-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
GIANT CELL REPARATIVE GRANULOMA IN THE MANDIBLE – CASE REPORT AND REVIEW OF THE LITERATURE
Autoři: M. Hubáček 1; T. Dostálová 1; M. Bartoňová 2; J. Kozák 1; M. Seydlová 1
Působiště autorů: Charles University in Prague, nd Medical School, Department of Paediatric Stomatology, Prague and 1; Charles University in Prague, 1st Faculty of Medicine, Department of Stomatology, Prague Czech Republic 2
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 50, 2, 2008, pp. 59-63
INTRODUCTION
Before the early 1950s, central giant cell lesions of the jaws were generally diagnosed as giant cell tumor usually found in epiphyseal regions of long bones. In 1953, Jaffe proposed the term “giant cell reparative granuloma” to distinguish this lesion from the giant cell tumor. Jaffe believed that the jaw lesions were not true neoplasms and represented a local reparative reaction (13). Central GCG is defined by the World Health Organization as an intraosseous lesion consisting of cellular fibrous tissue containing multiple foci of hemorrhage, aggregations of multinucleated giant cells, and, occasionally, trabeculae of woven bone (17). Peripheral giant cell granuloma (PGCG) is a reactive exophytic lesion occurring on the gingiva and alveolar ridge originating from the periosteum or periodontal membrane, usually as a result of local irritating factors after tooth extraction, poor dental restorations, food impaction, ill-fitting dentures, plaque, and calculus (17).
The lesions occur more frequently in females than in males and are more often located in the mandible than in the maxilla. The age of most patients ranges from 10 to 25 years (18). The incidence of 1.1 per 106 was found for the whole population (1.05 per 10 for males, 1.25 per 106 for females). This means that the female predilection is not as large as was earlier assumed (man:female = 1 : 2). There was a peak incidence for males between 10 and 14 years of age and for females between 15 and 19 years of age. The lesions did occur twice more often in the mandible than in the maxilla (4).
Giant-cell granuloma – clinical findings
There is considerable variation in the clinical behavior of GCG. It may occur with rapid onset of pain, paraesthesia, root resorption, and tooth displacement. This form is also able to expand or damage surrounding bone, resulting in facial asymmetry. Another form of CGCG is sometimes asymptomatic and may be simply encountered through routine examinations (10).
In the most cases, the lesion presents as a painless, slow-growing swelling of the jaw. Pain and sensory disturbances are rare. Intraorally, a swelling with sometimes a bluish-brown aspect can be observed. Displacement of teeth occurs frequently and can lead to a malocclusion (5).
The PGCG manifests as a red-purple nodule located in the region of the gums or edentulous alveolar margins, commonly in the lower jaw. The lesion can develop at any age. It is, however, more common in the fifth and sixth decades of life with a slight female predilection. Peripheral GCG rarely affects the underlying bone, although the latter may cause superficial erosion (11).
Radiological findings
Radiological findings are diverse, ranging from small unilocular lesions to large multilocular lesions with displacement of teeth and tooth germs, root resorption, and cortical perforation (10). The tendency to be aggressive and multilocular increases in the same way as the size of the lesion (3, 24). CT can give a more detailed analysis of the GCG. The soft-tissue distribution of the lesion, cortical perforation, the rate of bone destruction and the expansion into anatomical features such as the maxillar sinus, nasal cavity and the orbita are better examined with CT than conventional radiology (3).
Differential diagnosis
In the differential diagnosis, there are lesions which causes are salivary gland, fibrous, nervous, bone and lymphoid tissue (16). In this case, the place of the lesion and the mucosa being intact on it made us think firstly about minor salivary gland neoplasm. On the other hand, in the histopathological differential diagnosis, other giant cellular lesions of the bone should be kept in mind; such as primary or secondary hyperparathyroidism, fibrous dysplasia, cherubism, and aneurismal bone cysts (21).
Histology
Highly cellular, fibroblastic stroma with plump, spindle-shaped cells with a high mitotic rate; the vascular density is high. Dystrophic calcification and metaplastic ossification are often seen, especially around the periphery of the lesion.
Etiology
The etiology is unknown but the occurrence of CGCG in patients with anomalies with a known genetic origin such as neurofibromatosis type 1, cherubism, and Noonan syndrome (Noonan-like/multiple giant cell lesion syndrome) indicates a genetic-related etiology. In 1994, a Chinese report described chromosome abnormalities in giant cell tumors in the long bones and in 1999 a case of chromosome translocation in a CGCG of the distal phalanx was published (t(X;4)(q22;q31.3)(7, 9). Also in 1999, chromosome translocations in aneurysmal bone cysts, which are giant cell granuloma-like lesions, were demonstrated (2).
Therapy
Surgical curettage is still the most frequently applied therapy. Surgical options vary from excisional biopsy to block resection, according to the level of soft-tissue invasion and the contagion of the mass. The most widespread treatment is the curettage or resection of the lesion (1). The limits of the lesion are incised with a laser or cryroprobe (12).
Corticosteroid and steroid injections (15, 20), calcitonin and IFNα application (6, 22) can be also methods of choice.
CASE REPORT
Patient – 22-year-old male
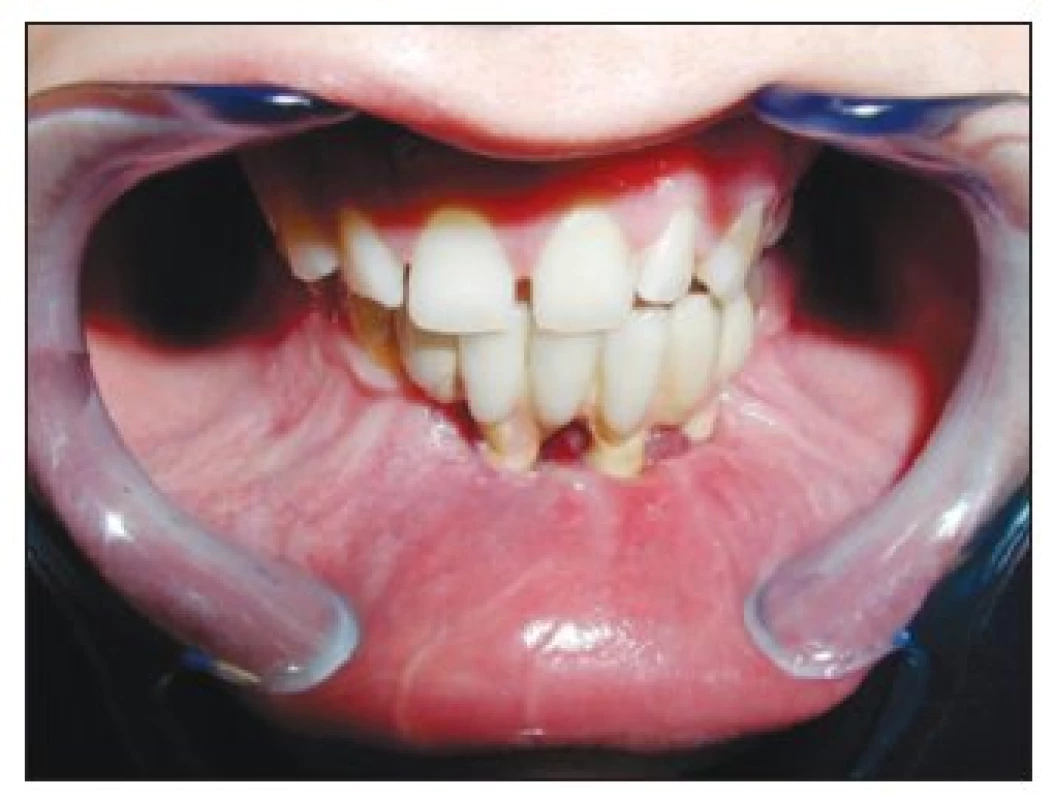
As a 9-year-old boy (in 1994), generally healthy, the patient was admitted to the Department of Paediatric Stomatology at the Faculty Hospital Prague-Motol with a swelling in the frontal area of mandible. Consequent to the examination and investigation, pain, bleeding, ulceration, loss of weight were not found. In the physical examination, a 20 mm x 20 mm sized mass was located in the left canine of the lower jaw. The mass was smooth, covered with mucosa, and was found to be elastic in palpation. No other pathology was identified other than these findings. The pre-operative orthopanthonogram image (Fig. 1) showed 55 mm x 25 mm sized oval mass, noticeable radiolucent. The cavity was observed to be contusing the mandible and causing expansion. The routine hematological and biochemical test results were within normal limits.
Obr. 1. A 9-year-old boy with an aggressive CGCG of the mandible 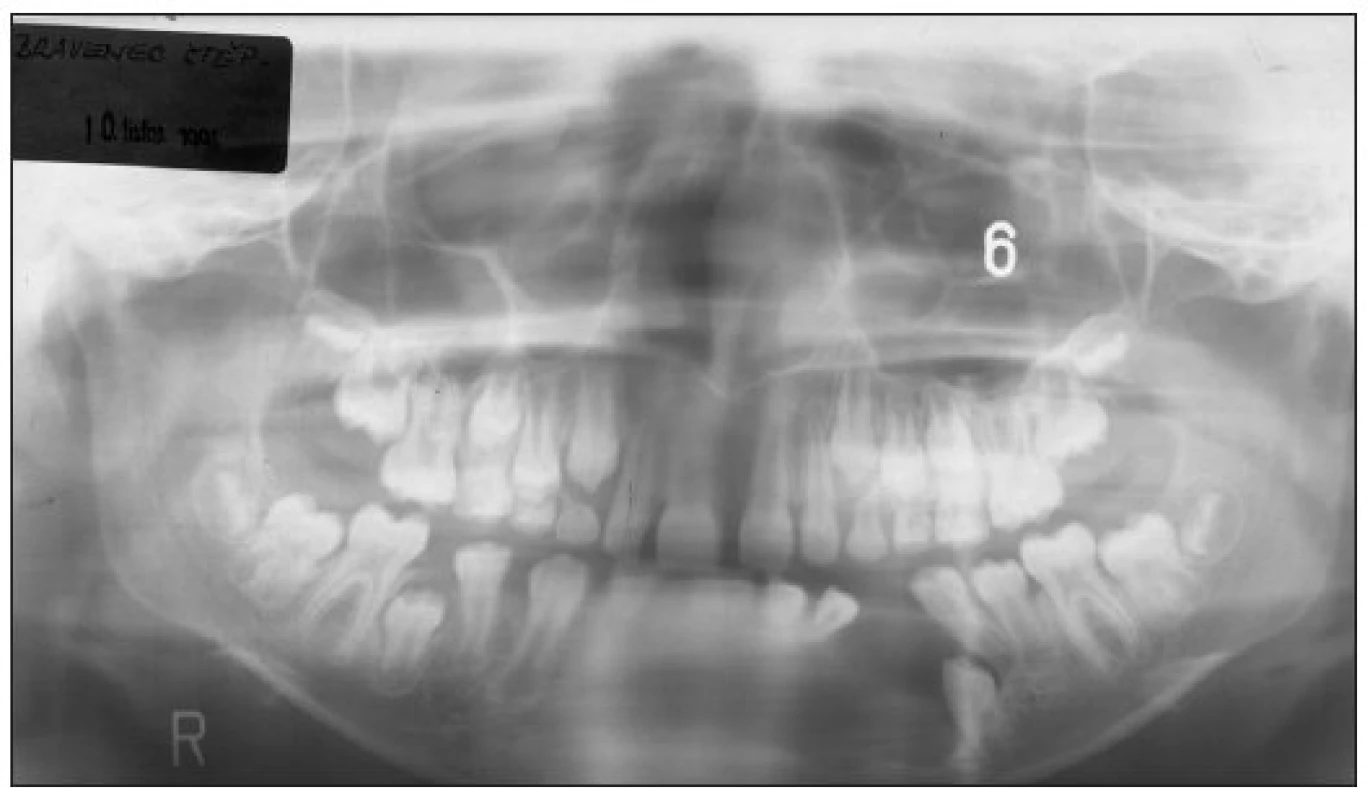
Upon these findings, a surgical curettage was applied. Under general anesthesia, and with safety limits, the mass was incised with a cutter and moved from the mandible and excised from there by curettage. The teeth 33, 32, 31, 41, 42 were extracted. The intra-operative biopsy was affirmed to be benign. The histology results showed large cytoplasmic cells with coarse chromatin and a large number of giant cells on the hemorrhagic surface. The osteoclast-like giant cells had a patchy distribution usually associated with areas of hemorrhage. A high number of osteoclast like giant cells in a stroma rich with fibroblasts showed hemorrhage, and a lesion made up of new bone formations was detected. Upon these findings, the case was diagnosed. On the physical examination that took place six weeks post-operatively, it was found that the epithelization process was complete and the defect was healed.
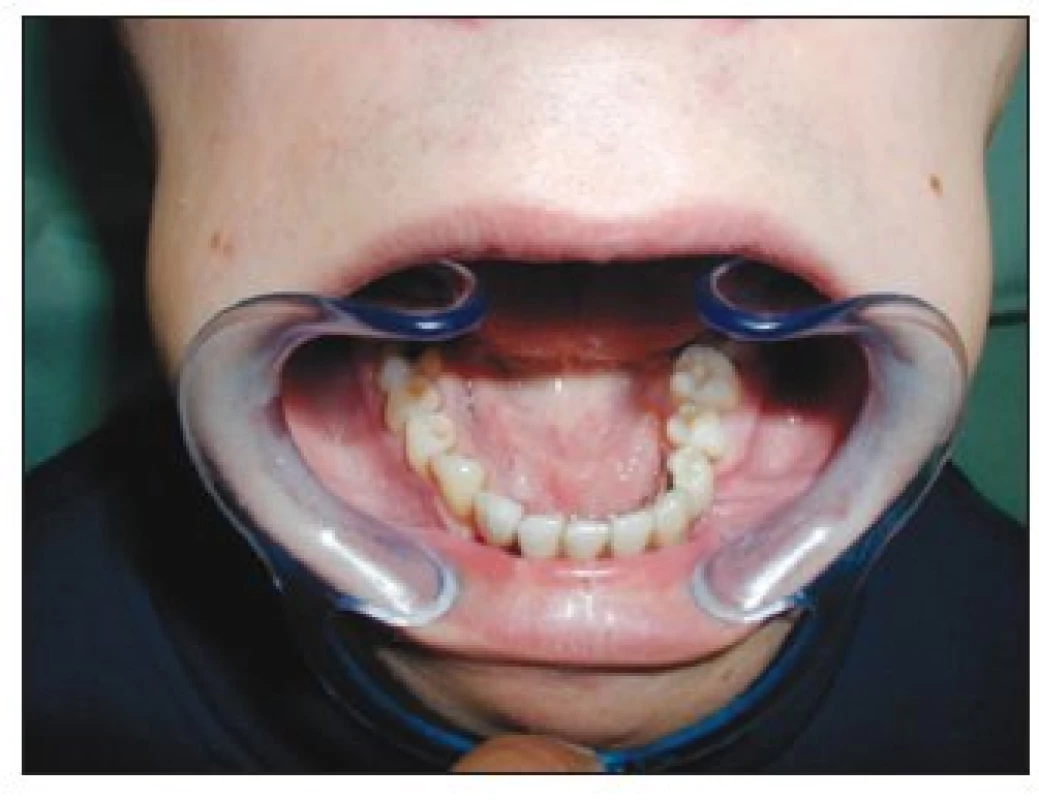
Three years after the operation (in 1997), the recurrence was seen on the physical examination. X-ray image confirmed the clinical findings (Fig. 2). The new surgical intervention was planed and the new GCG was removed. The similar histological conclusions were observed.
Obr. 2. A 12-year old boy – new surgical intervention 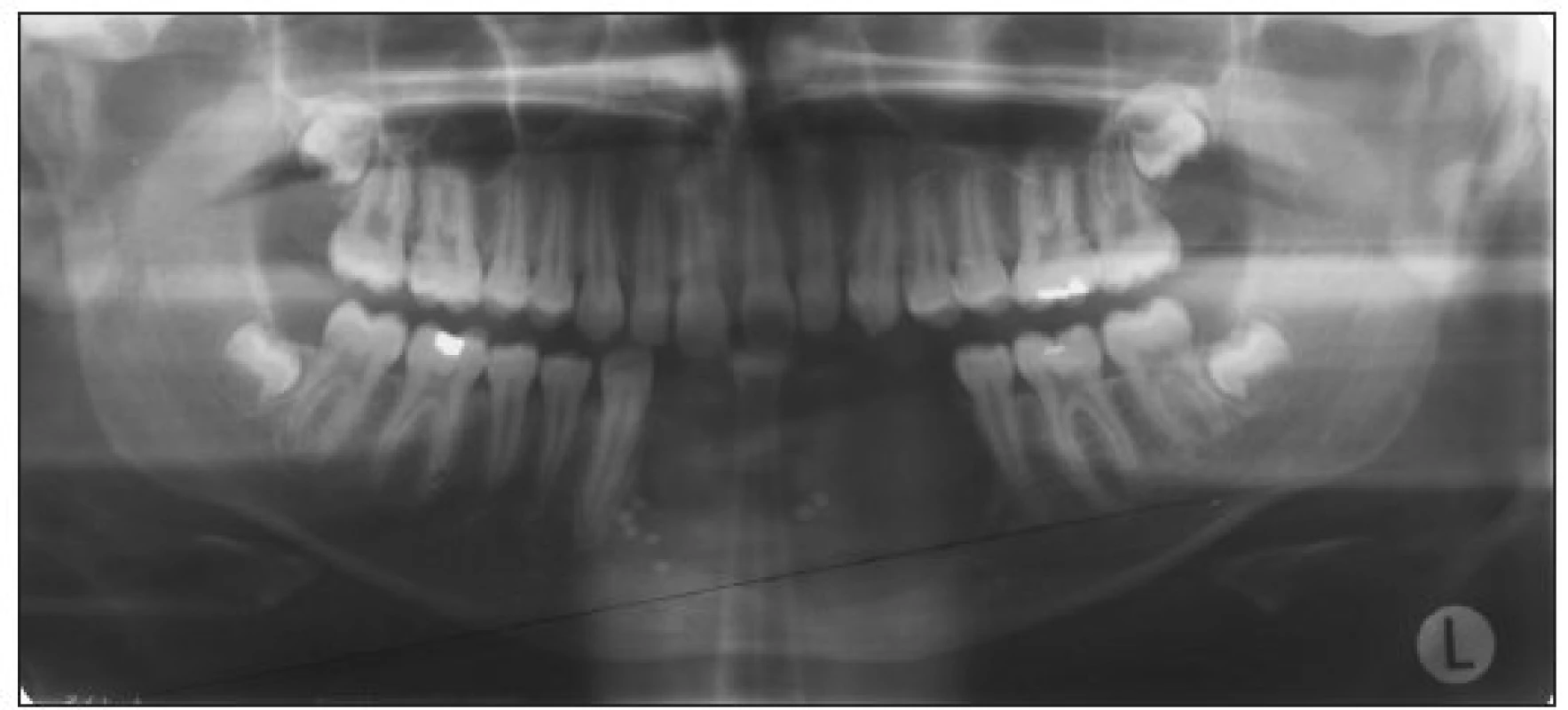
The prosthetic rehabilitation including implants insertion started in 2003, when the patient was an 18-year-old adult. There were several reasons for difficulties during reconstruction and functioning of the dental replacements: A discrepancy in the interrelationship between the jaw bones especially due to lower jaw frontal area defect. The deformation and flat embossment of mandible augmented by resilience of the thickened mucous membrane and atypical tentacles of mucosal folds was used for the closure of previous defect. To rebuild bone height, shape and size, the vertical distractor (TRACK 1.5 mm Distractor, Martin) (Fig. 3) was used for 2 months. We received 10 mm new bone increase (Fig. 4).
Obr. 4. Two-month bone rebuilding – 10 mm new bone increase 
Then, three implants had to be inserted into an edentulous jaw (STIO-Bio Impladent, Lasak (length 18 mm, average 3.7 mm). As soon as they were integrated (6 months), a surgeon performed the X-ray examination (panoramic radiograph) and checked the grade of osseointegration (Fig. 5). Until this time the implants fixtures were still covered by mucosa. After the healing process, the surgeon cut through the mucosal cover (incision was made along the alveolar ridge) and suitable healing caps were attached. After the forming of attached gingiva a dentist unscrewed the healing caps and attached the impression posts with the special spines. The mandible ridge was impressed using the polyether impression material. A reconstruction of the jaws relations (wax bite rim) was part of this visit as well.
Obr. 5. Three implants (STI-BIO Impladent Lasak) 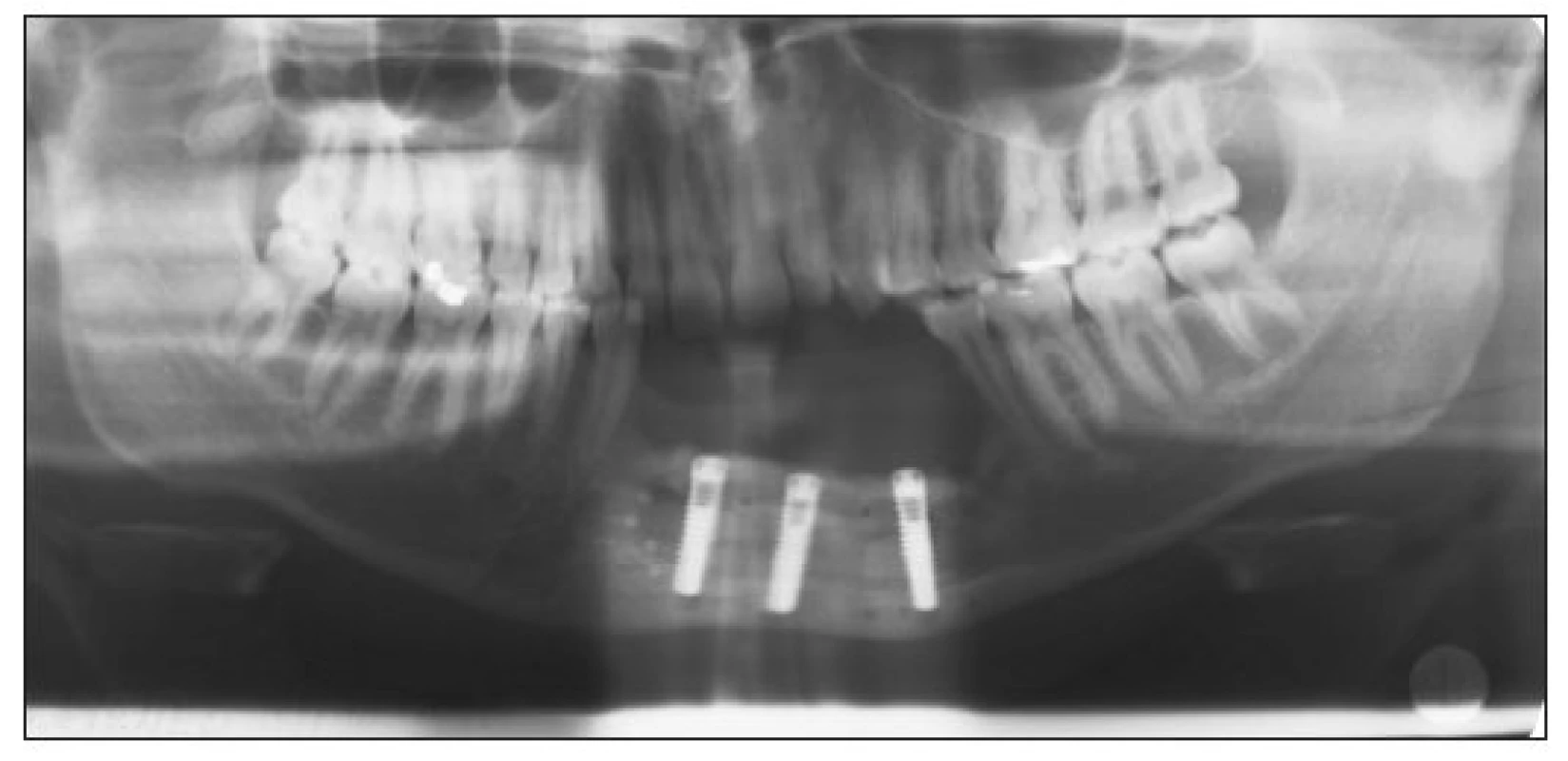
The dental technician filled the impression using the silicone gingival material and then created the master model using the plaster type IV (stone), consequently sealed the working models with the reconstructed inter-jaw position into the articulator. He attached the combustible impression copings on the laboratory analogues and finished modeling the re-shape of the future construction. A titanium alloy (Grade 2) and Cresco method reconstruction (Cresco Titan, Prague) was in our case prepared according to the instructions of the manufacturer (Fig. 6) (8).
Obr. 6. Plaster cast including gingival mask with fixed bridge 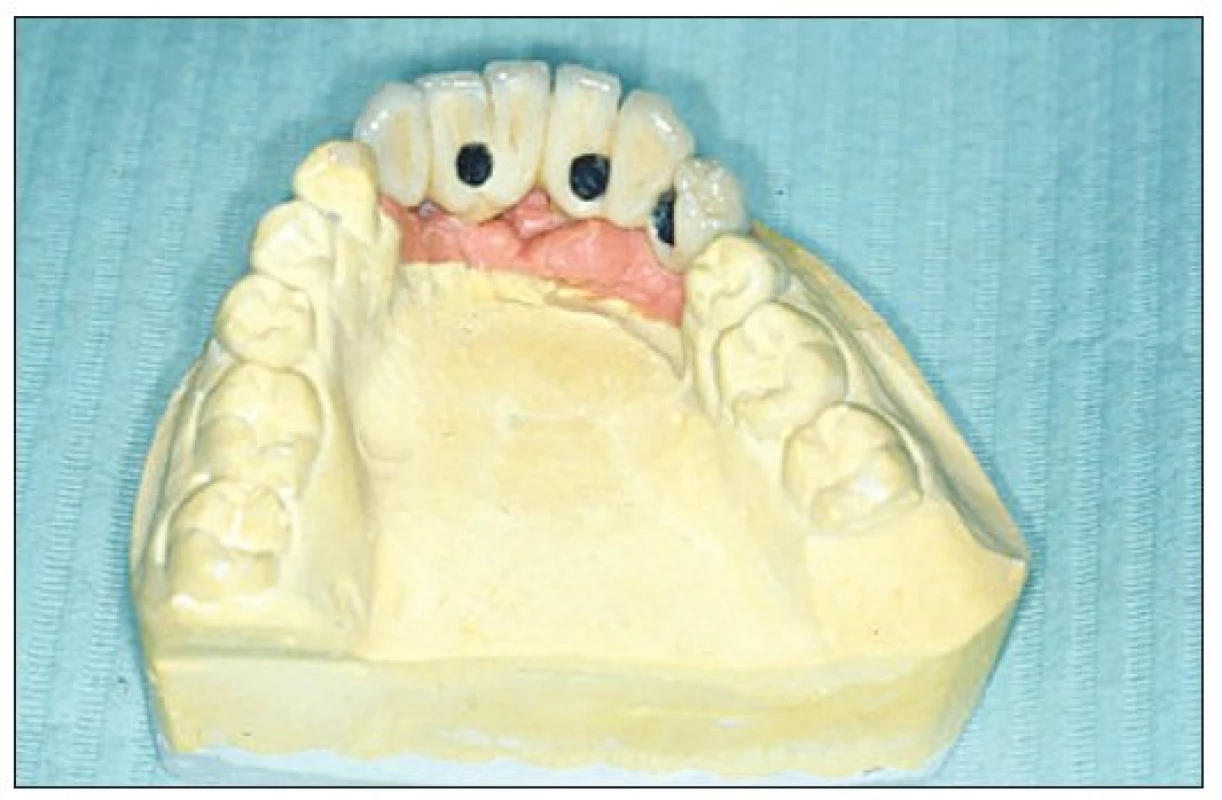
The technician had to continually view the free track of the screws of the future potentially removable framework. Because the jaw bone was cicatrized and contained defects it was suitable to augmentate not only hard but also soft tissues. As for the adjustment of the vertical maxillary relation, the construction is often sectional with the addition of pink ceramics simulating marginal gingiva (Fig. 7). After check-out of the metal framework, the bridge was completed using the ceramic material (Triceram, Dentaurum). The final evaluation was done to see whether it fulfills the functional and aesthetic requirements (Fig. 8). During the following few weeks (adaptation phase) the screw holes were closed using cotton pellet over the screw heads and glassionomer cement. The connection of the construction and implants should always be checked using an X-ray image (Fig. 9, 10).
Obr. 7. Cresco titan reconstruction: titanium framework grade 2 + Triceram ceramics 
Obr. 10. Panoramic radiograph after reconstruction 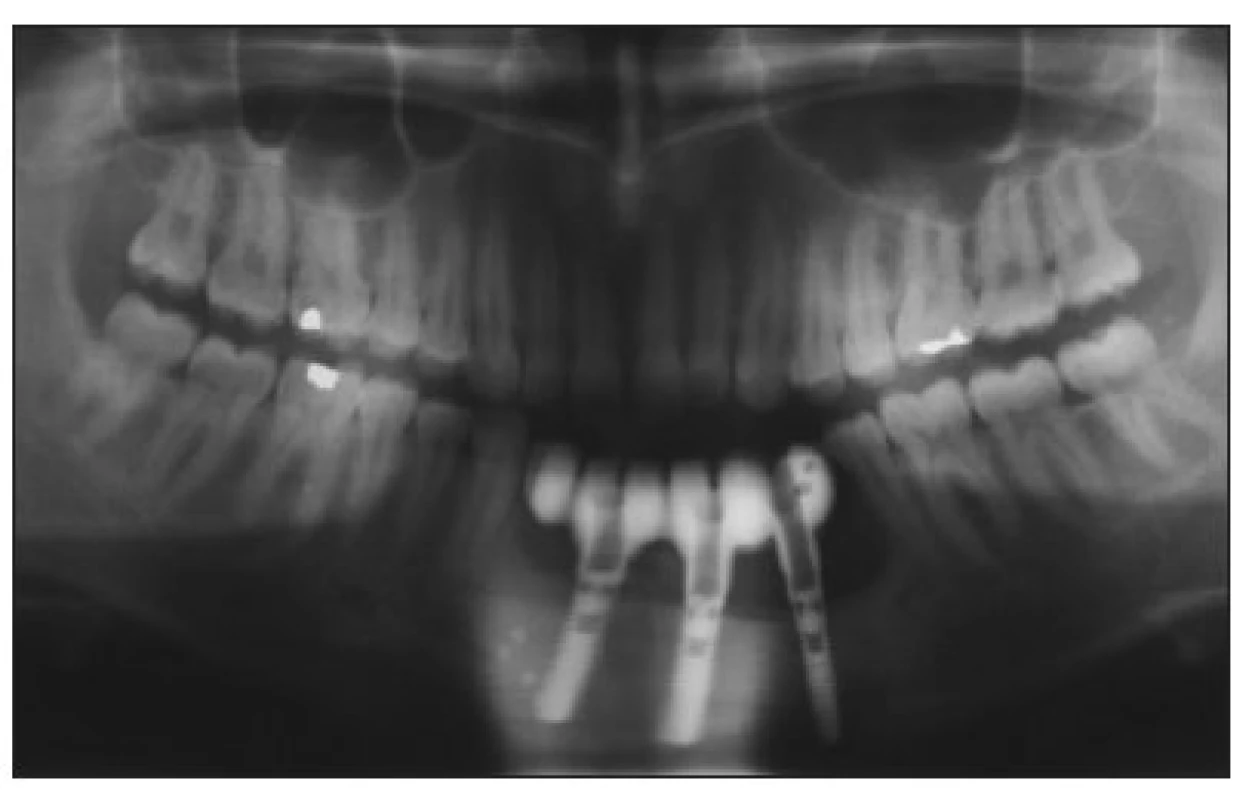
Three years recall (in 2007) shows a small 1 mm dehiscence surrounding implant 41. The functional and aesthetic result was stable and patient was satisfied. (Fig. 11–13.)
Obr. 12. A 3-year recall – detail of implant 41 – 1 mm dehiscence 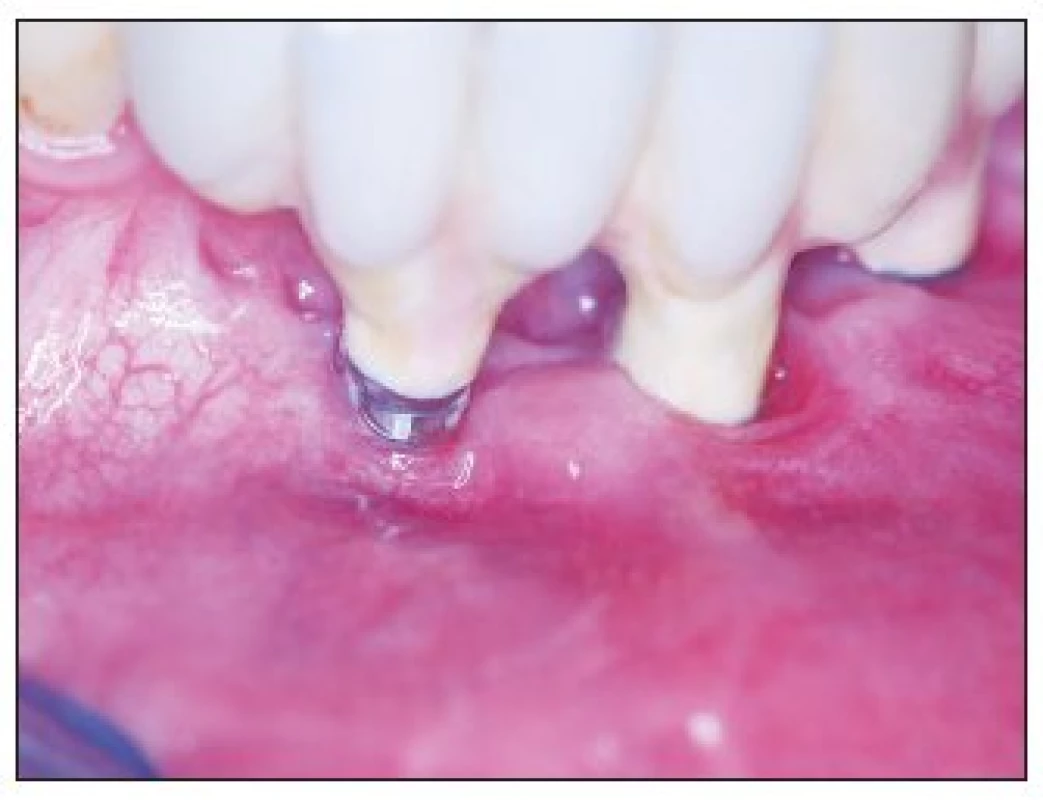
Obr. 13. Status three years after reconstruction 
DISCUSSION
Treatment and complete resolution of CGCG by surgical excision is strongly supported by many authors (1, 19, 23). The extent of surgery is related to the size and position of the lesion, ranging from simple excision and curettage to en bloc resection and reconstruction (6). Aggressive giant cell lesions have also been treated with other methods such as radiation, systemic application of calcitonin, intralesional injections of corticosteroids, and subcutaneous α-interferon injections and laser therapy, including carbon dioxide laser (6).Rebuilding of soft and hard tissues is not simple and contains several steps – bone reconstruction including tissue augmentation, implants insertion and prosthodontic rehabilitation might be possible. We confirmed that implants insertion is possible.
CONCLUSION
This contribution reviews the rationale and principles of CGCG lower jaw treatment. Prosthetic reconstruction including bone distraction and implants insertion needs individual approach to the patient’s rehabilitation. Esthetical and functional therapy is of fundamental importance in the patient’s rehabilitation, which affects the patient’s life (aesthetics, speech, food intake etc.).
ACKNOWLEDGMENTS
This research has been supported by Faculty Hospital Motol Research project No. 64203 VZ 00064203.
Address for correspondence:
Prof. Tatjana Dostálová, M.D., D.Sc., MBA
Department of Paediatric Stomatology
2nd Medical School of the Charles University and the Faculty Hospital Motol
V Úvalu 84
150 06 Prague 5
Czech Republic
E-mail: tatjana.dostalova@fnmotol.cz
Zdroje
1. Bataineh AB., Al Khateeb T., Rawashdeh MA. The surgical treatment of central giant cell granuloma of the mandible. J. Oral Maxillofac. Surg., 60, 2002, p. 756–761.
2. Buresh CJ., Seemayer TA., Nelson M., Neff JR., Dorfman HD., Bridge J. t(X;4)(q22;q31.3) in giant cell reparative granuloma. Cancer Genet. Cytogenet., 115, 1999, p. 80–81.
3. Cohen MA., Hertzanu Y. Radiologic features, including those seen with computed tomography, of central giant cell granuloma of the jaws. Oral Surg. Oral Med. Oral Pathol., 65, 1988, p. 255–261.
4. De Lange J., Van den Akker HP., Klip H. Incidence and disease-free survival after surgical therapy of central giant-cell granulomas of the jaw in The Netherlands: 1990–1995. Head Neck, 26, 2004, p. 792–795.
5. De Lange J., Van den Akker HP., Van den Berg H. Central giant cell granuloma of the jaw: A review of the literature with emphasis on therapy options. 2007 in press, online 20 August 2007.
6. De Lange J., Van den Akker HP., Veldhuijzen van Zanten GO., Engelshove HA., Van den Berg H., Klip H. Calcitonin therapy in central giant cell granuloma of the jaw: A randomized double-blind placebo-controlled study. Int. J. Oral Maxillofac. Surg., 35, 2006, p. 791–795.
7. De Souza PEA., Paim JFO., Carvalhais JN., Gomez RS. Immunohistochemical expression of p53, MDM2, Ki-67, and PCNA in central giant cell granuloma and giant cell tumor. J. Oral Pathol. Med., 28, 1999, p. 54–58.
8. Dostálová T., Kudrnová D., Bartoňová M.. Chlubna T., Hubálková H. Podmíněně snímatelná náhrada: I. Litá precizovaná konstrukce. Progresdent, 4, 2005, p. 52–57.
9. Evdokiou A., Atkins GJ., Bouralexis S., Hay S., Raggatt LJ., Cowled PA. et al. Expression of alternatively-spliced MDM2 transcripts in giant cell tumors of bone. Int. J Oncol., 19, 2001, p. 625–632.
10. Farrier SL., Farrier JN., Smart MK., Nash ES. A 10-year review of the occurrence and treatment of central giant cell granulomas in a District General Hospital. J. Oral Pathol. Med., 35, 2006, p. 332–337.
11. Chaparro-Avendano AV., Berini-Aytes L., Gay-Escoda C. Peripheral giant cell granuloma: A report of five cases and review of the literature. Med. Oral Pathol. Oral Cir. Bucal, 10, 2005, p. 53–57.
12. Chuong R., Kaban LB., Kozakewich H., Perez-Atayde A. Central giant cell lesions of the jaws: A clinicopathologic study. J. Oral Maxillofac. Surg., 44, 1986, p. 708–713.
13. Jaffe HL. Giant cell reparative granuloma, traumatic bone cyst and fibrous (fibro-osseous) dysplasia of jaw bones. Oral Surg., 6, 1953, p. 159–175.
14. Kramer IRH., Pindborg JJ., Shear M. Histological typing of odontogenic tumours (2nd ed.), Berlin: Springer-Verlag, 1991, p. 31.
15. Kremer C., Millesi W., Watzke M. Local injections of cortico-steroids for central giant cell granuloma. Int. J Oral Maxillofac. Surg., 23, 1994, p. 366–368.
16. Moss S., Domingo J., Stratton D., Wilk RM. Slowly expanding palatal mass. J. Oral Maxillofac. Surg., 59, 2001, p. 655–659.
17. Regezi JA., Sciubba JJ. Oral Pathology. St. Louis: Saunders, 2003, p. 116–117, 298–301.
18. Sidhu MS., Parkash H., Sidhu SS. Central giant cell granuloma of the jaws – review of 19 cases. Br. J. Oral Maxillofac. Surg., 33, 1995, p. 43–46.
19. Sidhu MS., Parkash H., Sidhu SS. Central giant cell granulomas of jaws: Review of 19 cases. Br. J. Oral Maxillofac. Surg., 35, 1995, p. 33–43.
20. Terry BC., Jacoway JR. Management of central giant cell lesions: An alternative to surgical therapy. Oral Maxillofac. Surg. Clin. N. Am., 6, 1994, p. 579–601.
21. Urade M., Furusawa K., Watatani K., Matsuya T. Mandibular giant cell granuloma. Oral Surg. Oral Med. Oral Pathol., 66, 1988, p. 121–122.
22. Vered M., Buchner A., Dayan V. Immunohistochemical expression of glucocorticoid and calcitonin receptors as a tool for selecting therapeutic approach in central giant cell granuloma of the jaw bones. Int. J. Oral Maxillofac. Surg., 35, 2006, p. 756–760.
23. Webb DJ., Brockbank J. Combined curettage and cryo surgical treatment for aggressive “giant cell lesion” of the mandible. Int. J. Oral Maxillofac. Surg., 5, 1986, p. 780.
24. Whitaker SB., Waldron CA. Central giant cell lesions of the jaws. A clinical, radiologic, and histopathologic study. Oral Surg. Oral Med. Oral Pathol., 75, 1993, p. 199–208.
Štítky
Chirurgie plastická Ortopedie Popáleninová medicína Traumatologie
Článek vyšel v časopiseActa chirurgiae plasticae
Nejčtenější tento týden
2008 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Léčba akutní pooperační bolesti z pohledu ortopeda
-
Všechny články tohoto čísla
- ARTERIALIZED VENOUS FREE FLAPS – A RECONSTRUCTIVE ALTERNATIVE FOR LARGE DORSAL DIGITAL DEFECTS
- RECONSTRUCTION OF LARGE UPPER LIP DEFECTS BY FREE TISSUE TRANSFER
- THE VALUE OF CLINICAL DIAGNOSIS OF DIGITAL GLOMUS TUMORS
- GIANT CELL REPARATIVE GRANULOMA IN THE MANDIBLE – CASE REPORT AND REVIEW OF THE LITERATURE
- IPSILATERAL FIBULAR TRANSFER: A VALUABLE OPTION FOR TREATMENT OF LARGE TIBIAL DEFECTS IN CHILDREN
- ČESKÉ A SLOVENSKÉ SOUHRNY
- Acta chirurgiae plasticae
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- ARTERIALIZED VENOUS FREE FLAPS – A RECONSTRUCTIVE ALTERNATIVE FOR LARGE DORSAL DIGITAL DEFECTS
- GIANT CELL REPARATIVE GRANULOMA IN THE MANDIBLE – CASE REPORT AND REVIEW OF THE LITERATURE
- THE VALUE OF CLINICAL DIAGNOSIS OF DIGITAL GLOMUS TUMORS
- RECONSTRUCTION OF LARGE UPPER LIP DEFECTS BY FREE TISSUE TRANSFER
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání