-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Panton-Valentine Leukocidin Is a Very Potent Cytotoxic Factor for Human Neutrophils
The role of the pore-forming Staphylococcus aureus toxin Panton-Valentine leukocidin (PVL) in severe necrotizing diseases is debated due to conflicting data from epidemiological studies of community-associated methicillin-resistant S. aureus (CA-MRSA) infections and various murine disease-models. In this study, we used neutrophils isolated from different species to evaluate the cytotoxic effect of PVL in comparison to other staphylococcal cytolytic components. Furthermore, to study the impact of PVL we expressed it heterologously in a non-virulent staphylococcal species and examined pvl-positive and pvl-negative clinical isolates as well as the strain USA300 and its pvl-negative mutant. We demonstrate that PVL induces rapid activation and cell death in human and rabbit neutrophils, but not in murine or simian cells. By contrast, the phenol-soluble modulins (PSMs), a newly identified group of cytolytic staphylococcal components, lack species-specificity. In general, after phagocytosis of bacteria different pvl-positive and pvl-negative staphylococcal strains, expressing a variety of other virulence factors (such as surface proteins), induced cell death in neutrophils, which is most likely associated with the physiological clearing function of these cells. However, the release of PVL by staphylococcal strains caused rapid and premature cell death, which is different from the physiological (and programmed) cell death of neutrophils following phagocytosis and degradation of virulent bacteria. Taken together, our results question the value of infection-models in mice and non-human primates to elucidate the impact of PVL. Our data clearly demonstrate that PVL acts differentially on neutrophils of various species and suggests that PVL has an important cytotoxic role in human neutrophils, which has major implications for the pathogenesis of CA-MRSA infections.
Published in the journal: . PLoS Pathog 6(1): e32767. doi:10.1371/journal.ppat.1000715
Category: Research Article
doi: https://doi.org/10.1371/journal.ppat.1000715Summary
The role of the pore-forming Staphylococcus aureus toxin Panton-Valentine leukocidin (PVL) in severe necrotizing diseases is debated due to conflicting data from epidemiological studies of community-associated methicillin-resistant S. aureus (CA-MRSA) infections and various murine disease-models. In this study, we used neutrophils isolated from different species to evaluate the cytotoxic effect of PVL in comparison to other staphylococcal cytolytic components. Furthermore, to study the impact of PVL we expressed it heterologously in a non-virulent staphylococcal species and examined pvl-positive and pvl-negative clinical isolates as well as the strain USA300 and its pvl-negative mutant. We demonstrate that PVL induces rapid activation and cell death in human and rabbit neutrophils, but not in murine or simian cells. By contrast, the phenol-soluble modulins (PSMs), a newly identified group of cytolytic staphylococcal components, lack species-specificity. In general, after phagocytosis of bacteria different pvl-positive and pvl-negative staphylococcal strains, expressing a variety of other virulence factors (such as surface proteins), induced cell death in neutrophils, which is most likely associated with the physiological clearing function of these cells. However, the release of PVL by staphylococcal strains caused rapid and premature cell death, which is different from the physiological (and programmed) cell death of neutrophils following phagocytosis and degradation of virulent bacteria. Taken together, our results question the value of infection-models in mice and non-human primates to elucidate the impact of PVL. Our data clearly demonstrate that PVL acts differentially on neutrophils of various species and suggests that PVL has an important cytotoxic role in human neutrophils, which has major implications for the pathogenesis of CA-MRSA infections.
Introduction
Staphylococcus aureus is an important human pathogen that can cause serious diseases [1]. In the last few years, there was a dramatic increase in the incidence of community-associated methicillin-resistant S. aureus (CA-MRSA) infections in otherwise healthy individuals and resistance to multiple antibiotic classes largely limits therapeutic options. Especially the MRSA strain USA300 has widely spread within the United States and has become the cause of more unusually severe diseases, including necrotizing pneumonia, skin infections, osteomyelitis and necrotizing fasciitis [2],[3]. Necrotizing pneumonia seems to be a specific disease entity and often follows infection with influenza virus [4],[5]. To combat these life-threatening infections, there is a need to better understand the bacteria-host interaction and virulence factors involved.
Clinical studies propose the exotoxin Panton-Valentine leukocidin (PVL) as a crucial virulence factor in necrotizing diseases [4],[6]. PVL is a two component pore-forming toxin, which mainly acts on neutrophils [7]. It is expressed by only a small percentage of S. aureus wild-type isolates (2–3%) [8], but it is highly prevalent in S. aureus strains isolated from necrotizing infections [4],[6]. However, several studies that used a diversity of animal models have created conflicting results concerning the role of PVL. One study, applying a mouse acute pneumonia model, suggests PVL as major virulence factor [9]. By contrast, other groups fail to detect a pathogenic function of PVL in murine lung and skin infections and in cell culture experiments, but demonstrate a predominant role of α-hemolysin (α-toxin) and a possible relevance of the bacterial surface protein A (Spa) [10]–[12]. Both factors are expressed at high prevalence among clinical isolates and are considered to contribute to various disease entities [1],[13],[14]. Yet, when a rabbit bacteremia model was used, a transient effect of PVL in the acute phase of infection could be demonstrated [15]. Furthermore, a recent study identified a group of S. aureus peptides, the phenol-soluble modulins (PSMs), with strong cytolytic activity on human neutrophils. As PSMs are released at high concentrations by CA-MRSA strains and contribute to disease development in murine models, the authors propose that PSMs account for the enhanced virulence of CA-MRSA [16].
However, there is some evidence that the actions of S. aureus toxins can be strongly dependent on the animal species used, which should be analysed in detail to better interpret disease-models. In particular, the host cell response to PVL may be species-specific [17], whereas the effects of other staphylococcal factors, such as PSMs, might be species-independent. In this study, we used polymorphonuclear cells (neutrophils) from different species including humans, mice, rabbits and monkeys to test the effect of several virulence factors. As neutrophils are the major defending cells against bacterial invasion, their excessive cell death most likely largely promotes disease development.
Results
The effect of purified S. aureus virulence factors on neutrophils from different species
First, we challenged human neutrophils with purified S. aureus components, including PVL, α-toxin, protein A and PSMs. For PVL, doses≥40 ng/ml (0.04 µg/ml) were sufficient to induce cell damage (Figure 1A). Cell death occurred rapidly, within 1 h, and most likely due to necrosis, as we could not detect characteristic apoptotic features (Figure S2) [18]. In contrast to PVL, α-toxin or protein A did not cause cell death, even when applied at high concentrations, which have pro-inflammatory or cytotoxic effects in other cell types [19],[20]. As recently published [16], three different forms of S. aureus PSMs (PSMα1, PSMα2, PSMα3) were able to provoke cell-lysis. However, cell death induction required relatively high doses of PSMs (≥40 µg/ml) in comparison to PVL (≥40 ng/ml) (Figure 1A). In previous studies, the impact of PVL was mainly tested on human or rabbit neutrophils, as cells from both species were reported to be susceptible to PVL [17]. In line with published data, we found similar responses of human and rabbit neutrophils to low doses of PVL (Figure 1B). The action of PVL appears to be tightly restricted to these species, as neutrophils isolated from Java monkeys (Macaca fascicularis, cynomolgus), the most commonly used non-human primate in biomedical research, were not killed in response to PVL (Figure 1C). In recent reports, models of severe staphylococcal infections were mainly performed in the murine strains BALB/c or C57/BL6 [9],[10]. However, murine neutrophils from both strains were largely resistant to PVL (Figure 1D, E), irrespective of their maturation and inflammatory state (Figure S3).
Fig. 1. The cytolytic effect of purified S.aureus virulence factors on neutrophils from different species. 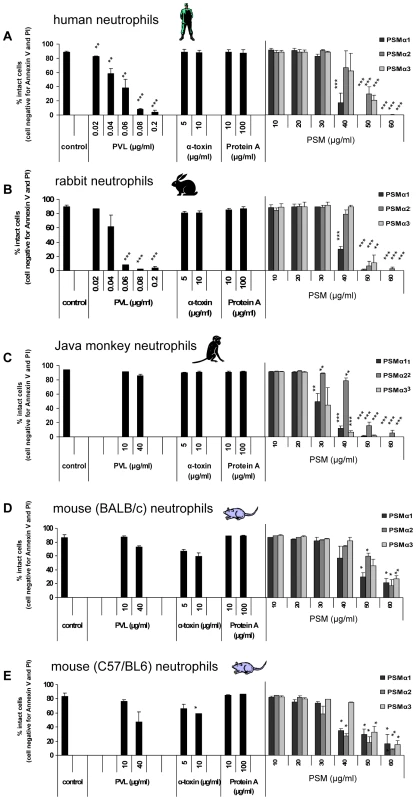
Neutrophils from different species, including human (A), rabbit (B), Java monkey (C), BALB/c mice (D), C57/BL6 mice (E) were freshly isolated and 1×106 0.5 ml−1 cells were incubated with increasing doses of PVL, α-toxin, protein A or PSMs (PSMα1, PSMα2, PSMα3), respectively. PVL: 0.02–0.2 µg/ml (0.5–5 nM); α-toxin: 5, 10 µg/ml (150, 300 nM); protein A: 10, 100 µg/ml (0.238, 2.38 µM); PSMs: 10–60 µg/ml (4–24 µM). Neutrophils were stimulated for 1 h and then cells were washed, stained with annexin V and propidium iodide (taking another hour) and then cell death was measured by flow cytometry. The values represent the mean ± SEM of at least three independent experiments. * P≤0.05, ** P≤0.01, *** P≤0.001 (independent t-test comparing the rate of intact cells between control and stimulated cells). Taking of blood samples from humans and animals were approved by the local ethics committee. In contrast to PVL, all PSM-types tested (PSMα1–3) lysed neutrophils from different species at concentrations≥40 µg/ml, indicating that the actions of PSMs apparently lack species-specificity (Figure 1A–E). Further on, we detected additional differences between PVL - and PSM-induced cell death. Incubation with PVL caused changes in cell morphology, including rounding and swelling of cells and nuclei (Figure 2A, 2B), which persisted for several hours (data not shown). By contrast, PSM-stimulated cells were rapidly destroyed without characteristic changes in morphology (Figure 2A). In PVL-treated neutrophils, an oxidative burst reaction (Figure 2C) and pro-inflammatory activation (Figure S4) accompanied cell death induction, whereas incubation with PSMs did not cause an oxidative burst (Figure 2C). These results point to completely different mechanisms of action provoked by the S. aureus cytotoxic components PVL and PSMs.
Fig. 2. Differences between PVL- and PSMs-induced cell death. 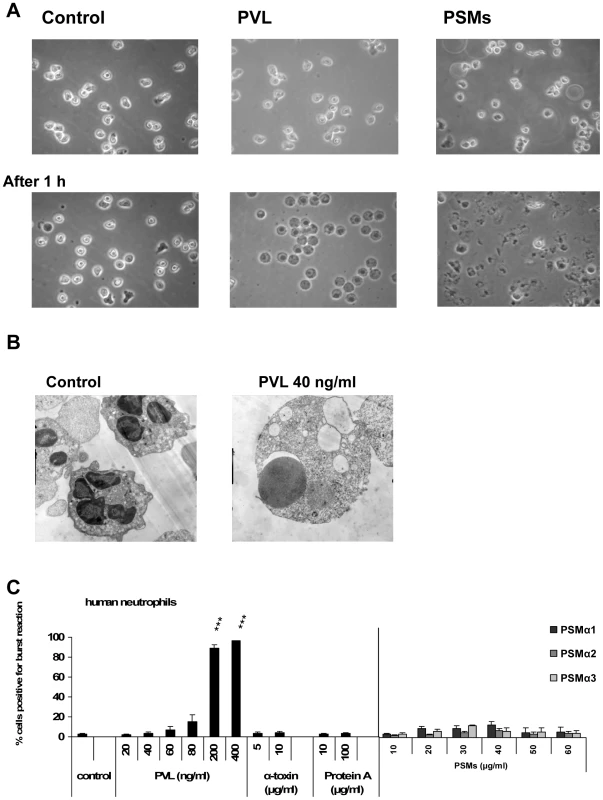
Human neutrophils were freshly isolated and stimulated with staphylococcal components as described in figure 1. Neutrophils were stimulated for 1 h with PVL (80 ng/ml) or PSMs (60 µg/ml) and cells were analyzed by light microscopy with a live cell imaging system (A). Neutrophils were stimulated for 1 h with PVL (40 ng/ml) and processed for electron microscopy (B). Cells were stimulated for 10 min and an oxidative burst reaction was determined by a burst-test (Orpegen Pharma). The values represent the mean ± SEM of at least three independent experiments. * P≤0.05, ** P≤0.01, *** P≤0.001 (independent t-test comparing the rate of burst reaction between control and stimulated cells; C). The effect of live bacteria, which differ in virulence factor expression, on human neutrophils
To investigate the impact of defined virulence factor expression we transformed S. carnosus TM300 with a plasmid encoding the genes for PVL, α-toxin, protein A (Spa) or PSMs, respectively (Table 1). Using live bacteria with these constructs revealed that the expression of PVL most efficiently induced neutrophils cell death (Figure 3A). The effect of TM300+PVL was comparable to the cytotoxic potential of clonally independent MRSA (ST239) and MSSA (6850) strains (Figure 3B) and of pvl-positive clinical isolates, which were recovered from severe invasive (including necrotizing pneumonia) diseases (Figure 3C). However, cytotoxicity was not restricted to PVL-expressing strains, as live bacteria of some pvl-negative isolates compromised cell viability to a similar extent (Figure 3D). Moreover, we could not detect differences between strain USA300 and the corresponding mutant USA300ΔPVL (Figure 3B), indicating that the presence of the pvl-gene does not necessarily contribute to neutrophils cell death following phagocytosis of bacteria. We also failed to block the cytotoxic effect of USA300 by the use of antibodies against PVL (Figure S5). These findings indicate that other staphylococcal factors can also induce cell death, which might mask the cytotoxic function of PVL. However, the expression of α-toxin and PSMs in TM300 had no effect on neutrophils. Apparently, PSMs need to accumulate to lyse neutrophils, as the corresponding bacterial supernatants, which contained PSMs, were cytolytic (Figure S6) [16].
Fig. 3. The impact of PVL expression on human neutrophil survival. 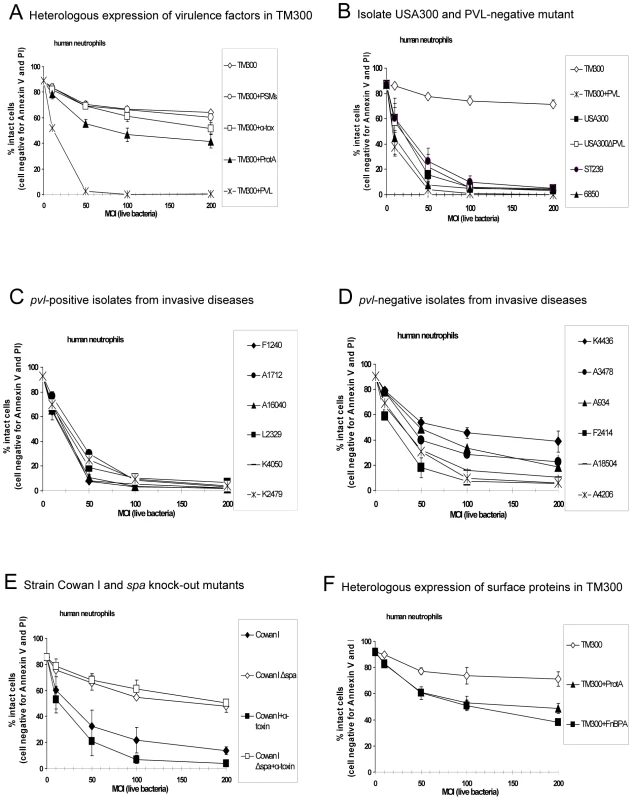
Human neutrophils were freshly isolated and 1×106 0.5 ml−1 cells were incubated with live bacteria, which were grown in overnight cultures and used for stimulating cells at an multiplicity of infection (MOI 10–200) as indicated. In these experiments we used heterologous expression strains of TM300 and Cowan I (A, E, F), the wild-type strain USA300 and its knock-out mutant USA300ΔPVL (B) and pvl-positive (C) and pvl-negative (D) clinical isolates from invasive diseases. After 1 h of incubation with bacteria the cells were washed, stained with annexin V and propidium iodide (taking another hour) and then cell death was measured by flow cytometry. The values represent the mean ± SEM of at least three independent experiments. Tab. 1. Strains used in this study. 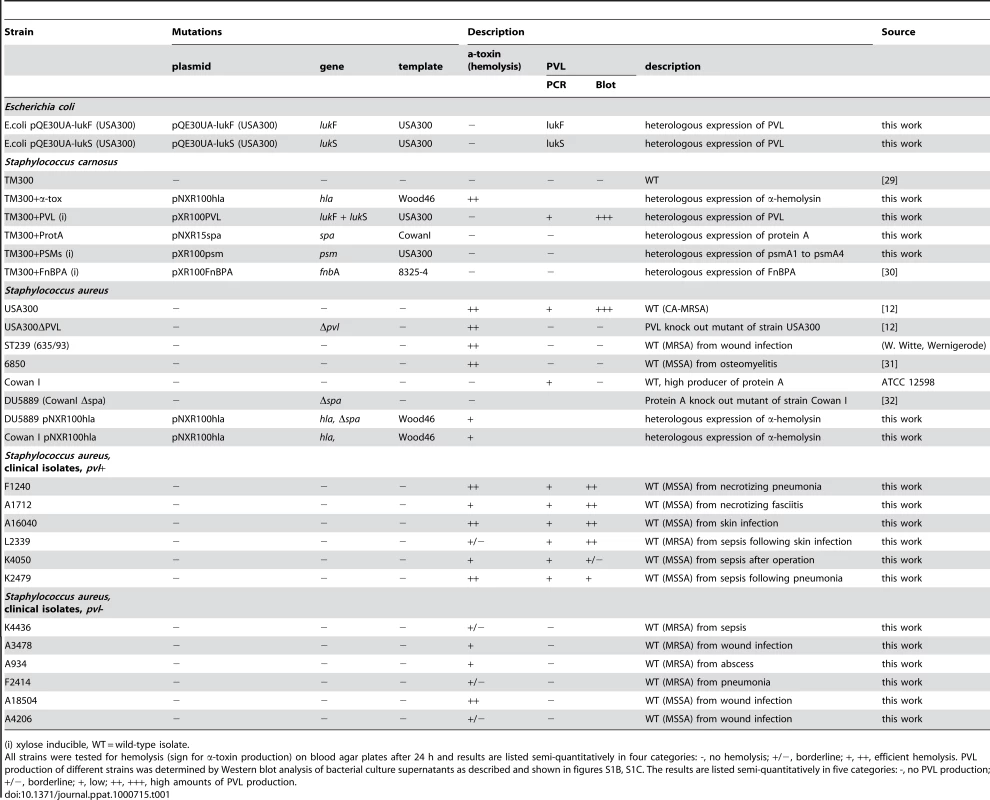
(i) xylose inducible, WT = wild-type isolate. Besides PVL, the expression of protein A moderately decreased the number of intact cells (Figure 3A). This is further demonstrated by using strain Cowan I, which is a high producer of protein A, whereas two isogenic mutants (Δspa) were much less cytotoxic (Figure 3E). Although protein A is known to be a cell wall-anchored protein with an anti-phagocytic effect [14], we observed an increased rate of cell death. In our experiments, the action of protein A was dependent on the expression by bacteria, which exhibit protein A on the bacterial surface. This phenomenon was not specific for protein A, as the expression of another wall-associated protein, namely fibronectin-binding protein A (FnBPA), also reduced the number of intact neutrophils (Figure 3F). In general, phagocytosis of pathogens triggers mechanisms to kill ingested bacteria. Further on, it has been shown that phagocytosis significantly accelerates neutrophils apoptosis, which appears to contribute to the resolution of the inflammatory response [21],[22]. These processes promote healthy resolution and could be an explanation for the enhanced rate of cell death caused by bacteria holding virulent surface proteins. This assumption is further confirmed by apoptotic features detected in neutrophils (Figure S7, annexin V-positive cells).
However, bacterial toxins, such as PVL and PSMs, could interfere with the physiological functions of neutrophils, by rapidly and prematurely killing cells. To investigate this possibility we analysed neutrophils cell death in a time-dependent manner. Challenge with PVL (≥40 ng/ml) induced cell death within the first 20 min (Figure 4A), whereas incubation of neutrophils with live bacteria resulted in a much slower rate of death induction (within 2–3 h), which is most likely associated with the neutrophils physiological function [21]. Using PVL-expressing (USA300) or non PVL-expressing (ST239, 6850) strains did not reveal any differences (Figure 4B).
Fig. 4. Time-dependent effect of purified PVL vs. live bacteria on neutrophil cell death induction. 
Human neutrophils were freshly isolated and 1×106 0.5 ml−1 cells were stimulated with purified PVL (A) or with live bacteria of wild-type strains at an MOI of 100 (B). Cell death was determined every 15 min. For this, cells were washed, rapidly (for 5 min) stained with PI and cell death was instantly determined by flow cytometry. The values represent the mean ± SEM of at least three independent experiments. The cytotoxic effect of bacterial culture supernatants is dependent on PVL expression
PVL is a bacterial exotoxin, which is rapidly released and could act on cells at the infection sites. To mimic this situation, we stimulated neutrophils with sterile-filtered bacterial supernatants from overnight cultures. Culture media from strain TM300+PVL induced rapid cell death within 20 min, whereas supernatants from the control strain TM300 did not affect cell integrity. Further on, comparing supernatants from the wild-type strain USA300 with supernatants from the corresponding knock-out mutant USA300ΔPVL revealed that culture media from the PVL-deletion strain had a much reduced ability to induce cell death, as the majority of cells remained intact (Figure 5A). The impact of PVL release was further strengthened by testing clinical isolates. Supernatants from four out of six pvl-positive strains, recovered from severe (including necrotizing) diseases, had a much higher cytotoxic activity than supernatants from pvl-negative strains (also recovered from severe invasive diseases). It is of particular importance, that PVL secretion of the strains (measured by Western blot in the bacterial supernatants; Figure S1C) clearly corresponded to the cytotoxic activity in all cases (Figure 5B).
Fig. 5. The cytotoxic effect of bacterial culture supernatants is dependent on PVL expression. 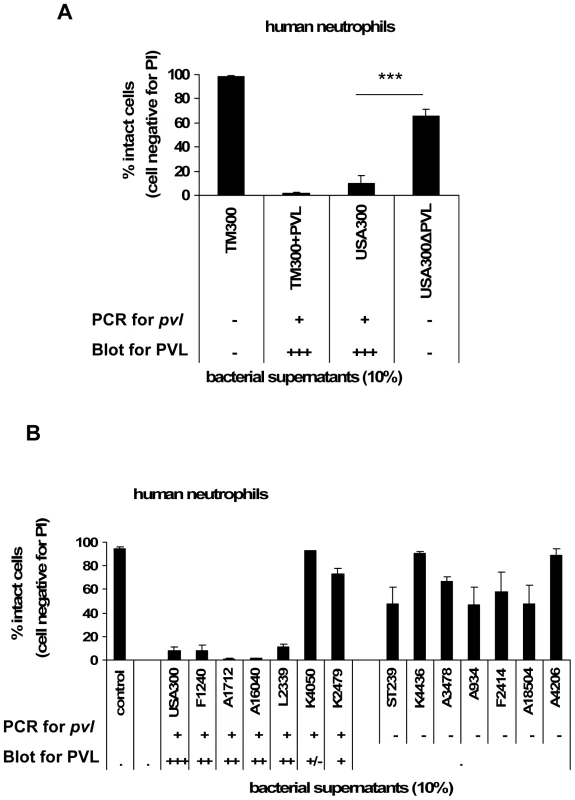
Human neutrophils were freshly isolated and 1×106 0.5 ml−1 cells were incubated with bacterial supernatants, which were prepared from overnight cultures of different strains and used for stimulating cells (10%). In these experiments we used bacterial supernatants of the heterologous expression strain TM300+PVL and of the wild-type strain USA300 and its knock-out mutant USA300ΔPVL (A); furthermore we used bacterial supernatants of pvl-positive and pvl-negative clinical isolates from invasive diseases (B). The presence of the pvl-gene in the indicated strains and the amount of PVL production in the bacterial supernatants is given semi-quantitatively as listed in table 1 and demonstrated in Figure S1C. After 30 min of incubation of the cells with bacterial supernatants, cells were washed, rapidly (for 5 min) stained with PI and cell death was instantly determined by flow cytometry. The values represent the mean ± SEM of at least three independent experiments. *** P≤0.001 (independent t-test comparing the rate of intact cells after stimulation with supernatants of USA300 and USA300ΔPVL). Discussion
The role of PVL in severe CA-MRSA infections is debated due to conflicting data from epidemiological studies, in vitro cell culture experiments, and different animal disease models [9],[10],[12],[23]. As PVL was found in almost all MRSA strains that cause CA-MRSA infections, such as necrotizing pneumonia, skin - and soft tissue infections, it was assumed to be a crucial virulence factor [4],[6]. These disease entities are characterized by massive tissue necrosis and leukopenia, which has been linked to the ability of PVL to kill neutrophils, the primary defending cells against invading bacteria. However, different disease models in mice, in which USA300 and the corresponding knock-out mutant were used, failed to detect a pathogenic function for PVL [10],[12]. In line with these data, we found that murine neutrophils, isolated from different commonly used mice strains, were quite insensitive to PVL. Neutrophils from Java monkeys, a species much more closely related to humans, were not affected by PVL. The reason for the differential sensitivity of cells from various species is completely unknown, but receptors/signal transduction pathways, which are confined to certain species, might be involved. By contrast, all PSM-types tested lysed neutrophils from different species equally efficient and induced membrane damaging effects [16]. Since murine and simian cells are largely resistant to PVL, PSMs might play a more dominant role in S. aureus infections in mice or non-human primates than in humans, especially when high S. aureus inocula are needed to cause diseases. Our data strongly suggest that animal models using mice or non-human primates do not correctly replicate S. aureus diseases in humans, at least if the role of PVL is elucidated. As neutrophils from rabbits are much more susceptible to PVL, this species is most likely more appropriate to study the function of PVL in necrotizing diseases.
Very recently, a rabbit bacteremia model has been published, which describes a modest and transient effect of PVL in the acute phase of infection [15]. However, this type of infection might not show the full pathogenicity of PVL expression, as during bacteremia staphylococci are directly exposed to cells of the immune system. In our experiments, we could not detect differences in virulence between PVL-expressing and pvl-negative (knock-out mutants or wild-type isolates) strains, when live bacteria were directly phagocytized by neutrophils. This is in line with other published data, demonstrating that disruption or absence of the pvl-gene in S. aureus wild-type isolates (including USA300) did not alter their capacity to induce neutrophils cell death [12],[24]. Nevertheless, as cell death of neutrophils is part of the physiological immune response following phagocytosis of bacteria [21],[22] and as S. aureus wild-type isolates express a wide variety of factors promoting this process (e.g. diverse surface proteins) [1], the effect of secreted PVL on human neutrophils might be masked in this model. Furthermore, it is reasonable to suspect that PVL is not (highly) expressed, when staphylococci are instantly phagocytized by neutrophils, as toxic virulence factors were found to be down-regulated after internalization of bacteria [25]. Like other toxins, PVL is mainly expressed in the post-exponential bacterial growth phase [26], which is most likely reached in encapsulated infection foci, e.g. folliculitis, abscesses, tissue necrosis. Only recently, high expression of PVL was found directly in clinical samples from cutaneous abscesses of invasive CA-MRSA infections [27]. Here, PVL most likely accumulates and can also exert systemic pathogenic actions upon entering the bloodstream. In human neutrophils, low doses of PVL were sufficient to cause cell death, which correspond to amounts produced by clinical CA-MRSA strains [28]. Granted that the action of PVL involves yet unknown host receptors/signal transduction pathways, PVL might interfere with various functions of susceptible cells. Furthermore, it is reasonable to speculate that host organisms can become even more vulnerable against PVL, e.g. following an infection with influenza virus. Additional studies on human cells and in susceptible animal models (rabbits) will be necessary to clarify these possibilities and to better define the functions of PVL in staphylococcal infections.
Taken together, our results clearly demonstrate that PVL is a strong cytotoxic factor for human neutrophils, which can play an important role in CA-MRSA infections. Our results do not contradict previously published work, as we could not find an effect of PVL on murine neutrophils or when bacteria were directly phagocytised by neutrophils. However, under certain pathogenic conditions, such as necrosis and abscesses, which are characteristic for severe invasive S. aureus diseases, PVL could exert its function as a cytotoxic exotoxin in susceptible organisms. The premature cell death of neutrophils may be extremely relevant in the virulence of CA-MRSA. As neutrophils are the major defense against invading bacteria, their excessive cell death most likely largely compromises the host's immune system. Furthermore, uncontrolled neutrophils cell damage discharges many pro-inflammatory components within the host tissue, which could also essentially promote disease development. These results are important for ongoing efforts to find therapeutics against S. aureus infections. Due to the rapid spread of CA-MRSA strains and situations, which favour S. aureus infections at a large scale, e.g. epidemic of influenza, there is an urgent need for efficient preventive and therapeutic strategies.
Materials and Methods
Ethics statement
Taking of blood samples from humans and animals and cell isolation were conducted with approval of the local ethics committee (Ethik-Komission der Ärztekammer Westfalen-Lippe und der Medizinischen Fakultät der Westfälischen Wilhelms-Universität Münster). Human blood samples were taken from healthy blood donors, who provided written informed consent for the collection of samples and subsequent neutrophil isolation and analysis. All animals were handled in strict accordance with good animal practice and animal keeping and taking of blood samples were supervised by the veterinary office of Münster (Veterinäramt der Stadt Münster).
Bacterial strains and cultures
Bacterial strains used in this study are listed in table 1. They were all characterized for presence of genes encoding PVL and α-toxin by PCR. Gene expression was investigated by Western blots for PVL (Figure S1B+C) or by hemolysis on sheep blood agar plates (sign for α-toxin production). For cell culture and animal experiments with live staphylococci, bacteria were grown overnight at 37°C in Müller-Hinton medium (MH, containing antibiotics/xylose, if mutants are used) without shaking. Bacteria were washed in PBS and resuspended in PBS with 1% HSA. Neutrophils were incubated with bacterial suspensions, resulting in a multiplicity of infection (MOI) as indicated. Bacterial supernatants were prepared by growing bacteria in 5 ml of brain-heart infusion (BHI) broth (Merck) in a rotary shaker (160 rpm) at 37°C for 12–14 h and pelleted for 10 min at 3350 g. Supernatants were sterile-filtered through a Millex-GP filter unit (0.22 µm; Millipore) and used for the experiments. For PVL isolation, E. coli TG1 strains containing expression vectors for lukF-PV and lukS-PV were grown in Luria Bertani (LB)-media with IPTG (1 mM) and ampicillin (100 mg/ml) and cell lysates were used to purify PVL (Figure S1A).
Plasmid construction and transformation
Different genes were amplified by PCR using chromosomal DNA from different strains (Table S1) as template. To create S. carnosus strains, which express virulence factors of S. aureus, we used two basic vectors, the xylose inducible pXR100 and the pNXR100, which is a non-inducible derivate of the pXR100. For the expression of lukF-PV and lukS-PV in E. coli TG1 the commercial IPTG inducible pQE30UA was used. For creation of the expression vectors the respective genes were amplified by PCR, purified and digested. The basic vectors were also digested corresponding to the genes. After ligation S. carnosus TM300 and E. coli were transformed by protoplast transformation or CaCl–method.
Generation of purified staphylococcal virulence factors and antibodies
The Six-histagged lukF-PV and lukS-PV proteins from E. coli were purified by nickel-nitrilotriacetic acid affinity resin (Qiagen, Germany). α-toxin and Protein A (P3838) were obtained from Sigma-Aldrich Chemie GmbH (Germany). PSMα1 – PSMα3 were synthesized by Genosphere Biotechnology (France). Polyclonal antibodies against lukF-PV and lukS-PV were raised separately and together in rabbits by standard procedures and this was performed by Genosphere-Biotechnology (France).
Preparation and culture of neutrophils
Human, rabbit and Java monkey polymorphonuclear cells (neutrophils) were freshly isolated from Na citrate-treated blood of healthy donors. Neutrophils from BALB/c and C57/BL6 mice were prepared from bone marrow. For neutrophil-isolation, dextran-sedimentation and density gradient centrifugation using Ficoll-Paque Plus (Amersham Bioscience) was used according to the manufacturer's instruction. Cell purity was determined by Giemsa staining and was always above 99%. For murine cells, sedimented cells were used as neutrophils and, in addition, were further deprived of CD3+ (T cells), CD19+ (B cells), and CD11c+ (dendritic cells) cells using MACS technology (Miltenyi Biotech, Bergisch - Gladbach) according to the manufacturer’s instruction. Resulting cells were <0.1% CD3+, CD19+, or CD11c+ and <95% CD11b+ and Gr1+. Neutrophils were resuspended at a final density of 1×106 cells/0.5 ml in RPMI 1640 culture medium (PAA Laboratories GmbH) supplemented with 10% heat-inactivated FCS (PAA Laboratories GmbH) and immediately used for the experiments. All incubations were performed at 37°C in humidified air with 5% CO2.
Cell culture experiments and measurements of oxidative burst activity and cell death
All experiments were performed in 24-well plates and neutrophils were incubated with PVL, α-toxin, PSMs, live bacteria or bacterial supernatants at the indicated concentrations. Oxidative burst activity was determined after 10 min of incubation using a phagoburst test (Orpegen Pharma) according to the manufacturer's instruction. Measurement of cell death was performed after 1 h of incubation followed by washing and double staining of cells with annexin V-FITC and propidium iodide (PI) (taking 1 hour) and then cells were analyzed in a FACScalibur flow cytometer using an annexin V-FITC apoptosis detection kit (Becton Dickinson). For analysis of time-dependent cell death inductions, cells were incubated for the indicated time periods, followed by washing and single staining with PI (taking 10 min) and then cells were immediately analysed by flow cytometry.
Light and transmission electron microscopy
A live cell imaging system (Zeiss) was used to obtain light micrographs. For transmission electron microscopy, 5×106/2.5 ml neutrophils were incubated with PVL at the indicated concentrations for 1 h. Then the cells were washed three times with PBS, fixed in 3% glutaraldehyde, stained in 1% osmium tetroxide and embedded in epoxy resin in the culture dish in situ. Electron micrographs were obtained using imaging plate technology.
Statistical analysis
Unpaired Student’s t-test was performed to compare cell survival. A value of P≤0.05 was considered significant in all cases.
Supporting Information
Zdroje
1. LowyFD
1998 Staphylococcus aureus infections. N Engl J Med 339 520 532
2. GordonRJ
LowyFD
2008 Pathogenesis of methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis 46 Suppl 5 S350 S359
3. KingMD
HumphreyBJ
WangYF
KourbatovaEV
RaySM
2006 Emergence of community-acquired methicillin-resistant Staphylococcus aureus USA 300 clone as the predominant cause of skin and soft-tissue infections. Ann Intern Med 144 309 317
4. GilletY
IssartelB
VanhemsP
FournetJC
LinaG
2002 Association between Staphylococcus aureus strains carrying gene for Panton-Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet 359 753 759
5. RubinsteinE
KollefMH
NathwaniD
2008 Pneumonia caused by methicillin-resistant Staphylococcus aureus. Clin Infect Dis 46 Suppl 5 S378 S385
6. LinaG
PiemontY
Godail-GamotF
BesM
PeterMO
1999 Involvement of Panton-Valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin Infect Dis 29 1128 1132
7. WoodinAM
1960 Purification of the two components of leucocidin from Staphylococcus aureus. Biochem J 75 158 165
8. KuehnertMJ
Kruszon-MoranD
HillHA
McQuillanG
McAllisterSK
2006 Prevalence of Staphylococcus aureus nasal colonization in the United States, 2001-2002. J Infect Dis 193 172 179
9. Labandeira-ReyM
CouzonF
BoissetS
BrownEL
BesM
2007 Staphylococcus aureus Panton-Valentine leukocidin causes necrotizing pneumonia. Science 315 1130 1133
10. BubeckWJ
BaeT
OttoM
DeleoFR
SchneewindO
2007 Poring over pores: alpha-hemolysin and Panton-Valentine leukocidin in Staphylococcus aureus pneumonia. Nat Med 13 1405 1406
11. BubeckWJ
PatelRJ
SchneewindO
2007 Surface proteins and exotoxins are required for the pathogenesis of Staphylococcus aureus pneumonia. Infect Immun 75 1040 1044
12. VoyichJM
OttoM
MathemaB
BraughtonKR
WhitneyAR
2006 Is Panton-Valentine leukocidin the major virulence determinant in community-associated methicillin-resistant Staphylococcus aureus disease? J Infect Dis 194 1761 1770
13. BhakdiS
Tranum-JensenJ
1991 Alpha-toxin of Staphylococcus aureus. Microbiol Rev 55 733 751
14. FosterTJ
2005 Immune evasion by staphylococci. Nat Rev Microbiol 3 948 958
15. DiepBA
Palazzolo-BallanceAM
TattevinP
BasuinoL
BraughtonKR
2008 Contribution of Panton-Valentine leukocidin in community-associated methicillin-resistant Staphylococcus aureus pathogenesis. PLoS ONE 3 e3198 doi:10.1371/journal.pone.0003198
16. WangR
BraughtonKR
KretschmerD
BachTH
QueckSY
2007 Identification of novel cytolytic peptides as key virulence determinants for community-associated MRSA. Nat Med 13 1510 1514
17. SzmigielskiS
PrevostG
MonteilH
ColinDA
JeljaszewiczJ
1999 Leukocidal toxins of staphylococci. Zentralbl Bakteriol 289 185 201
18. GenestierAL
MichalletMC
PrevostG
BellotG
ChalabreysseL
2005 Staphylococcus aureus Panton-Valentine leukocidin directly targets mitochondria and induces Bax-independent apoptosis of human neutrophils. J Clin Invest 115 3117 3127
19. GomezMI
O'SeaghdhaM
MagargeeM
FosterTJ
PrinceAS
2006 Staphylococcus aureus protein A activates TNFR1 signaling through conserved IgG binding domains. J Biol Chem 281 20190 20196
20. HaslingerB
StrangfeldK
PetersG
Schulze-OsthoffK
SinhaB
2003 Staphylococcus aureus alpha-toxin induces apoptosis in peripheral blood mononuclear cells: role of endogenous tumour necrosis factor-alpha and the mitochondrial death pathway. Cell Microbiol 5 729 741
21. DeleoFR
DiepBA
OttoM
2009 Host defense and pathogenesis in Staphylococcus aureus infections. Infect Dis Clin North Am 23 17 34
22. ZhangB
HirahashiJ
CullereX
MayadasTN
2003 Elucidation of molecular events leading to neutrophil apoptosis following phagocytosis: cross-talk between caspase 8, reactive oxygen species, and MAPK/ERK activation. J Biol Chem 278 28443 28454
23. BubeckWJ
Palazzolo-BallanceAM
OttoM
SchneewindO
DeleoFR
2008 Panton-Valentine leukocidin is not a virulence determinant in murine models of community-associated methicillin-resistant Staphylococcus aureus disease. J Infect Dis 198 1166 1170
24. Said-SalimB
MathemaB
BraughtonK
DavisS
SinsimerD
2005 Differential distribution and expression of Panton-Valentine leucocidin among community-acquired methicillin-resistant Staphylococcus aureus strains. J Clin Microbiol 43 3373 3379
25. GarzoniC
FrancoisP
HuygheA
CouzinetS
TapparelC
2007 A global view of Staphylococcus aureus whole genome expression upon internalization in human epithelial cells. BMC Genomics 8 171
26. ArvidsonS
2006 Extracellular Enzymes.
FischettiVA
Gram-Positive Pathogens Washington ASM Press 478 516
27. LoughmanJA
FritzSA
StorchGA
HunstadDA
2009 Virulence gene expression in human community-acquired Staphylococcus aureus infection. J Infect Dis 199 294 301
28. HamiltonSM
BryantAE
CarrollKC
LockaryV
MaY
2007 In vitro production of panton-valentine leukocidin among strains of methicillin-resistant Staphylococcus aureus causing diverse infections. Clin Infect Dis 45 1550 1558
29. GötzF
SchumacherB
1987 Improvment of protoplast trasnformation in Staphylococcus carnosus. FEMS Immunol Med Microbiol 40 285 288
30. SinhaB
FrancoisP
QueYA
HussainM
HeilmannC
2000 Heterologously expressed Staphylococcus aureus fibronectin-binding proteins are sufficient for invasion of host cells. Infect Immun 68 6871 6878
31. BalwitJM
van LangeveldeP
VannJM
ProctorRA
1994 Gentamicin-resistant menadione and hemin auxotrophic Staphylococcus aureus persist within cultured endothelial cells. J Infect Dis 170 1033 1037
32. HartleibJ
KohlerN
DickinsonRB
ChhatwalGS
SixmaJJ
2000 Protein A is the von Willebrand factor binding protein on Staphylococcus aureus. Blood 96 2149 2156
33. HaslingerB
StrangfeldK
PetersG
Schulze-OsthoffK
SinhaB
2003 Staphylococcus aureus alpha-toxin induces apoptosis in peripheral blood mononuclear cells: role of endogenous tumour necrosis factor-alpha and the mitochondrial death pathway. Cell Microbiol 5 729 41
34. ReichardtHM
UmlandT
BauerA
KretzO
SchutzG
2000 Mice with an increased glucocorticoid receptor gene dosage show enhanced resistance to stress and endotoxic shock. Mol Cell Biol 20 9009 17
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek Polyoma Virus-Induced Osteosarcomas in Inbred Strains of Mice: Host Determinants of MetastasisČlánek Nutrient Availability as a Mechanism for Selection of Antibiotic Tolerant within the CF AirwayČlánek Type I Interferon Induction Is Detrimental during Infection with the Whipple's Disease Bacterium,
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2010 Číslo 1- Stillova choroba: vzácné a závažné systémové onemocnění
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
- Diagnostika virových hepatitid v kostce – zorientujte se (nejen) v sérologii
- Jak souvisí postcovidový syndrom s poškozením mozku?
- Infekční komplikace virových respiračních infekcí – sekundární bakteriální a aspergilové pneumonie
-
Všechny články tohoto čísla
- CD8+ T Cell Control of HIV—A Known Unknown
- The Deadly Chytrid Fungus: A Story of an Emerging Pathogen
- Characterization of the Oral Fungal Microbiome (Mycobiome) in Healthy Individuals
- Polyoma Virus-Induced Osteosarcomas in Inbred Strains of Mice: Host Determinants of Metastasis
- Within-Host Evolution of in Four Cases of Acute Melioidosis
- The Type III Secretion Effector NleE Inhibits NF-κB Activation
- Protease-Sensitive Synthetic Prions
- Histone Deacetylases Play a Major Role in the Transcriptional Regulation of the Life Cycle
- Parasite-Derived Plasma Microparticles Contribute Significantly to Malaria Infection-Induced Inflammation through Potent Macrophage Stimulation
- β-Neurexin Is a Ligand for the MSCRAMM SdrC
- Structure of the HCMV UL16-MICB Complex Elucidates Select Binding of a Viral Immunoevasin to Diverse NKG2D Ligands
- Nutrient Availability as a Mechanism for Selection of Antibiotic Tolerant within the CF Airway
- Like Will to Like: Abundances of Closely Related Species Can Predict Susceptibility to Intestinal Colonization by Pathogenic and Commensal Bacteria
- Importance of the Collagen Adhesin Ace in Pathogenesis and Protection against Experimental Endocarditis
- N-glycan Core β-galactoside Confers Sensitivity towards Nematotoxic Fungal Galectin CGL2
- Two Plant Viral Suppressors of Silencing Require the Ethylene-Inducible Host Transcription Factor RAV2 to Block RNA Silencing
- A Small-Molecule Inhibitor of Motility Induces the Posttranslational Modification of Myosin Light Chain-1 and Inhibits Myosin Motor Activity
- Temporal Proteome and Lipidome Profiles Reveal Hepatitis C Virus-Associated Reprogramming of Hepatocellular Metabolism and Bioenergetics
- Marburg Virus Evades Interferon Responses by a Mechanism Distinct from Ebola Virus
- B Cell Activation by Outer Membrane Vesicles—A Novel Virulence Mechanism
- Killing a Killer: What Next for Smallpox?
- PPARγ Controls Dectin-1 Expression Required for Host Antifungal Defense against
- TRIM5α Modulates Immunodeficiency Virus Control in Rhesus Monkeys
- Immature Dengue Virus: A Veiled Pathogen?
- Panton-Valentine Leukocidin Is a Very Potent Cytotoxic Factor for Human Neutrophils
- In Vivo CD8+ T-Cell Suppression of SIV Viremia Is Not Mediated by CTL Clearance of Productively Infected Cells
- Placental Syncytiotrophoblast Constitutes a Major Barrier to Vertical Transmission of
- Type I Interferon Induction Is Detrimental during Infection with the Whipple's Disease Bacterium,
- The M/GP Glycoprotein Complex of Porcine Reproductive and Respiratory Syndrome Virus Binds the Sialoadhesin Receptor in a Sialic Acid-Dependent Manner
- Social Motility in African Trypanosomes
- Melanoma Differentiation-Associated Gene 5 (MDA5) Is Involved in the Innate Immune Response to Infection In Vivo
- Protection of Mice against Lethal Challenge with 2009 H1N1 Influenza A Virus by 1918-Like and Classical Swine H1N1 Based Vaccines
- Upregulation of xCT by KSHV-Encoded microRNAs Facilitates KSHV Dissemination and Persistence in an Environment of Oxidative Stress
- Persistent ER Stress Induces the Spliced Leader RNA Silencing Pathway (SLS), Leading to Programmed Cell Death in
- Evolutionary Trajectories of Beta-Lactamase CTX-M-1 Cluster Enzymes: Predicting Antibiotic Resistance
- Nucleoporin 153 Arrests the Nuclear Import of Hepatitis B Virus Capsids in the Nuclear Basket
- CD8+ Lymphocytes Control Viral Replication in SIVmac239-Infected Rhesus Macaques without Decreasing the Lifespan of Productively Infected Cells
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Panton-Valentine Leukocidin Is a Very Potent Cytotoxic Factor for Human Neutrophils
- CD8+ T Cell Control of HIV—A Known Unknown
- Polyoma Virus-Induced Osteosarcomas in Inbred Strains of Mice: Host Determinants of Metastasis
- The Deadly Chytrid Fungus: A Story of an Emerging Pathogen
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



