-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Voluntary Medical Male Circumcision: A Framework Analysis of Policy and Program Implementation in Eastern and Southern Africa
Background:
Following confirmation of the effectiveness of voluntary medical male circumcision (VMMC) for HIV prevention, the World Health Organization and the Joint United Nations Programme on HIV/AIDS issued recommendations in 2007. Less than 5 y later, priority countries are at different stages of program scale-up. This paper analyzes the progress towards the scale-up of VMMC programs. It analyzes the adoption of VMMC as an additional HIV prevention strategy and explores the factors may have expedited or hindered the adoption of policies and initial program implementation in priority countries to date.Methods and Findings:
VMMCs performed in priority countries between 2008 and 2010 were recorded and used to classify countries into five adopter categories according to the Diffusion of Innovations framework. The main predictors of VMMC program adoption were determined and factors influencing subsequent scale-up explored. By the end of 2010, over 550,000 VMMCs had been performed, representing approximately 3% of the target coverage level in priority countries. The “early adopter” countries developed national VMMC policies and initiated VMMC program implementation soon after the release of the WHO recommendations. However, based on modeling using the Decision Makers' Program Planning Tool (DMPPT), only Kenya appears to be on track towards achievement of the DMPPT-estimated 80% coverage goal by 2015, having already achieved 61.5% of the DMPPT target. None of the other countries appear to be on track to achieve their targets. Potential predicators of early adoption of male circumcision programs include having a VMMC focal person, establishing a national policy, having an operational strategy, and the establishment of a pilot program.Conclusions:
Early adoption of VMMC policies did not necessarily result in rapid program scale-up. A key lesson is the importance of not only being ready to adopt a new intervention but also ensuring that factors critical to supporting and accelerating scale-up are incorporated into the program. The most successful program had country ownership and sustained leadership to translate research into a national policy and program.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 8(11): e32767. doi:10.1371/journal.pmed.1001133
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001133Summary
Background:
Following confirmation of the effectiveness of voluntary medical male circumcision (VMMC) for HIV prevention, the World Health Organization and the Joint United Nations Programme on HIV/AIDS issued recommendations in 2007. Less than 5 y later, priority countries are at different stages of program scale-up. This paper analyzes the progress towards the scale-up of VMMC programs. It analyzes the adoption of VMMC as an additional HIV prevention strategy and explores the factors may have expedited or hindered the adoption of policies and initial program implementation in priority countries to date.Methods and Findings:
VMMCs performed in priority countries between 2008 and 2010 were recorded and used to classify countries into five adopter categories according to the Diffusion of Innovations framework. The main predictors of VMMC program adoption were determined and factors influencing subsequent scale-up explored. By the end of 2010, over 550,000 VMMCs had been performed, representing approximately 3% of the target coverage level in priority countries. The “early adopter” countries developed national VMMC policies and initiated VMMC program implementation soon after the release of the WHO recommendations. However, based on modeling using the Decision Makers' Program Planning Tool (DMPPT), only Kenya appears to be on track towards achievement of the DMPPT-estimated 80% coverage goal by 2015, having already achieved 61.5% of the DMPPT target. None of the other countries appear to be on track to achieve their targets. Potential predicators of early adoption of male circumcision programs include having a VMMC focal person, establishing a national policy, having an operational strategy, and the establishment of a pilot program.Conclusions:
Early adoption of VMMC policies did not necessarily result in rapid program scale-up. A key lesson is the importance of not only being ready to adopt a new intervention but also ensuring that factors critical to supporting and accelerating scale-up are incorporated into the program. The most successful program had country ownership and sustained leadership to translate research into a national policy and program.
: Please see later in the article for the Editors' SummaryIntroduction
In 2009, more than 25 y after HIV was first identified, 2.6 million people had become infected, and there were an estimated 33.3 million people living with HIV worldwide [1]. In the absence of a vaccine, the next best means to combat new HIV infections is the implementation of evidence-based prevention strategies including male and female condoms [2], antiretroviral prophylaxis to prevent vertical transmission from mother to child [3],[4], harm reduction for people who inject drugs [5], and, most recently, treating HIV-infected people in serodiscordant couples with antiretroviral drugs to reduce transmission to partners [6]. However, the scale-up of these HIV prevention programs remains challenging despite evidence demonstrating their effectiveness. The use of male and female condoms, despite decades of promotion and distribution, remains suboptimal. The use of female condoms as a prevention strategy for HIV is reportedly lower than male condom use, including in countries in sub-Saharan Africa, where the majority of new HIV infections are occurring through heterosexual transmission [7] and are predominantly among women.
Evidence demonstrating the effectiveness of voluntary medical male circumcision (VMMC) in preventing HIV sexual transmission was first released in 2005 from the South Africa (Orange Farm) randomized controlled trial (RCT) [8]. This was followed by results in 2006 from RCTs in Uganda (Rakai District) and Kenya (Kisumu) [9],[10]. All three RCTs confirmed that male circumcision performed by well-trained and equipped medical providers is safe and reduces the risk of heterosexual acquisition of HIV infection among men by as much as 60%. These RCT results confirmed decades of evidence from observational studies suggesting male circumcision's strong protective effect for men against HIV [11]. Male circumcision also has a strong protective effect against other sexually transmitted infections in men and in women [12]–[16]. Although there is no conclusive evidence that medical male circumcision has a direct effect on women's risk of HIV infection [17], a systematic review, largely based on observational studies, estimated an overall 20% lower HIV incidence in female partners of circumcised men, compared with partners of uncircumcised men [18].
Following the release of the results of the RCTs, in 2007 the World Health Organization (WHO) and the Joint United Nations Programme on HIV/AIDS (UNAIDS) convened an international consultation of stakeholders from a range of disciplines to review the body of evidence from the three trials and the wealth of earlier ecological and observational studies [19]. The consultation resulted in a firm endorsement of the evidence from the three trials, and the formulation of eleven key conclusions and recommendations for the implementation and scale-up of VMMC programs in countries and settings with generalized high-prevalence HIV epidemics and low levels of male circumcision [19].
WHO and UNAIDS identified 13 countries in southern and eastern African as high-priority countries for the implementation and rapid scale-up of VMMC programs: Botswana, Kenya, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, Swaziland, Tanzania, Uganda, Zambia, and Zimbabwe. These countries have been working towards the implementation of VMMC programs using operational guidance developed by WHO and UNAIDS. The guidance emphasizes ten essential components of program implementation: leadership and partnerships, situation analysis, advocacy, enabling policy and regulatory environments, national strategy and operational plans, quality assurance and improvement, human resource development, commodity security, social change communication, and monitoring and evaluation [20].
A consensus report of six different models showed that in settings with high HIV prevalence and low circumcision prevalence, one new HIV infection could be averted for every five to 15 circumcisions performed [21]. More detailed modeling was incorporated into the Decision Maker's Program Planning Tool (DMPPT), and it is estimated that scaling up circumcision programs to reach 80% of adult uncircumcised men within 5 y in 13 priority countries would require a total of 20.3 million circumcisions to be performed and a further 8.4 million between 2016 and 2025, averting an estimated 3.4 million new HIV infections and 386,000 AIDS deaths through 2025 [22]. Despite convincing results demonstrating that VMMC is an effective, cost-saving intervention in the fight against HIV, there have been major challenges and barriers to implementing programs in the high priority countries.
This paper analyzes the progress towards achievement of VMMC for HIV prevention program scale-up in 13 priority countries. We analyze the adoption of VMMC as an additional HIV prevention strategy. We further explore the factors that may have expedited or hindered the adoption of VMMC policies and strategies as well as initial program implementation in the 13 priority countries to date. We also explore the factors that may have influenced subsequent program scale-up. Challenges encountered and lessons learned are highlighted for application to countries still in the early stages of VMMC scale-up as well as to other potential HIV prevention strategies such as topical (vaginal and rectal microbicides) and oral pre-exposure prophylaxis.
Methods
The actual numbers of VMMCs performed in priority countries per calendar year since 2008 were recorded and the totals used to classify countries into five adopter categories according to the Diffusion of Innovations (DOI) framework. Country progress towards achievement of the goal of circumcising 80% of eligible men was also calculated [22].
The DOI and ExpandNet frameworks were selected to analyze the status of VMMC programming in the 13 priority countries as they are complimentary theories that both refer to the process by which innovations are disseminated and taken to scale. The DOI and ExpandNet frameworks highlight the importance of the nature of the innovation itself and the sociopolitical context or environment in which diffusion takes place (see Figure 1). Whereas the DOI theory addresses the diffusion of any innovation, the WHO ExpandNet framework explicitly addresses the adoption and scale-up of public health programs and services in the health sector. Both frameworks stress that innovations that are Credible, Observable, and Relevant; have Relative advantages; are Easy to install and understand; and are Compatible and Testable (“CORRECT”) are most likely to be successfully adopted and scaled up [23].
Fig. 1. Comparison of Diffusion of Innovation and ExpandNet frameworks. 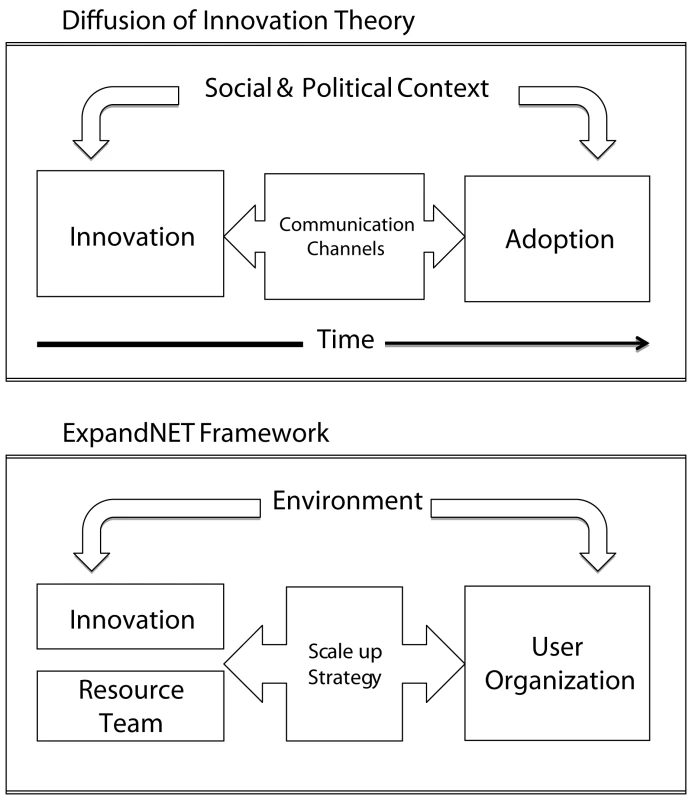
A comparison of the DOI and ExpandNet frameworks is shown. Whereas the DOI describes the process through which innovations are adopted and diffused through the population, the ExpandNet framework specifically addresses the diffusion and scale-up of public health interventions. As highlighted in the figure, the ExpandNet framework reflects the earlier thinking of the DOI and incorporates the elements of context as environment, communication channels as scale-up strategy, and adoption by the population as adoption by the organization implementing the intervention. The DOI theory defines diffusion as the process by which an innovation is communicated through certain channels over time among members of a social system [24]. The DOI theory posits that regardless of the setting, initially there are a few individuals who adopt innovations, known as the “innovators”—these are those who are willing to adopt new ideas before they are mainstream. Following this, another small proportion, the “early adopters,” of the population follow. The “early majority” is the next group to adopt the innovation. By this time, more than half of the population has adopted the innovation. The “late majority” is the next group to accept new interventions; the “laggards” are the last to adopt innovations, they represent those who are least likely to accept innovation (see Figure 2). While the DOI theory refers to the adoption pattern of individuals within a community, we applied these concepts to analyze the adoption of VMMC policies, strategies, and initial program implementation by countries. The DOI framework was used to define the adoption status of each country to comparatively assess progress towards scale-up among the 13 priority countries.
Fig. 2. Diffusion of Innovation adoption status. 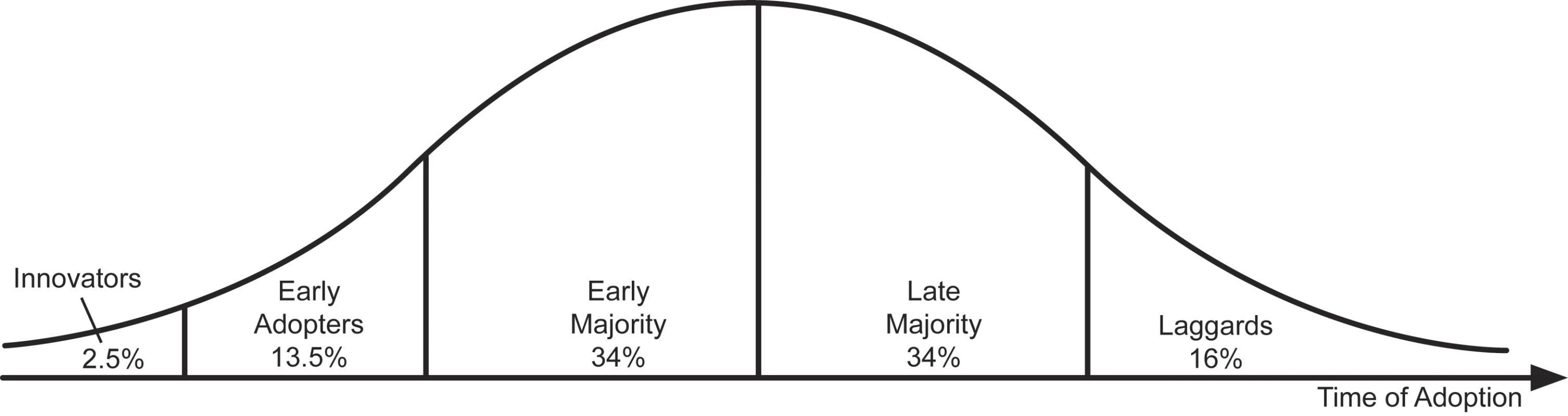
The typical distribution of categories of adopters according to the DOI theory is shown in this figure. The very first adopters or innovators typically represent 2.5% of the population. The next group of adopters, called early adopters, represent about 13.5% of the population and are followed by the early majority, who represent approximately 34% of the total population. The next 34% of the population to adopt are the late majority; this group is followed by the remaining 16% of the population, who are the laggards, the last to adopt a new innovation. In order to facilitate analysis using the DOI framework, six program components based on key elements defined as essential for the operationalization of VMMC programs described in the WHO/UNAIDS operational guidance were used to assess overall country progress towards VMMC program scale-up [20]. The six elements selected were those for which progress towards scale up over a 3-y period could be objectively quantified. A country was assigned a score for each key element, ranging from 0 (no progress) to 3 (maximum progress). A total scale-up score, a composite indicator of progress in program scale-up, was calculated for each country. Additionally, further analyses were undertaken in order to understand if there were differences in the contributions of the six key elements to the overall DOI adoption status, since one can argue that some elements are better predictors of adoption and scale-up than others. To do this, the association between the DOI classification “adopter status” and the scores on the individual elements of scale-up was determined using a crude estimation of association based on an R-squared analysis.
The ExpandNet framework is based on the theory underpinning the DOI model and supplemented with experiences applying the model in low-resource settings [25]. The ExpandNet framework views scaling up as an open system that draws on five interacting elements: the innovation itself, the resource team, the scale-up strategy, the user organization, and the environment. We used the ExpandNet framework to explore the factors that may have influenced subsequent program scale-up, highlighting factors specific to VMMC.
Results
The “CORRECT” attributes of VMMC are highlighted in Table 1. Male circumcision, an old procedure but an innovation for HIV prevention, has many of the “CORRECT” attributes needed to enhance scalability. VMMC is Credible, with consistent evidence of reduced HIV rates from numerous Observational studies and RCTs conducted by respected researchers in Africa, where the intervention is Relevant, as it provides a new solution to address a high-burden public health problem; VMMC has Relative advantages, as it is a one-time intervention conferring lifetime reduction in risk of HIV infection. Medical male circumcision is not particularly Easy to install, as it is a surgical intervention that requires training and expertise, with complex social and cultural barriers that need to be overcome as programs are scaled up. However, it is a one-time intervention, provides a rare opportunity to reach men, and it is cost saving [22],[26]. Medical male circumcision is Compatible with existing national priorities for HIV prevention in the priority countries. In all priority countries, VMMC services have been or are being pilot Tested, providing critical information for moving to scale.
Tab. 1. ExpandNet innovation characteristics. 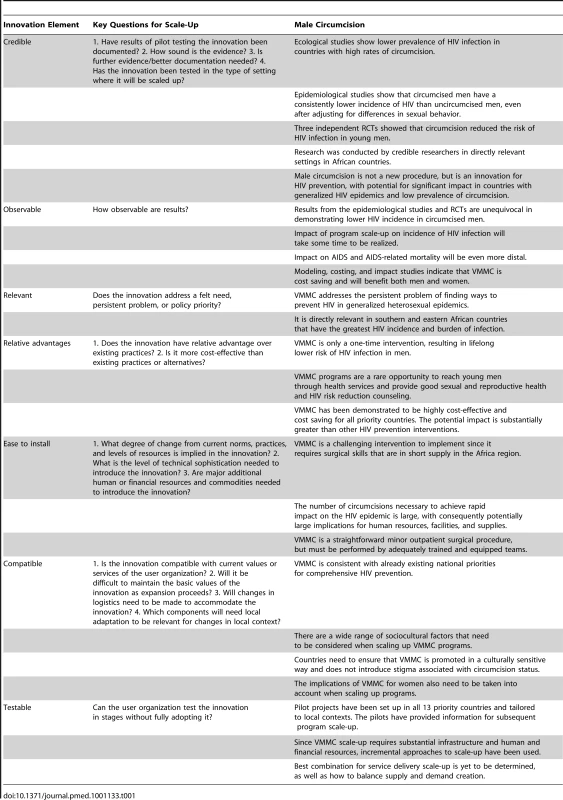
Table 2 shows that between 2008 and 2010, an estimated total of 559,528 VMMCs for HIV prevention have been done in the 13 priority countries, with a large majority (417,974) done in 2010. Kenya has carried out the largest number (232,287) of VMMCs, followed by South Africa (145,475) and then Zambia (81,849). Table 2 also shows the classification of countries according to DOI adopter status. The innovator (8% of countries), Kenya, started performing VMMCs in or before 2008 and reached more than 10,000 VMMCs in 2008. Early adopters (23% of countries), South Africa, Zambia, and Swaziland, started in or before 2008. The early majority (38% of countries), Botswana, Zimbabwe, Tanzania, Namibia, and Mozambique started in 2009. The late majority (15% of countries), Uganda and Rwanda, started in 2010 and did more than 1,000 VMMCs. The laggards (15% of countries), Malawi and Lesotho, did fewer than 1,000 VMMCs in 2010. The distribution of the total scale-up scores reflecting adoption status among the 13 countries in this study compares well with the distribution proposed by the DOI theory. Also highlighted in Table 2, only Kenya appears to be on track towards achievement of the DMPPT-estimated 80% coverage goal by 2015, having already achieved 61.5% of the DMPPT target. None of the other countries—including the early adopters—appear to be on track to achieve their targets.
Tab. 2. Service delivery statistics. 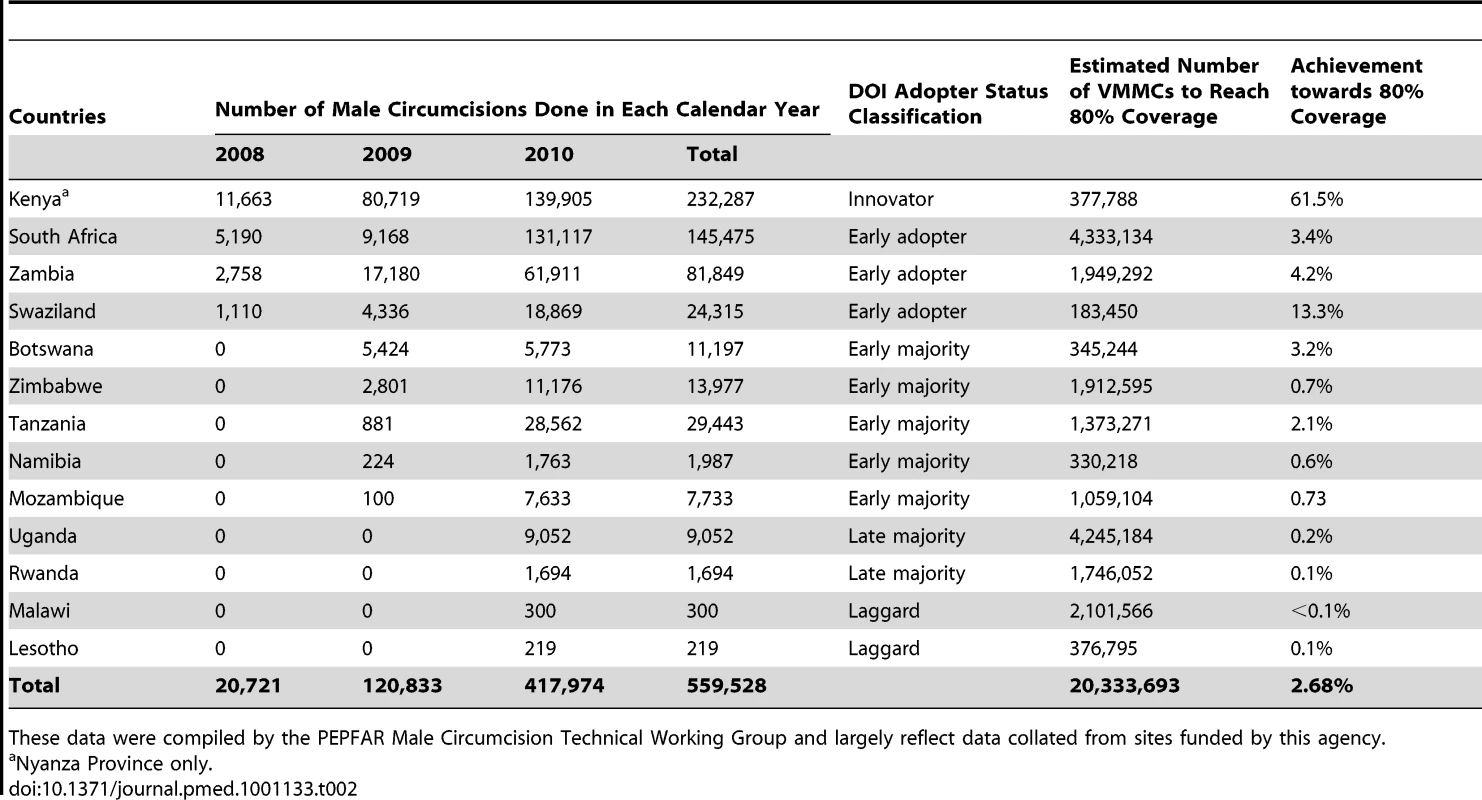
These data were compiled by the PEPFAR Male Circumcision Technical Working Group and largely reflect data collated from sites funded by this agency. Table 3 shows the scoring scheme for each of the six key elements derived from the WHO/UNAIDS operational guidance, reflecting also the time when the different milestones were achieved (earlier completion resulting in higher scores). Table 4 shows the scores for each element by country and reflects the progress in scaling up key program elements in all of the priority countries. The total scale-up scores calculated for each of the 13 countries ranged from a low of 4 (Mozambique) to a high of 17 (Kenya) out of a maximum score of 18. To date, all countries have conducted a situation analysis to assess the acceptability of introducing VMMC programs with the support of a WHO toolkit [27]. At least seven countries had conducted their situation analyses in 2008, within a year of the release of the WHO/UNAIDS recommendations. Beyond the conduct of the situation analysis, progress towards the other key elements of scale-up varies significantly among the 13 countries.
Tab. 3. VMMC key elements of program scale-up scoring key. 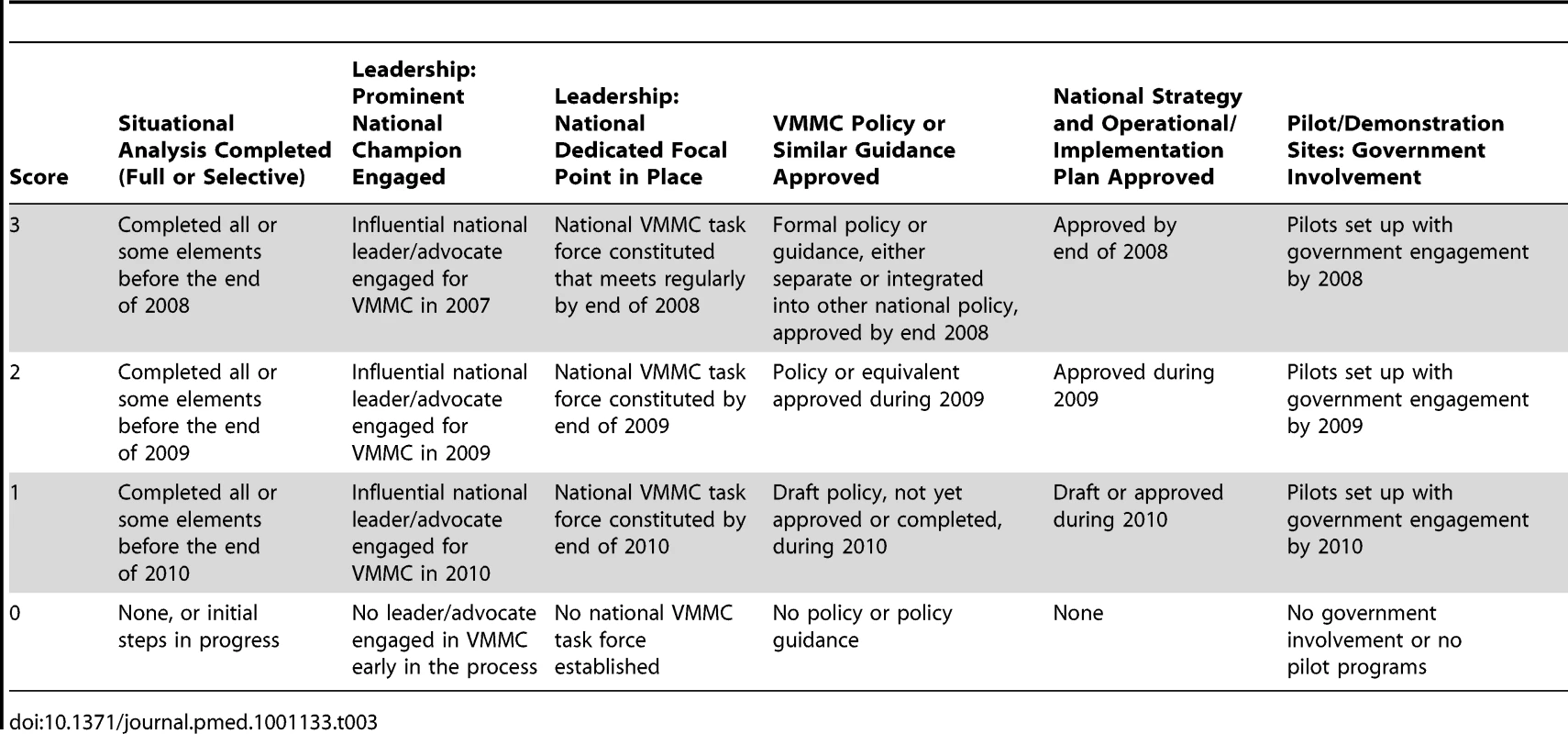
In particular, large variation is seen in the leadership scores, with only Botswana, Kenya, Rwanda, and Swaziland having clearly identifiable prominent national champions for VMMC. We found that although almost all countries had a dedicated national focal person for VMMC in place, Botswana and Kenya had identified theirs within the first year of scale-up. Twelve out of the 13 countries had nationally approved policies for VMMC scale-up by the end of 2010, with Botswana and Kenya having their policies in place within a year of the WHO/UNAIDS recommendations. By the end of 2010, only Mozambique and Uganda did not have nationally approved scale-up strategies.
Figure 3 summarizes the results of the R-squared analysis for each of the six key elements of scale-up identified in this study. The figure shows each of the 13 countries according to their DOI classification and their scores on the individual elements of VMMC program scale-up (Table 4), together with a crude estimate of association (R-squared) computed by assigning a linear score to the DOI classes. The association values can range from 0 to 1, with an R-squared value of 1 indicating perfect association. For this analysis, the association values ranged from 0.16 to 0.57. As the results suggest, conducting a pilot program (R-squared = 0.57) may be the most important predictor of DOI class, followed by establishing a male circumcision focal point (R-squared = 0.27), developing a national male circumcision policy (R-squared = 0.27), and developing a national implementation strategy (R-squared = 0.26). The role of having a national champion (R-squared = 0.17) and conducting a situation analysis (R-squared = 0.16) was shown to have a weaker predictive value on the likelihood of VMMC adoption and program scale-up.
Fig. 3. Association of scale-up element scores and Diffusion of Innovation adoption status. 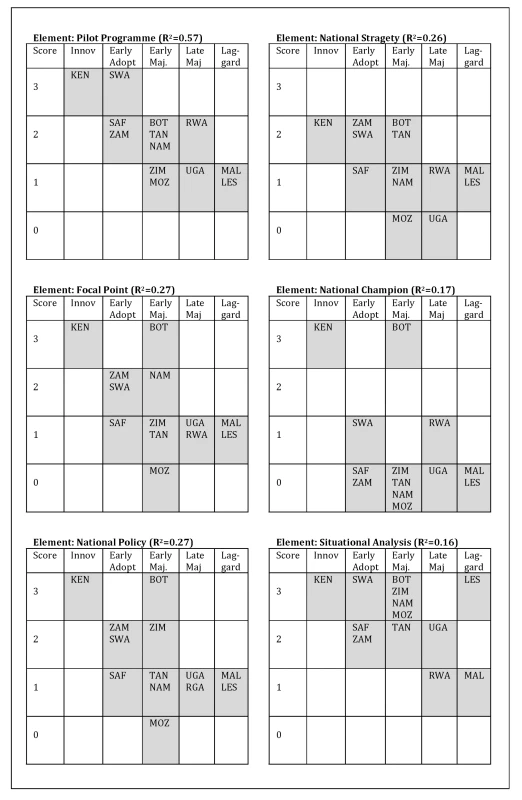
The correlation between each of the six elements of scale-up and DOI adoption status is shown in this figure. The scores obtained (ranging from 0 to 3) for each element by each country is shown (on the vertical axis) in relation to the adoption status (shown on the horizontal axis). Having a pilot program appears to be the strongest predictor of adoption status; this can be seen in the linear clustering of the countries. Conversely, having conducted a situational analysis appears to the least predictive of adoption status; the clustering of the countries is less linear and appears more random. BOT, Botswana; KEN, Kenya; LES, Lesotho; MAL, Malawi; MOZ, Mozambique; NAM, Namibia; RWA, Rwanda; SAF, South Africa; SWA, Swaziland; TAN, Tanzania; UGA, Uganda; ZAM, Zambia; ZIM, Zimbabwe. Tab. 4. Country progress with scaling- up VMMC programs in focal countries (December 2010). 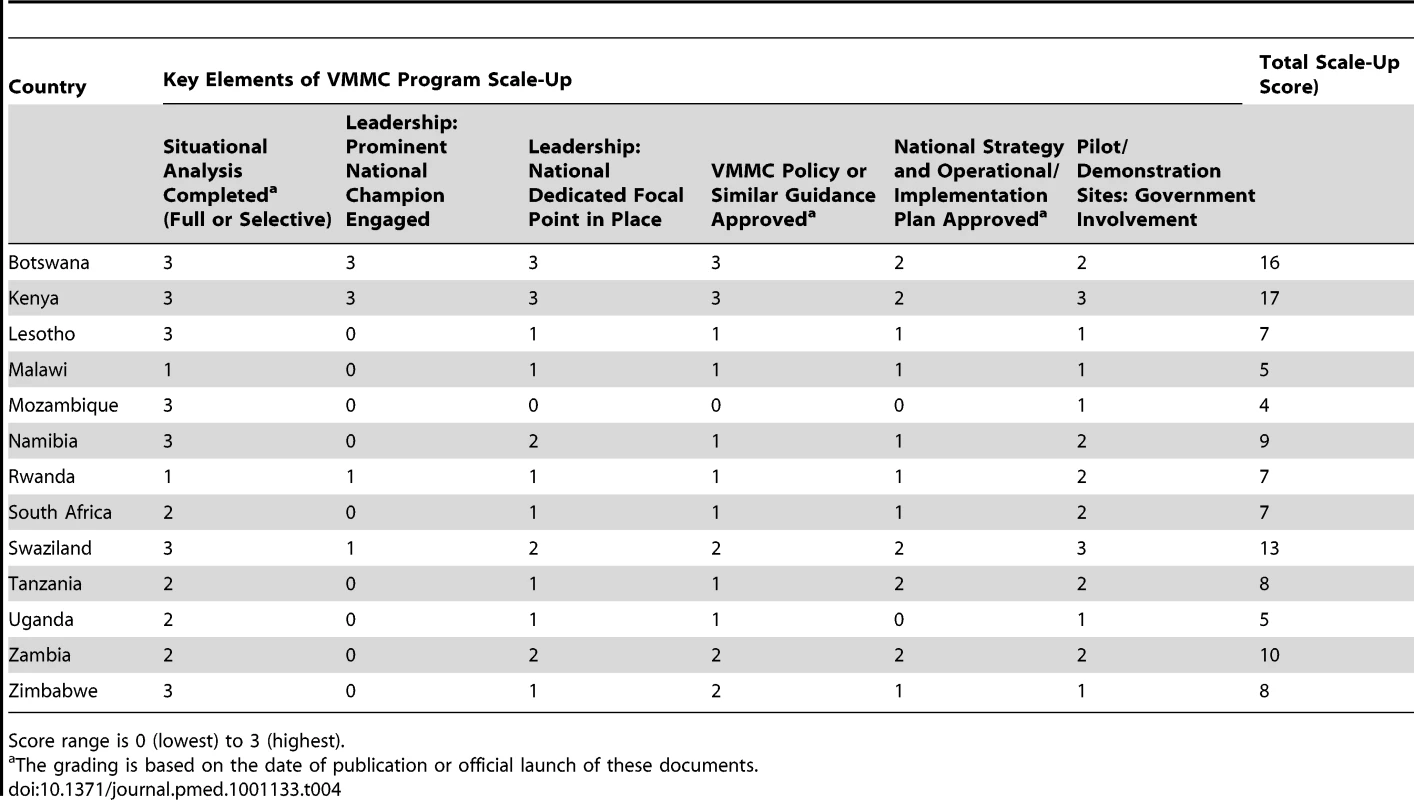
Score range is 0 (lowest) to 3 (highest). Specific examples of how the “user organization,” “resource team,” scaling-up strategy, and environment influenced scale-up are highlighted in Box 1. The type of policy document developed varies by country: some countries have stand-alone policy documents, while others have VMMC incorporated into other HIV prevention policies. Governments have been engaged in the setting up of pilot sites to test the feasibility of scale-up in all countries.
Box 1. ExpandNet VMMC Components
User organization: the organizations and programs adopting the innovation
-
National Ministries of Health in all 13 priority countries have taken ownership and are leading the roll out in most countries.
-
All countries have coordination structures (VMMC task forces) that are functioning to varying degrees. These task forces are partnerships between the Ministries of Health and the implementing partners. Kenya and South Africa also have provincial task forces.
-
Human resource constraints—lack of personnel at national and facility level.
Environment: the social, cultural, political, and economic context within which scaling up takes place
-
Notable political champions in Botswana and Kenya. Political changes in Botswana and South Africa affected initial trajectories both negatively and positively.
-
Gaining political support – it has been a process to get political buy-in in some countries
-
Global and national advocacy has moved some “early adopter” countries; peer pressure is working to bring the “late majority” on board. Preparatory stakeholders meetings were held in 2006 in five countries (Lesotho, Kenya, Tanzania, Swaziland, and Zambia) before the release of the WHO/UNAIDS recommendations. Regional consultations were held and national stakeholders meetings held in all countries after the release of the recommendations.
-
Cultural context: issue raised of conflation with female genital mutilation (which occurs in some parts of Kenya and Uganda). In Lesotho, Malawi, and South Africa, cultural issues have been a challenge—the role of traditional providers has caused much debate and tensions. Lack of traditional male circumcision in Swaziland facilitated adoption.
-
Legal issues: few countries have laws governing practice of traditional circumcisers. Task shifting, while successful in Kenya, is a challenge in other countries.
Resource team: those involved in the development and testing of the innovation and/or seeking to promote its wider use
-
Developing countries look to WHO to provide norms and standards, therefore the timely release of the WHO/UNAIDS recommendations provided guidance for national policy and strategy development.
-
The recommendations address the sociocultural, gender, and human rights issues that countries need to consider as well as health service issues, and therefore provide a comprehensive framework for policy development.
-
The UN provided tools and guidance for scale-up, including operations guidance, legal regulatory tool, clinical manual for practice, and training, quality assurance, monitoring, and evaluation.
-
Funding from donor organizations was made available and coordinated to enhance capacity of Ministries of Health and provider organizations in country.
-
Partners in countries available to provide technical support for scale-up.
-
Coordinated international leadership and advocacy supported country action.
-
Strong partnerships between governments and non-governmental organizations have facilitated program scale-up in Kenya and, recently, Tanzania.
Scaling up strategy: the means by which the innovation is communicated, disseminated, transferred, or otherwise promoted
-
Policy development was diverse across countries with differing types of policy instruments, e.g., Botswana has no separate policy but strategy with policy elements; Zambia sent Information note to Cabinet; Kenya developed policy guidelines; dedicated policies were developed in Lesotho, Namibia, South Africa, Swaziland, Uganda, and Zimbabwe.
-
Country strategies developed that include objectives, target population, numbers of men to be reached, costs, service delivery strategies, resource mobilization, monitoring, and evaluation.
-
DMPPT used to estimate cost, impact, pace of scale-up, and to develop or revise strategies.
-
Different scale-up strategies have influenced program implementation. Most countries have “catch-up” strategies to reach adult men—Kenya, Swaziland, Zimbabwe, Zambia—however, implementation varies; Kenya has gone ahead with focused campaigns to achieve numbers, while Botswana is focusing on integrated service delivery.
-
Demand creation—matching services to demand is difficult.
-
Communicating partial protection and risk compensation are challenging.
Discussion
We found that the DOI theory was most useful in analyzing the adoption and initial implementation of VMMC programs, while the ExpandNet theory helped to explore the factors that have facilitated or hindered scale-up. The analysis shows that although progress in VMMC program implementation has been made in all 13 countries within the first 3 y of the release of the WHO/UNAIDS recommendations, much more needs to be done if countries are to take programs to scale and achieve their targets of circumcising 80% of eligible men by 2015. The innovator country, Kenya, and the early adopters (South Africa, Zambia, and Swaziland) initiated VMMC program implementation soon after the release of the recommendations by adopting national policies and strategies and starting to perform VMMCs as part of pilot programs in 2008. However, only Kenya appears to be on track to achieving 80% coverage by 2015. To date, VMMC programs in priority countries have reached only approximately 3% of the target coverage level of 80% of eligible African men proposed by Njeuhmeli et al. [22]. Clearly an accelerated pace of VMMC service delivery is needed to take programs to scale and to maximize the impact of the programs.
Although the rate of adoption of VMMC programs varies among the 13 priority countries, the initiation of program adoption and initial implementation as a whole have been carried out relatively quickly compared to other public health interventions. Although there is much more research and scientific discovery now than ever before, the uptake of innovations does not seem to be much faster than it was 100 y ago. A review of nine landmark clinical procedures suggested that, on average, it takes a minimum of 6.3 y for research evidence to reach reviews, papers, and text books. They estimated that a further 9.3-y transition period is needed to implement the evidence from scientific publications [28]. ExpandNet case studies of scaling up reproductive health interventions indicate that about 10 y is required to scale up from pilot testing to nationwide expansion [25],[29]. Whereas in the case of VMMC, within 4 mo of the results of the three RCTs being released (in December 2006), WHO/UNAIDS had endorsed VMMC as a safe and effective means of HIV prevention and published recommendations for the implementation and scale-up of VMMC programs [19]. Less than a year later, pilot programs were initiated in the priority countries. Within 3 y of the release of the WHO/UNAIDS recommendations, the majority of the 13 priority countries had established national policies/strategies for HIV prevention that included VMMC and had begun to initiate service delivery. However, although the uptake of VMMC RCT evidence was relatively quick, it took almost two decades from the first cohort data [30] to the RCT meta-analysis, and implementation research is still insufficient.
Potential predictors of innovation and early adoption of the VMMC programs identified by this analysis include having a VMMC focal person, establishing a national policy, and having an operational strategy, as well as having a pilot or demonstration site with government involvement. These are important elements in confirming country ownership of the program. To create an environment for increasing country ownership and country-to-country learning, preparatory multi-stakeholder meetings were held in Kenya, Lesotho, Swaziland, Tanzania, and Zambia in 2006 [31]–[36]. Apart from Lesotho, all the other countries that held early stakeholder consultations are classified within the early majority, possibly also highlighting the significant role of the environment.
The DOI and the ExpandNet frameworks both postulate that the sociopolitical context and cultural relevance of an innovation are also critical factors influencing the widespread adoption of an innovation. The DOI theory also emphasizes that opinion leaders directly affect the adoption of an innovation; this explains why some innovations are quickly adopted in one setting but fail to take off in others. It is therefore interesting to note that from our analysis, the role of having a national champion engaged early on in the process does not appear to be a predictor of adoption status. However, despite the low association scores that having a national champion was shown to have in this analysis, we also know from our program implementation experience that former Botswana President Festus Mogae and Kenya's Prime Minister Raila Odinga were prominent leaders that championed VMMC programs in their respective countries [37]. In addition, in 2009, South Africa acquired a government that prioritized the strengthening of HIV programs, and on World AIDS Day in December 2009, the new president of South Africa publicly announced the government's determination to move the AIDS agenda forward, saying, “Let the politicization and endless debates about HIV and AIDS stop” and, regarding the need to struggle against AIDS as they had done with apartheid, “We have no choice but to deploy every effort, mobilize every resource, and utilize every skill our nation possesses.” [38],[39] This commitment at the highest level undoubtedly contributed to the significant number of VMMCs (131,117) performed in South Africa in 2010. Botswana had strong political support from their former President Festus Mogae; however, his presidency ended at the end of March 2008. This may explain why Bostwana has reached only 3.2% of its 2015 DMPPT target despite strong momentum in the initial phases.
In Kenya, consistent political support and ongoing community consultation have allowed implementation challenges to be addressed as they arise [40]. Kenya established a national VMMC task force that engaged all the key partners and was replicated at the provincial level. In addition, in 2007, Kenya initiated community mobilization activities that engaged community leaders and other key stakeholders in VMMC program implementation and generated the demand for services. These activities helped to overcome some of the initial political and cultural tensions and to accelerate service delivery [41] This further highlights the importance of the sociopolitical context and environment as well as sustained leadership at all levels (described in the ExpandNet framework) for moving `programs from initial adoption to scale-up. As suggested by the results of this study, it might therefore be that the consistency of political support and leadership, at all levels, is more important than just the initial engagement. This is due to the fact that while adoption is a one-time event, the scaling up of an innovation such as VMMC is an iterative process carried out over an extended period of time that requires continued political support and, in many instances, the input of decision makers to resolve implementation challenges as they arise. This ongoing need for political support and the involvement of decision makers is highlighted in the Kenya experience. An evaluation of the first year of VMMC program implementation in Kenya provides insights into some of the challenges of the Kenya program, including human resource constraints, inadequate infrastructure, and shortages of equipment and supplies, as well as difficulties with data management [40]. Despite challenges, the innovative responses that the Kenya Ministry of Health implemented in collaboration with other partners facilitated the translation of the national policies and programs into service delivery. Program managers facing shortages in human resources and inadequate infrastructure would not, without strong political support, be able to address these implementation challenges to the scale-up of an innovation.
While this analysis has not focused on the differences between country strategies for VMMC scale-up, the choice of strategy undoubtedly had an impact on VMMC program implementation and subsequent scale-up. For example, the scale-up strategy of Botswana has differed from that of other countries that acknowledge the need for a phase of vertical programs—the “catch-up” phase—to rapidly expand access to safe VMMC services in addition to a strategy for integration [19]. The Botswana strategy has focused on the integration of VMMC within existing health services; this is perhaps a reflection of the country's experience with scaling up ART. This may explain why Botswana has not performed as many VMMCs as the early adopter countries even though it had a VMMC focal person, policy, and strategy early on in the process. The timing of when countries conducted a situation analysis does not appear to have a bearing on the process of adoption of VMMC programs. However, for this analysis we did not take into account the type of situation analysis that was conducted or the process for dissemination and utilization of the situation analysis findings.
This analysis is not intended to criticize progress in any particular country; rather, it is an attempt to identify elements critical to success and underscore some of the challenges to scale-up. While medical male circumcision has many of the “CORRECT” characteristics, it is difficult to scale up the intervention, particularly as a result of human resources limitations in terms of both quantity and quality [42]. Also challenging are logistics and supply management: successful scale-up will in part depend on the definition and accessibility of commodities essential for VMMC programming and the appropriate allocation of resources to support commodity procurement and supply chain logistics [43].
This study suggests that the adoption of a health services innovation—the development of national policies and strategies, and the initiation of pilot programs—and program scale-up are distinct processes. This is clearly illustrated by the limited progress made towards scale-up by the early adopter countries. Thus, although the DOI theory was useful for predicting the adoption of VMMC as an innovation for HIV prevention, it was less useful as a model to describe what is actually needed to scale up VMMC services. The ExpandNet framework helps to provide some insights into the critical components required for scale-up.
Limitations
The VMMC scale-up process has not been well documented in countries and therefore data were obtained from limited sources. The total scale-up score has not been used or validated in other programs and is reliant on assessments by a number of key informants who have been closely involved in VMMC scale-up at global and national levels. These individuals were interviewed and the information triangulated in an attempt to limit the potential bias. We limited our predictors of adoption status to the elements defined in the WHO/UNAIDS operational guidance, and yet there may be other important program elements that are not well captured in the guidance. We have attempted to draw out some of these other factors in the discussion but recognize that there may be other elements of program adoption that are not easily quantifiable.
Although the scores have captured the time when the different milestones were recorded and published, these only indirectly reflect the timing and pace of scale-up. The date of publication may have been several months after the work was initiated and/or completed, so the impact of the element may have been realized. The number of male circumcisions performed in priority countries may be underestimated as the data largely reflects male circumcisions done through programs funded by the United States President's Emergency Plan for AIDS Relief (PEPFAR). However, in many of the priority countries, initial male circumcision sites have been set up by PEPFAR implementing partners working closely with government. Finally, the quantitative analyses included in this study were based on a total sample of 13 countries. As such, although the results are indicative of experiences of these specific countries, the ability to generalize these findings to other contexts is limited.
Conclusion
Three years after the WHO/UNAIDS recommendations to expand, promote, and integrate VMMC into comprehensive HIV prevention packages, VMMC has been adopted as a national HIV prevention strategy and implementation has been initiated in all of the priority countries. Policies, national scale-up strategies, and pilot projects have been put in place, and by the end of 2010, approximately 559,528 VMMCs had been performed in the priority countries, and yet this represents only about 3% of what is needed to achieve country-derived targets. The variability in progress in scale-up of male circumcision is evident, and the two diffusion frameworks suggest that the adoption of VMMC as a HIV prevention innovation does not guarantee scale-up. A key lesson is the importance of not only being ready to adopt a new intervention but also ensuring that those factors that accelerate and sustain program implementation are built and maintained. The most successful national program exhibited country ownership and sustained leadership at all levels, in addition to the adoption of a national policy and strategy to translate the research into a viable program.
Zdroje
1. Joint United Nations Programme on HIV/AIDS 2010 Global report: UNAIDS report on global AIDS epidemic 2010. Geneva Joint United Nations Programme on HIV/AIDS
2. WellerSDavis-BeatyK 2002 Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Rev 2002 CD003255
3. DeCockKFowlerMMercierEdeVincenziISabaJ 2000 Prevention of mother-to-child HIV transmission in resource-poor countries: translating research into policy practice. JAMA 9 1175 1182
4. World Health Organization 2010 Antiretroviral drugs for treating pregnant women and preventing HIV infection in infants: recommendations for a public health approach—2010 version. Geneva World Health Organization
5. World Health Organization 2009 WHO, UNODC, UNAIDS technical guide for countries to set targets for universal access to HIV prevention, treatment and care for injecting drug users. Geneva World Health Organization
6. StoverK 2011 May 12 Treating HIV-infected people with antiretrovirals significantly reduces transmission to partners: findings result from NIH-funded international study. NIH News. Bethesda (Maryland) United States National Institutes of Health
7. PetersAJansenWvan DrielF 2010 The female condom: the international denial of a strong potential. Reprod Health Matters 18 119 128
8. AuvertBTaljaardDLagardeE 2005 Randomized controlled intervention trial of male circumcision for reduction of HIV infection risk: The ANRS 1265 trial. PLoS Med 2 e298 doi:10.1371/journal.pmed.0020298
9. GrayRHKogoziGSerwaddaDMakumbiFWatyaS 2007 Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet 369 657 666
10. BaileyRMosesSParkerC 2007 Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet 643 656
11. WeissHQuigleyMHayesR 2000 Male circumcision and risk of HIV infection in sub-Saharan Africa: a systematic review and meta-analysis. AIDS 14 2361 2370
12. TobianASerwaddaDQuinnTKigoziGGravittP 2009 Male circumcision for the prevention of HSV-2 and HPV infections and syphilis. New Engl J Med 13 1298 1309
13. AuvertBSobngwi-TambekouJCutlerENieuwoudtMLissoubaP 2009 Effect of male circumcision on the prevalence of high-risk human papillomavirus in young men: results of a randomized controlled trial conducted in Orange Farm, South Africa. J Infect Dis 199 14 19
14. GrayRSerwaddaDKongXMakumbiFKigoziG 2010 Male circumcision decreases acquisition and increases clearance of high-risk human papillomavirus in HIV-negative men: a randomized trial in Rakai, Uganda. J Infect Dis 201 1455 1462
15. SerwaddaDWawerMMakumbiFKongXKigoziG 2010 Circumcision of HIV-infected men: effects on high-risk human papillomavirus infections in a randomized trial in Rakai, Uganda. J Infect Dis 201 1463 1469
16. WawerMTobianAKigoziGKongXGravittP 2011 Effect of circumcision of HIV-negative women: a randomised trial in Rakai, Uganda. Lancet 377 209 218
17. WawerMMakumbiFKigoziGSerwaddaDWatyaS 2009 Circumcision in HIV-infected men and its effect on HIV transmission to female partners in Rakai, Uganda. Lancet 374 229 237
18. WeissHHankinsCDicksonK 2009 Male circumcision and risk of HIV infection in women: a systematic review and meta-analysis. Lancet Infect Dis 9 669 677
19. World Health Organization/Joint United Nations Programme on HIV/AIDS 2007 WHO/UNAIDS technical consultation on male circumcision and HIV prevention: research implications for policy and programming. Conclusions and recommendations. Geneva World Health Organization
20. World Health Organization/Joint United Nations Programme on HIV/AIDS 2008 Operational guidance for scaling up male circumcision services for HIV prevention. Geneva World Health Organization
21. UNAIDS/WHO/SACEMA Expert Group on Modelling the Impact and Cost of Male Circumcision for HIV Prevention 2009 Male circumcision for HIV prevention in high HIV prevalence settings: what mathematical models contribute to informed decision making. PLoS Med 9 doi:10.1371/journal.pmed.1000109 e:1000109
22. NjeuhmeliEForsytheSReedJOpuniMBollingerL 2011 Voluntary medical male circumcision: modeling the impact and cost of expanding male circumcision for HIV prevention in eastern and southern Africa. PLoS Med 8 e1001132 doi:10.1371/journal.pmed.1001132
23. GlaserEAbelsonHGarrisonK 1983 Putting knowledge to use: facilitating the diffusion of knowledge and the implementation of planned change. San Francisco Jossey-Bass
24. RogersE 1995 Diffusion of innovations, 4th ed. New York Free Press
25. SimmonsRFajansPGhironL 2007 Scaling up health service delivery: from pilot innovations to policies and programmes. Geneva World Health Organization
26. BollingerLStoverJ 2009 The potential cost and impact of expanding male circumcision in 14 countries. Geneva World Health Organization
27. World Health Organization 2009 Male circumcision: situation analysis toolkit. Geneva World Health Organization
28. BalasEBorenS 2000 Managing clinical knowledge for health care improvement. BemmelJMcCrayA Yearbook of medical informatics Stuttgart Schattauer Publishing 65 70
29. World Health Organization 2009 Practical guidance for scaling up health service innovations. Geneva World Health Organization
30. HalperinDTBaileyRC 1999 Male circumcision and HIV infection: 10 years and counting. Lancet 354 1813 1815
31. MuulaAS 2006 On evidence in support of male circumcision in HIV prevention: what next? PLoS Med 3 e66 doi:10.1371/journal.pmed.0030066
32. Joint United Nations Programme on HIV/AIDS 2006 Report on the male circumcision and HIV prevention country consultation meeting. Geneva Joint United Nations Programme on HIV/AIDS Esibayeni Lodge, Matsapha. 26-27 September 2006
33. Joint United Nations Programme on HIV/AIDS 2006 Male circumcision and HIV prevention: Tanzania country stakeholder consultation. Geneva Joint United Nations Programme on HIV/AIDS Dar es Salaam Protea Hotel. 14-15 September 2006
34. Joint United Nations Programme on HIV/AIDS 2006 Male circumcision consultative meeting report. Geneva Joint United Nations Programme on HIV/AIDS Protea in Lusaka, Zambia. 11-12 September 2006
35. Joint United Nations Programme on HIV/AIDS 2006 Kenya stakeholder consultation on male circumcision in the context of HIV prevention. Geneva Joint United Nations Programme on HIV/AIDS Mayfair Holiday Inn, Nairobi, Kenya. 7-8 September 2006
36. Joint United Nations Programme on HIV/AIDS 2006 Male circumcision and HIV prevention: Lesotho country consultation meeting report. Geneva Joint United Nations Programme on HIV/AIDS Lesotho Sun Hotel, Lesotho. 25 July 2006
37. DicksonK 2010 Male circumcision for HIV prevention: progress in scale-up [presentation]. 17th Conference on Retroviruses and Opportunistic Infections; San Francisco, California; 16–19 February 2010
38. DuggerCW 2009 December 2 Breaking with past, South Africa issues broad AIDS policy. The New York Times A6
39. SmithD 2009 December 1 South Africa's Jacob Zuma promises to take HIV test in AIDS policy reversal. The Guardian 16
40. National AIDS and STI Control Programme 2010 Progress report on Kenya's voluntary medical male circumcision programme, 2008-09: summary. Nairobi Government of Kenya, Ministry of Public Health and Sanitation, National AIDS and STI Control Programme
41. Herman-RoloffALlewellynEObieroWAgotKNdinya-AcholaJ 2011 Implementing voluntary medical male circumcision for HIV prevention in Nyanza Province, Kenya: lessons learned during the first year. PLoS ONE 6 e18299 doi:10.1371/journal.pone.0018299
42. CurranKNjeuhmeliEMirelmanADicksonKAdamuT 2011 Voluntary medical male circumcision: strategies for meeting the human resource needs of scale-up in southern and eastern Africa. PLoS Med 8 e1001129 doi:10.1371/journal.pmed.1001129
43. EdgilDStankardPSForsytheSReedJRechD 2011 Voluntary medical male circumcision: logistics, commodities, and waste management requirements for scale-up of services. PLoS Med 8 e1001128 doi:10.1371/journal.pmed.1001128
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2011 Číslo 11- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
-
Všechny články tohoto čísla
- Voluntary Medical Male Circumcision: Strategies for Meeting the Human Resource Needs of Scale-Up in Southern and Eastern Africa
- Voluntary Medical Male Circumcision: Translating Research into the Rapid Expansion of Services in Kenya, 2008–2011
- Quality of Maternal Health Care: A Call for Papers for a Maternal Health Task Force–PLoS Collection
- Voluntary Medical Male Circumcision: Matching Demand and Supply with Quality and Efficiency in a High-Volume Campaign in Iringa Region, Tanzania
- Priorities for Research on Equity and Health: Towards an Equity-Focused Health Research Agenda
- What Research Is Needed to Stop TB? Introducing the
- Responsible Governance for Mental Health Research in Low Resource Countries
- Voluntary Medical Male Circumcision: Modeling the Impact and Cost of Expanding Male Circumcision for HIV Prevention in Eastern and Southern Africa
- Effect of Supplementation with Zinc and Other Micronutrients on Malaria in Tanzanian Children: A Randomised Trial
- HIV, Gender, Race, Sexual Orientation, and Sex Work: A Qualitative Study of Intersectional Stigma Experienced by HIV-Positive Women in Ontario, Canada
- Voluntary Medical Male Circumcision: A Framework Analysis of Policy and Program Implementation in Eastern and Southern Africa
- Voluntary Medical Male Circumcision: Logistics, Commodities, and Waste Management Requirements for Scale-Up of Services
- Optimal Uses of Antiretrovirals for Prevention in HIV-1 Serodiscordant Heterosexual Couples in South Africa: A Modelling Study
- Managing the Demand for Global Health Education
- Post-neonatal Mortality, Morbidity, and Developmental Outcome after Ultrasound-Dated Preterm Birth in Rural Malawi: A Community-Based Cohort Study
- Voluntary Medical Male Circumcision: An Introduction to the Cost, Impact, and Challenges of Accelerated Scaling Up
- On the Futility of Screening for Genes That Make You Fat
- Rapid Diagnosis of Tuberculosis with the Xpert MTB/RIF Assay in High Burden Countries: A Cost-Effectiveness Analysis
- Physical Activity Attenuates the Influence of Variants on Obesity Risk: A Meta-Analysis of 218,166 Adults and 19,268 Children
- A Head-to-Head Comparison of Four Artemisinin-Based Combinations for Treating Uncomplicated Malaria in African Children: A Randomized Trial
- Evidence-Based Guidelines for Mental, Neurological, and Substance Use Disorders in Low- and Middle-Income Countries: Summary of WHO Recommendations
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Evidence-Based Guidelines for Mental, Neurological, and Substance Use Disorders in Low- and Middle-Income Countries: Summary of WHO Recommendations
- Voluntary Medical Male Circumcision: Strategies for Meeting the Human Resource Needs of Scale-Up in Southern and Eastern Africa
- Rapid Diagnosis of Tuberculosis with the Xpert MTB/RIF Assay in High Burden Countries: A Cost-Effectiveness Analysis
- Physical Activity Attenuates the Influence of Variants on Obesity Risk: A Meta-Analysis of 218,166 Adults and 19,268 Children
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



