-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Catheter-Related Infections in Burn Patients at the Burn Centre of the University Hospital in Ostrava
Autoři: J. Tymonová 1; M. Adámková 1; V. Toršová 2; M. Kadlčík 1; J. Jackanin 1; Z. Crkvenjaš 1
Působiště autorů: Burn Centre of the University in Ostrava, and 1; Hygienic Institute in Ostrava, Czech Republic 2
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 50, 1, 2008, pp. 23-26
Introduction
While we are aware of risks related to central venous catheterization, we cannot avoid using CVCs (central venous catheters) in critically ill patients with severe burns. CVCs are commonly used for the administration of fluids, medications, blood products and parenteral nutrition and to monitor hemodynamic status, and also to facilitate patient positioning. Central venous catheterization may cause different early or late complications, which depend on the physician’s erudition, the quality of the catheters and quality of ICU nursing care for insertion sites (6, 8, 10, 11).
Catheter-related sepsis (endogenous sepsis or catheter colonization during bacteraemia from other known infection source) is dangerous for immunodeficient burn patients (5, 7). We can consider the incidence of exogenous catheter sepsis as the hygiene criterion of ICU.
Materials and methods
Catheter-related sepsis was defined according to Maki’s criteria (7) - catheter tip colonization was the significant growth of a micro organism (>15 colony-forming units) from the catheter tip, 10x more than in blood culture obtained from a peripheral vein, no apparent source of bacteraemia except the catheter, and signs of systemic infection which end after catheter removal. The placement of catheters was performed in operating rooms or ICU boxes with laminar air-conditioning after dressing removal, skin disinfection and use of sterile drapes around the insertion site. The catheters were inserted by experienced physicians using sterile-barrier precautions: surgical antiseptic hand wash, sterile gown, gloves, mask and cap. The percutaneous entry sites were attended 3 times per day by the ICU nurse. First, insertion sites were disinfected with povidone-iodine, and then topical antimicrobial ointment (neomycin plv. ads.) was applied. The connecting lines were disinfected and coated by occlusive dressing to prevent infection from dressings covering burned areas.
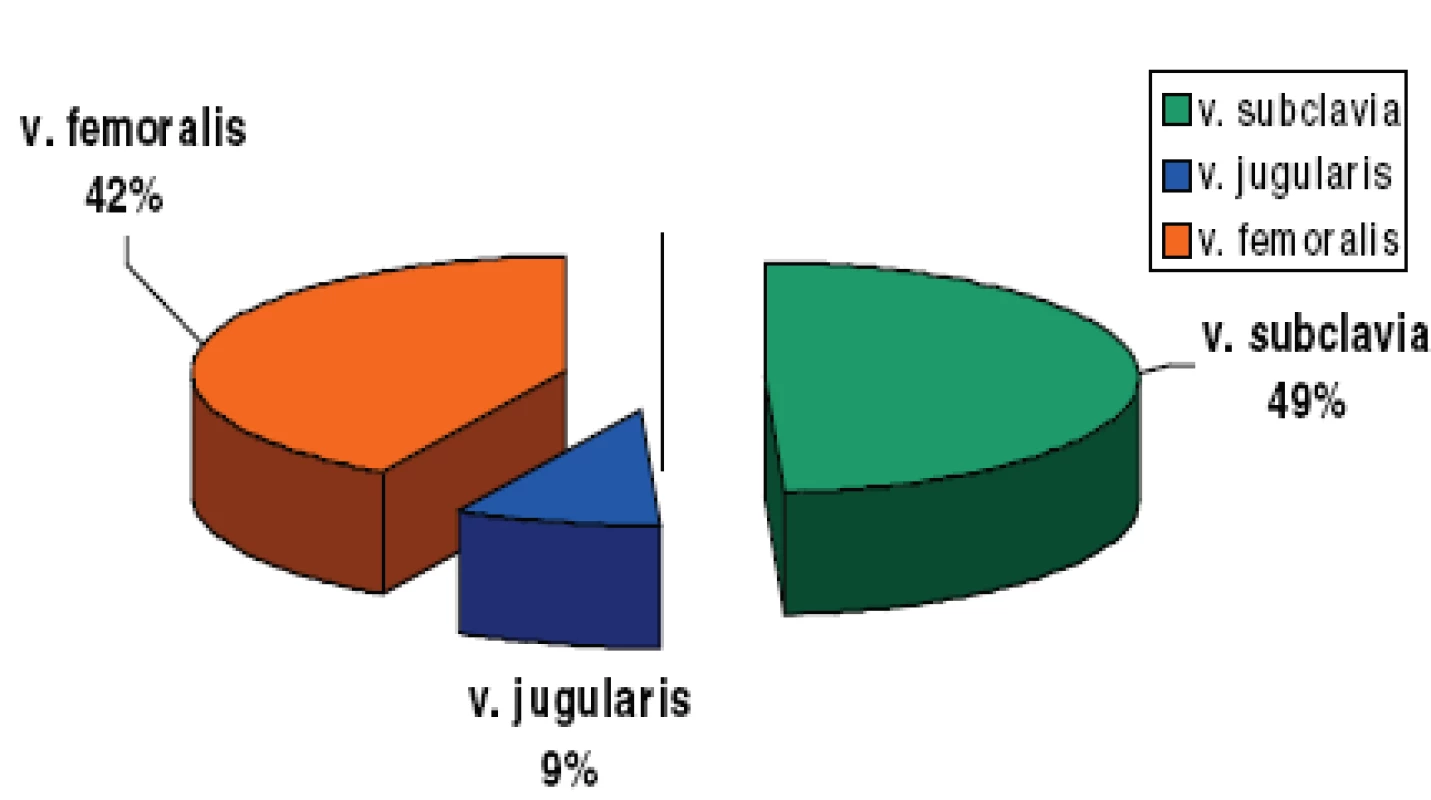
During the study period, 362 burn patients were admitted, of whom 114 had central venous catheter inserted (Fig. 1).
Obr. 1. Patients with CVCs in Burn Centre of Faculty Hospital in Ostrava 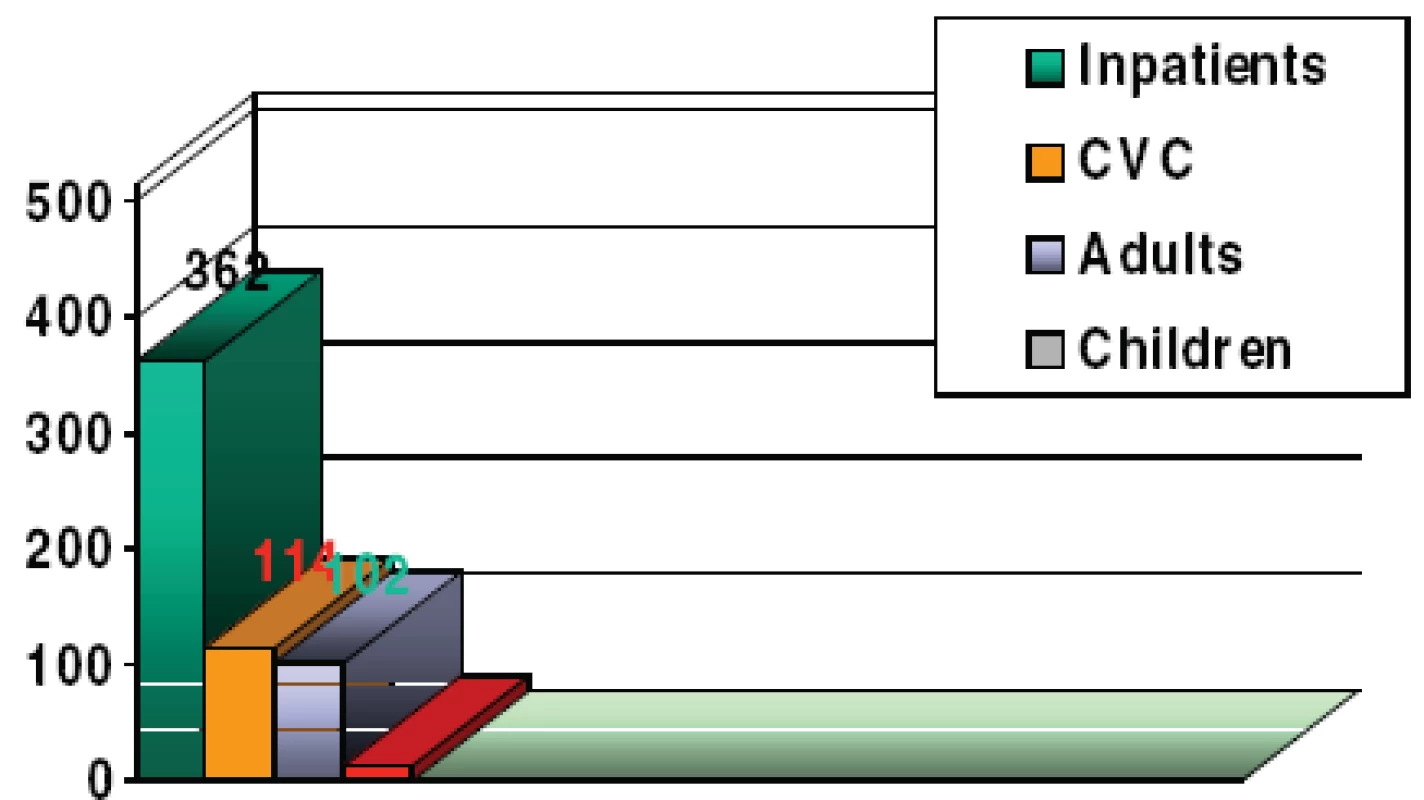
CVCs were inserted in 114 patients (mostly adults) out of 272. The number of CVCs/days of catheterization duration were for adult burn patients 2.8/10, for pediatric burn patients 1.75/9.25. The average length of catheterization was 24.2 days. The average insertion length of the catheter was 10.2 days (Fig. 2).
Obr. 2. Clinical characteristics of burned patients with CVCs 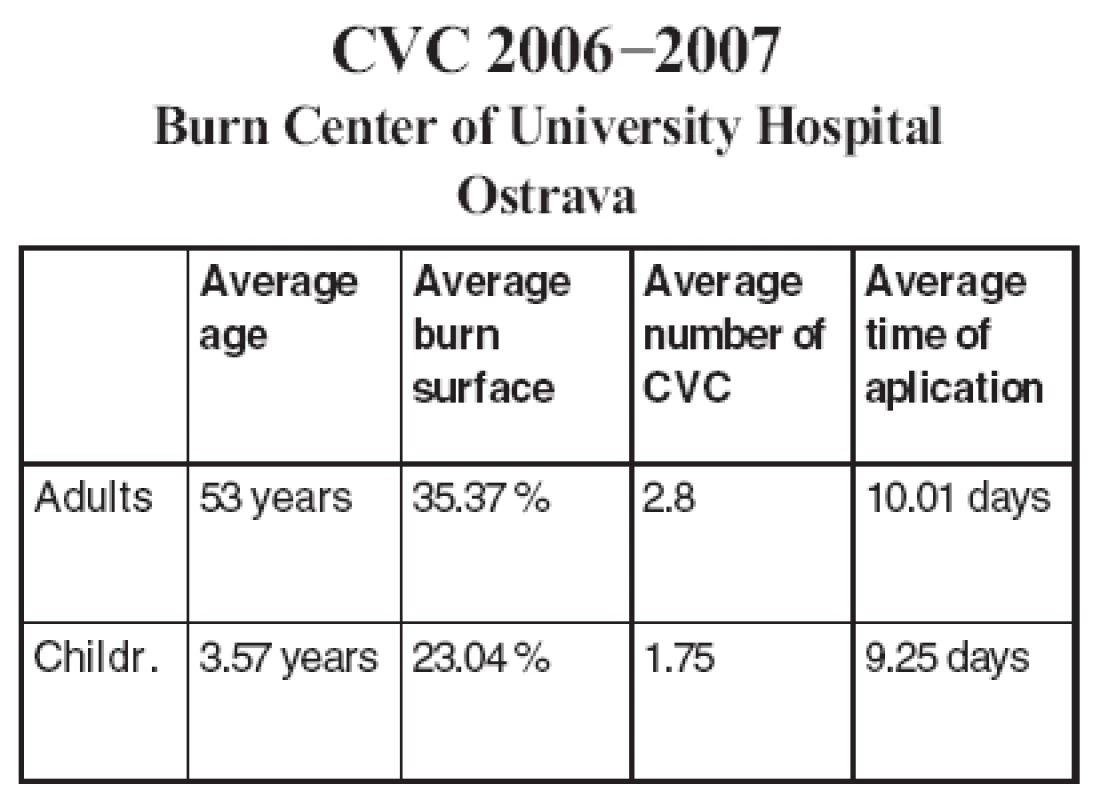
Near equal frequency of subclavian and femoral catheter insertion in this study group relates to a localization of burns and preferred short-term femoral insertions of dialysis catheters for lower risk of technical complications (Fig. 3).
All catheter tips removed were routinely cultured. Eight out of 272 catheters were massively colonized and 37 were only contaminated. The rest of them (227) were sterile (Fig. 4).
Obr. 4. Rates of catheters with bacterial colonization and contaminat 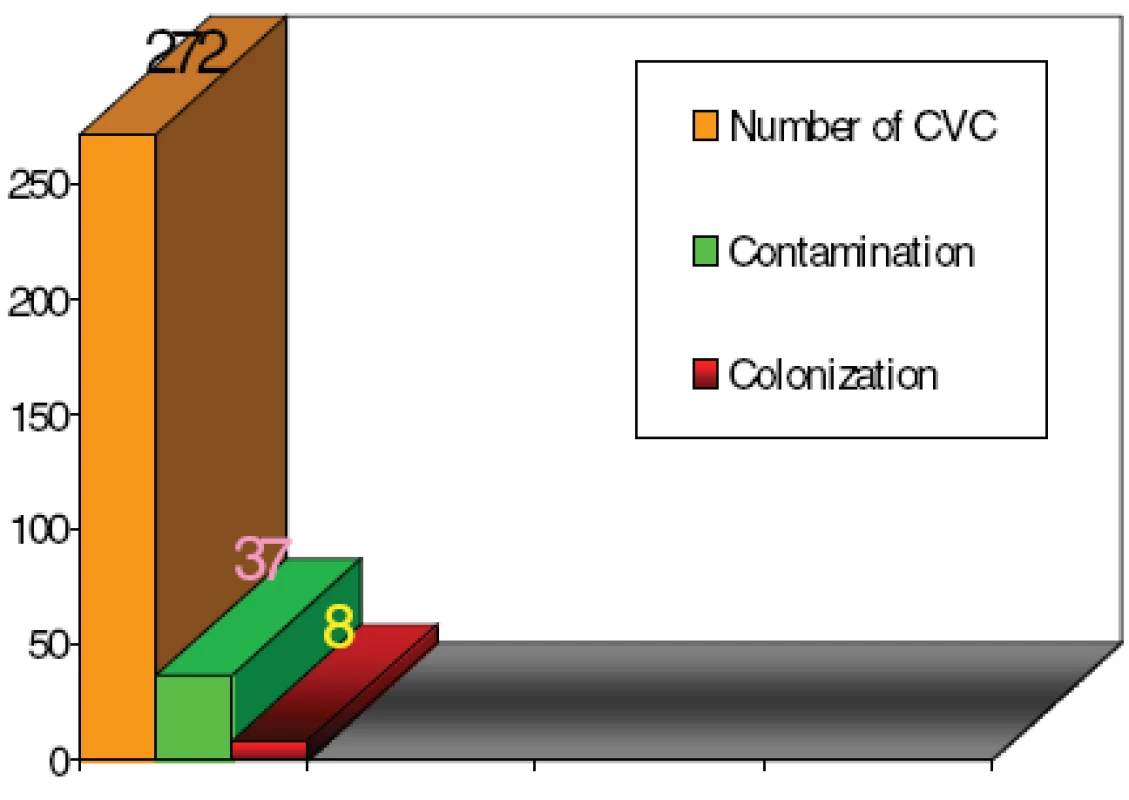
The most frequent infecting pathogens were coagulase-negative Staphylococci; less frequent was an Enterobacteriaceae species, while the other microorganisms occurred sporadically (Fig. 5).
Obr. 5. Bacterial findings from catheter tips (45x) 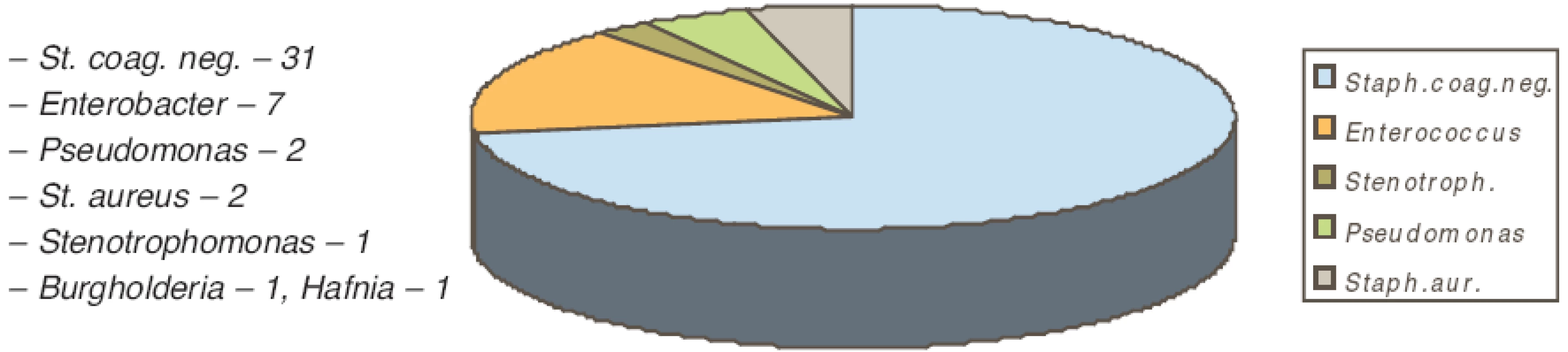
In massively colonized catheters we found positive endogenous bacterial colonization and in 4 cases positive peripheral blood culture (Fig. 6).
Obr. 6. Bacterial findings in burn patients with catheter colonization 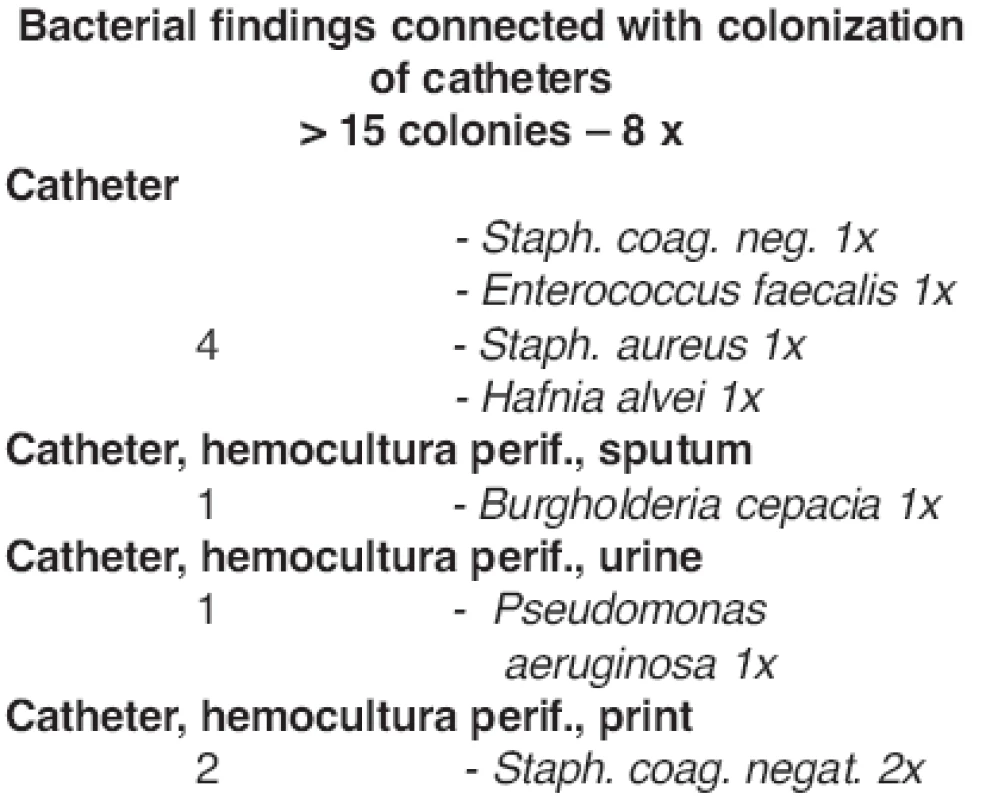
In contaminated catheters we found only positive endogenous bacterial colonization (Fig. 7).
Obr. 7. Bacterial findings in burn patients with catheter contamination 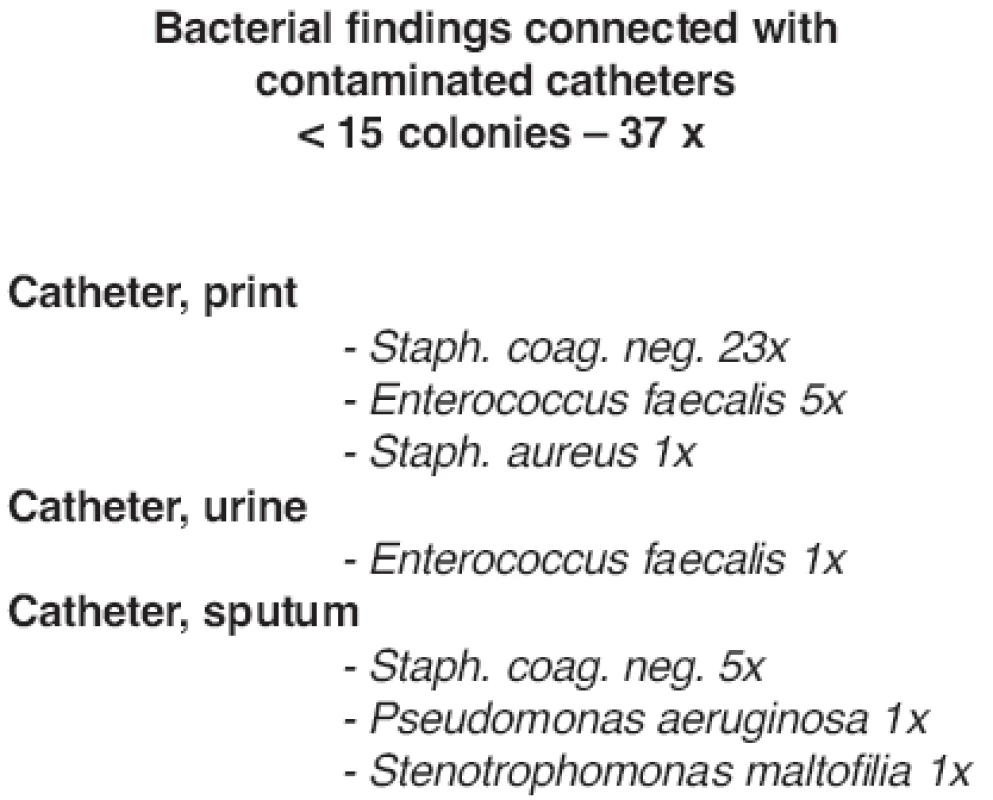
Results
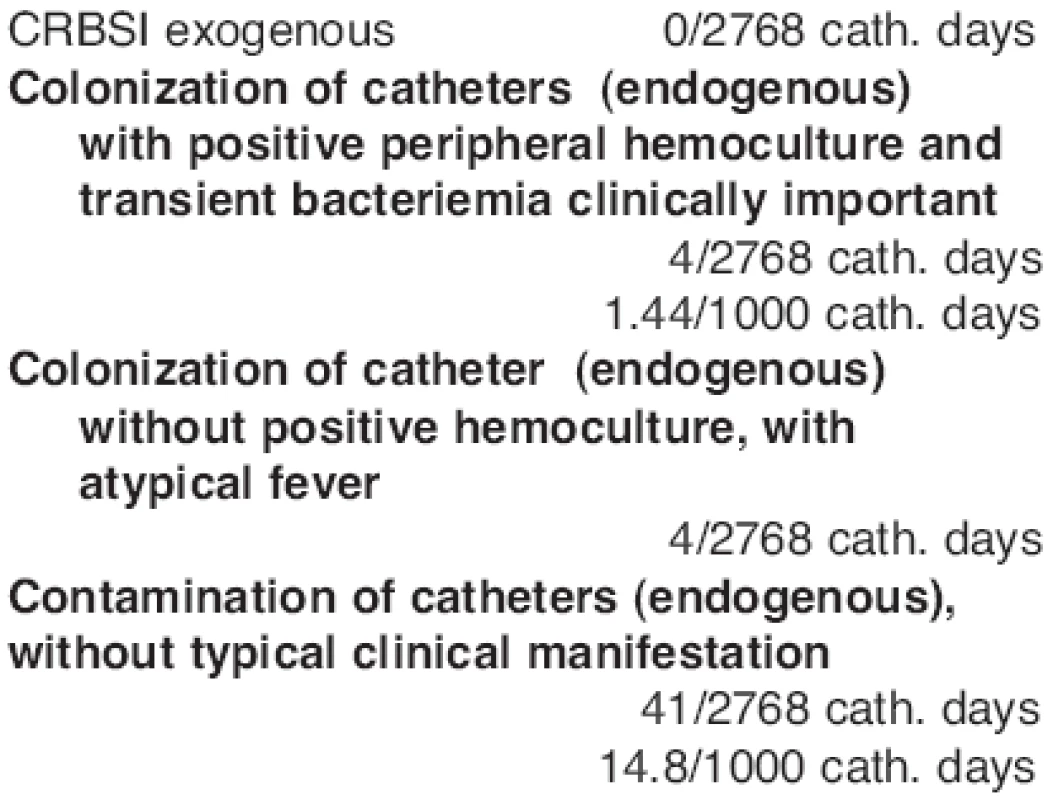
There was no exogenous catheter sepsis according to Maki’s criteria in our study group (Fig. 8).
Endogenous catheter colonization with positive peripheral blood culture and bacteraemia occurred in 4 cases, which means an incidence density of 1.44 infections/ 1000 catheter-days.
The other endogenous colonized or contaminated catheters were not associated with positive peripheral blood culture or with typical clinical manifestation.
Discussion
In burn patients it is necessary to consider general criteria of insertion-site choice (to prefer vena cava superior to inferior because of lower risk of thromboembolism and infection (4), jugular vein to subclavian in patients with tracheostomy; to consider clavicular fracture in anamnesis) but also to avoid the burn areas if possible (5). It is necessary for a physician to know more central venous access sites to avoid the catheter insertion in burn areas. It is recommended to change the insertion site every 3 days if the burned area is nearby. The insertion site for the new catheter was changed immediately in patients suspected of having a catheter-related infection (5). A number of materials have been used in catheter production since Aubaniac, who was the first to perform central venous catheterization in 1952. Catheters made from silicone, acrylate and polyurethane, antimicrobial-coated with chlorhexidine or sulphadiazine are used nowadays. Antimicrobial-coated catheters usage is evidently cheaper than treatment of sepsis, despite the fact that acquisition costs of these catheters are high (8). Triple-lumen catheters percutaneously inserted using the Seldinger technique are preferred in burn patients because they can be simultaneously used either for fluids and drug administration and hemodynamic monitoring. Catheter-related sepsis has been associated with high mortality rate, up to 28% (9). Regarding prevention of both infectious and occlusive complications, full sterile barrier precautions during CVC insertion and maintenance are recommended (10, 11). Also the use of multiple-lumen impregnated catheter avoiding the burn areas and CVCs replacement within the first signs of infection is needed. CVCs should be removed as soon as possible when they are no longer needed. Elective CVC replacement on aĘroutine basis is not recommended because of high risk of technical complications and minimal impact on catheter-related sepsis incidence (4). It is important to choose suitable diameter of catheter compared with the vessel size. Flushing of the CVC with an anticoagulant and not using it for blood sampling is also recommended (1). There is evidence of double risk of technical complications and early catheter-related sepsis if the physician performing the insertion procedure is not sufficiently experienced (10). A relatively large diameter of the inserted catheter, infected insertion site (13), no sterile maintenance (6, 10, 11) and relatively long indwelling time (2) were associated with higher incidence of catheter-related infection. The catheter-related local infection (CRLI) incidence was higher for femoral than for subclavian accesses. The incidence of arterial catheter-related infection is the lowest (3). In some studies there is no difference in catheter infection incidence between the catheters located in the upper or lower vena cava in burn patients (13). The incidence number of catheter-related sepsis was 1.55 per 1000 catheter-days in the ICUs in the EU countries and 0.33 per 1000 catheter-days in countries outside the EU. This discrepancy may be due to variable level of surveillance in different countries (12).
Conclusion
To prevent infectious complications connected with central venous catheterization in burn patients it is important that catheter insertion should be performed in operating rooms or ICU sterile boxes by experienced physicians using sterile-barrier precautions: surgical antiseptic hand wash, sterile gown, gloves, mask and cap. We recommend the use of triple-lumen catheters impregnated with chlorhexidine or silversulphadiazine. It is of great importance to attend to the percutaneous entry sites 3 times per day by using povidone-iodine and topical antimicrobial ointment (neomycin plv.ads.) and to have the connecting lines disinfected and covered by occlusive dressing.
Address for correspondence:
Jarmila Tymonová, M.D.
Burn Center
17. listopadu 1790
708 52 Ostrava
Czech Republic
E-mail: jarmila.tymonova@fnspo.cz
Zdroje
l. Zadák Z.,Výživa v intenzivní péči. Praha: Grada, 2002, p. 229-231.
2. Pawar, M., Mehta Y., Kapoor P., Sharma J., Gupta A., Trehan N., Central venous catheter-related blood stream infections. Incidence, risk factors, outcome and associated pathogens. J. Cardiothorac. Vasc. Anesth., 18, 2004, p. 304-308.
3. Lorente, L., Villegas J., Martin, MM., Jimenez A., Mora, ML. Catheter related infection in critically ill patients. Intensive Care Med., 30, 2004, p.-1681-1684.
4. Rickard, CM., Lipman J., Courtney, M., Siversen R., Daley P., Routine changing of intravenous administration sets does not reduce colonization or infection in central venous catheters. Infect. Control Hos. Epidemiol., 25, 2004, p. 650-655.
5. Königová R., Rozsáhlé popáleninové trauma. Praha: Avicenum, 1990, p. 172-185.
6. Warren DK., Zack JE., Mayfield JL., Chen A., Fraser VJ., Kollet MH. The effect of an education program on the incidence of central venous catheter associated bloodstream infection in a medical ICU. Crit. Care Medicine, 32, 2004, p. 2014-2020.
7. Maki DG., Weise CE., Safarin HW. A semiquantitative culture method for identifying intravenous-catheter-related infection. N. Engl. J. Med., 296, 1977, p. 1305-1309 .
8. Maki DG., Stolz SM., Wheeler S., Mermel LA. Prevention of central venous catheter-related bloodstream infection by use of antiseptic-impregnated catheter. Ann. Intern. Med., 127, 1997, p. 267-274.
9. Polderman KH et al. Central venous catheter use. Infections complications. Intensive Care Med., 28, 2002, p. 18-28.
10. Sheretz RJ., et al. Education of physician in training can decrease the risk for vascular catheter infection. Ann. Intern. Med., 132, 2000, p. 641-648.
11. Road II. et al. Prevention of central venous catheter-related infections by maximal sterile precautions during insertion. Infect. Control Hosp. Epidemiol., 15, 1994, p. 231-238.
12. Munoz P., Bouza E., San Juan R., Voss A., Pascau J., Desco, M. Clinical-epidemiological characteristics and outcome of patients with catheter - related bloodstream infections in Europe. Clin. Microbiol. Infect., 10, 2004, p. 843-845.
13. Still JM., Law E., Thiruvaiyaru D., Belcher K., Donker K. Central line-related sepsis in acute burn patients. Am. Surg., 64, 1998, p. 165-170.
Štítky
Chirurgie plastická Ortopedie Popáleninová medicína Traumatologie
Článek ČESKÉ A SLOVENSKÉ SOUHRNYČlánek HOW EAST DISCOVERED WEST
Článek vyšel v časopiseActa chirurgiae plasticae
Nejčtenější tento týden
2008 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Léčba akutní pooperační bolesti z pohledu ortopeda
-
Všechny články tohoto čísla
- MutilATing electrotrauma – case REPORT
- Award of the G. Whitaker International Burns Prize for 2007
- Specific aspects of the treatment of patients with multiple mechanical and burn injuries
- Catheter-Related Infections in Burn Patients at the Burn Centre of the University Hospital in Ostrava
- G. WHITAKER INTERNATIONAL BURNS PRIZE – PALERMO (Italy)
- Acinetobacter – serious danger FOR burn patients
- THE 25TH ANNIVERSARY OF BRNO BURN CENTRE: WHAT HAS CHANGED AND WHAT HAS NOT
- THE EFFECT OF NIFEDIPINE ON THE PATENCY OF MICROVASCULAR ANASTOMOSIS IN RATS
- Report of the 12th Congress of European Burns Association (EBA), Budapest, Hungary, September 12–15, 2007
- ČESKÉ A SLOVENSKÉ SOUHRNY
- HOW EAST DISCOVERED WEST
- Acta chirurgiae plasticae
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Specific aspects of the treatment of patients with multiple mechanical and burn injuries
- Acinetobacter – serious danger FOR burn patients
- THE EFFECT OF NIFEDIPINE ON THE PATENCY OF MICROVASCULAR ANASTOMOSIS IN RATS
- MutilATing electrotrauma – case REPORT
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání