-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Reccurent Erythema Migrans as a Persistent Infection
Reccurent Erythema Migrans as a Persistent Infection
Background.
Effective antibiotic therapy administered early in the course of the clinical presentation of erythema migrans (EM) prevents further progression of infection and dissemination of the agent to internal organs.Case report.
A 73-year old woman was referred with a history of five episodes of recurrent EM after repeated adequate antibiotic treatment. The patient who had visited an endemic area only once before the disease recalled no tick bite either prior to the first episode or later. After the first episode, the serological examination was negative (IFA, ELISA, Western blot). In the second episode, not preceded by her visit to any endemic area, the patient showed borderline positivity. Western blot confirmed Borrelia burgdorferi sensu lato. The following episodes were observed again without a prior visit to any endemic area. The most recent EM episode was accompanied by nonspecific moderate symptoms such as fatigue and malaise without involvement of internal organs, with the same serological result as found previously. Peripheral blood PCR assay detected Borrelia burgdorferi specific DNA. Intravenous cephalosporin was effective in treating both the skin and extracutaneous signs of the disease.Conclusion.
Recurrent episodes of appropriately treated EM may occur as a result of either reinfection due to contact with another vector tick or persistent infection. Intravenous cephalosporin is likely to be appropriate therapy for recurrent borrelial infection in the skin, in particular when accompanied by general extracutaneous signs and symptoms that might indicate dissemination of the spirochetes.Key words:
erythema migrans – recurrent infection – intravenous cephalosporin.
Autoři: D. Švecová 1; P. Gavornik 2
Působiště autorů: Dpt. of Dermatovenerology, Faculty of Medicine, Comenius University, Bratislava, Slovak Republic 1; nd Dpt. of Internal Medicine, Faculty of Medicine, Comenius University, Bratislava, Slovak Republic Prof. M. Šimaljaková, M. D., PhD. Head of Dpt. Dermatovenerology Faculty of Medicine, Comenius University, Bratislava, Slovak Republic 22
Vyšlo v časopise: Epidemiol. Mikrobiol. Imunol. 79, 2008, č. 3, s. 97-100
Souhrn
Pozadie problému:
Účinná antibiotická liečba, ktorá sa podáva včas, počas klinických prejavov erythema migrans (EM), prerušuje ďalšiu progresiu infekcie a zabraňuje invázii do vnútorných orgánov.Kazuistika:
Autori predkladajú prípad 73-ročnej ženy, u ktorej sa 5-krát opakoval rekurentný EM, napriek adekvátnej antibiotickej liečbe. Pacientka navštívila endemickú oblasť iba raz pred začiatkom ochorenia, a nepozorovala poštípanie kliešťom ani pred prvou epizódou ani pred ďalšími epizódami ochorenia. Po prvej epizóde bolo sérologické vyšetrenie negatívne (IFA, ELISA, Western blot). Pred druhou epizódou nenavštívila endemickú lokalitu a sérologické vyšetrenie bolo hranične pozitívne. Western blot potvrdil Borrelia burgdorferi sensu lato. Posledná epizóda EM sa spájala s nešpecifickými miernymi symptómami ako je únava a nevoľnosť bez postihnutia vnútorných orgánov a s rovnakými hodnotami sérologického vyšetrenia. PCR z periférnej krvi potvrdila DNA špecifické pre Borrelia burgdorferi. Intravenózna aplikácia cefalosporínu účinne podporila resorpciu kožných a extrakutánnych prejavov ochorenia.Záver:
Rekurentné epizódy vhodne liečenej infekcie EM môžu byť zapríčinené buď reinfekciou po opakovanom poštípaní vektorom – kliešťom alebo ako relaps perzistujúcej infekcie. Intravenózna aplikácia cefalosporínov sa považuje za vhodnú terapiu v prípade rekurentnej boriéliovej infekcie kože, najmä ak ju doprevádzajú celkové extrakutánne príznaky a symptómy, ktoré môžu byť prejavom diseminácie spirochét.Kľúčové slová:
erythema migrans, rekurentná infekcia, intravenózne cefalosporíny.Conflict of interest: There was no financial or other arrangement with the company whose product is mentioned in this article.
Ethics: The patient agrees with the depicting of their affected areas of the body according to the Helsinki Declaration of 1975 as revised in Edinburg 2000.
Submission: The article is original and unpublished and not being considered for publication elsewhere.
Introduction
Lyme borreliosis (LB) is considered to be the most common tick-borne disease in the Europe and USA. Effective antibiotic therapy administered early in the course of the clinical presentation of the disease may discontinue the further progression of infection and avoid invasion in intrinsic organs. However, recurrent episodes of appropriately treated infection may reflect either reinfection after subsequent contact with a vector tick or relapse of a persistent infection [5]. Reinfection has been well - documented and can be often recognized clinically by the development of a repeat episode of erythema migrans (EM) rash occurring at a different location on the skin during the season of principal tick vectors being abundant in the environment [6]. Limited date suggest that relapse of persistent infection could be considered as a subsequent EM lesion at the site of previous EM lesion accompanied by persistence of B. burgdorferi antibody between the episodes [1]. Patients with recurrent infections afford an opportunity to study the role of immune response of this disease. Reccurent infection of B.burgdorferi is described rarely in epidemiological studies and in case reports. We would like to draw further attention to this issue with a rare persistent infection.
Case report
73-year old woman was referred for evaluation at Dpt.of Dermatovenerology with recurrent EM after repeated adequate antibiotic treatment. The history started 6 years before succeeded staying in endemic region in Small Carpathy Mountains for one day trip. The patient did not remark a tick bite but the affection with premature infected tick can not bee excluded. The EM lesion was developed after 10 days. The diagnosis was established according to the clinical sign of EM lesion at the site of buttock (erythematous rash of 7x6.5 cm in diameter with active peripheral border 0.5cm), serological examination proved negative (IFA, ELISA, Western blot). The treatment started immediately with doxycycline 2x100 mg for 10 days and revealed resolution of the skin lesion. New episode started 10 months after at the same site of the previous EM lesion. A new EM lesion of 6 cm in diameter was created. The patient did not refer tick bite and did not visit any endemic locality in this actual time. Serological examination proved borderline positive. IFA using the endemic strains of B.burgdorferi sensu lato as antigens found out the positive titer of IgM antibodies as well as of IgG antibodies. ELISA IgM and IgG found bordeline positive. Western blot proved positive for B.burgdorferi sensu lato. Azitromycin was administered in course of 2x500 mg the first day continued with 500 mg daily next 4 days with good efficacy and resolution of the skin lesion. The third recurrent infection occurred again after 9 months with EM lesion on new site of left forearm (6 cm in diameter with active border). The patient did not refer tick bite and did not visit any endemic locality in this actual time. The serological examination proved the same result as previous. Antibiotic treatment started with amoxicillin 3x500 mg for 21 days with appropriate efficacy. The last fourth recurrence of EM started after 10 months on the right forearm accompanied with nonspecific moderate symptoms as fatigue and malaise without elevated temperature and the same value of serological examination. The patient did not refer tick bite and did not visit any endemic locality in this actual time. The general physician admitted the patient to hospitalization because of suspicion of intrinsic organs involvement by LB. Despite the intrinsic organ involvement was not confirmed and the treatment started with ceftriaxone 2g daily for 21 days intravenously. During intravenous infusions of ceftriaxone after two days administration a new recurrent EM occurred at the same site on the buttock (Fig.1). Repeated serological examination confirmed borreliosis using IFA (IgM, IgG), ELISA (IgM, IgG) and Western blot (B.burgdorferisensu lato). PCR with hybridization on peripheral blood demonstrated the Borrelia burgdorferi specific DNA. From the personal history the patient suffered from arterial hypertension. In the past (7 years ago) she underwent hysterectomy proper carcinoma followed with X-ray therapy. Immunological screening did not show discrepancy. Intravenously administration of cephalosporine successfully resolved the skin and extracutaneous signs of the disease as well the nonspecific moderate symptoms as fatigue and malaise. At the 2 years follow up the patient did not complain signs and symptoms of LB.
Obr. 1. Recurrent erythema migrans on the buttock area. The first episode developed 10 days after visiting an endemic area, and was followed by other 4 EM episodes, with EM observed twice at the same site on the buttock. 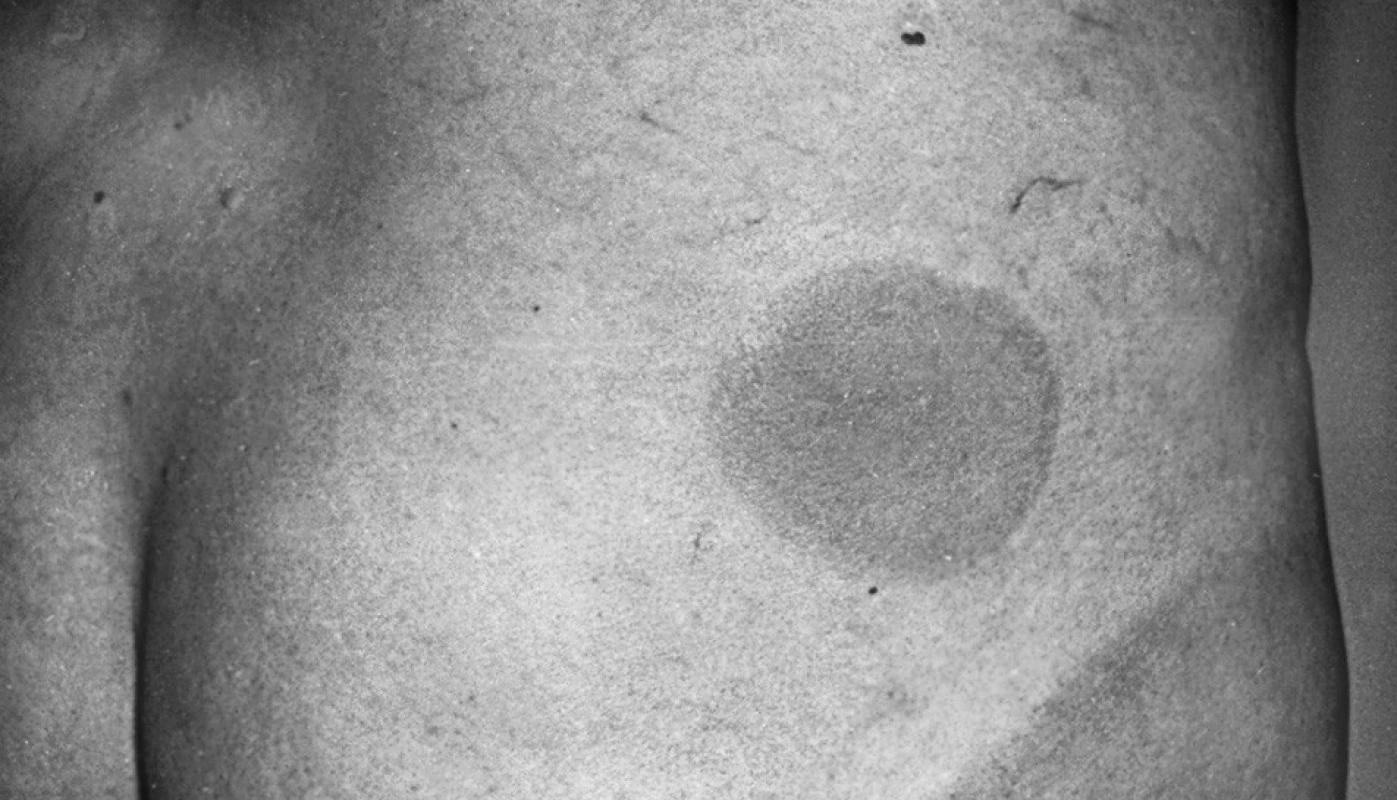
Discussion
Prompt antibiotic therapy effectively eliminates the causative pathogen B.burgdorferi and thereby prevents relapse of LB. However, in spite of the more severe course and more frequent need for retreatment among patients whose immune system was impaired, the outcome of borrelial infection after one year was found out favorable [3]. Despite of this, certain patients who received standard courses of therapy may experience recurrent or persistant symptoms [2]. It was found that B.burgdorferi can persist in resolved EM migrans [8] and in spite of antibiotic therapy and the patients may remain asymptomatic without developing any specific antibodies against B.burgdorferi [4]. Results of experimental infection suggest that B.burgdorferi may disseminate in the skin over a long period of time without causing disease, unless the host’s defense are imbalanced [7]. On the other side in the case of reinfection the mean interval between the first and subsequent episodes is not less than 12 months [1]. Our patient did not remark the tick bite neither before the first episode nor before others. The history started after 10 days staying in endemic region. We support that the patient did not remark the first tick bite because it was done by premature stage of infected tick. Before the next episodes the patient does not have opportunity to be in contact with infectious vector of borreliosis therefore we excluded the possibility of reinfection. The risk of reinfection increases with increased number of tick bites and has seasonal pattern. Limited data suggest that the clinical and laboratory manifestations of reinfection at patients with EM are not different from those of initial infection [1]. We mentioned the recurrence of EM 5-times at our patient. Every episode of EM had the typical clinical sign of the erythematous rash with active border and was treated with antibiotics according to the European guideline for treatment of LB. At last episode the patient suffered from EM lesion and nonspecific moderate symptoms as fatigue and malaise, borrelemia was confirmed using PCR on peripheral blood. In the history of immunodeficiency we did not find the discrepancy in the screening of immune status despite of patient’s advancing age and hysterectomy proper carcinoma in the past. One possible explanation for the eruption of the last lesion at the site of initial EM rash that was created meanwhile cephalosporine intravenous dose may be the response to the released immunochemical substances of the disintegrated borrelial organism. The intravenous administration of cephalosporine could be an appropriate therapy in the case of recurrent borrelial infection in the skin especially if it is accompanied with general extracutaneous signs and symptoms that might indicate dissemination of the spirochetes and there exists association with suspected and discovered imbalanced patient’s immune defense.
Conclusion
Recurrent episodes of appropriately treated EM may reflect either reinfection after subsequent contact with a vector tick or relapse of a persistent infection. Patients with recurrent infections have to be found for immunodeficiency and discrepancy in the screening of immune status. The intravenous administration of cephalosporine could be an appropriate therapy in the case of recurrent borrelial infection in the skin especially if it is accompanied with general extracutaneous signs and symptoms.
Acknowledgements
The authors would like to thank S.Bazovska, M.D. PhD.of Institute of Epidemiology for her laboratory collaboration to this article with recurrent infections afford an opportunity to study the role of immune response of this disease.
Do redakce došlo 25. 1. 2008
Danka Švecová, M.D., PhD., Assoc.Prof.
Dpt. Dermatovenerology
University Hospital
Faculty of Medicine
Comenius University
Mickiewiczova 13
81369 Bratislava
Slovak Republic
e-mail danka.svecova@faneba.sk
Zdroje
1. Krause, P.J., Foley, D.T., Burke, G.S., Christianson, D., Closter, L., Spielman, A. Reinfection and relapse in early lyme disease. Am J Trop Med Hyg, 2006, 75, 1090-1094.
2. Liegner, K.B., Shapiro, J.R., Ramsay, D., Halperin, A.J., Hogrefe, W., Kong, L. Reccurent erythema migrans despite extended antibiotic treatment with minocycline in a patient with persisting Borrelia burgdorferi infection. J Am Acad Derm, 1993, 28, 312-314.
3. Maraspin, V., Lotrič-Furlan, S., Cimperman, J., Ruzic-Sabljic, E., Strle, F. Erythema migrans in the immunocompromised host. Wien Klin Wchsch 1999, 111, 923-932.
4. Maraspin, V., Ruzic-Sabljic, E., Strle, F., Cimperman, J., Jereb, M., Preac-Mursic, V. Persistence of Borrelia burgdorferi after treatment with antibiotics. Alpe Adria Microbiol J, 1995, 4, 211-216.
5. Nadelman, R.B., Wormser, G.P. Reinfection in patients with Lyme disease. Clin Infect Dis, 2007, 45, 1032-1038.
6. Nowakowski, J., Schwarz, I., Nadelman, R.B., Liveris, A., Wguero-Rosenfeld, M., Wormser, G. Culture-confirmed infection and reinfection with Borrelia burgdorferi. Ann Intern Med, 1997, 127,130-132.
7. Straubinger, R.K., Summers, B.A., Chang, J.F., Appel, M.J.G. Persistence of Borrelia burgdorferi in experimentally infected dogs after antibiotic treatment. J Clin Microbiol, 1997, 35, 111–116.
8. Strle, F., Cheng, Y., Cimperman, J., Maraspin, V., Lotric-Furlan, S., Nelson, J.A., Picken, M.M., Ruzic-Sabljic, E., Picken, R.N. Persistence of Borrelia burgdorferi sensu lato in resolved erythema migrans lesions. Clin Infect Dis, 1995, 21, 380-389.
Štítky
Hygiena a epidemiologie Infekční lékařství Mikrobiologie
Článek TEST
Článek vyšel v časopiseEpidemiologie, mikrobiologie, imunologie
Nejčtenější tento týden
2008 Číslo 3- Stillova choroba: vzácné a závažné systémové onemocnění
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
- Diagnostika virových hepatitid v kostce – zorientujte se (nejen) v sérologii
- Jak souvisí postcovidový syndrom s poškozením mozku?
-
Všechny články tohoto čísla
- Aminoglykozidy a kolistín potláčajú tvorbu biofilmu u Klebsiella pneumoniae
- Micromodification of Virus-neutralisation Assay with Vital Staining in 96-well Plate and its Use in Diagnostics of Ťahyňa Virus Infections
- Profesor Ivo Hána osmdesátníkem
- Spomienka na profesora MUDr. Emila Kmetyho, DrSc
- MUDr. Eduard Sajdák, * 6.5.1934 - † 4.5.2008
- TEST
- Časopis Epidemiologie, mikrobiologie, imunologie zařazen do Seznamu recenzovaných neimpaktovaných periodik vydávaných v České republice
- Opomíjené virové infekce přenášené hematofágními členovci v České republice
- Od historických poznatkov a názorov až po súčasné úlohy na poli celiakie
- Reccurent Erythema Migrans as a Persistent Infection
- Epidemiologie, mikrobiologie, imunologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Opomíjené virové infekce přenášené hematofágními členovci v České republice
- Aminoglykozidy a kolistín potláčajú tvorbu biofilmu u Klebsiella pneumoniae
- Od historických poznatkov a názorov až po súčasné úlohy na poli celiakie
- Reccurent Erythema Migrans as a Persistent Infection
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



