-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
NEUROCUTANEOUS METACARPAL FLAPS
Autoři: M. Kateva; K. Dimitrov
Působiště autorů: Pirogov Hospital for Emergency Medicine, Hand Surgery Department, Sofia, Bulgaria
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 50, 3, 2008, pp. 89-92
INTRODUCTION
The dorsal skin, subsutaneous tissue and the sensory branches (1, 2) are supplied with blood by the perforative branches of the radial artery, the dorsal carpal branch of the ulnar artery, the dorsal metacarpal arteries and the palmar digital arteries. Each perforative branch that is directed to the skin gives collaterals supplying an area of 3.5 cm2 (17). Most of the perforative branches can be found at the level of the radiocarpal joint, carpometacarpal joints and the middle 1/3 of the metacarpals and the metacarpophalangeal joints. In the paraneural tissue the neurocutaneous perforative branches are connected in collateral arteries – 0.2–0.4 mm in diameter. Branches originating from these vessels enter inside the nerve and form intraneural longitudinal vessels (14, 2, 15). There are many anastomoses between the extra and the intraneural vascular network (13). There are branches separating from the paraneural arteries that direct themselves to the underlying fascia (10). Each artery is accompanied by two comitant veins that drain into the larger subcutaneous venous vessels (4, 12, 8) (Fig. 1).
Fig. 1. Blood and nerve supply of the flap 
MATERIALS AND METHOD, SURGICAL TECHNIQUE
The neurocutaneous flaps are based on the constancy of the para - and intraneural vessels (2, 18, 13, 16, 6). Based on topography, the flaps that can be raised from the dorsum of the hand are as follows (Fig. 2):
Fig. 2. Topography of the flap raising 
- based on the superficial branch of the radial nerve with all its branches,
- at the level of the IV and V carpometacarpal joint based on the dorsal branches of the ulnar nerve.
The flap is centered over the dorsal sensory branch. It is developed from proximal to distal – skin, subcutaneous tissue and fascia. The point of rotating the flap (pivot point) is up to the middle 1/3 of the proximal phalanx. The location of the anastomoses is between the paraneural arteries with the dorsal branches of the palmar digital arteries (6).
CASE STUDY
A 30-year-old male presenting with a lateral soft tissue defect at the level of middle and distal phalanx of the index finger caused by a circular saw (Fig. 3).
Fig. 3. Soft tissue defect of the hand 
The flap is marked in the first intermetacarpal space, centered over the ulnar branch of the superficial branch of the radial nerve. The nerve is resected at the proximal edge of the flap, and the accompanying artery is ligated. The flap was developed as cutaneous-subcutaneous-fascial one with the size of the defect (Fig. 4).
Fig. 4. Course of the operation 
The pedicle is separated distally with 1 cm paraneural tissue up to the base of the proximal phalanx where the pivot point is. The donor site was closed primarily with intradermal suture. Clinical result after 6 months: full range of movement in the interphalangeal joints is achieved as well as protective sensation (Fig. 5).
Fig. 5. Clinical result after 6 months 
RESULTS
We performed 11 reconstructions with neurocutaneous flaps. All flaps survived. Two flaps presented with edge necrosis at the distal site of the flap (Tab. 1, Fig. 6).
Tab. 1. Neurocutaneous flap reconstruction – Survey 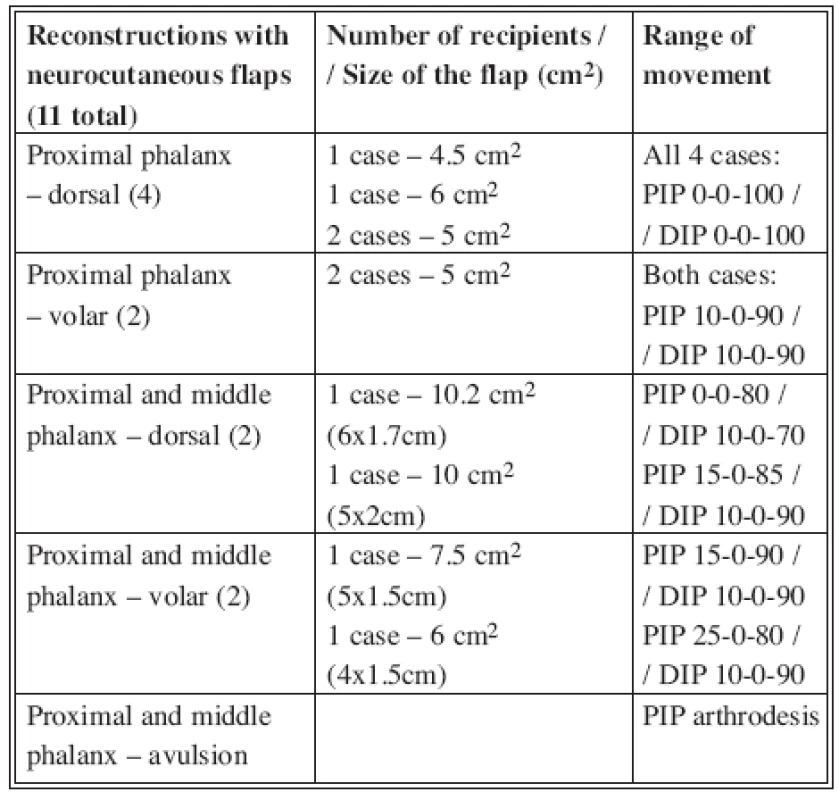
Fig. 6. Flap survival and post-op range of movement 
There were no postoperative infections in our reconstructive operations. We consider that success is founded on thorough but reasonable debridement, atraumatic approach at the most during developing the flap and its re-attachment, adequate rheologic protection combined with good perfusion of the flap. Authors such as Dautel, Merle (7) and Oberlin, Vuppalapati (19) use retrograde island flaps for coverage of infected defects.
Our results with edge necrosis (6.7%) are comparable with those in other studies by leading authors in this field (5, 11, 3). The reason for inadequate oxygenation at the distal site of the flap is decreased venous drainage. This is most often caused by compression or torsion of the pedicle during wound closure. In our cases with edge necrosis we performed a secondary suture.
DISCUSSION
There are many plastic methods known for reconstruction of finger defects. The non-free distant flaps from other regions of the body like Miura-Nacamura flap, Mc Cash’s cross-arm flap, etc., involve prolonged immobilization of the hand to the donor site, which often leads to interphalangeal joins contracture. These methods involve multi-stage surgical procedure – separation of the flap, modeling and remodeling operations. The donor skin is much larger than the recipient site and differs in structure. The duration of treatment is between 90 and 120 days.
The forearm non-free flaps (Chinese flap, interoseous flap) have the opportunity for resensibilization, but they barely reach the base of the proximal phalanx of the long fingers after being rotated distally. Moreover, these flaps sacrifice a main artery with significant cold intolerance up to 1 year postoperatively. They are also connected with heavy and long morbidity of the donor site. Immobilization of the hand attached to the donor site is no less than three weeks. Separation, remodeling and rehabilitation follow. The patient returns to his normal work not earlier than after 6 months. Reconstruction of only cutaneous-subcutaneous defect with a distant non-free flap requires at least 70 days for complete recovery.
METHOD ADVANTAGES
With the retrograde dorsal metacarpal flaps, when the donor site is closed primarily, the hand is immobilized for only a week to 10 days. This decreases the risk of developing contractures. Physiotherapy follows, and the patient is back to his normal life in about a month.
These flaps correspond to the defect size. The subcutaneous layer of the dorsal skin is thin, and therefore it does not require a remodeling procedure later – as is the case with forearm flaps or the groin flaps. In most cases the donor site can be closed primarily (defects less than 2.5cm2). Good blood supply of the cutaneous-subcutaneous-fascial flap makes it appropriate for coverage of infected defects. The operative technique is comparatively easy, requires magnification up to 3.5x. There are no main arteries sacrificed.
METHOD DISADVANTAGES
The use of neurocutaneous flap causes loss of sensation distal to the donor site.
When the flap is wider than 2.5 cm in the metacarpal region and wider than 1 cm in the finger zone, the donor site requires free skin graft.
If there is a postoperative scar at the dorsum of the hand then it might require additional surgical procedure for cosmetic reasons.
Address for correspondence:
Margarita Kateva, M.D.
Pirogov Hospital For Emergency Medicine,
Hand Surgery Dept.
Totleben 21 blvd.
Sofia1606
Bulgaria
E-mail: mkateff@yahoo.com
Zdroje
1. Bertelli J. Neurocutaneous axial island flaps in the forearm: anatomical, experimental and preliminary clinical results. Br. J. Plast. Surg., 46, 1993, p. 489.
2. Bertelli J., Khoury Z. Neurocutaneous island flaps in the hand: anatomical basis and preliminary results. Br. J. Hand Surg., 45, 1992, p. 586–590.
3. Bertelli J., Catarina S. Neurocutaneous island flaps in upper limb coverage: experience with 44 clinical cases. J. Hand. Surg., 22A, 1997, p. 515–526.
4. Botte M., Cohen M., Lavernia C., von Schroeder H., Gellman H., Zinberg E. The dorsal branch of the ulnar nerve: an anatomic study. J. Hand Surg., 15A, 1990, p. 603–607.
5. Brunelli F., Mathoulin C. Presentation d’un nouveau lambeau en ilot homo-digital sensible a contre-courant. Ann. Chir. Main., 10, 1991, p. 48–53.
6. Casoli V., Pelissier P.: The retrograde neurocutaneous island flap of the dorsal branch of the ulnar nerve: anatomical basis and clinical application. Surg. Radiol. Anat., 26, 2004, p. 8–13.
7. Dautel G., Merle M.. Dorsal metacarpal reverse flaps: anatomical basis and clinical applications. J. Hand Surg., 16B, 1991; p. 400–405.
8. Del Pinal F., Taylor G. The venous drainage of nerves; anatomical study and clinical implications. Br. J. Plast. Surg., 43, 1990, p. 511–520.
9. Foucher G., Smith D., Pempinello C., Braun F., Citron N. Homodigital neurovascular island flaps for digital pulp loss. J. Hand Surg., 14B, 1989, p. 204–208.
9. Hallock G. “Microleaps” in the progression of flaps and grafts. Clin. Plast. Surg., 23, 1996, p. 117–138.
10. Karacalar A., Ozcan M. A new approach to the reverse dorsal metacarpal artery flap. J. Hand Surg., 22A, 1997, p. 307–310.
11. Lunborg G., Dahlin L. Anatomy, function, and pathophysiology of peripheral nerves and nerve compression. Hand Clin., 12, 1996, p. 185–193.
12. Masquelet A., Romana M., Wolf G. Skin island flaps supplied by the vascular axis of the sensitive superficial nerves: anatomic study and clinical experience in the leg. Plast. Reconstr. Surg., 89, 1992, p. 1115–1121.
13. Murata K., Inada Y. Clinical application of the reversed pedicled venous flap containing perivenous areolar tissue and/or nerve in the hand. Br. Ass. Plast. Surg., 54, 2001, p. 615–620.
14. Nakajima H., Imanishi N., Fukuzumi S., Minabe T., Aiso S., Fujino T. Accompanying arteries of the cutaneous veins and cutaneous nerves in the extremities: anatomical study and a concept of the venoadipofascial and/or neuroadipofascial pedicled fasciocutaneous flap. Plast. Reconstr. Surg., 102, 1998, p. 779–791.
15. Nakajima H., Imanishi N., Fukuzumi S., Kishi K., Fujino T., Minabe T. The veno - and/or neuroadipofascial pedicled flap. In Harii K., ed. Transactions of the 11th Congress of the International Confederation of Plast. Reconstr. Aesthet. Surg. Amsterdam: Kugler Publications, 1995, p. 609.
16. Olave E. Perforating branches: important contribution to the formation of the dorsal metacarpal arteries. Scand. J. Plast. Reconstr. Hand Surg., 32, 1998, p. 221–227.
17. Shalaby H., Saad M. The venous island flap: is it purely venous? Br. J. Plast. Surg., 46, 1993, p. 85–87.
18. Vuppalapati G., Oberlin C. Distally based dorsal hand flaps: clinical experience, cadaveric studies and an update. Br. Ass. Plast. Surg., 57, 2004, p. 653–667.
Štítky
Chirurgie plastická Ortopedie Popáleninová medicína Traumatologie
Článek ČESKÉ SOUHRNY
Článek vyšel v časopiseActa chirurgiae plasticae
Nejčtenější tento týden
2008 Číslo 3- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Neodolpasse je bezpečný přípravek v krátkodobé léčbě bolesti
- Léčba akutní pooperační bolesti z pohledu ortopeda
-
Všechny články tohoto čísla
- THE PRESERVATION OF A SPARE HEMI-ABDOMINAL FLAP IN UNILATERAL BREAST RECONSTRUCTION WITH ABDOMINAL FREE FLAP IN HIGH RISK PATIENTS
- PRIMARY RECONSTRUCTION OF ARTERIAL SUPPLY IN THE PALM AFTER AN INJURY: A CASE STUDY
- CLINICAL EFFICACY OF A NEW CHITIN NANOFIBRILS-BASED GEL IN WOUND HEALING
- SYNMASTIA – AN UNUSUAL COMPLICATION OF AUGMENTATION MAMMAPLASTY
- NEUROCUTANEOUS METACARPAL FLAPS
- PERFORATOR-BASED FOREARM ISLAND FLAP
- ČESKÉ SOUHRNY
- Acta chirurgiae plasticae
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- ČESKÉ SOUHRNY
- SYNMASTIA – AN UNUSUAL COMPLICATION OF AUGMENTATION MAMMAPLASTY
- NEUROCUTANEOUS METACARPAL FLAPS
- CLINICAL EFFICACY OF A NEW CHITIN NANOFIBRILS-BASED GEL IN WOUND HEALING
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



