-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Ethical Alternatives to Experiments with Novel Potential Pandemic Pathogens
article has not abstract
Published in the journal: . PLoS Med 11(5): e32767. doi:10.1371/journal.pmed.1001646
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001646Summary
article has not abstract
Summary Points
-
“Gain of function” experiments involving the creation and manipulation of novel potential pandemic pathogens (PPPs) deserve ethical scrutiny regarding the acceptability of the risks of accidental or deliberate release and global spread.
-
The Nuremberg Code, a seminal statement of clinical research ethics, mandates that experiments that pose a risk to human life should be undertaken only if they provide humanitarian benefits that sufficiently offset the risks and if these benefits are unachievable by safer means.
-
A novel PPP research program of moderate size would pose substantial risks to human life, even optimistically assuming a low probability that a pandemic would ensue from a laboratory accident.
-
Alternative approaches would not only be safer but would also be more effective at improving surveillance and vaccine design, the two purported benefits of gain-of-function experiments to create novel, mammalian-transmissible influenza strains.
-
A rigorous, quantitative, impartial risk–benefit assessment should precede further novel PPP experimentation. In the case of influenza, we anticipate that such a risk assessment will show that the risks are unjustifiable. Given the risk of a global pandemic posed by such experiments, this risk assessment should be part of a broader international discussion involving multiple stakeholders and not dominated by those with an interest in performing or funding such research.
Two recent publications reporting the creation of ferret-transmissible influenza A/H5N1 viruses [1],[2] are controversial examples of research that aims to produce, sequence and characterize “potential pandemic pathogens” (PPPs) [3], novel infectious agents with known or likely efficient transmission among humans, with significant virulence, and for which there is limited population immunity. There is a quantifiable possibility that these novel pathogens could be accidentally or deliberately released. Exacerbating the immunological vulnerability of human populations to PPPs is the potential for rapid global dissemination via ever-increasing human mobility. The dangers are not just hypothetical. The H1N1 influenza strain responsible for significant morbidity and mortality around the world from 1977 to 2009 is thought to have originated from a laboratory accident [4].
Risk evaluations surrounding biomedical research have not kept pace with scientific innovations in methodology and application. This gap is particularly disconcerting when research involves the construction of PPPs that pose risks of accidental release and global spread. We argue here that accepted principles of biomedical research ethics present a high bar to PPP experiments, requiring that risks arising from such experiments be compensated by benefits to public health not achievable by safer approaches. Focusing on influenza, the object of most current PPP experimentation, we further argue that there are safer experimental approaches that are both more scientifically informative and more straightforward to translate into improved public health through enhanced surveillance, prevention, and treatment of influenza.
Influenza “Gain of Function” Experiments: Prototypical Examples of Potential Pandemic Pathogen Studies
Although several pathogens may be categorized as PPPs (see Box 1), “gain of function” experiments involving influenza strains modified to be PPPs are expanding [5]–[7] (Box 2), and hence of immediate concern. In addition to the two controversial studies recently published, studies with H5N1 [8], H7N9 [9], and H7N1 [10] have used similar ferret passage protocols, while still others have created mammalian-transmissible strains in vitro, followed by in vivo analysis [11],[12]. Related studies have genetically combined less pathogenic zoonotic avian viruses, such as H9N2, with human seasonal influenza viruses to generate strains that exhibit enhanced transmissibility, and to which humans would be immunologically susceptible [13]–[15].
Box 1. Scope for Heightened Ethical Scrutiny of Potential Pandemic Pathogen Experiments
This article describes the responsible ethical scrutiny that should be applied to experimental studies creating or employing PPPs. We define PPPs as infectious agents with four characteristics:
-
Having known or likely efficient transmission among humans
-
Significantly virulent
-
Unmitigated by preexisting population immunity
-
Genetically distinct from pathogens currently circulating
These criteria define pathogens on which experimentation would pose a risk of sparking a pandemic, placing the human population at risk of morbidity or mortality, over and above the background risk of a naturally occurring pandemic. The paradigm case is the creation of variants of influenza A/H5N1 that are readily transmissible between ferrets, a model for human transmission. Such criteria would likely be applicable to experimentation with human isolates of smallpox or SARS, since these pathogens are no longer known to be circulating naturally. In the future, the list may expand [57].
We do not advocate the necessity of heightened scrutiny for isolation and characterization of naturally occurring pathogens, such as wild-type H5N1 or H7N9, consistent with the HHS framework for evaluating gain-of-function studies of H5N1 viruses, which exempts characterization of naturally occurring viruses [33].
Box 2. Gain of Function: What's in a Name?
The recent ferret transmission experiments with influenza A viruses have been termed “gain of function” experiments because they involve engineering viruses that gain transmissibility in ferrets. Gain of function is a common and important approach in biological experimentation, and is not by itself cause for concern [58]. However, the elevated concern over these experiments arises from the particular function that is gained. Ferret transmission is thought to be a good [59],[60] (albeit imperfect [61],[62]) model for human-to-human transmission. Consequently, strains resulting from selection for heightened ferret transmission are likely to be similarly transmissible by humans via respiratory droplets, a prerequisite for pandemic spread. In combination with demonstrated virulence for humans, this particular gain of function presents unique risks and raises special ethical issues.
These studies have typically been conducted in biosafety level (BSL) 3 or 3+ containment facilities. Laboratory-associated infections in BSL3 facilities are conservatively estimated to occur at a rate of two per 1,000 laboratory-years [3],[16] in the United States, where protocols and enforcement are relatively stringent. Globally, high-containment laboratories have variable standards and enforcement [17]. Experimentation in less-regulated or unregulated laboratories, with the attendant risks of accidental or deliberate release, is facilitated by the publication of sequence and functional data on PPPs, even if the original research was conducted with state-of-the-art safety and security [18].
From the conservative estimate of the rate of laboratory-associated infections of two per 1,000 laboratory-years [3],[16], it follows that a moderate research program of ten laboratories at US BSL3 standards for a decade would run a nearly 20% risk of resulting in at least one laboratory-acquired infection, which, in turn, may initiate a chain of transmission. The probability that a laboratory-acquired influenza infection would lead to extensive spread has been estimated to be at least 10% [19]. Simple branching process models suggest a probability of an outbreak arising from an accidental influenza infection in the range of 5% to 60% [20],[21]. Such probabilities cannot be ignored when multiplied by the potential devastation of an influenza pandemic [22],[23], even if the resulting strain were substantially attenuated from the observed virulence of highly pathogenic influenza A/H5N1 [24], the subject of much of the published PPP work to date. We advocate a dispassionate review of pertinent evidence and calculations of the probabilities and magnitudes of potential risks parameterized for specific PPP research programs.
Ethical Frameworks for Novel Potential Pandemic Pathogens
Thus far, experiments with novel PPPs have been assessed in the context of “dual use research of concern” (DURC), a designation for “research that could be used for good or bad purposes” [25]. Within the broader category of DURC, PPP experimentation raises ethical issues that deserve more extensive evaluation than other DURC, because the scale of risk posed by PPPs is much greater. While DURC by definition presents a risk of malevolent use, the impact of the accidental release of many agents involved in DURC—anthrax, hemorrhagic fever viruses, and, most recently, a novel Clostridium botulinum toxin [26],[27] –is constrained by transmission mode or limited host susceptibility. The magnitude of accidental risk for a novel PPP is much greater.
The Nuremberg Code, a seminal document in clinical research ethics, specifies that in research conducted on human participants, “the degree of risk to be taken should never exceed that determined by the humanitarian importance of the problem to be solved by the experiment.” More broadly, 74 national academies of science have stated: “Scientists have an obligation to do no harm. They should always take into consideration the reasonably foreseeable consequences of their own activities” [28]. The ethical principles underlying both guidelines would seem to apply a fortiori to research that imposes far-reaching risk to the public [29]. Given the global nature of influenza transmission, and thus implications beyond a country's borders, international agreement regarding acceptable risks is needed.
Ethical constructs and risk evaluations must be tailored to scientific advances in methodology and application. Limited attention has been paid to the ethics of scientific experiments that pose risks beyond identified human participants [30]–[32]. On a practical level, however, the spirit of the Nuremberg Code's “humanitarian importance” criterion is embodied in the recent frameworks for evaluating PPP experiments from the US Department of Health and Human Services (HHS), the primary sponsor of such experiments to date. The HHS frameworks for studies anticipated to create mammalian-transmissible H5N1 [33] and H7N9 [34],[35] viruses specify that the risks and benefits should be weighed.
The Nuremberg Code's second point states: “The experiment should be such as to yield fruitful results for the good of society, unprocurable by other methods or means of study, and not random and unnecessary in nature.” When projecting the benefits of experiments that put human life at risk, therefore, it is critical to compare against alternatives. What unique public health benefits do PPP experiments offer relative to the benefits of investing equivalent resources in alternative research strategies? If there are unique benefits to novel PPP experiments, do they justify the risks entailed? This concept, too, is partially incorporated in the HHS frameworks, which permit funding of H5N1 [33] or H7N9 [34],[35] transmissibility gain-of-function experiments only if “there are no feasible alternative methods to address the same scientific question in a manner that poses less risk than does the proposed approach” [33]. The Nuremberg Code suggests a broader criterion: that PPP experiments should be performed if the public health benefits envisaged cannot be obtained by safer methods. We argue that alternative scientific approaches are not only less risky, but also more likely to generate results that can be readily translated into public health benefits.
Challenges in Translating Understanding of Influenza Transmission into Public Health Practice
Proponents of PPP experimentation cite two main benefits of such studies: improving our interpretation of surveillance data to detect dangerous viruses and facilitating vaccine development against future natural pandemics. Both claims have been disputed. The vaccine claim has been denied by vaccine developers, who note that many, if not all, vaccines have been developed without a detailed molecular understanding of transmission [36]. Advocates of PPP experimentation further argue that creating potentially pandemic strains of a particular virus, e.g., A/H5N1, could facilitate the production and stockpiling of vaccines against that variant. However, given that PPP experiments inevitably consider only a few possible genetic pathways to transmissibility, and that the precise correspondence between transmissibility in the ferret model and human transmissibility remains uncertain, we can never know whether PPP experimentation would hit upon the antigenic composition of the next pandemic strain that will emerge from nature. Indeed, as described below, it is clear that there is no one-to-one mapping between a few genetic changes in a virus and its transmissibility. By contrast, universal influenza vaccines currently in preclinical and clinical trials [37] may, with further development, prove to be more worthwhile to stockpile for the purposes of pandemic preparedness than an assortment of vaccines targeting antigenic variants manufactured via PPP experimentation.
Current surveillance is likely inadequate to detect an emerging pandemic strain before it is too late [29],[38], regardless of any warnings that PPP experimentation might generate about potentially worrisome mutations. Between 2008 and 2013, over 1,580 highly pathogenic avian influenza (almost all H5N1) outbreaks, involving over 5 million birds, were reported to the World Organisation for Animal Health [39]. The US National Center for Biotechnology Information Influenza Virus Resource [40] received about 1,400 complete or partial avian H5N1 virus sequences over this period [41]. Most of these sequences were over eight months old by the time they were publicly available in the Influenza Virus Resource. Similar considerations apply to GISAID's EpiFlu Database, the other major influenza virus sequence database [42]. Given that birds [43], like humans [44], harbor a genetically diverse quasispecies of influenza variants, it is highly unlikely that such limited surveillance could detect a pandemic viral sequence and, furthermore, spur effective mitigation actions, before the worrisome variant was already widespread in birds. As an example of the limited public health response even when a dangerous virus has been observed, consider the global response to H7N9 avian influenza, which has proven zoonotic potential and has probably been repeatedly transmitted from human to human [45]. Isolates from human cases reveal efficient binding to human sialic acid receptors and airborne transmission in ferrets [9] and guinea pigs [46]. These indicators of pandemic potential are much stronger than sequence comparisons with engineered viruses could provide, yet most live bird markets in China remain open, and human cases continue to emerge [47]. Given these realities, it is difficult to envision how a surveillance signal alone would prompt swifter actions than these existing warning signs for H7N9 have. In short, the benefits for public health of the scientific findings from PPP experimentation are speculative at best.
Epistatic Interactions in Influenza Genetics: A Challenge to Predicting Complex Phenotypes
A further challenge to realizing public health benefits from PPP experimentation is that the predictability of phenotype from viral sequence is complex [38],[48],[49], as demonstrated by a recent assessment [50] of the generality of mutations that conferred human receptor binding in engineered ferret-transmissible H5N1 strains. When these mutations were introduced into the genetic background of more recent avian isolates of H5N1, affinity to human receptors was lost [50]. Instead, the phenotype of any mutation depends on interactions with its genetic background, a phenomenon known as epistasis that is observed broadly in nature and in influenza viruses specifically [51],[52] (Table 1). Thus, it is unlikely that a catalog of mutations could inform reliable predictions of transmission phenotype in circulating strains.
Tab. 1. Evidence of strong epistasis: examples of mutations in influenza A viruses and their varying phenotypes that are dependent on genetic background. 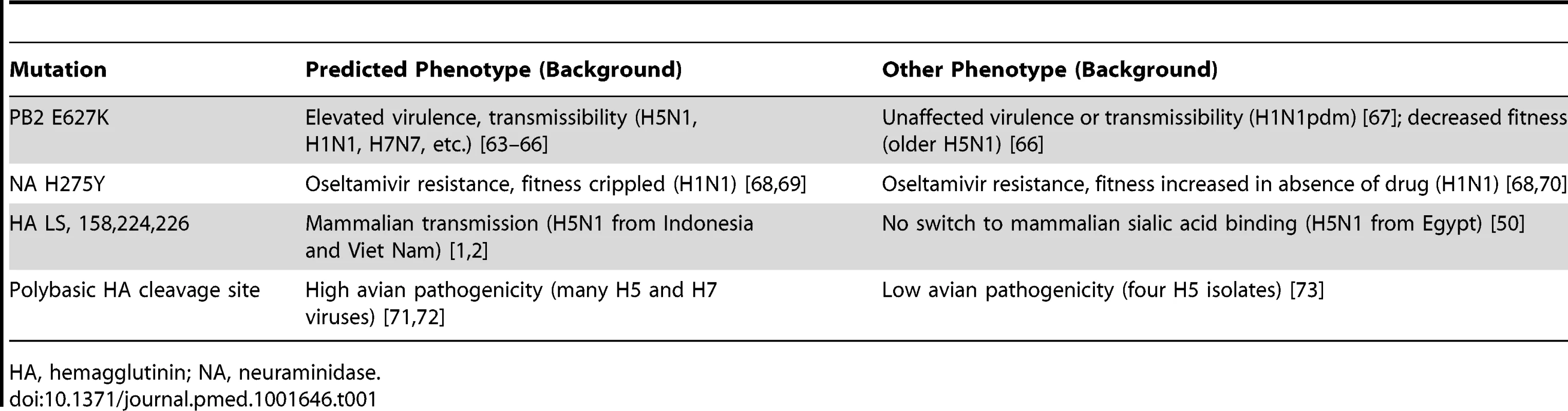
HA, hemagglutinin; NA, neuraminidase. Alternative Approaches: Safer and More Promising
The prominent role of epistasis in influenza biology suggests that alternative approaches to studying the phenotypic impact of mutations on mammalian transmissibility would be not only less risky, but also more informative. In vivo replication and transmission of influenza in humans depend on myriad interdependent factors, including the binding affinity between hemagglutinin and human sialic acids, the ability of the virion to fuse with the endosomal membrane at the appropriate pH and temperature, as well as the stability of various viral proteins [11],[51],[53],[54]. Each of these traits, in turn, is not simply determined by the presence or absence of individual amino acids at particular sites, but by biophysical properties arising from the interaction of many sites within and between proteins [50],[51]. Consequently, the challenge of predicting transmissibility hinges on understanding the genetic determinants of each trait, coupled with the interactions of the traits from which the higher-level phenotype of transmissibility arises. An array of safer approaches (Table 2) to studying influenza pathogenesis and transmission focus on dissecting these interactions. Some approaches start with sequence analysis and molecular dynamics modeling, which are intrinsically safe. The experimental evaluation of hypotheses raised by such studies may use viral components rather than the entire infectious virus, making these experiments simultaneously safer and more precise and mechanistic than engineering PPPs. Furthermore, these approaches are typically less costly than PPP experimentation, facilitating phenotypic evaluation of a greater diversity and abundance of genetic variants. Ultimately, studies with intact viruses will be necessary for a full understanding of human transmissibility, a phenotype of a whole virus. Elucidating the evolutionary trajectory through which existing seasonal (former pandemic) viruses became transmissible from avian precursors is safer than PPP experimentation, given that there is preexisting population immunity to seasonal strains, the products of such evolution.
Tab. 2. Safer approaches to studying human adaptation of influenza A viruses, and more generally to improving vaccines and therapeutics. 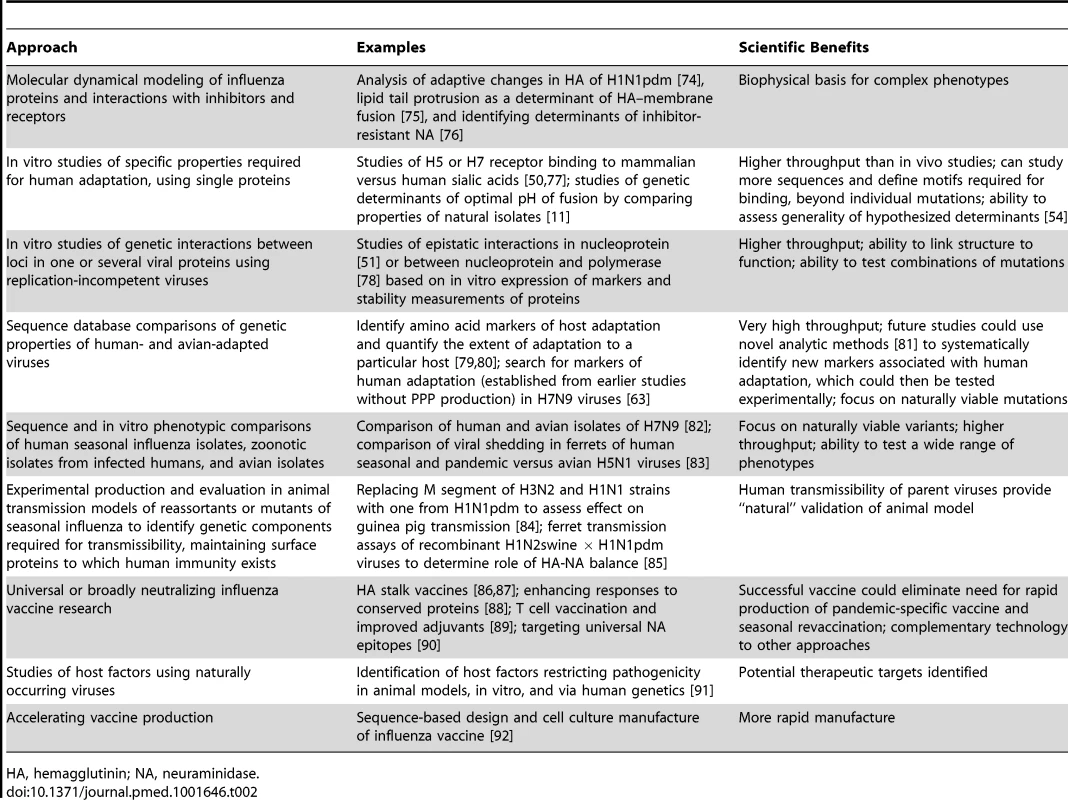
HA, hemagglutinin; NA, neuraminidase. More generally, it should be remembered that the public health goal is to curtail influenza pandemics and seasonal transmission [55],[56]. Exploring basic biology is just one scientific means to this end. Other approaches, such as developing universal influenza vaccines and novel antiviral drugs and strategies to enhance host responses, as well as improving technologies for rapid vaccine manufacture, are being pursued without risks of PPP release (Table 2).
Paths Forward
We urge that proposals for any future experiments on PPPs be evaluated according to quantitative risk–benefit analysis guided by the principles of the Nuremberg Code. Indeed, HHS frameworks require a risk–benefit analysis to approve gain-of-function experimentation on H5N1 and H7N9 [33]–[35] viruses, yet no such analysis has been made public, if it has been conducted. Other funding and regulatory agencies, which have not yet called for a risk–benefit analysis, should require one as well. In biomedical grant review processes, proposals compete for limited funding, and most proposals that could advance science are never supported, because of budget constraints or because funding agencies conclude that there are more promising, safer, more humane, or otherwise superior ways to achieve scientific goals. PPP experimentation poses a significant risk to public health, arguably the highest level of risk posed by any biomedical research. Such experiments should be assessed on the basis of their marginal benefits, compared to those of safer approaches. In the case of influenza, given the higher throughput and lower cost of alternatives, we believe the benefits of alternative approaches will be greater than those of novel PPP experimentation, yet without the risks–thereby negating the justification for taking such risks. Similarly, careful consideration should be given to analyses of novel PPP experiments beyond the study of influenza, as these are proposed. Funders and regulators should evaluate the balance of risks and benefits before further novel PPP experiments are undertaken.
Zdroje
1. ImaiM, WatanabeT, HattaM, DasSC, OzawaM, et al. (2012) Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486 : 420–428.
2. HerfstS, SchrauwenEJ, LinsterM, ChutinimitkulS, de WitE, et al. (2012) Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336 : 1534–1541.
3. Klotz LC, Sylvester EJ (2012) The unacceptable risks of a man-made pandemic. Bulletin of the Atomic Sciences. Available: http://thebulletin.org/unacceptable-risks-man-made-pandemic. Accessed 15 April 2014.
4. WebsterRG, BeanWJ, GormanOT, ChambersTM, KawaokaY (1992) Evolution and ecology of influenza A viruses. Microbiol Rev 56 : 152–179.
5. FouchierRA, Garcia-SastreA, KawaokaY (2013) H5N1 virus: transmission studies resume for avian flu. Nature 493 : 609.
6. FouchierRA, KawaokaY, CardonaC, CompansRW, FouchierRA, et al. (2013) Avian flu: Gain-of-function experiments on H7N9. Nature 500 : 150–151.
7. FouchierRA, KawaokaY, CardonaC, CompansRW, Garcia-SastreA, et al. (2013) Gain-of-function experiments on H7N9. Science 341 : 612–613.
8. MainesTR, ChenLM, Van HoevenN, TumpeyTM, BlixtO, et al. (2011) Effect of receptor binding domain mutations on receptor binding and transmissibility of avian influenza H5N1 viruses. Virology 413 : 139–147.
9. RichardM, SchrauwenEJ, de GraafM, BestebroerTM, SpronkenMI, et al. (2013) Limited airborne transmission of H7N9 influenza A virus between ferrets. Nature 501 : 560–563.
10. Sutton TC, Finch C, Shao H, Angel M, Chen H, et al.. (2014) airborne transmission of highly pathogenic H7N1 influenza in ferrets. J Virol. E-pub ahead of print. doi:10.1128/JVI.02765-13
11. SheltonH, RobertsKL, MolestiE, TempertonN, BarclayWS (2013) Mutations in haemagglutinin that affect receptor binding and pH stability increase replication of a PR8 influenza virus with H5 HA in the upper respiratory tract of ferrets and may contribute to transmissibility. J Gen Virol 94 : 1220–1229.
12. ZhangY, ZhangQ, KongH, JiangY, GaoY, et al. (2013) H5N1 hybrid viruses bearing 2009/H1N1 virus genes transmit in guinea pigs by respiratory droplet. Science 340 : 1459–1463.
13. QiaoC, LiuQ, BawaB, ShenH, QiW, et al. (2012) Pathogenicity and transmissibility of reassortant H9 influenza viruses with genes from pandemic H1N1 virus. J Gen Virol 93 : 2337–2345.
14. SorrellEM, WanH, ArayaY, SongH, PerezDR (2009) Minimal molecular constraints for respiratory droplet transmission of an avian-human H9N2 influenza A virus. Proc Natl Acad Sci U S A 106 : 7565–7570.
15. KimbleJB, SorrellE, ShaoH, MartinPL, PerezDR (2011) Compatibility of H9N2 avian influenza surface genes and 2009 pandemic H1N1 internal genes for transmission in the ferret model. Proc Natl Acad Sci U S A 108 : 12084–12088.
16. HenkelRD, MillerT, WeyantRS (2012) Monitoring select agent theft, loss and release reports in the United States–2004–2010. Appl Biosaf 18 : 171–180.
17. Hottes AK, Rusek B, Sharples F, Committee on Anticipating Biosecurity Challenges of the Global Expansion of High Containment Biological Laboratories, National Academy of Sciences and National Research Council (2012) Biosecurity challenges of the global expansion of high-containment biological laboratories: summary of a workshop. Washington (District of Columbia): National Academies Press.
18. CasadevallA, EnquistL, ImperialeMJ, KeimP, OsterholmMT, et al. (2013) Redaction of sensitive data in the publication of dual use research of concern. MBio 5: e00991–13.
19. MerlerS, AjelliM, FumanelliL, VespignaniA (2013) Containing the accidental laboratory escape of potential pandemic influenza viruses. BMC Med 11 : 252.
20. LipsitchM, CohenT, CooperB, RobinsJM, MaS, et al. (2003) Transmission dynamics and control of severe acute respiratory syndrome. Science 300 : 1966–1970.
21. Lloyd-SmithJO, SchreiberSJ, KoppPE, GetzWM (2005) Superspreading and the effect of individual variation on disease emergence. Nature 438 : 355–359.
22. US Department of Health and Human Services (2007) Interim pre-pandemic planning guidance: community strategy for pandemic influenza mitigation in the United States–early targeted layered use of nonpharmaceutical interventions. Washington (District of Columbia): US Department of Health and Human Services.
23. Van KerkhoveMD, HirveS, KoukounariA, MountsAW (2013) Estimating age-specific cumulative incidence for the 2009 influenza pandemic: a meta-analysis of A(H1N1)pdm09 serological studies from 19 countries. Influenza Other Respir Viruses 7 : 872–886.
24. Van KerkhoveMD, RileyS, LipsitchM, GuanY, MontoAS, et al. (2012) Comment on “Seroevidence for H5N1 influenza infections in humans: meta-analysis”. Science 336 : 1506.
25. BernsKI, CasadevallA, CohenML, EhrlichSA, EnquistLW, et al. (2012) Public health and biosecurity. Adaptations of avian flu virus are a cause for concern. Science 335 : 660–661.
26. BarashJR, ArnonSS (2013) A novel strain of Clostridium botulinum that produces type B and type H botulinum toxins. J Infect Dis 209 : 183–191.
27. RelmanDA (2013) “Inconvenient truths” in the pursuit of scientific knowledge and public health. J Infect Dis 209 : 170–172.
28. Interacademy Panel on International Issues (2005) IAP statement on biosecurity. Trieste (Italy): Interacademy Panel on International Issues.
29. LipsitchM, BloomBR (2012) Rethinking biosafety in research on potential pandemic pathogens. MBio 3: e00360–12.
30. BachFH, FishmanJA, DanielsN, ProimosJ, AndersonB, et al. (1998) Uncertainty in xenotransplantation: individual benefit versus collective risk. Nat Med 4 : 141–144.
31. OrdT, HillerbrandR, SandbergA (2010) Probing the improbable: methodological challenges for risks with low probabilities and high stakes. J Risk Res 13 : 191–205.
32. Presidential Commission for the Study of Bioethical Issues (2010) New directions: the ethics of synthetic biology and emerging technologies. Washington (District of Columbia): Presidential Commission for the Study of Bioethical Issues.
33. PattersonAP, TabakLA, FauciAS, CollinsFS, HowardS (2013) Research funding. A framework for decisions about research with HPAI H5N1 viruses. Science 339 : 1036–1037.
34. JaffeH, PattersonAP, LurieN (2013) Extra oversight for H7N9 experiments. Science 341 : 713–714.
35. JaffeHW, PattersonAP, LurieN (2013) Avian flu: extra oversight for H7N9 experiments. Nature 500 : 151.
36. MahmoudA (2013) Gain-of-function research: unproven technique. Science 342 : 310–311.
37. PicaN, PaleseP (2013) Toward a universal influenza virus vaccine: prospects and challenges. Annu Rev Med 64 : 189–202.
38. LipsitchM, PlotkinJB, SimonsenL, BloomB (2012) Evolution, safety, and highly pathogenic influenza viruses. Science 336 : 1529–1531.
39. World Organisation for Animal Health (2013) WAHID Interface [database]. Available: http://www.oie.int/wahis_2/public/wahid.php/Countryinformation/Diseasetimeseries. Accessed 28 December 2013.
40. BaoY, BolotovP, DernovoyD, KiryutinB, ZaslavskyL, et al. (2008) The influenza virus resource at the National Center for Biotechnology Information. J Virol 82 : 596–601.
41. US National Center for Biotechnology Information (2013) Influenza Virus Resource [database]. Available: http://www.ncbi.nlm.nih.gov/genomes/FLU/Database/nph-select.cgi?go=database. Accessed 27 December 2013.
42. The GISAID Initiative (2013) EpiFlu Database [database]. Available: http://platform.gisaid.org/epi3/frontend#3ef74c. Accessed 14 April 2013.
43. RamakrishnanMA, TuZJ, SinghS, ChockalingamAK, GramerMR, et al. (2009) The feasibility of using high resolution genome sequencing of influenza A viruses to detect mixed infections and quasispecies. PLoS ONE 4: e7105.
44. PoonLL, ChanKH, ChuDK, FungCC, ChengCK, et al. (2011) Viral genetic sequence variations in pandemic H1N1/2009 and seasonal H3N2 influenza viruses within an individual, a household and a community. J Clin Virol 52 : 146–150.
45. Leung NH, Worby CJ, Hanage WP, Lipsitch M, Cowling BJ (2013) Human-to-human transmission of H7N9 in a family: “probable” vs “possible”. BMJ Online Rapid Response. Available: http://www.bmj.com/content/347/bmj.f4752/rr/657652. Accessed 15 April 2014.
46. GabbardJD, DlugolenskiD, Van RielD, MarshallN, GallowaySE, et al. (2014) Novel H7N9 influenza virus shows low infectious dose, high growth rate, and efficient contact transmission in the guinea pig model. J Virol 88 : 1502–1512.
47. World Health Organization (2014) Human infection with avian influenza virus–update. Available: http://www.who.int/csr/don/2014_01_31/en/. Accessed 28 February 2014.
48. MorensDM, TaubenbergerJK, FauciAS (2013) Pandemic influenza viruses–hoping for the road not taken. N Engl J Med 368 : 2345–2348.
49. Wain-HobsonS (2013) Pandemic influenza viruses: time to recognize our inability to predict the unpredictable and stop dangerous gain-of-function experiments. EMBO Mol Med 5 : 1637–1641.
50. TharakaramanK, RamanR, ViswanathanK, StebbinsNW, JayaramanA, et al. (2013) Structural determinants for naturally evolving H5N1 hemagglutinin to switch its receptor specificity. Cell 153 : 1475–1485.
51. GongLI, SuchardMA, BloomJD (2013) Stability-mediated epistasis constrains the evolution of an influenza protein. Elife 2: e00631.
52. KryazhimskiyS, DushoffJ, BazykinGA, PlotkinJB (2011) Prevalence of epistasis in the evolution of influenza A surface proteins. PLoS Genet 7: e1001301.
53. TrockSC, BurkeSA, CoxNJ (2012) Development of an influenza virologic risk assessment tool. Avian Dis 56 : 1058–1061.
54. SheltonH, Ayora-TalaveraG, RenJ, LoureiroS, PicklesRJ, et al. (2011) Receptor binding profiles of avian influenza virus hemagglutinin subtypes on human cells as a predictor of pandemic potential. J Virol 85 : 1875–1880.
55. IskanderJ, StrikasRA, GensheimerKF, CoxNJ, ReddSC (2013) Pandemic influenza planning, United States, 1978–2008. Emerg Infect Dis 19 : 879–885.
56. Wellcome Trust (2014) Influenza. Available: http://www.wellcome.ac.uk/About-us/Policy/Spotlight-issues/Influenza/index.htm. Accessed 15 April 2014.
57. Garrett L (2013 October 15) Biology's brave new world: the promise and perils of the synbio revolution. Foreign Affairs. Available: http://www.foreignaffairs.com/articles/140156/laurie-garrett/biologys-brave-new-world. Accessed 15 April 2014.
58. BreithauptH (2014) Flu season: an interview with Jeffery K. Taubenberger, Chief of the Viral Pathogenesis and Evolution Section at the US National Institute of Allergy and Infectious Diseases. EMBO Rep 15 : 212–217.
59. BelserJA, KatzJM, TumpeyTM (2011) The ferret as a model organism to study influenza A virus infection. Dis Model Mech 4 : 575–579.
60. BelserJA, MainesTR, KatzJM, TumpeyTM (2013) Considerations regarding appropriate sample size for conducting ferret transmission experiments. Future Microbiol 8 : 961–965.
61. PaleseP, WangTT (2012) H5N1 influenza viruses: facts, not fear. Proc Natl Acad Sci U S A 109 : 2211–2213.
62. LipsitchM (2013) Avian influenza: ferret H7N9 flu model questioned. Nature 501 : 33.
63. JongesM, MeijerA, FouchierRA, KochG, LiJ, et al. (2013) Guiding outbreak management by the use of influenza A(H7Nx) virus sequence analysis. Euro Surveill 18 : 20460.
64. de WitE, MunsterVJ, van RielD, BeyerWE, RimmelzwaanGF, et al. (2010) Molecular determinants of adaptation of highly pathogenic avian influenza H7N7 viruses to efficient replication in the human host. J Virol 84 : 1597–1606.
65. SteelJ, LowenAC, MubarekaS, PaleseP (2009) Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog 5: e1000252.
66. LongJS, HowardWA, NunezA, MoncorgeO, LycettS, et al. (2013) The effect of the PB2 mutation 627K on highly pathogenic H5N1 avian influenza virus is dependent on the virus lineage. J Virol 87 : 9983–9996.
67. HerfstS, ChutinimitkulS, YeJ, de WitE, MunsterVJ, et al. (2010) Introduction of virulence markers in PB2 of pandemic swine-origin influenza virus does not result in enhanced virulence or transmission. J Virol 84 : 3752–3758.
68. BloomJD, GongLI, BaltimoreD (2010) Permissive secondary mutations enable the evolution of influenza oseltamivir resistance. Science 328 : 1272–1275.
69. HerlocherML, TrusconR, EliasS, YenHL, RobertsNA, et al. (2004) Influenza viruses resistant to the antiviral drug oseltamivir: transmission studies in ferrets. J Infect Dis 190 : 1627–1630.
70. ChaoDL, BloomJD, KochinBF, AntiaR, LonginiIMJr (2012) The global spread of drug-resistant influenza. J R Soc Interface 9 : 648–656.
71. VeyM, OrlichM, AdlerS, KlenkHD, RottR, et al. (1992) Hemagglutinin activation of pathogenic avian influenza viruses of serotype H7 requires the protease recognition motif R-X-K/R-R. Virology 188 : 408–413.
72. WoodGW, McCauleyJW, BashiruddinJB, AlexanderDJ (1993) Deduced amino acid sequences at the haemagglutinin cleavage site of avian influenza A viruses of H5 and H7 subtypes. Arch Virol 130 : 209–217.
73. LondtBZ, BanksJ, AlexanderDJ (2007) Highly pathogenic avian influenza viruses with low virulence for chickens in in vivo tests. Avian Pathol 36 : 347–350.
74. Jimenez-AlbertoA, Alvarado-FacundoE, Ribas-AparicioRM, Castelan-VegaJA (2013) Analysis of adaptation mutants in the hemagglutinin of the influenza A(H1N1)pdm09 virus. PLoS ONE 8: e70005.
75. LarssonP, KassonPM (2013) Lipid tail protrusion in simulations predicts fusogenic activity of influenza fusion peptide mutants and conformational models. PLoS Comput Biol 9: e1002950.
76. RipollDR, KhavrutskiiIV, ChaudhuryS, LiuJ, KuschnerRA, et al. (2012) Quantitative predictions of binding free energy changes in drug-resistant influenza neuraminidase. PLoS Comput Biol 8: e1002665.
77. TharakaramanK, JayaramanA, RamanR, ViswanathanK, StebbinsNW, et al. (2013) Glycan receptor binding of the influenza A virus H7N9 hemagglutinin. Cell 153 : 1486–1493.
78. CauldwellAV, MoncorgeO, BarclayWS (2013) Unstable polymerase-nucleoprotein interaction is not responsible for avian influenza virus polymerase restriction in human cells. J Virol 87 : 1278–1284.
79. TamuriAU, Dos ReisM, HayAJ, GoldsteinRA (2009) Identifying changes in selective constraints: host shifts in influenza. PLoS Comput Biol 5: e1000564.
80. dos ReisM, TamuriAU, HayAJ, GoldsteinRA (2011) Charting the host adaptation of influenza viruses. Mol Biol Evol 28 : 1755–1767.
81. WongEH, SmithDK, RabadanR, PeirisM, PoonLL (2010) Codon usage bias and the evolution of influenza A viruses. Codon usage biases of influenza virus. BMC Evol Biol 10 : 253.
82. ZhangQ, ShiJ, DengG, GuoJ, ZengX, et al. (2013) H7N9 influenza viruses are transmissible in ferrets by respiratory droplet. Science 341 : 410–414.
83. GustinKM, KatzJM, TumpeyTM, MainesTR (2013) Comparison of the levels of infectious virus in respirable aerosols exhaled by ferrets infected with influenza viruses exhibiting diverse transmissibility phenotypes. J Virol 87 : 7864–7873.
84. ChouYY, AlbrechtRA, PicaN, LowenAC, RichtJA, et al. (2011) The M segment of the 2009 new pandemic H1N1 influenza virus is critical for its high transmission efficiency in the guinea pig model. J Virol 85 : 11235–11241.
85. YenHL, LiangCH, WuCY, ForrestHL, FergusonA, et al. (2011) Hemagglutinin-neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets. Proc Natl Acad Sci U S A 108 : 14264–14269.
86. KrammerF, PaleseP (2013) Influenza virus hemagglutinin stalk-based antibodies and vaccines. Curr Opin Virol 3 : 521–530.
87. WeiCJ, YassineHM, McTamneyPM, GallJG, WhittleJR, et al. (2012) Elicitation of broadly neutralizing influenza antibodies in animals with previous influenza exposure. Sci Transl Med 4 : 147ra114.
88. SchmitzN, BeerliRR, BauerM, JegerlehnerA, DietmeierK, et al. (2012) Universal vaccine against influenza virus: linking TLR signaling to anti-viral protection. Eur J Immunol 42 : 863–869.
89. HughesB, HaydenF, PerikovY, HombachJ, TamJS (2012) Report of the 5th meeting on influenza vaccines that induce broad spectrum and long-lasting immune responses, World Health Organization, Geneva, 16–17 November 2011. Vaccine 30 : 6612–6622.
90. DoyleTM, JaentschkeB, Van DomselaarG, HashemAM, FarnsworthA, et al. (2013) The universal epitope of influenza A viral neuraminidase fundamentally contributes to enzyme activity and viral replication. J Biol Chem 288 : 18283–18289.
91. EverittAR, ClareS, PertelT, JohnSP, WashRS, et al. (2012) IFITM3 restricts the morbidity and mortality associated with influenza. Nature 484 : 519–523.
92. DormitzerPR, SuphaphiphatP, GibsonDG, WentworthDE, StockwellTB, et al. (2013) Synthetic generation of influenza vaccine viruses for rapid response to pandemics. Sci Transl Med 5 : 185ra168.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2014 Číslo 5- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
-
Všechny články tohoto čísla
- The Role of Open Access in Reducing Waste in Medical Research
- Provider-Initiated HIV Testing and Counselling for Children
- Fecal Contamination of Drinking-Water in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis
- Call to Action: Promoting Domestic and Global Tobacco Control by Ratifying the Framework Convention on Tobacco Control in the United States
- Methods for Specifying the Target Difference in a Randomised Controlled Trial: The Difference ELicitation in TriAls (DELTA) Systematic Review
- Achieving the HIV Prevention Impact of Voluntary Medical Male Circumcision: Lessons and Challenges for Managing Programs
- Effectiveness of a Pre-treatment Snack on the Uptake of Mass Treatment for Schistosomiasis in Uganda: A Cluster Randomized Trial
- Communicating and Monitoring Surveillance and Response Activities for Malaria Elimination: China's “1-3-7” Strategy
- Improving the Quality of Adult Mortality Data Collected in Demographic Surveys: Validation Study of a New Siblings' Survival Questionnaire in Niakhar, Senegal
- Yellow Fever in Africa: Estimating the Burden of Disease and Impact of Mass Vaccination from Outbreak and Serological Data
- Gene-Lifestyle Interaction and Type 2 Diabetes: The EPIC InterAct Case-Cohort Study
- Barriers to Provider-Initiated Testing and Counselling for Children in a High HIV Prevalence Setting: A Mixed Methods Study
- Maternal Overweight and Obesity and Risks of Severe Birth-Asphyxia-Related Complications in Term Infants: A Population-Based Cohort Study in Sweden
- Ethical Alternatives to Experiments with Novel Potential Pandemic Pathogens
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Provider-Initiated HIV Testing and Counselling for Children
- Fecal Contamination of Drinking-Water in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis
- Achieving the HIV Prevention Impact of Voluntary Medical Male Circumcision: Lessons and Challenges for Managing Programs
- Effectiveness of a Pre-treatment Snack on the Uptake of Mass Treatment for Schistosomiasis in Uganda: A Cluster Randomized Trial
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



