-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
A 58-Year-Old Woman with Abdominal Symptoms and Elevated C-Reactive Protein
article has not abstract
Published in the journal: . PLoS Med 5(7): e149. doi:10.1371/journal.pmed.0050149
Category: Learning Forum
doi: https://doi.org/10.1371/journal.pmed.0050149Summary
article has not abstract
Description of Case
A 58-year-old woman presented to her primary care physician in April 2002 complaining of troubling abdominal symptoms. She described abdominal bloating and pain with frequent diarrhoea and modest weight loss. There was no history of fevers or rigors. She had a background of irritable bowel syndrome, monoclonal gammopathy of uncertain significance (MGUS), ureteric stones, hysterectomy, and fracture of her left tibia and fibula. Investigations for possible inflammatory bowel disease in the 1980s had been negative. Investigations revealed normal electrolytes, renal function coeliac screen, and full blood count, but raised rheumatoid factor, an erythrocyte sedimentation rate of 26 mm/hr, and a C-reactive protein (CRP) level of more than 250 mg/l (Addenbrooke's Hospital does not quantify CRP at levels of more than 250 mg/l). Because of the raised inflammatory markers, she was referred for further evaluation to the infectious diseases clinic at Addenbrooke's Hospital.
The patient's case was reviewed in the infectious diseases clinic in July 2002. A course of sulfasalazine for presumed inflammatory bowel disease had been commenced by her primary care physician, but had been stopped due to lack of efficacy. Examination of the patient was entirely unremarkable.
At This Stage, What Was Our Differential Diagnosis?
Given her symptoms and raised inflammatory markers, inflammatory, infectious, and malignant processes were all considered in the initial differential diagnosis. However, given the preponderance of abdominal symptoms, a diagnosis of inflammatory bowel disease was thought to be most likely. A gallium scan was arranged to investigate this possibility. The result showed non-specific uptake in the right iliac fossa, and was reported as consistent with inactivated or treated Crohn's disease rather than active inflammatory bowel disease. By March 2003, the patient reported ongoing symptoms of bloating, abdominal pain, and watery diarrhoea. Weight loss had ceased, but her CRP remained highly elevated. As inflammatory bowel disease remained our main differential, she was referred to gastroenterology for colonoscopy, with biopsies taken of the ascending colon and terminal ileum. Colonoscopic as well as histological examination of the patient's bowel was completely normal. In September 2003, the patient developed pain over her left sacro-iliac joint.
What Was the New Differential Diagnosis?
Raised inflammatory markers with sacro-iliac pain suggested sacro-iliitis, and would be consistent with past or present inflammatory bowel disease. Infectious and inflammatory causes are the most common; blood cultures and early morning urine specimens were sought, but failed to grow mycobacteria or other pathogens. Plain radiographs of the lumbo-sacral spine revealed no evidence of sacro-iliitis or fracture. Given the ongoing abdominal symptoms, imaging of the abdomen with ultra-sound was arranged to allow investigation of abscesses or masses. This showed mild fatty infiltration of the liver and a probable angiomyolipoma in the lower pole of the right kidney.
Is MGUS Entirely Benign? Could It Account for the Patient's Condition?
Re-assessment of the patient in clinic in August 2004 outlined the patient's main problems as: (1) raised CRP of unknown aetiology, (2) back pain, and (3) MGUS. Given that MGUS can progress to multiple myeloma, and in view of the back pain, a formal diagnosis of multiple myeloma needed to be excluded. Urinary Bence-Jones proteins were negative, and serum electrophoresis again confirmed normal levels of immunoglobulin G (IgG) and IgA, with a monoclonal band in IgM of 5 g/l, unchanged since the initial diagnosis of MGUS in 1999. A haematology opinion was sought, and the patient was re-assured that her MGUS was stable, and unlikely to be the cause of her raised inflammatory markers.
What Potential Diagnoses Remained?
By November 2004, the patient remained without a diagnosis, more than 30 months after initial presentation. Echocardiogram of the heart to exclude atrial myxoma was normal. A computerized tomography scan of the abdomen and pelvis was arranged to look for occult abscess or malignancy. A rheumatology review suggested diagnoses of early rheumatoid arthritis and amyloidosis. Plain radiographs of the hands and feet were normal, and the previous colonic biopsies were re-examined for evidence of amyloid deposition by Congo red staining, but were normal. It was at further review at the infectious diseases clinic in April 2005 that it was suggested that the elevated CRP measurements might be due to interference in the biochemical assay. By that time, the patient had had eight alternative diagnoses considered (Table 1), and had been investigated for three years.
Tab. 1. Potential Differential Diagnoses Considered to Explain Elevated CRP 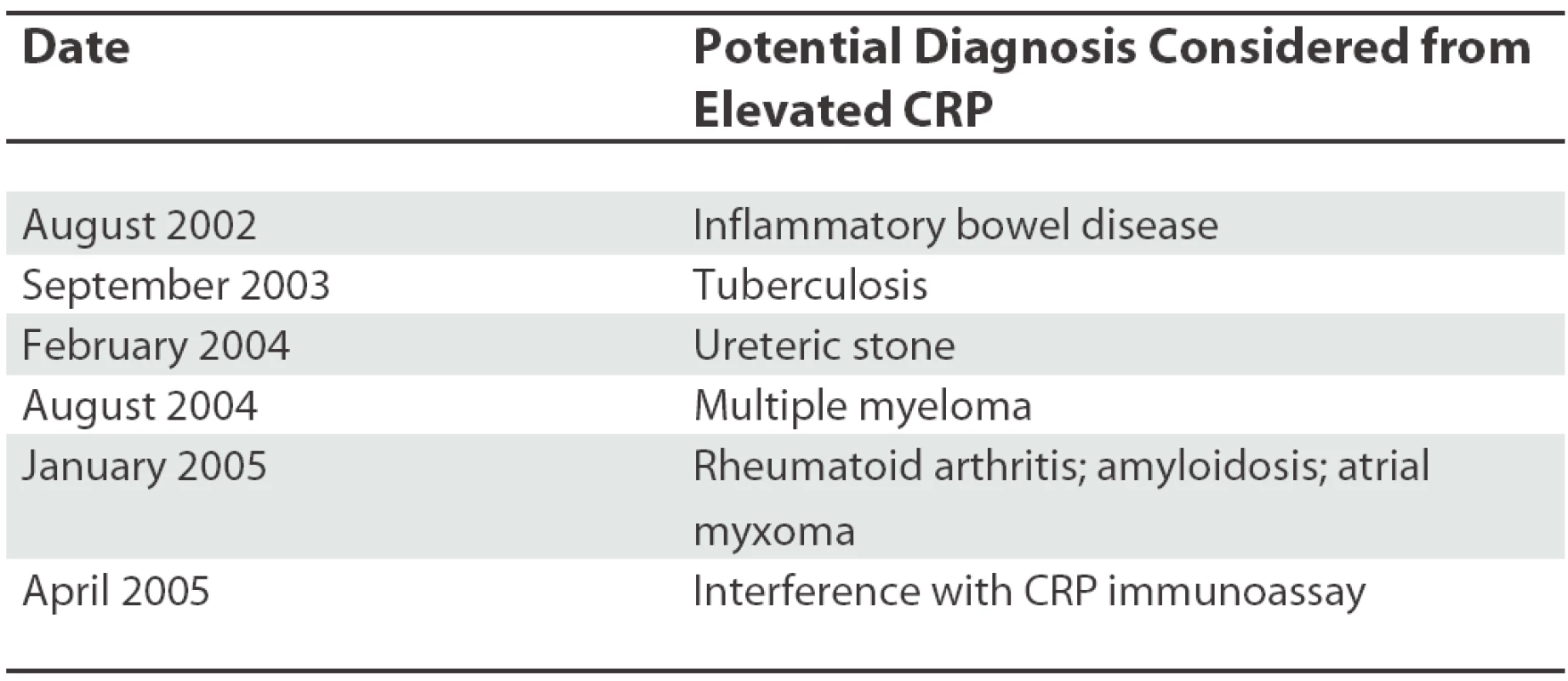
The biochemistry department confirmed that there was indeed interference in the CRP assay due to the patient's monoclonal gammopathy. This was determined on the basis of three observations: (1) removal of high molecular species by polyethylene glycol removed the interference; (2) the “interferent” in the patient's serum mobilised in the same fraction as her monoclonal band; and (3) interference by the patient's serum was also detected in the laboratory's phenytoin assay (see below). Since the weight loss and abdominal pain had ceased, and the patient's only remaining symptom was mild back pain, the patient was re-assured, and discharged from further follow-up.
Discussion
CRP is a cyclic-pentamer acute-phase protein synthesised rapidly in the liver in response to inflammatory stimuli, especially interleukin-6. The subunits of CRP bind to a range of biologically significant ligands, causing activation of the complement cascade via the classical pathway. Measures of CRP are useful for the detection and assessment of infection, tissue injury, and inflammatory diseases [1]. The majority of routine methods for the detection of CRP use the principle of turbidimetry. Less light is able to pass through a turbid (cloudy) sample than a clear sample, and turbidimetry is the measure of this difference. The sensitivity of turbidimetric assays can be increased by using particle-enhanced turbidimetric immunoassays (PETIAs). Latex particles, coated with anti-CRP monoclonal antibodies, bind CRP and agglutinate resulting in increased sample turbidity. The decrease in transmitted light is proportional to the CRP concentration. Paraprotein-induced latex particle agglutination also causes increased sample turbidity, and hence a false increase in the measured CRP concentration (Figure 1). This interference could be specific (i.e., limited to measurement of CRP only) or non-specific. In this case, the patient's IgM paraprotein also interfered with measurement of phenytoin, but not phenobarbitone levels (both of which use a particle-enhanced turbidimetric inhibition assay, or PETINIA). No other assays in the Addenbrooke's laboratory used a PETIA or PETINIA, so interference against other immunoassays was not determined.
Fig. 1. Schematic Illustrating One Possible Mechanism of How Antibody Interferes with PETIAs 
(A) In PETIAs, latex particles coated with antibody against CRP bind specifically to the target. This increases the turbidity of the sample, resulting in a decreased transmission of light, which reads as an increased concentration of CRP. (B) In interference by, e.g., monoclonal antibody, the antibody binds the anti-CRP-coated beads, increasing turbidity and leading to falsely elevated readings of CRP concentration. Key Learning Points
-
Interference in immunoassays is a rare, but often underestimated problem.
-
Common tests using immunoassays are endocrine tests, cardiac biomarkers (e.g., troponin), serum proteins, (e.g., CRP and ferritin), and tumour markers (e.g., carcinoembryonic antigen and prostate-specific antigen).
-
Immunoassay interference should be suspected when results of an investigation are either clinically unexpected or inconsistent with other test results.
-
Immunoassay interference cannot be detected by routine laboratory quality assurance measures, and liaison with the laboratory is essential in making the diagnosis.
-
Although it is routine for “diagnostic conundrums” to be referred to the infectious diseases clinic, referrals on the basis of single abnormal blood test results should prompt clinicians to consider false positives.
Immunoassay interference is rare, with a quoted incidence of 0.05% to 2%, but is probably underestimated [2]. In one large prospective study of over 5,000 patients, the incidence of interference in a thyroid stimulating hormone immunoassay with potentially adverse clinical effect was 0.4% [3]. Although interference of CRP immunoassays by both polyclonal and monoclonal antibodies has been described in the clinical chemistry literature [4–7], this phenomenon is less appreciated in the general medical community [8]. Interference with immunoassays have previously led to extensive and sometimes invasive investigation of patients [3,9]. In our patient, at least eight definitive diagnoses were considered as part of her investigation in the out-patient department over a course of two years (Table 1), and she underwent numerous tests including endoscopy and multiple radiological investigations. In cases of patients with persistently elevated CRP levels, or other markers measured by immunoassay, outside of the clinical context, the possibility of interference from paraproteins or other endogenous antibodies should be considered.
Zdroje
1. PepysMBBaltzML
1983
Acute phase proteins with special reference to C-reactive protein and related proteins (pentaxins) and serum amyloid A protein.
Adv Immunol
34
141
212
2. IsmailAAWalkerPLCawoodMLBarthJH
2002
Interference in immunoassay is an underestimated problem.
Ann Clin Biochem
39
366
373
3. IsmailAAWalkerPLBarthJHLewandowskiKCJonesR
2002
Wrong biochemistry results: Two case reports and observational study in 5310 patients on potentially misleading thyroid-stimulating hormone and gonadotropin immunoassay results.
Clin Chem
48
2023
2029
4. HamwiAFodingerMSunder-PlassmannGHorlWHVukovichTC
1997
Disturbed latex immunoassays for C-reactive protein and ferritin in a renal transplant patient due to polyclonal IgM hypergammaglobulinaemia.
Nephrol Dial Transplant
12
1229
1233
5. MullerWMierauRWohltmannD
1985
Interference of IgM rheumatoid factor with nephelometric C-reactive protein determinations.
J Immunol Methods
80
77
90
6. OhtakeTKanoSWatanabeK
2000
[Interference in turbidimetric immunoassay for serum C-reactive protein due to serum protein abnormalities an immune complex and rheumatoid factor]. [Article in Japanese].
Rinsho Byori
48
752
759
7. YamadaKYagihashiAIshiiSTanemuraKKidaT
1997
Interference with nephelometric assay of C-reactive protein and antistreptolysin-O by monoclonal IgM-kappa from a myeloma patient.
Clin Chem
43
2435
2437
8. IsmailYIsmailAAIsmailAAA
2007
Erroneous laboratory results: What clinicians need to know.
Clin Med
7
357
361
9. MakaryusANMakaryusMNHassidB
2007
Falsely elevated cardiac troponin I levels.
Clin Cardiol
30
92
94
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2008 Číslo 7- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
-
Všechny články tohoto čísla
- International Funding for Malaria Control in Relation to Populations at Risk of Stable Transmission
- Immunological Outcomes of New Tuberculosis Vaccine Trials: WHO Panel Recommendations
- A 58-Year-Old Woman with Abdominal Symptoms and Elevated C-Reactive Protein
- Organophosphate Poisoning–Induced Intermediate Syndrome: Can Electrophysiological Changes Help Predict Outcome?
- Evidence-Based Tuberculosis Diagnosis
- Divergent Goals and Commitments in Global Malaria Intervention
- Next Stop, Don't Block the Doors: Opening Up Access to Clinical Trials Results
- The Effects of International Monetary Fund Loans on Health Outcomes
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Evidence-Based Tuberculosis Diagnosis
- Organophosphate Poisoning–Induced Intermediate Syndrome: Can Electrophysiological Changes Help Predict Outcome?
- The Effects of International Monetary Fund Loans on Health Outcomes
- Next Stop, Don't Block the Doors: Opening Up Access to Clinical Trials Results
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



