement, and the purulent complication did not reoccur. In two patients (8%) the fracture consolidation was not completed, and the extremity could not fully weight bear at the time of control.
The difference in the number of postsurgical complications in both subgroups was not significant (p=0.123, see Table 7).
Follow-up surgeries
In the retrospective part of the group 20 surgeries in 13 patients were completed (between 1 and 4 surgeries in one patient). In two cases this entailed revision of anastomoses due to failure of blood supply to the flap in the early post-surgical stage (in two patients), in one case it was transfer of a new flap, in four cases it was revision due to secretion (in two patients), three times it was reosteosynthesis (in three patients), in nine cases it was decortications and spongioplasty (in 8 patients), and there was one case of extremity amputation.
In the prospective part of the group we completed 17 follow-up surgeries in 12 patients (between 1 and 3 surgeries per patient). In one case it was revision of anastomoses due to a failure of blood supply to the flap in the early post-surgical period, once it was modelation of the flap, there was one case of revision due to secretion, in 8 cases it was reosteosynthesis (in 6 patients), there was one case of follow-up dynamization of the osteosynthesis, and in six cases it was decortications and spongioplasty.
In the prospective part of the study, after the treatment was completed tibial re-fracture occurred in two patients after an adequate trauma. These were resolved by a new osteosynthesis. These surgeries were not included in the number of follow-up surgeries.
The difference in number of follow-up surgeries was not significant in both parts of the group (p=0.706, see Table 7).
Actual weight-bearing capacity of the operated extremity
At the time of control 21 patients (84%) of the retrospective part of the group were fully weight-bearing, as were 22 patients (88%) of the prospective part of the group. Two patients from the prospective part of the group were not able to fully weight bear at the time of control; they were both still in treatment. However, even in the case of full recovery of the weight-bearing capacity in these patients, the difference was not significant (p=0.670, see Table 7).
Subjective evaluation by the patients
Subjective evaluation of the surgical results by patients is listed in Table 8. Five patients (20%) of the retrospective part of the group were not satisfied with the treatment, while none of the prospective part of the group made this claim. This difference was not significant (p=0.311).
In the retrospective part of the group the dissatisfied patients included three with non-union, one patient after amputation and one patient with primary completed arthrodesis of the ankle joint indicated for infected fracture reaching into the ankle joint. In the prospective part of the group none of the patients were dissatisfied; however, in the concluding evaluation we have considered as dissatisfied two patients who have not yet completed the treatment.
All 49 controlled patients (no matter the final result) responded positively to the question as to whether they would undergo this difficult treatment again.
DISCUSSION
The retrospective part of the study indicated that 20% of patients were dissatisfied with the treatment results (17). They perceived negatively the recurrence of the infection and their inability to fully weight bearing on the extremity, though they were not negative about the length of the treatment or the resulting cosmetic effect. That led us to the prospective study, where priority was safe debridement and necrectomy of non-vital tissues without respect to the extent of the defect. Prior experience leads us to the conclusion that in the area of the lower leg it is possible to cover any size defect with a muscle flap. We were interested to establish whether such a study would bring significantly better results. From Table 3 it is obvious that the size of flaps used was greater in the prospective part of the study. That confirms that we maintained the basic postulate of the prospective study of how radical the debridement was.
Gender and age of patients
The number of patients in each subgroup was the same; differences in gender distribution and age were not significant. Therefore, within the basic indicators we can consider both groups comparable.
Severity of injury, type of fracture, degree of soft tissue injury
In these respects, too, the subgroups did not show any significant differences (Table 4–7). Many authors points to the higher risk of infection complications in patients with comminuted fractures and devastation of soft tissues (15, 18, 24). Both subgroups corresponded to that category, because 21 patients (81%) or 23 patients (88%) had type B or C fracture according to the AO classification (see Table 5).
Risk factors for developing infection complication
Many publications point to a higher incidence of infection complications in some patients with risk factors (rheumatoid arthritis, diabetes mellitus with glycemia above 12 mml/L, malnutrition defined by long term leucopenia under 1.5x109/l, hypalbunemia under 35g/L and level of transferrin under 2.26 g/L, known immunodeficiency, distant focal infection, psoriasis with damage to the skin integrity, obesity, long term corticosteroid therapy, age above 75, hemophilia, alcoholism, nicotinism, intravenous drugs abuse, severe injury to the soft tissues after open and closed fractures, polytrauma, long term stay at the anesthesiology and resuscitation unit) (1, 5, 9, 21, 22). We therefore used this criterion as the main factor to compare both groups. In the prospective part of the study we noticed a higher occurrence of risk factors (11 versus 23); however, this difference was not significant (Table 7). Therefore, even in terms of evaluated risk factor we can regard the two groups as comparable.
Preceding surgeries in patients with infected fracture
The number of preceding surgeries in patients with infected fractures is also important for comparison of both groups. Repeated revisions without being able to cover the area of the fracture with a well perfused tissue is a risk factor for development of infection complication (8, 10, 15, 16). However, the difference in the number of preceding surgeries (32 versus 33) was not significant (Table 7). So in this respect too, both subgroups were comparable.
Postoperative complications
The occurrence of complications in 27% of patients from the retrospective part of the study led us to complete the prospective part of the study with the goal of increasing the extent of the debridement and necrectomy. In the prospective part of the study we noted only 8% of complications. However, this difference was not significant (Table 7).
Failure of flap blood perfusion in the early postsurgical time occurred in 8% and 4% of patients respectively. This finding corresponded to the level of 12% found by other authors (3, 15). Failure of the flap can be considered a failure of the method. However, during long-term inflammation we have always found scarring of the blood-vessel bundles used as recipient blood vessels. Its preparation was always extremely difficult. Luckily, in two patients we managed to solve this complication by reanastomosis and in one patient by a new free transfer.
Recurrence of infection usually leads to amputation. We consider this the main failure of the treatment. It occurred in one patient of the retrospective part of the study. A similar complication has also been described by other authors (15).
We consider the development of pseudoarthrosis as an adverse result even if infection is eliminated. We noted this complication only in patients in the retrospective part of the study. We therefore think that analysis of complications showed better results in the prospective part of the study, despite the lack of statistical proof.
Follow-up surgeries
Several authors commented on the necessity to biologically stimulate healing after the defect was covered by a flap in some patients (7, 10). We also noted this in patients of our group. Twenty follow-up surgeries in 13 patients (50%) of the retrospective subgroup and 17 surgeries in 12 patients (46%) of the prospective subgroup are comparable numbers.
Actual weight-bearing capacity of the operated extremity
Even in this aspect we did not notice significant difference between the subgroups. However, recovery of full weight-bearing capacity in 84% and 92% of patients respectively can be considered a very positive result. Naique et al. documented restoration of full weight-bearing in 74% of extremities after a devastating injury of tibia treated by muscle flap transfer (15).
Subjective evaluation by patients
Subjective evaluation by a patient is always misleading. Results can be influenced by the way the questions are asked. Nevertheless, we list the results in our work. All patients commented at the time of control assessment that they would undergo this procedure again in order to maintain their extremity.
CONCLUSION
Results achieved during the treatment of patients of the group we followed allow us to express following conclusions about the method of extensive debridement with following covering of the soft tissue defect by a free muscle flap:
- Radical debridement of skeleton and extensive necrectomy of non-vital soft tissues is the main requirement to manage the infection.
- Covering of the defect by a well-perfused flap allows healing of the infected skeleton.
- Surgical biological support of healing of the infected fractures that follows is possible and usually leads to recovery of full weight-bearing capacity.
- We use this method at our workplace during the treatment of tibial osteomyelitis as a method of choice.
The study was supported by a grant from Internal Grant Agency of the Ministry of Public Health, Czech Republic, NR 8538-4/2005 “Comprehensive treatment of infectious complications of devastating injuries of the tibia”.
Address for correspondence:
Jiří Záhorka, M.D.
Department of Orthopaedics, Third Faculty of Medicine,
Charles University
Šrobárova 50
100 34 Prague 10
Czech Republic
e-mail: jiri.zahorka@seznam.cz
Zdroje
1. Bonnaire F., Hohaus T., Cyffka R., Lein T. Knocheninfektionen. Unfallchirurg, 73, 2002, p. 716-733.
2. Dzupa V., Dzupova O., Bendova E., Zahorka J., Richtr V., Bartoska R., Skala-Rosenbaum, J., Zidka M. Infectious complications of surgically treated musculoskeletal injuries: review of risk factors and etiological agents in years 2000–2005. (In Czech) Klin. Mikrobiol. Inf. Lek., 13, 2007, p. 242-247.
3. Gonzalez MH., Tarandy DI., Troy D., Phillips,D., Weinzweig N. Free tissue coverage of chronic traumatic wounds of the lower leg. Plast. Reconstr. Surg., 109, 2002, p. 592-600.
4. Gustilo RB., Anderson JT. Prevention of infection in the treatment of bone, thousand and twenty-five open fractures of long bones: Retrospective and prospective analysis. J. Bone Joint Surg., 58-A, 1976, p. 453-458.
5. Hanssen AD., Rand JA. Evaluation and treatment of infection at the site of a total hip or knee arthroplasty. J. Bone Joint Surg., 80-A, 1998 p. 910-922.
6. Harley BJ., Beaupre LA., Jones CA., Dulai SK., Weber DW. The effect of time to definitive treatment on the rate of nonunion and infection in open fractures. J. Orthop. Trauma, 16, 2002, p. 484-490.
7. Chen CE., Ko JY., Pan CC. Results of vancomycin-impregnated cancellous bone grafting for infected tibial nonunion. Arch. Orthop. Trauma Surg., 125, 2005, p. 369-375.
8. Jaeger K., Giebel GD. Treatment of osteomyelitis using free myocutaneous flap in the lower leg. Handchir. Mikrochir. Plast. Chir., 19, 1987, p. 104-108.
9. Jahoda D., Nyč O., Pokorný D., Landor I., Sosna A. Antibiotic treatment for prevention of infectious complications in joint replacement. (In Czech) Acta Chir. Orthop. Traumatol. Cech., 73, 2006, p. 108-114.
10. Khouri RK., Shaw WW. Reconstruction of the lower extremity with microvascular free flaps: A 10-year experience with 304 consecutive cases. J. Trauma, 29, 1987, p. 1086-1094.
11. Kuokkanen HO., Tukiainen EJ., Asko-Seljavaara S. Radical excision and reconstruction of chronic tibial osteomyelitis with microvascular muscle flaps. Orthopedics, 25, 2002, p. 137-140.
12. Kutscha-Lissberg F., Hebler U., Kalicke T., Arens S. Prinzipien chirurgischer Therapienkonzepte der postoperativen und chronischen Osteomyelitis. Orthopäde, 33, 2004, p. 439-454.
13. Mader JT., Wang J., Calhoun JH. Antibiotic therapy for musculoskeletal infections. J. Bone Joint Surg., 83-A, 2001, p. 1878-1890.
14. Müller ME., Nazarian S., Koch P., Schatzker J. The comprehensive classification of fractures of long bones. Berlin, Heidelberg, New York: Springer-Verlag, 1990.
15. Naique SB., Perse M., Nanchahal J. Management of severe open tibial fractures. The need for combinated orthopaedic and plastic surgical treatment in specialist centers. J. Bone Joint Surg., 88-B, 2006, p. 351-357.
16. Nejedly A., Tvrdek M., Stehlik J. Final report of the Grant IGA MZ CR 1651-3 „Early tissue transport in management of injury with defect of lower limb“. (In Czech) Prague: Third Faculty of Medicine, Charles University, 1995.
17. Nejedly A., Dzupa V., Zahorka J., Tvrdek M. Muscle flap transfer of the treatment infected tibial and malleolar fractures and chronic osteomyelitis of the tibia. (In Czech) Acta Chir. Orthop. Traumatol. Cech., 74, 2007, p. 162-170.
18. Ochsner PE., Müller U. Acute Infection. In Rüedi TP., Murphy WM. (Eds) AO Principles of Fracture Management. Stuttgart, New York: Thieme, 2000, p. 729-747.
19. Pros Z., Tvrdek M., Kletensky,J., Nejedly A., Svoboda S. Chronic traumatic wounds of the leg. Acta Chir. Plast., 38, 1996, p. 83-86.
20. Salvana J., Rodner C., Browner BD., Livingston K., Schreiber J., Pesanti E. Chronic osteomyelitis: Results obtained by an integrated team approach to management. Conn. Med., 69, 2005, p. 195-202.
21. Stuhldreier G, Gaebel G, Kramer W, Neugebauer W. Beobachtungen zur posttraumatischen Osteitis. Akt. Traumatol. 19, 1989, p. 28-34.
22. Stastnik M. Antimicrobial prophylaxis in surgery. (In Czech) Klin. Mikrobiol. Inf. Lek., 10, 2004, p. 73-79.
23. Tvrdek M., Nejedly A., Kletensky J., Kufa R. Treatment of chronic osteomyelitis of the lower extremity using free flap transfer. Acta Chir. Plast., 41, 1999, p. 46-49.
24. Willenegger H., Roth B. Behandlungstaktik und Spätergebnisse bei Frühinfekt nach Osteosynthese. Unfallchirurgie, 12, 1986, p. 241-246.
Štítky
Chirurgie plastická Ortopedie Popáleninová medicína Traumatologie
Článek ČESKÉ SOUHRNY
Článek vyšel v časopiseActa chirurgiae plasticae
Nejčtenější tento týden
2009 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Léčba bolesti po jednodenní chirurgii
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Neodolpasse je bezpečný přípravek v krátkodobé léčbě bolesti
-
Všechny články tohoto čísla
- PRESERVATION OF VENOUS OUTFLOW IMPROVES TRANSVERSE RECTUS ABDOMINIS MUSCULOCUTANEOUS FLAP SURVIVAL FOLLOWING VASCULAR DELAY
- THE EFFICACY OF MAGNESIUM SULFATE ON RESOLVING SURGICALLY PROVOKED VASOSPASM OF THE FLAP PEDICLE IN AN EXPERIMENT
- AWARD OF THE G. WHITAKER INTERNATIONAL BURNS PRIZE FOR 2009 PALERMO, ITALY
- THE EFFECT OF BLOOD AROUND A FLAP PEDICLE ON FLAP PERFUSION IN AN EXPERIMENTAL RODENT MODEL
- USE OF PIEZOELECTRIC BONE SCALPEL IN HAND AND RECONSTRUCTIVE MICROSURGERY
- MANAGEMENT OF INFECTED TIBIAL FRACTURES AND CHRONIC TIBIAL OSTEOMYELITIS BY MUSCLE FLAP TRANSFER: A COMPARISON OF TWO SERIES OF PATIENTS
- ČESKÉ SOUHRNY
- G. WHITAKER INTERNATIONAL BURNS PRIZE – PALERMO (Italy)
- Acta chirurgiae plasticae
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- USE OF PIEZOELECTRIC BONE SCALPEL IN HAND AND RECONSTRUCTIVE MICROSURGERY
- MANAGEMENT OF INFECTED TIBIAL FRACTURES AND CHRONIC TIBIAL OSTEOMYELITIS BY MUSCLE FLAP TRANSFER: A COMPARISON OF TWO SERIES OF PATIENTS
- THE EFFICACY OF MAGNESIUM SULFATE ON RESOLVING SURGICALLY PROVOKED VASOSPASM OF THE FLAP PEDICLE IN AN EXPERIMENT
- ČESKÉ SOUHRNY
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



