-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Effects of the angiotensin receptor blocker Valsartan (Valsacor®) on arterial pressure, indices of myocardial diastolic function and global longitudinal strain in patients with uncontrolled arterial hypertension
The objective of this study was to evaluate the effects of Valsartan (Valsacor®) on arterial pressure (AP) and indices of myocardial diastolic and global function in patients with uncontrolled arterial hypertension (AH).
Material and methods:
60 patients (39 men and 21 women, mean age 63.9 ± 10.8 years, P > 140/90 mmHg with a background of combined antihypertensive therapy) were involved in the study. Valsartan (Valsacor®) was added to the standard therapy. The follow-up continued for three months, with clinical visits at initiation and completion of the study. The echocardiographic (EchoCG) evaluation included measurements of left ventricular and left atrial dimensions and function via longitudinal strain and Doppler-analysis of the transmitral blood flow.Results:
The administration of Valsartan (Valsacor®) resulted in a significant improvement in the antihypertensive control in the studied patients. The mean values of the baseline systolic blood (SBP) and diastolic blood (DBP) pressure in the studied group of patients were 174.9 ± 17.9 (range 150–230) mmHg and 97.5 ± 6.4 (range 85–110) mmHg, respectively. The mean SBP and DBP values at the end of the third month of the follow-up period were 139.1 ± 10.9 (range 120–180) mmHg and 84.9 ± 6.2 mmHg, respectively, at p < 0.05, compared to the baseline. The results of the echocardiographic analysis revealed significant differences in the dynamic performance of the indices: telesystolic dimension of the left ventricle, deceleration time (DT), E‘, E/E‘ ratio and values of longitudinal strain. The observed dynamic performance reflects favourable responses of the indices for diastolic function and longitudinal strain in the studied patients.Conclusion:
Valsartan (Valsacor®), used as an adjunct to the standard antihypertensive therapy in patients with insufficiently controlled AH, leads to optimisation of the AP values and improvement of the indices of diastolic and global myocardial function, with a very good safety profile.Keywords:
Valsartan – arterial hypertension – diastolic dysfunction –strain
Authors: K. Vitlyanova; Naidenov St.; N. Runev; E. Manov; R. Shabani; Y. Rangelov; K. Koshtikova; T. Donova
Authors place of work: Clinic of Cardiology, Clinic of Propedeutics of Internal Diseases “Prof. Dr. S. Kirkovich”, Department of Cardiology, Medical University Sofia
Published in the journal: Vnitř Lék 2013; 59(12): 1124-1129
Category: Aktualita
Summary
The objective of this study was to evaluate the effects of Valsartan (Valsacor®) on arterial pressure (AP) and indices of myocardial diastolic and global function in patients with uncontrolled arterial hypertension (AH).
Material and methods:
60 patients (39 men and 21 women, mean age 63.9 ± 10.8 years, P > 140/90 mmHg with a background of combined antihypertensive therapy) were involved in the study. Valsartan (Valsacor®) was added to the standard therapy. The follow-up continued for three months, with clinical visits at initiation and completion of the study. The echocardiographic (EchoCG) evaluation included measurements of left ventricular and left atrial dimensions and function via longitudinal strain and Doppler-analysis of the transmitral blood flow.Results:
The administration of Valsartan (Valsacor®) resulted in a significant improvement in the antihypertensive control in the studied patients. The mean values of the baseline systolic blood (SBP) and diastolic blood (DBP) pressure in the studied group of patients were 174.9 ± 17.9 (range 150–230) mmHg and 97.5 ± 6.4 (range 85–110) mmHg, respectively. The mean SBP and DBP values at the end of the third month of the follow-up period were 139.1 ± 10.9 (range 120–180) mmHg and 84.9 ± 6.2 mmHg, respectively, at p < 0.05, compared to the baseline. The results of the echocardiographic analysis revealed significant differences in the dynamic performance of the indices: telesystolic dimension of the left ventricle, deceleration time (DT), E‘, E/E‘ ratio and values of longitudinal strain. The observed dynamic performance reflects favourable responses of the indices for diastolic function and longitudinal strain in the studied patients.Conclusion:
Valsartan (Valsacor®), used as an adjunct to the standard antihypertensive therapy in patients with insufficiently controlled AH, leads to optimisation of the AP values and improvement of the indices of diastolic and global myocardial function, with a very good safety profile.Keywords:
Valsartan – arterial hypertension – diastolic dysfunction –strainIntroduction
Arterial hypertension (AH) is a leading cause of death and one of the most serious problems in the field of public health worldwide [1]. The incidence of the disease is high and increases sharply with age. There is an unfavourable upward trend in the incidence of arterial hypertension: the number of people affected by the disease in 2025 is expected to reach 1.5 billion people, accounting for one third of the world population. [2–4].
Patients with AH are subjected to control through a wide range of examinations involving non-invasive assessment of myocardial function for specifying the degree of morphological changes, further therapeutic behaviour, short-term and long-term clinical prognosis [5].
Tissue Doppler-echocardiography is a modern echocardiographic (EchoCG) method for assessing myocardial function. The method is suitable for evaluating the diastolic function in patients with uncontrolled arterial hypertension. This technique allows both visual and quantitative interpretation of the regional tissue velocity, the strain, as well as the displacement and acceleration of the whole cardiac cycle in one image. The term “echocardiographic strain” is used to describe the regional deformations occurring in the myocardium during the cardiac cycle (myocardial lengthening, shortening, thickening) [7,10]. The high temporal and velocity resolution of this methodology allows assessment of the rapid movements during the systolic and diastolic isovolumic period. The analysis of isovolumic velocity and acceleration characteristics in assessing the global systolic and diastolic changes allows the examination of elastic and contractile properties of the myocardium. Tissue motion imaging, developed from the integral of the tissue velocity curve in the longitudinal axis, represents a temporal-spatial colour map of myocardial movement throughout the cardiac cycle [6].
Despite the large choice of antihypertensive medicines, a relatively small proportion of the patients with hypertension reaches the target levels of arterial pressure (AP). Current guidelines define angiotensin receptor blockers (ARBs) as a suitable alternative for the long-term treatment of arterial hypertension (AH), used either as monotherapy (first-choice agents) or as a part of combined therapy. [7].
The objective of this study was to evaluate the effects of Valsartan (Valsacor®) on arterial pressure (AP) and myocardial diastolic function, assessed via TDI and longitudinal strain in patients with uncontrolled arterial hypertension (AH).
Material and methods
A total of 60 consecutive patients (39 female (65.0%) and 21 male (35.0%) patients, mean age 63.9 ± 10.8; range 33-85 years) with uncontrolled hypertension, defined as arterial blood pressure > 140/90 mmHg on antihypertensive treatment, were enrolled in the study. The mean age of the male and female patients was 57.9 ± 9.8 (range 33-76 years) and 66.6 ± 10.2 (range 34-85 years), respectively.
All patients underwent a detailed clinical examination and an interview, according to the standard protocol, to collect information on biological and demographic data, including age, gender, arterial pressure and symptoms related to the registered uncontrolled arterial hypertension. All information on the medical history and medications was documented. The major part of the interview consisted of questions on symptoms of heart failure, such as tiredness, dyspnoea, heart rate control, oppression and headache. The therapeutic regime for all patients was Valsartan 160 mg/day, added to the previously administered combined antihypertensive therapy with insufficient antihypertensive effect.
Instrumental investigation
Transthoracic echocardiography was performed, with the patient in the left lateral decubitus position, by using a 3.5 MHz transducer and Phillips HD IE 33 equipment. A standard M-mode was applied for obtaining left ventricular end-diastolic (LVEDD) and left ventricular end-systolic diameters (LVESD) and atrial dimensions. Standard two-dimentional images were examined offline. Left ventricular end-systolic volumes (LVESV) and left ventricular end-diastolic volumes (LVEDV), as well as the LVEF (%) were quantified by using manual planimetry of conventional two - and four-chamber views and Simpson’s technique. [13].
A pulsed wave Doppler (PWD) examination of the LV inflow was performed from the four-chamber view, with the sample volume placed between the mitral leaflet tips and the early (E) and late (A) diastolic peak velocities; the E deceleration time (DT) was measured and then the E/A ratio was derived. The echocardiographic images were recorded by using a commercially available system equipped with TDI, and Speckle Tracking. The longitudinal function was evaluated by using pulsed TDI at the mitral annulus, placing the sample volume in the basal segment of the inter-ventricular septum (IVS) from the apical four-chamber view: peak velocities in the systole, early diastolic motion (E’) and late (A – atrial contraction) diastole, both at the septal and lateral mitral annulus, were measured. Mean values of both septal and lateral measures were finally calculated and presented. LV longitudinal function was evaluated from raw data; systolic myocardial velocity (S) was also quantified [8].
The same experienced echocardiographer carried out all examinations of each individual. EchoCG assessment of the left ventricular function was performed at baseline and three months.
Statistical analysis
The data were summarised by frequencies and percentages for the categorical variables and by mean and standard deviations (SD) for the continuous variables. Comparisons were made by using the independent t-test and χ2-test, where appropriate. The results were considered statistically significant for p values ≤ 0.05. The statistical analysis was performed by applying the SPSS, version 13.0 (SPSS Inc, Chicago, IL) programme.
Results
The administration of Valsartan (Valsacor®) resulted in significant improvement of the antihypertensive control in the studied patients. The mean values of the baseline systolic arterial (SBP) and diastolic arterial (DBP) pressure in the studied group of patients were 174.9 ± 17.9 (range 150–230) mmHg and 97.5 ± 6.4 (range 85–110) mmHg, respectively. The mean SBP and DBP values at the end of the follow-up period were 139.1 ± 10.9 (range 120–180) mmHg and 84.9 ± 6.2 mmHg, respectively, at p < 0.05, compared to the baseline (Fig. 1).
Fig. 1. SBP and DBP values at the baseline and 3 months after initiation of the treatment, p < 0.05 
The inclusion of Valsartan (Valsacor®) to the ongoing antihypertensive therapy led also to improved control of the heart rate. Optimisation of arterial pressure and heart rate was observed in all patients, regardless of gender, at the end of the follow-up period (Tab. 1).
Tab. 1. SBP, DBP and HR values of the patients, included in the study 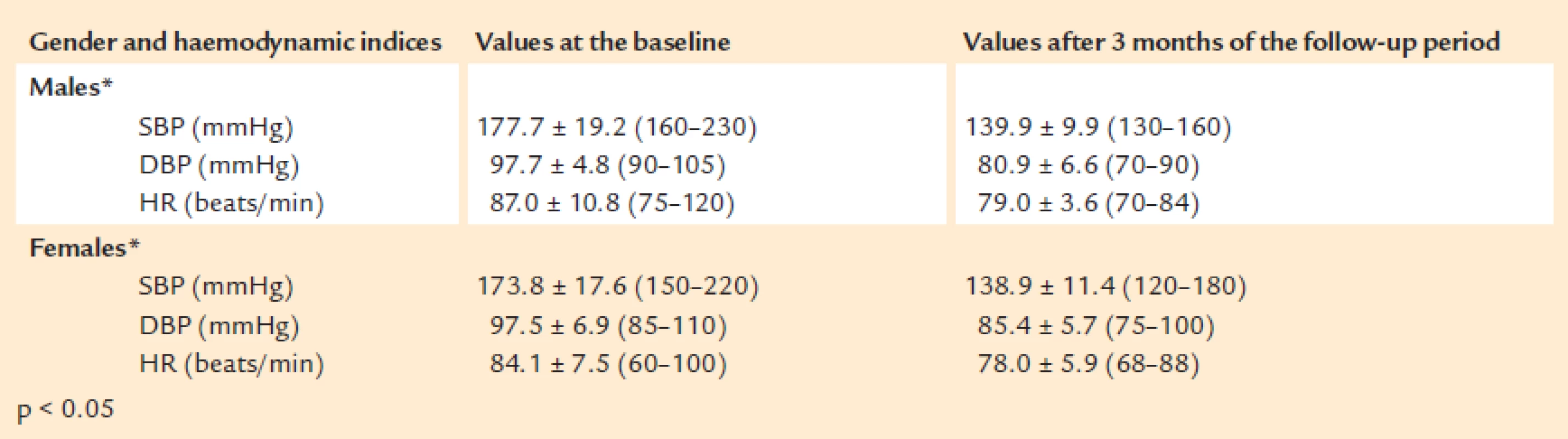
On month three of the follow-up period, control over AH (AP <140/90 mmHg) was achieved in a total of 25 patients (41.7%), eight males (38.1%) and 17 females (43.6%). The data of achieved control on AH by gender are presented on Fig. 2.
Fig. 2. Control on AH, achieved in male and female patients, p = N.S. 
Treatment with Valsartan (Valsacor®) resulted in a significant reduction of complaints, due to uncontrolled AH and to significant improvement of the quality of life of the studied patients (Fig. 3).
Fig. 3. AH-related complaints prior to initiation of the treatment with Valsacor<sup>®</sup> and after completion of the follow-up period (p<sub>males/females</sub>= N.S.) 
The data of the echocardiographic examinations, performed at initiation and completion of the follow-up period, are presented in Tab. 2 and on Fig. 4, 5, 6 and 7, and show the assessed dynamic performance of the echocardiographic indices DT, E’, E/E’ and the strain, with the background of the treatment, carried out after the addition of Valsartan (Valsacor®) to the therapy.
Tab. 2. Data of the echocardiographic examination at the baseline and after 3 months of the follow-up period, P<sub>males/females</sub>= N.S. 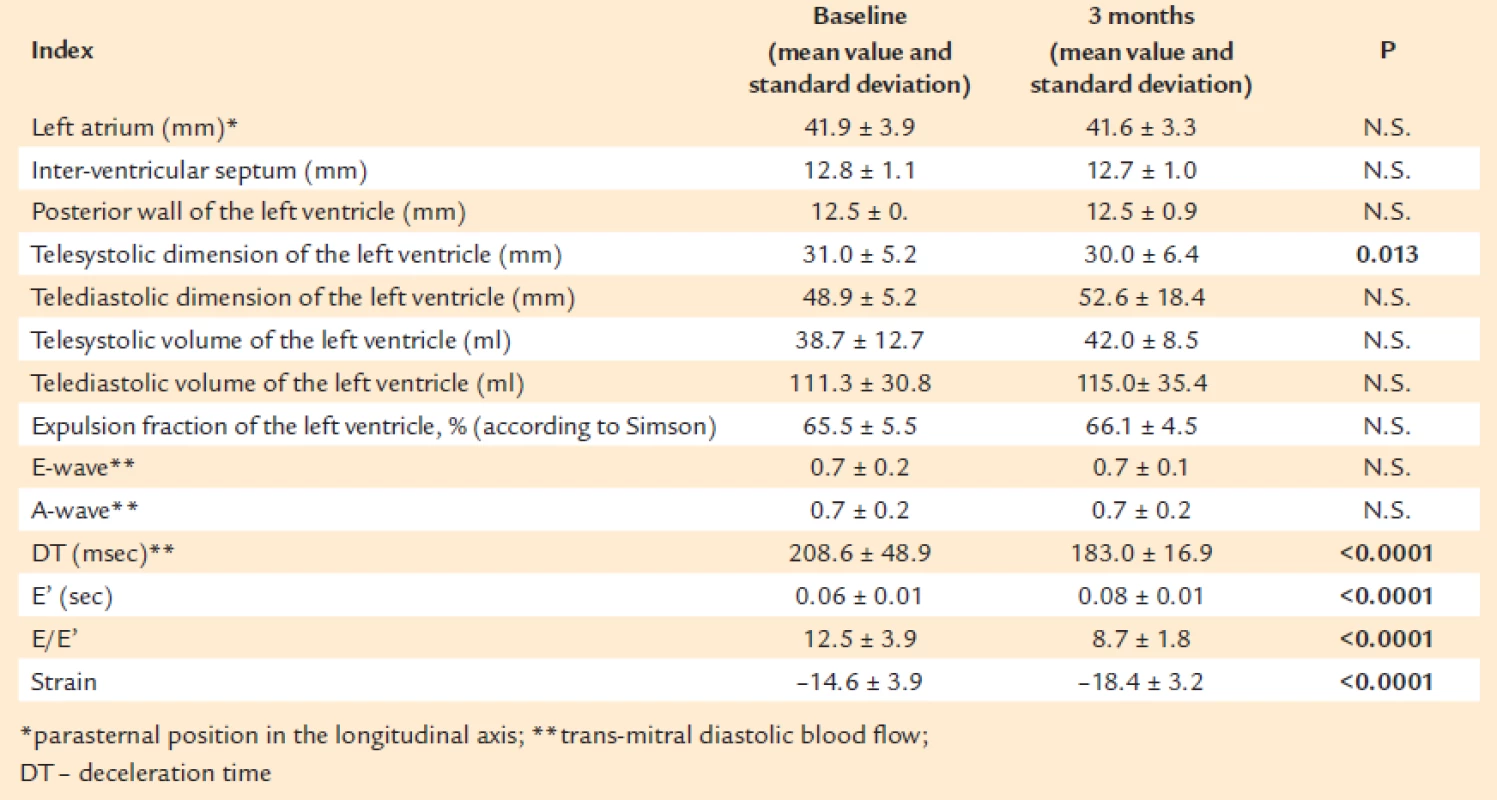
Fig. 4. Dynamic performance of the index DT, p < 0.0001 
Fig. 5. Dynamic performance of the index E’, p < 0.0001 
Fig. 6. Dynamic performance of the E/E’ ratio, p < 0.0001 
Fig. 7. Dynamic performance of the index strain, p < 0.0001 
The results of the echocardiographic analysis revealed significant differences in the dynamic performance, at the baseline and three months, of the indices: telesystolic dimension of the left ventricle, deceleration time (DT), E‘, E/E‘ ratio and values of longitudinal strain. The observed dynamic performance reflects favourable responses of the indices for diastolic function and longitudinal strain in the studied patients.
No undesirable effects, related with the administered medicine and requiring discontinuation of therapy, were registered.
Discussion
The results of our study reveal a significant antihypertensive effect of the investigational angiotensin receptor blocker Valsartan (Valsacor®), with significant improvement of the indices for myocardial diastolic and global function. The obtained results comply with the results of recent clinical studies demonstrating that monotherapy with ARB has resulted in satisfactory control of AP, observed in 63% of the patients. The hypotensive effect of ARBs, in accordance with the results of other studies, was similar in both sexes and equally effective in both younger and older age groups.
Angiotensin II exerts its effects by acting on two types of receptors, angiotensin I (AT1) and angiotensin II (AT2) receptors. The activation of AT2 receptors is the key to the protective effects of ARBs, whose main representative is the studied medicine Valsartan. APBs cause vasodilation, natriuresis, stimulation of tissue regeneration. ARBs displace angiotensin II from its specific AT1 receptor, thus antagonising its negative effects in terms of reduction in glomerular filtration rate, occurrence of proteinuria, albuminuria, glomerulosclerosis and aldosterone release, left ventricular hypertrophy, fibrosis. ARBs also participate in the processes of remodelling and apoptosis of myocytes, vasoconstriction, vascular hypertrophy, endothelial dysfunction and atherosclerosis. A dose-dependent decrease in the peripheral resistance with insignificant changes in the heart rate and cardiac output is achieved. In this regard, the observed improvement of the symptoms, determined by the baseline non-optimal antihypertensive control, is consistent with the known mechanisms of action and myocardial protective effects of ARBs, beyond the reduction of AP alone. On the other hand, the observed high baseline frequency of the studied symptoms is probably preconditioned by both uncontrolled arterial hypertension at the enrolment for the study and the aggravated indices for diastolic and global myocardial function in the studied patients, which was confirmed by the measured significant improvement of these indices at the third month.
The treatment of diastolic heart failure (DHF) remains empiric, since trial data are limited. The medicinal agent, selected by us for control of arterial pressure, is in compliance with the recommendations for treatment of patients with DHF, published in 2013 by the American College of Cardiology Foundation/American Heart Association in the guidelines on HF [9,10], including also strong recommendations for control of systolic and diastolic hypertension.
Angiotensin II receptor blockers (ARBs) may be beneficial in patients with left ventricular diastolic dysfunction due to hypertension, although the data on the impact are limited [11,12]. In various studies of hypertensive patients with left ventricle hypertrophy (LVH), ARBs caused more regression of LVH and improvement in LV diastolic filling than beta blockers [12,13].
Regression of LVH is an important therapeutic goal, since it may improve indices of diastolic function. A meta-analysis attempted to evaluate the relative efficacy of different antihypertensive drugs for their ability to reverse LVH in patients with hypertension. Eighty trials that included 146 and 17 active treatment and placebo arms, respectively, were evaluated. After statistical adjustments for the length of therapy and degree of blood pressure lowering, the relative reductions in left ventricular mass index were highest for the ARBs – 13 % in comparison to the other classes of medications [11].
In patients with cardiac hypertrophy of various etiologies, Sun et al demonstrated that the longitudinal strain showed the best correlation with LVEF and diastolic function indices. It was also demonstrated that the longitudinal global strain can predict cardiovascular events in patients with CHF and death due to different causes in individuals with heart disease. [14,15,16]. It should be taken into account, however, that there are still no standardised norms for GLS. Regardless of this, more important is the statistically significant trend towards improvement in myocardial function assessed echocardiographically via GLS with the background of added Valsartan (Valsacor®) to the ongoing therapy of the studied patients. The observed improvement of both the indices of diastolic function and GLS in the studied patients supports the hypothesis that the systole and diastole are closely related. Moreover, it has been shown that in patients with preserved LVEF, both systolic and diastolic myocardial mechanical parameters significantly correlate with the LV filling pressure. A possible explanation for the results is the assumption that patients with preserved LVEF have also significant abnormalities in systolic function, a finding that may challenge the concept of isolated diastolic dysfunction. [17].
In conclusion, Valsartan (Valsacor®), used as an adjunct to the standard antihypertensive therapy in patients with insufficiently controlled AH, leads to optimisation of the AP values and improvement of the indices of diastolic and global myocardial function, with a very good safety profile.
K. Vitliyanova, M.D.,
E-mail: k.vitlianova@abv.bg
Zdroje
1. Daskalov I. Terapia s angiotenzin receptorni blokeri. Medinfo, Sofia 2008; 9: godina VIII.
2. 2003 European Society of Hypertension / European Society of Cardiology Guidelines for the management of Arterial Hypertension. J. Hypertens 2003; 21 : 1011–1153.
3. 2003 Word Health Organisation / International Society of Hypertension. Statement Management of Hypertension. J.Hypertens 2003; 21 : 1983–1892.
4. World Health Report, 2002.
5. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.The National High Blood Pressure Education Program Coordinating Committee. Hypertension. 2003; 42 : 1206–1252.
6. Nagueh SF, Appleton C, Gillebert TC. Reccomendations for the evaluation of LV diastolic function by echocardiography; Eur J Echocardiogr 2009; 10 : 165–193
7. Catanzaro D., Frishman W. Angiotensin receptor blockers for management of hypertension. South Med J 2010; 103 : 669–673.
8. Ho CY, Solomon SD. A Clinician’s Guide to Tissue Doppler Imaging. Circulation 2006; 113: e396–e398.
9. Yancy CW, Jessup M, Bozkurt B et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013; 128 : 1810.
10. Hunt SA, Abraham WT, Chin MH et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009; 119:e391.
11. Wachtell K, Bella JN, Rokkedal J et al. Change in diastolic left ventricular filling after one year of antihypertensive treatment: The Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) Study. Circulation 2002; 105 : 1071–1076.
12. Dahlöf B, Devereux RB, Kjeldsen SE et al, LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 2002; 359 : 995–1003.
13. Klingbeil AU, Schneider M, Martus P et al. A meta-analysis of the effects of treatment on left ventricular mass in essential hypertension. Am J Med 2003; 115 : 41–46.
14. Sun JP, Stewart WJ, Yang XS et al. Differentiation of hypertrophic cardiomyopathy and cardiac amyloidosis from other causes of ventricular wall thickening by two-dimensional strain imaging echocardiography. Am J Cardiol 2009; 103 : 411–415.
15. Cho GY, Marwick TH, Kim HS et al. Global 2-dimensional strain as a new prognosticator in patients with heart failure. J Am Coll Cardiol 2009; 54 : 618–624.
16. Stanton T, Leano R, Marwick TH. Prediction of all-cause mortality from global longitudinal speckle strain: comparison with ejection fraction and wall motion scoring. Circ Cardiovasc Imaging 2009; 2 : 356–364.
17. Nguyen JS, Lakkis NM, Bobek J et al. Systolic and Diastolic Myocardial Mechanics in Patients with Cardiac Disease and Preserved Ejection Fraction: Impact of Left Ventricular Filling Pressure. J Am Soc Echocardiogr. 2013; 23 : 1273–1280.
Štítky
Diabetologie Endokrinologie Interní lékařství
Článek vyšel v časopiseVnitřní lékařství
Nejčtenější tento týden
2013 Číslo 12- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
-
Všechny články tohoto čísla
- Indikátory zánětu u pacientů s koronární aterosklerózou – editorial
- Komentář ke studii EDGE – editorial
- Pozice tiotropia v nových léčebných doporučeních pro chronickou obstrukční plicní nemoc – editorial
- Prospektivní, multicentrická, neintervenční studie na zhodnocení současné léčby pacientů s diabetes mellitus 2. typu, nedostatečně kompenzovaných monoterapií metforminem – KOMETA CZ
- Účinnost a bezpečnost vildagliptinu jako léku druhé volby ve srovnání s jinými perorálními antidiabetiky u pacientů s diabetes mellitus 2. typu: české výsledky v rámci celosvětové prospektivní kohortové studie EDGE
- Indikátory zápalu u pacientov s koronárnou aterosklerózou – úloha usCRP v diagnostike a predikcii prognózy ochorenia
- Současný pohled na onemocnění jater u srdečního selhání
- Pozice tiotropia v nových léčebných doporučeních pro chronickou obstrukční plicní nemoc
- Súčasnosť a budúcnosť farmako-artériotromboprofylaxie v klinickej praxi. Odporúčania Angiologickej sekcie Slovenskej lekárskej komory
- Doporučené postupy v léčbě starších pacientů s diabetes mellitus v ČR
- Doporučení KDIGO pro léčbu zvýšeného krevního tlaku u chronického onemocnění ledvin
- Zánětlivá borreliová dilatační kardiomyopatie
- Závažná rizika spojená s užíváním natrium-fosfátových projímadel
- Histiocytární sarkom
- Effects of the angiotensin receptor blocker Valsartan (Valsacor®) on arterial pressure, indices of myocardial diastolic function and global longitudinal strain in patients with uncontrolled arterial hypertension
- Mechanizmus pleiotropního účinku sulodexidu
- Rifaximin v léčbě jaterní encefalopatie
- Vnitřní lékařství
- Archiv čísel
- Aktuální číslo
- Pouze online
- Informace o časopisu
Nejčtenější v tomto čísle- Současný pohled na onemocnění jater u srdečního selhání
- Rifaximin v léčbě jaterní encefalopatie
- Histiocytární sarkom
- Závažná rizika spojená s užíváním natrium-fosfátových projímadel
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



